Candida Genotyping of Blood Culture Isolates from Patients Admitted to 16 Hospitals in Madrid: Genotype Spreading during the COVID-19 Pandemic Driven by Fluconazole-Resistant C. parapsilosis
Abstract
1. Introduction
2. Materials and Methods
2.1. Isolates Collected and Studied during the CANDIMAD Study
2.2. Microsatellite Genotyping
3. Results
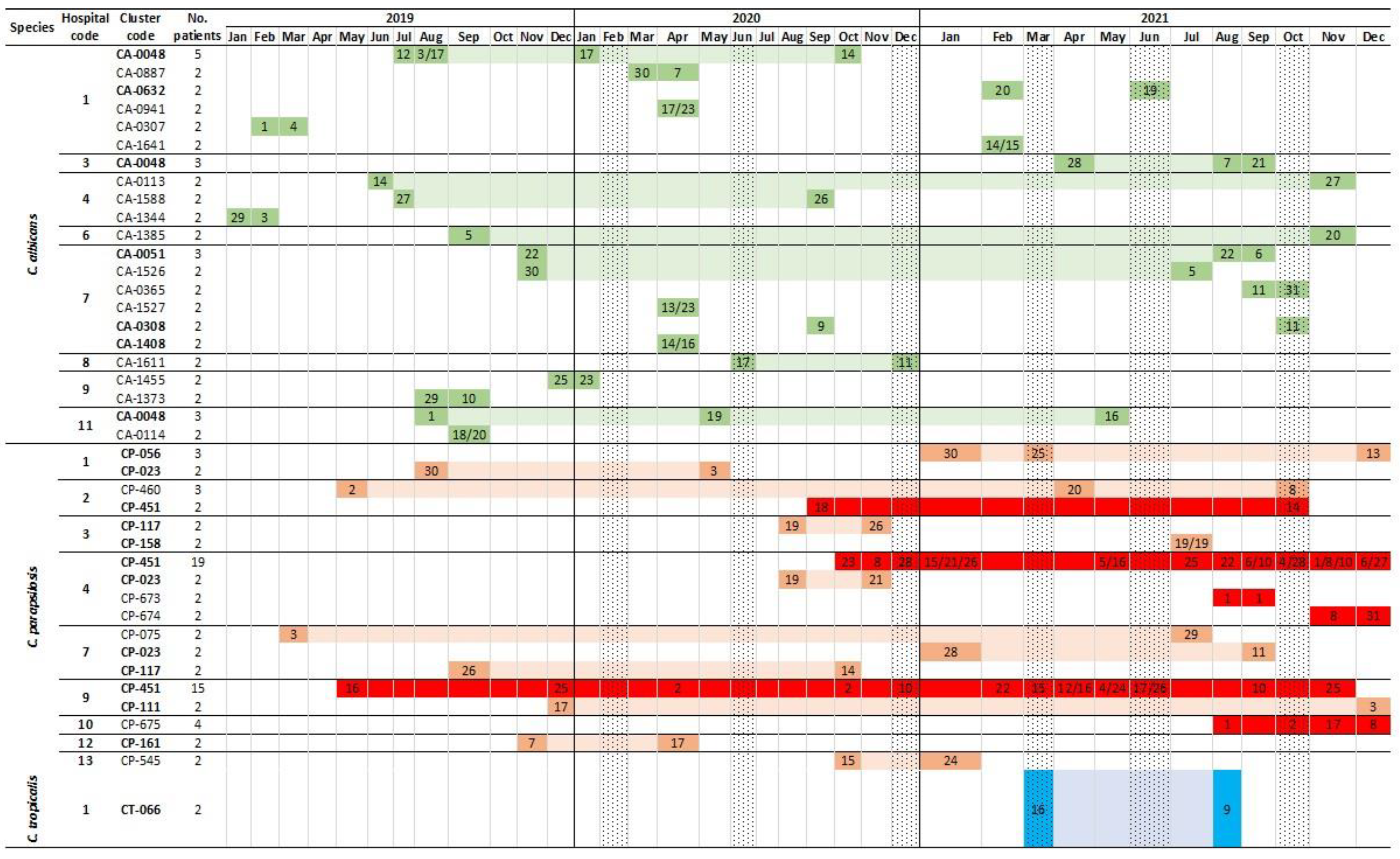
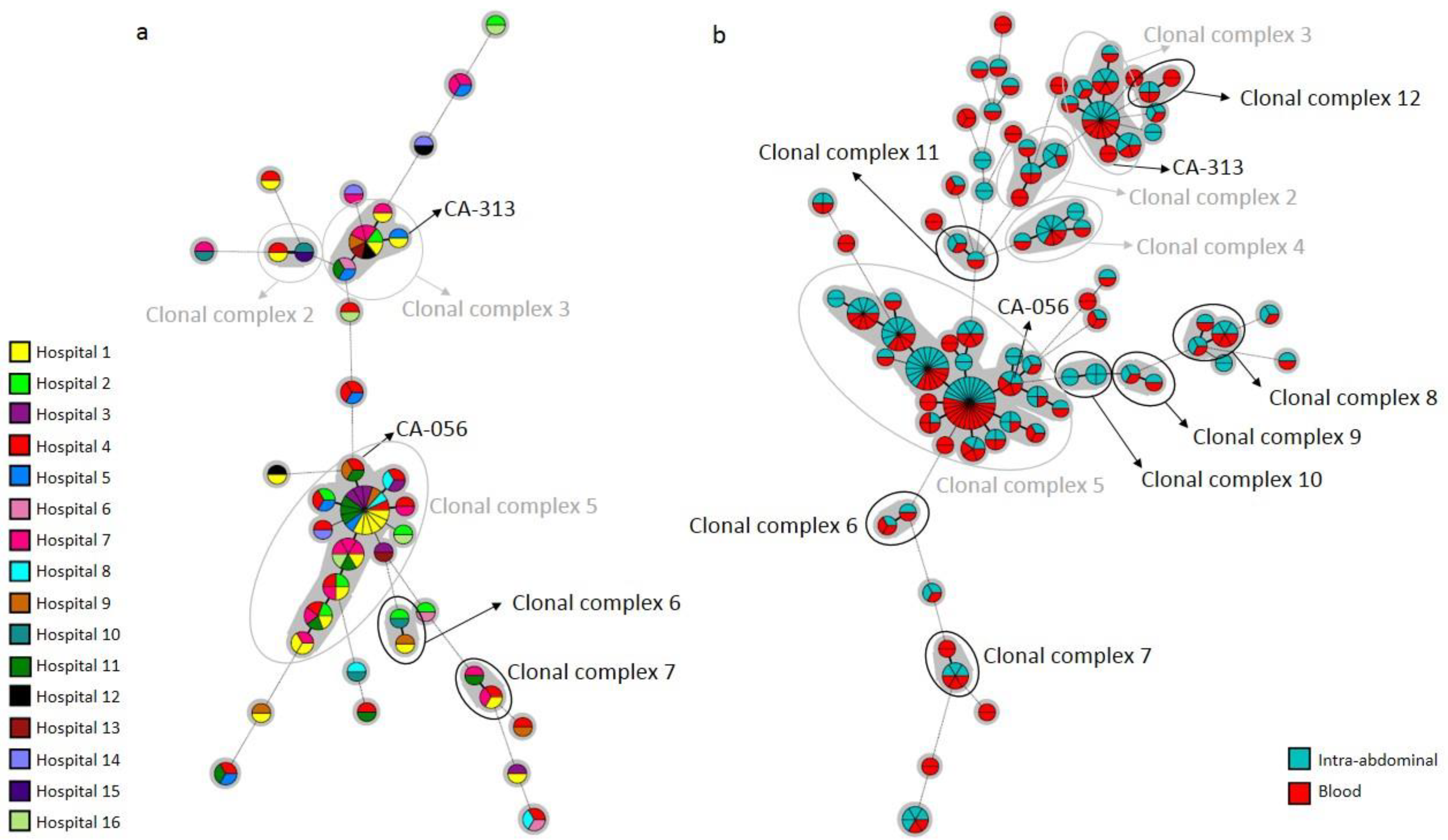
3.1. Genotypes Found in Blood Cultures and Comparisons with Intra-Abdominal Genotypes
3.2. Genotypes Involving Antifungal-Resistant Isolates
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pappas, P.G.; Lionakis, M.S.; Arendrup, M.C.; Ostrosky-Zeichner, L.; Kullberg, B.J. Invasive candidiasis. Nat. Rev. Dis. Primers. 2018, 4, 18026. [Google Scholar] [CrossRef] [PubMed]
- Bassetti, M.; Righi, E.; Ansaldi, F.; Merelli, M.; Scarparo, C.; Antonelli, M.; Garnacho-Montero, J.; Diaz-Martin, A.; Palacios-Garcia, I.; Luzzati, R.; et al. A multicenter multinational study of abdominal candidiasis: Epidemiology, outcomes and predictors of mortality. Intensive Care Med. 2015, 41, 1601–1610. [Google Scholar] [CrossRef] [PubMed]
- Escribano, P.; Guinea, J.; Marcos-Zambrano, L.J.; Martín-Rabadán, P.; Fernández-Cruz, A.; Sánchez-Carrillo, C.; Muñoz, P.; Bouza, E. Is catheter-related candidemia a polyclonal infection? Med. Mycol. 2014, 52, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Guinea, J.; Mezquita, S.; Gómez, A.; Padilla, B.; Zamora, E.; Sánchez-Luna, M.; Muñoz, P.; Escribano, P. Whole genome sequencing confirms Candida albicans and Candida parapsilosis microsatellite sporadic and persistent clones causing outbreaks of candidemia in neonates. Med. Mycol. 2021, 60, myab068. [Google Scholar] [CrossRef] [PubMed]
- Escribano, P.; Rodriguez-Creixems, M.; Sanchez-Carrillo, C.; Munoz, P.; Bouza, E.; Guinea, J. Endemic genotypes of Candida albicans causing fungemia are frequent in the hospital. J. Clin. Microbiol. 2013, 51, 2118–2123. [Google Scholar] [CrossRef][Green Version]
- Guinea, J.; Arendrup, M.C.; Cantón, R.; Cantón, E.; García-Rodríguez, J.; Gómez, A.; Gómez-García-De La Pedrosa, E.; Hare, R.K.; Orden, B.; Sanguinetti, M.; et al. Genotyping Reveals High Clonal Diversity and Widespread Genotypes of Candida Causing Candidemia at Distant Geographical Areas. Front. Cell. Infect. Microbiol. 2020, 10, 166. [Google Scholar] [CrossRef]
- Escribano, P.; Sanchez-Carrillo, C.; Munoz, P.; Bouza, E.; Guinea, J. Reduction in Percentage of Clusters of Candida albicans and Candida parapsilosis Causing Candidemia in a General Hospital in Madrid, Spain. J. Clin. Microbiol. 2018, 56, e00574–18. [Google Scholar] [CrossRef]
- Marcos-Zambrano, L.; Escribano, P.; Sanguinetti, M.; Gómez-García-De La Pedrosa, E.; De Carolis, E.; Vella, A.; Cantón, R.; Bouza, E.; Guinea, J. Clusters of patients with candidaemia due to genotypes of Candida albicans and Candida parapsilosis: Differences in frequency between hospitals. Clin. Microbiol. Infect. 2015, 21, 677–683. [Google Scholar] [CrossRef][Green Version]
- Machado, M.; Estévez, A.; Sánchez-Carrillo, C.; Guinea, J.; Escribano, P.; Alonso, R.; Valerio, M.; Padilla, B.; Bouza, E.; Muñoz, P. Incidence of Candidemia Is Higher in COVID-19 versus Non-COVID-19 Patients, but Not Driven by Intrahospital Transmission. J. Fungi 2022, 8, 305. [Google Scholar] [CrossRef]
- Ramos-Martínez, A.; Pintos-Pascual, I.; Guinea, J.; Gutiérrez-Villanueva, A.; Gutiérrez-Abreu, E.; Díaz-García, J.; Asensio, Á.; Iranzo, R.; Sánchez-Romero, I.; Muñoz-Algarra, M.; et al. Impact of the COVID-19 Pandemic on the Clinical Profile of Candidemia and the Incidence of Fungemia Due to Fluconazole-Resistant Candida parapsilosis. J. Fungi 2022, 8, 451. [Google Scholar] [CrossRef]
- Routsi, C.; Meletiadis, J.; Charitidou, E.; Gkoufa, A.; Kokkoris, S.; Karageorgiou, S.; Giannopoulos, C.; Koulenti, D.; Andrikogiannopoulos, P.; Perivolioti, E.; et al. Epidemiology of Candidemia and Fluconazole Resistance in an ICU before and during the COVID-19 Pandemic Era. Antibiotics 2022, 11, 771. [Google Scholar] [CrossRef] [PubMed]
- Papadimitriou-Olivgeris, M.; Kolonitsiou, F.; Kefala, S.; Spiliopoulou, A.; Aretha, D.; Bartzavali, C.; Siapika, A.; Marangos, M.; Fligou, F. Increased incidence of candidemia in critically ill patients during the Coronavirus Disease 2019 (COVID-19) pandemic. Braz. J. Infect. Dis. 2022, 26, 102353. [Google Scholar] [CrossRef] [PubMed]
- Nucci, M.; Barreiros, G.; Guimarães, L.F.; Deriquehem, V.A.S.; Castiñeiras, A.C.; Nouér, S.A. Increased incidence of candidemia in a tertiary care hospital with the COVID-19 pandemic. Mycoses 2021, 64, 152–156. [Google Scholar] [CrossRef] [PubMed]
- Thomaz, D.Y.; Del Negro, G.M.B.; Ribeiro, L.B.; da Silva, M.; Carvalho, G.O.M.H.; Camargo, C.H.; de Almeida, J.N.; Motta, A.L.; Siciliano, R.F.; Sejas, O.N.E.; et al. A Brazilian Inter-Hospital Candidemia Outbreak Caused by Fluconazole-Resistant Candida parapsilosis in the COVID-19 Era. J. Fungi 2022, 8, 100. [Google Scholar] [CrossRef] [PubMed]
- Díaz-García, J.; Gómez, A.; Alcalá, L.; Reigadas, E.; Sánchez-Carrillo, C.; Pérez-Ayala, A.; Pérez-Ayala, A.; Gómez-García de la Pedrosa, E.; González-Romo, F.; Merino-Amador, P.; et al. Evidence of Fluconazole-Resistant Candida parapsilosis Genotypes Spreading across Hospitals Located in Madrid, Spain and Harboring the Y132F ERG11p Substitution. Antimicrob Agents Chemother. 2022, 66, e0071022. [Google Scholar] [CrossRef]
- Díaz-García, J.; Gómez, A.; Machado, M.; Alcalá, L.; Reigadas, E.; Sánchez-Carrillo, C.; Pérez-Ayala, A.; Gómez-García-De-La-Pedrosa, E.; González-Romo, F.; Cuétara, M.S.; et al. Blood and intra-abdominal Candida spp. from a multicentre study conducted in Madrid using EUCAST: Emergence of fluconazole resistance in Candida parapsilosis, low echinocandin resistance and absence of Candida auris. J. Antimicrob. Chemother. 2022, 77, 3102–3109. [Google Scholar] [CrossRef]
- Pfaller, M.A.; Andes, D.; Diekema, D.J.; Espinel-Ingroff, A.; Sheehan, D.; CLSI Subcommittee for Antifungal Susceptibility Testing. Wild-type MIC distributions, epidemiological cutoff values and species-specific clinical breakpoints for fluconazole and Candida: Time for harmonization of CLSI and EUCAST broth microdilution methods. Drug Resist. Updat. 2010, 13, 180–195. [Google Scholar] [CrossRef]
- Díaz-García, J.; Mesquida, A.; Sánchez-Carrillo, C.; Reigadas, E.; Muñoz, P.; Escribano, P.; Guinea, J. Monitoring the Epidemiology and Antifungal Resistance of Yeasts Causing Fungemia in a Tertiary Care Hospital in Madrid, Spain: Any Relevant Changes in the Last 13 Years? Antimicrob. Agents Chemother. 2021, 65, e01827-20. [Google Scholar] [CrossRef]
- Botterel, F.; Desterke, C.; Costa, C.; Bretagne, S. Analysis of microsatellite markers of Candida albicans used for rapid typing. J. Clin. Microbiol. 2001, 39, 4076–4081. [Google Scholar] [CrossRef]
- Sampaio, P.; Gusmão, L.; Correia, A.; Alves, C.; Rodrigues, A.G.; Pina-Vaz, C.; Amorim, A.; Pais, C. New Microsatellite Multiplex PCR for Candida albicans Strain Typing Reveals Microevolutionary Changes. J. Clin. Microbiol. 2005, 43, 3869–3876. [Google Scholar] [CrossRef]
- Sabino, R.; Sampaio, P.; Rosado, L.; Stevens, D.A.; Clemons, K.V.; Pais, C. New polymorphic microsatellite markers able to distinguish among Candida parapsilosis sensu stricto isolates. J. Clin. Microbiol. 2010, 48, 1677–1682. [Google Scholar] [CrossRef] [PubMed]
- Vaz, C.; Sampaio, P.; Clemons, K.V.; Huang, Y.C.; Stevens, D.A.; Pais, C. Microsatellite multilocus genotyping clarifies the relationship of Candida parapsilosis strains involved in a neonatal intensive care unit outbreak. Diagn. Microbiol. Infect. Dis. 2011, 71, 159–162. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Zhou, H.-J.; Che, J.; Li, W.-G.; Bian, F.-N.; Yu, S.-B.; Zhang, L.-J.; Lu, J. Multilocus microsatellite markers for molecular typing of Candida tropicalis isolates. BMC Microbiol. 2014, 14, 245. [Google Scholar] [CrossRef] [PubMed]


| Hospital Code | Clinical Source and No. Isolates | ||||||
|---|---|---|---|---|---|---|---|
| Blood Cultures | Intra-Abdominal Samples | Overall | |||||
| C. albicans | C. parapsilosis | C. tropicalis | C. albicans | C. parapsilosis | C. tropicalis | ||
| 1 | 90 | 32 | 16 | 88 | 18 | 12 | 256 |
| 2 | 34 | 20 | 5 | 104 | 9 | 16 | 188 |
| 3 | 42 | 22 | 2 | 85 | 9 | 8 | 168 |
| 4 | 75 | 57 | 6 | 18 | 4 | 1 | 161 |
| 5 | 30 | 13 | 3 | 44 | 13 | 4 | 107 |
| 6 | 21 | 4 | 3 | 67 | 4 | 10 | 109 |
| 7 | 57 | 36 | 8 | 5 | 2 | 0 | 108 |
| 8 | 25 | 5 | 2 | 57 | 11 | 4 | 104 |
| 9 | 41 | 35 | 4 | 19 | 5 | 3 | 107 |
| 10 | 20 | 8 | 2 | 39 | 6 | 4 | 79 |
| 11 | 21 | 12 | 2 | 6 | 0 | 2 | 43 |
| 12 | 11 | 9 | 2 | 7 | 0 | 1 | 30 |
| 13 | 4 | 7 | 1 | 8 | 1 | 1 | 22 |
| 14 | 6 | 6 | 1 | 2 | 0 | 1 | 16 |
| 15 | 5 | 5 | 0 | 2 | 1 | 1 | 14 |
| 16 | 7 | 0 | 0 | 1 | 0 | 0 | 8 |
| Overall | 489 | 271 | 57 | 552 | 83 | 68 | 1520 * |
| C. albicans | C. parapsilosis | C. tropicalis | |
|---|---|---|---|
| Isolates/patients | 489 | 271 | 57 |
| Genotypes | 399 | 182 | 47 |
| Singleton, n (%) | 346 (86.7%) | 158 (86.8%) | 41 (87.2%) |
| Cluster, n (%) | 53 (13.3%) | 24 (13.2%) | 6 (12.8%) |
| Isolates/patients in cluster, n (%) | 143 (29.2%) | 113 (41.7%) | 16 (28.1%) |
| Range of isolates/patients per cluster | 2–15 | 2–37 | 2–4 |
| Intra-hospital cluster, n (%) | 14 (26.4%) | 6 (25.0%) | 0 (0.0%) |
| Widespread cluster, n (%) * | 39 (73.6%) | 18 (75.0%) | 6 (100%) |
| Hospital Code | Frequencies of Combinations of Widespread Genotypes | Numbers of Widespread Genotypes | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | C. albicans | C. parapsilosis | Total | |
| 1 | 3 | 2 | 6 | 2 | 0 | 7 | 1 | 4 | 0 | 3 | 2 | 1 | 0 | 0 | 1 | 15 | 5 | 20 | |
| 2 | 2 | 0 | 3 | 1 | 1 | 3 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 2 | 8 | 4 | 12 | |
| 3 | 1 | 0 | 2 | 1 | 0 | 0 | 2 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 4 | 6 | 10 | |
| 4 | 3 | 3 | 1 | 4 | 1 | 4 | 3 | 3 | 0 | 5 | 0 | 0 | 1 | 0 | 1 | 17 | 7 | 24 | |
| 5 | 3 | 2 | 1 | 3 | 1 | 1 | 1 | 1 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 7 | 7 | 14 | |
| 6 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 3 | 1 | 4 | |
| 7 | 1 | 1 | 2 | 2 | 2 | 1 | 0 | 1 | 1 | 3 | 1 | 1 | 1 | 0 | 1 | 12 | 6 | 18 | |
| 8 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 4 | 1 | 5 | |
| 9 | 3 | 3 | 3 | 3 | 4 | 1 | 3 | 0 | 0 | 2 | 1 | 1 | 0 | 0 | 0 | 6 | 8 | 14 | |
| 10 | 0 | 1 | 1 | 0 | 0 | 0 | 2 | 0 | 2 | 0 | 0 | 0 | 0 | 1 | 0 | 4 | 3 | 7 | |
| 11 | 2 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 1 | 8 | 3 | 11 | |
| 12 | 1 | 0 | 2 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 3 | 3 | 6 | |
| 13 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 2 | |
| 14 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 1 | 4 | |
| 15 | 1 | 2 | 0 | 2 | 1 | 1 | 1 | 0 | 2 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 2 | 3 | |
| 16 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 0 | 4 | |
| Hospital Code | Candidaemia Incidence (Cases per 100,000 Hospital Admissions) | |||||
|---|---|---|---|---|---|---|
| Overall (No. of Admissions) * | C. albicans (2019/2020/2021) | C. parapsilosis (2019/2020/2021) | C. tropicalis (2019/2020/2021) | |||
| 2019 | 2020 | 2021 | ||||
| 1 α | 114.8 (47,048) | 155.5 (42,444) | 135.7 (35,377) | 53.1/69.6/70.7 α | 31.9/16.5/28.3 | 10.6/14.1/14.1 |
| 2 | 50.7 (45,357) | 63.0 (39,669) | 78.3 (39,607) | 22.0/35.3/25.2 | 15.4/7.6/25.2 | 4.4/2.5/5.0 |
| 3 β | 83.2 (32,442) | 51.4 (60,348) | 83.3 (40,832) | 40.1/24.9/34.3 | 21.6/13.3/17.1 | 0.0/0.0/4.9 |
| 4 γ | 152.9 (31,399) | 201.1 (27,841) | 231.6 (28,067) | 86.0/89.9/81.9 | 38.2/53.9/106.9 β,γ | 12.7/3.6/3.6 |
| 5 | 130.7 (16,064) | 208.8 (13,886) | 137.2 (13,848) | 49.8/108.0/50.5 | 37.4/43.2/7.2 | 0.0/7.2/14.4 |
| 6 α | 53.6 (18,671) | 125.3 (16,755) | 77.4 (16,786) | 16.1/53.7/53.6 | 10.7/11.9/0.0 | 0.0/11.9/6.0 |
| 7 α,γ | 65.6 (48,757) | 131.2 (44,196) | 109.0 (44,949) | 20.5/58.8/46.7 α,γ | 16.4/45.3/17.8 α, β | 4.1/2.3/11.1 |
| 8 β | 104.8 (15,268) | 129.1 (13,940) | 55.6 (14,388) | 58.9/71.7/41.7 | 13.1/14.3/7.0 | 0.0/7.2/7.0 |
| 9 | 117.7 (26,348) | 171.8 (24,454) | 130.2 (24,577) | 45.5/102.2/16.3 α, β | 26.6/40.9/73.2 γ | 11.4/4.1/0.0 |
| 10 α,γ | 61.3 (13,049) | 150.6 (11,288) | 124.1 (11,283) | 30.7/88.6/53.2 | 7.7/17.7/44.3 | 15.3/0.0/0.0 |
| 11 | 87.4 (16,012) | 94.3 (15,902) | ND | 50.0/44.0/ND | 25.0/6.3/ND | 6.2/6.3/ND |
| 12 | 44.2 (15,826) | 86.8 (14,969) | 51.6 (15,501) | 19.0/33.4/19.4 | 19.0/33.4/6.5 | 0.0/13.4/0.0 |
| 13 α | 11.1 (9045) | 80.9 (8656) | ND | 0.0/23.1/ND | 11.1/34.7/ND | 0.0/11.6/ND |
| 14 | 34.9 (11,471) | 83.2 (9620) | ND | 26.2/10.4/ND | 8.7/31.2/ND | 0.0/10.4/ND |
| 15 | 86.2 (8116) | 14.4 (6946) | ND | 37.0/14.4/ND | 24.6/0.0/ND | 0.0/0.0/ND |
| 16 | 88.8 (4504) | 0.0 (4146) | ND | 66.6/0.0/ND | 0.0/0.0/ND | 0.0/0.0/ND |
| Overall α,γ | 85.4 (359,377) | 114.6 (355,060) | 112.9 (285,215) ** | 39.2/58.0/44.9 α, β | 21.7/24.5/31.9 γ | 5.3/5.4/6.7 |
| Species | Genotype | Hospitals Involved | Patients Involved | No. of Isolates and Source | Phenotypic Resistance | FKSp Substitution | ERG11p Substitution | |
|---|---|---|---|---|---|---|---|---|
| Blood | Intra -Abdominal | |||||||
| C. albicans | CA-0056 * | H9 | 1 | 0 | 1 | Echinocandin | F641L FKS1 HS1 | ND |
| CA-0511 | H6 | 2 | 1 | 1 | Echinocandin | S645P FKS1 HS1 | ND | |
| CA-1341 | H6 | 1 | 0 | 1 | Echinocandin | S645P FKS1 HS1 | ND | |
| CA-1872 | H2 | 1 | 1 | 0 | Echinocandin | R1361H FKS1 HS2 | ND | |
| CA-0313 ** | H1 | 1 | 1 | 0 | Fluconazole | ND | None | |
| CA-1283 | H7 | 1 | 1 | 0 | Fluconazole | ND | D115E, K128T, F145L, I471L/I | |
| CA-1505 | H2 | 1 | 0 | 1 | Fluconazole | ND | A114S, Y257H | |
| CA-1674 | H1 | 1 | 0 | 1 | Fluconazole | ND | None | |
| CA-1762 | H9 | 1 | 1 | 0 | Fluconazole | ND | D116E/D, D153E/D | |
| C. parapsilosis | CP-540 | H9 | 1 | 0 | 1 | Echinocandin | None | ND |
| CP-451 | H2, H4, H9, H15 | 39 | 37 | 2 | Fluconazole | ND | Y132F, R398I | |
| CP-673 | H4 | 2 | 2 | 0 | Fluconazole | ND | Y132F, R398I | |
| CP-674 | H4 | 2 | 2 | 0 | Fluconazole | ND | Y132F, R398I | |
| CP-675 | H10 | 5 | 4 | 1 | Fluconazole | ND | G458S | |
| C. tropicalis | CT-031 *** | H10 | 1 | 0 | 1 | Echinocandin | S654P/S FKS1 HS1 + V1352I/V, V1404I/V FKS1 | ND |
| CT-081 | H6 | 1 | 0 | 1 | Fluconazole | ND | None | |
| CT-313 | H7 | 1 | 1 | 0 | Fluconazole | ND | F449V | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Díaz-García, J.; Gómez, A.; Machado, M.; Alcalá, L.; Reigadas, E.; Sánchez-Carrillo, C.; Pérez-Ayala, A.; de la Pedrosa, E.G.-G.; González-Romo, F.; Cuétara, M.S.; et al. Candida Genotyping of Blood Culture Isolates from Patients Admitted to 16 Hospitals in Madrid: Genotype Spreading during the COVID-19 Pandemic Driven by Fluconazole-Resistant C. parapsilosis. J. Fungi 2022, 8, 1228. https://doi.org/10.3390/jof8111228
Díaz-García J, Gómez A, Machado M, Alcalá L, Reigadas E, Sánchez-Carrillo C, Pérez-Ayala A, de la Pedrosa EG-G, González-Romo F, Cuétara MS, et al. Candida Genotyping of Blood Culture Isolates from Patients Admitted to 16 Hospitals in Madrid: Genotype Spreading during the COVID-19 Pandemic Driven by Fluconazole-Resistant C. parapsilosis. Journal of Fungi. 2022; 8(11):1228. https://doi.org/10.3390/jof8111228
Chicago/Turabian StyleDíaz-García, Judith, Ana Gómez, Marina Machado, Luis Alcalá, Elena Reigadas, Carlos Sánchez-Carrillo, Ana Pérez-Ayala, Elia Gómez-García de la Pedrosa, Fernando González-Romo, María Soledad Cuétara, and et al. 2022. "Candida Genotyping of Blood Culture Isolates from Patients Admitted to 16 Hospitals in Madrid: Genotype Spreading during the COVID-19 Pandemic Driven by Fluconazole-Resistant C. parapsilosis" Journal of Fungi 8, no. 11: 1228. https://doi.org/10.3390/jof8111228
APA StyleDíaz-García, J., Gómez, A., Machado, M., Alcalá, L., Reigadas, E., Sánchez-Carrillo, C., Pérez-Ayala, A., de la Pedrosa, E. G.-G., González-Romo, F., Cuétara, M. S., García-Esteban, C., Quiles-Melero, I., Zurita, N. D., Algarra, M. M., Durán-Valle, M. T., Sánchez-García, A., Muñoz, P., Escribano, P., Guinea, J., & on behalf of the CANDIMAD Study Group. (2022). Candida Genotyping of Blood Culture Isolates from Patients Admitted to 16 Hospitals in Madrid: Genotype Spreading during the COVID-19 Pandemic Driven by Fluconazole-Resistant C. parapsilosis. Journal of Fungi, 8(11), 1228. https://doi.org/10.3390/jof8111228









