Shift in Epidemiology of Cryptococcal Infections in Ottawa with High Mortality in Non-HIV Immunocompromised Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Analysis
2.3. Ethical Approval
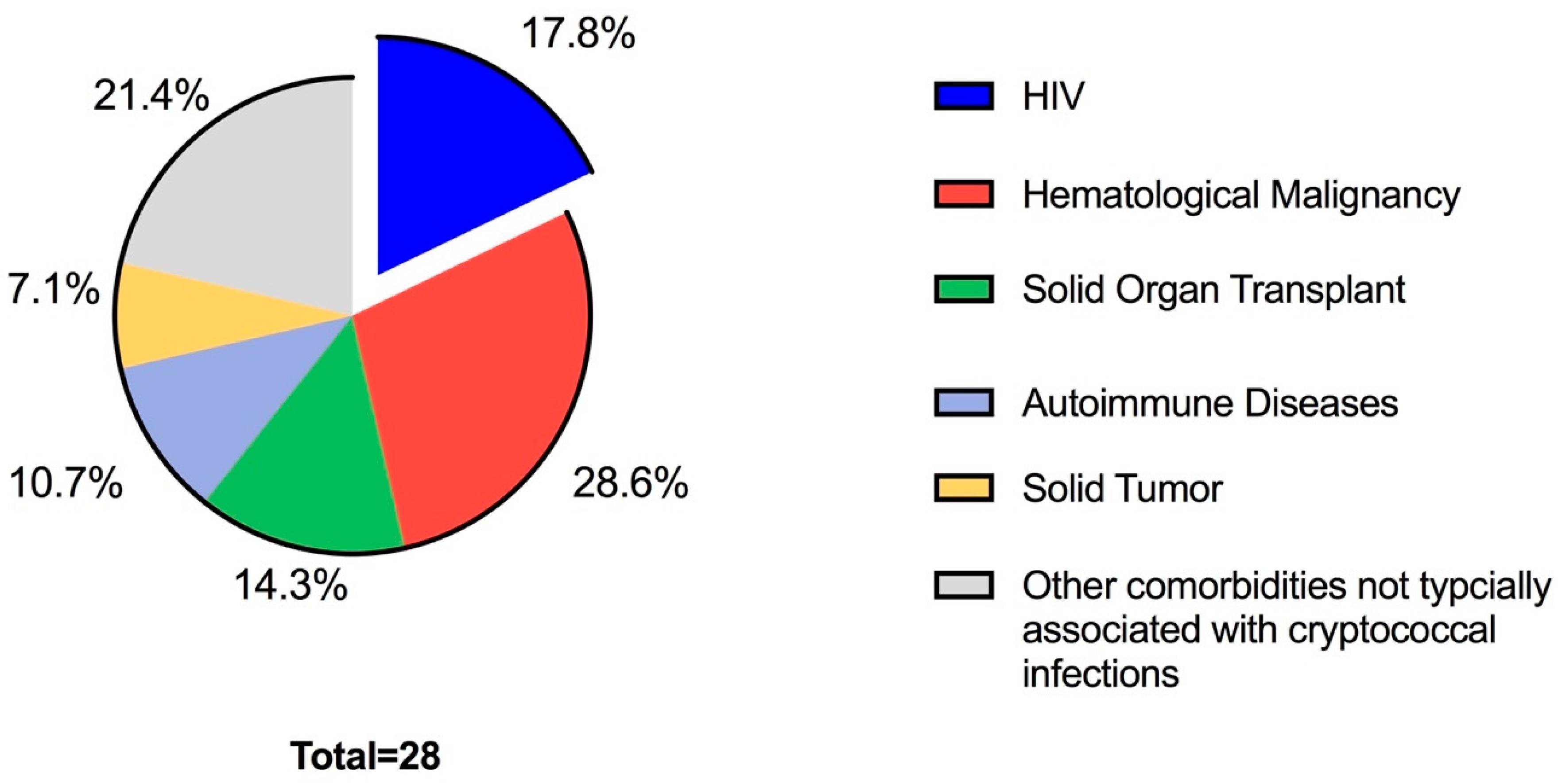
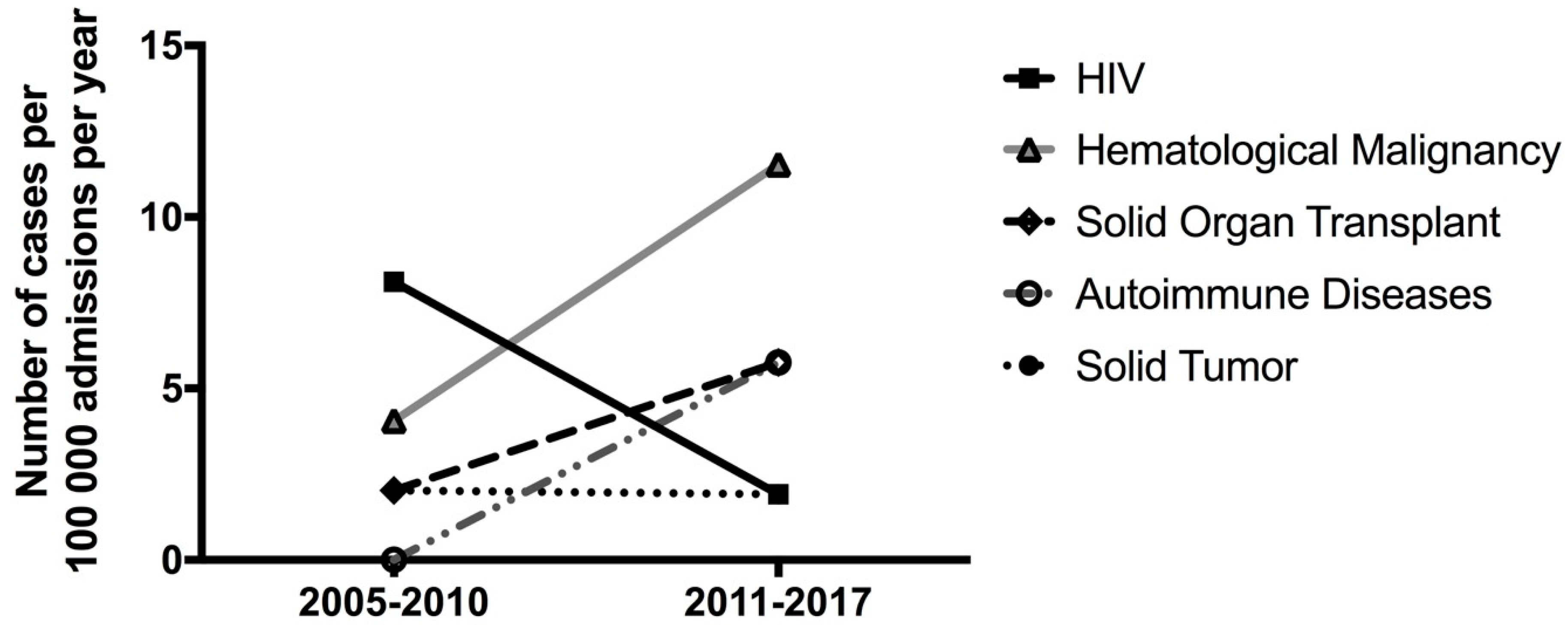
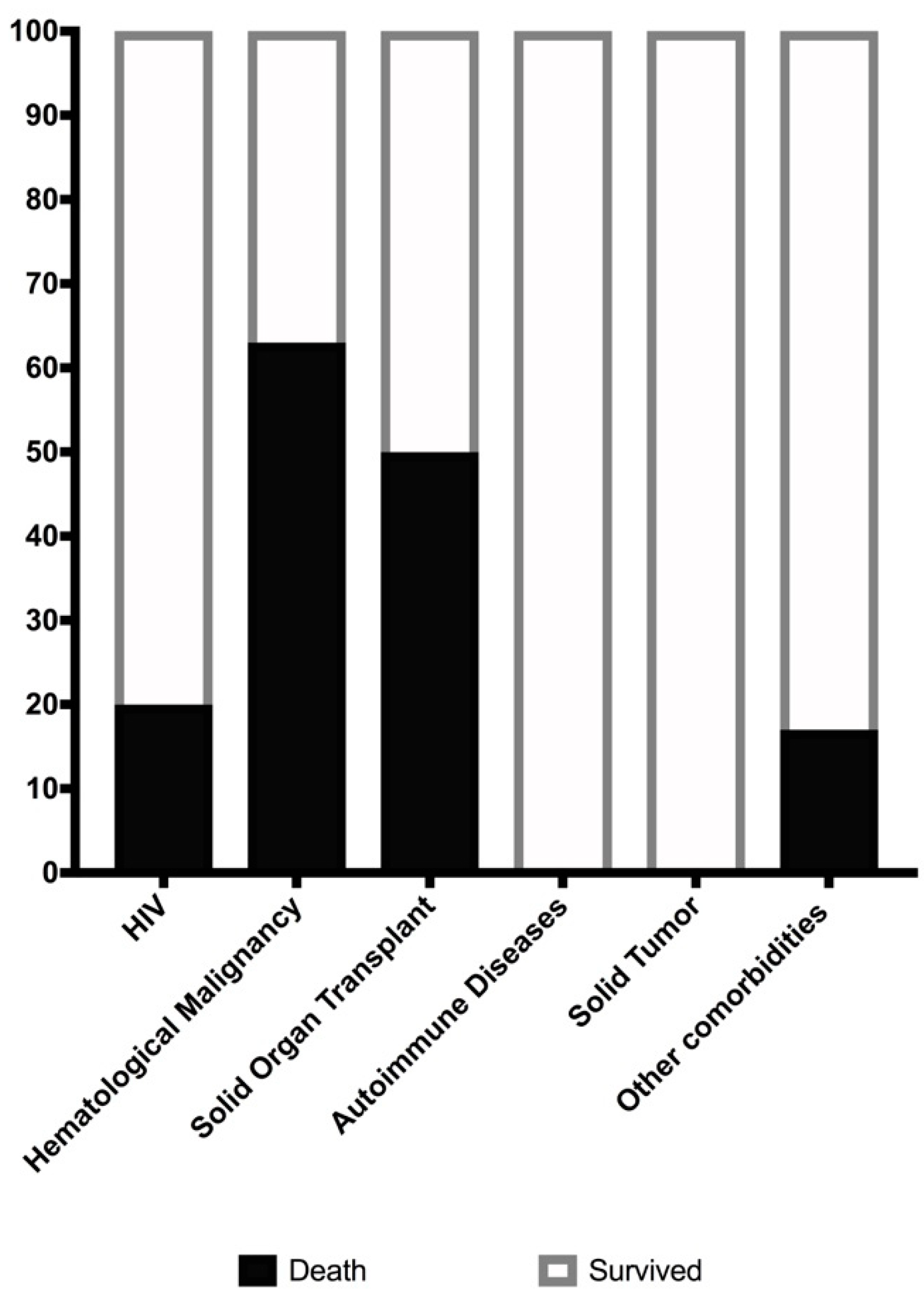
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Mitchell, T.G.; Perfect, J.R. Cryptococcosis in the era of AIDS - 100 years after the discovery of Crypotcoccus neoformans. Clin. Microbiol. Rev. 1995, 8, 515–548. [Google Scholar] [CrossRef] [PubMed]
- Chan, M.; Lye, D.; Win, M.K.; Chow, A.; Barkham, T. Clinical and microbiological characteristics of cryptococcosis in Singapore: Predominance of Cryptococcus neoformans compared with Cryptococcus gattii. Int. J. Infect. Dis. 2014, 26, 110–115. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Aguiar, P.A.D.F.; Pedroso, R.D.S.; Borges, A.S.; Moreira, T.A.; Araújo, L.B.; Röder, D.V.D.B. The epidemiology of cryptococcosis and the characterization of cryptococcus neoformans isolated in a Brazilian university hospital. Rev. Inst. Med. Trop. Sao Paulo 2017, 59, 13. [Google Scholar] [CrossRef] [PubMed]
- Antinori, S. New Insights into HIV/AIDS-Associated Cryptococcosis. ISRN AIDS 2013, 2013, 471363. [Google Scholar] [CrossRef] [PubMed]
- Park, B.J.; Wannemuehler, K.A.; Marston, B.J.; Govender, N.; Pappas, P.G.; Chiller, T.M. Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS. AIDS 2009, 23, 525–530. [Google Scholar] [CrossRef] [PubMed]
- Pappas, P.G. Cryptococcal infections in non-HIV-infected patients. Trans. Am. Clin. Climatol. Assoc. 2013, 124, 61–79. [Google Scholar] [PubMed]
- Mirza, S.A.; Phelan, M.; Rimland, D.; Graviss, E.; Hamill, R.; Brandt, M.E.; Gardner, T.; Sattah, M.; de Leon, G.P.; Baughman, W.; et al. The Changing Epidemiology of Cryptococcosis: An Update from Population-Based Active Surveillance in 2 Large Metropolitan Areas, 1992–2000. Clin. Infect. Dis. 2003, 36, 789–794. [Google Scholar] [CrossRef] [PubMed]
- Gassiep, I.; McDougall, D.; Douglas, J.; Francis, R.; Playford, E.G. Cryptococcal infections in solid organ transplant recipients over a 15-year period at a state transplant center. Transpl. Infect. Dis. 2017, 19, 12639. [Google Scholar] [CrossRef] [PubMed]
- Pappas, P.G.; Perfect, J.R.; Cloud, G.A.; Larsen, R.A.; Pankey, G.A.; Lancaster, D.J.; Henderson, H.; Kauffman, C.A.; Hass, D.W.; Saccente, M.; et al. Cryptococcosis in Human Immunodeficiency Virus–Negative Patients in the Era of Effective Azole Therapy. Clin. Infect. Dis. 2002, 33, 690–699. [Google Scholar] [CrossRef] [PubMed]
- Brizendine, K.D.; Baddley, J.W.; Pappas, P.G. Predictors of Mortality and Differences in Clinical Features among Patients with Cryptococcosis According to Immune Status. PLoS ONE 2013, 8, e60431. [Google Scholar] [CrossRef] [PubMed]
- Allahmoradi, E.; Taghiloo, S.; Tehrani, M.; Hossein-Nattaj, H.; Janbabaei, G.; Shekarriz, R.; Asgarian-Omran, H. CD4+ T Cells are Exhausted and Show Functional Defects in Chronic Lymphocytic Leukemia. Iran. J. Immunol. 2017, 14, 257–269. [Google Scholar] [PubMed]
- Forconi, F.; Moss, P. Perturbation of the normal immune system in patients with CLL. Blood 2015, 126, 573–581. [Google Scholar] [CrossRef] [PubMed]
- Suleman, A.; Padmore, R.; Faught, C.; Cowan, J. Disseminated cryptococcal infection in a patient with treatment-naive chronic lymphocytic leukemia (CLL). IDCases 2019, 17, 566. [Google Scholar] [CrossRef] [PubMed]
- Yoon, H.A.; Felsen, U.; Wang, T.; Pirofski, L. Cryptococcus neoformans infection in Human Immunodeficiency Virus (HIV)-infected and HIV-uninfected patients at an inner-city tertiary care hospital in the Bronx. Med. Mycol. 2019, 1–10. [Google Scholar] [CrossRef] [PubMed]
| Age | Sex | Underlying Medical Disease | Treatment of Underlying Condition within 6 Months of Cryptococcal Diagnosis | Site of Positive Culture | Treatment of Cryptococcal Infection | Outcome Following Cryptococcal Infection | Follow-Up Time |
|---|---|---|---|---|---|---|---|
| 56 | M | HIV | Anti-retroviral therapy | CSF | Amphotericin B and fluconazole | Resolved | 129 months |
| 35 | F | HIV | None | CSF | None | Death | 2 days |
| 53 | M | HIV | None | CSF and blood | Fluconazole | Resolved | 132 months |
| 54 | M | HIV | None | CSF | Amphotericin B and fluconazole | Resolved | 98 months |
| 59 | M | HIV | Anti-retroviral therapy | Bronchial washing | Fluconazole | Resolved | 142 months |
| 72 | M | Acute myeloid leukemia | Azacitidine | Blood | None | Death | 9 days |
| 77 | M | Multiple myeloma | Melphalan and dexamethasone | Blood | None | Death | 7 days |
| 62 | M | Hairy cell leukemia, and cirrhosis from chronic hepatitis B | None | Blood | Amphotericin B and fluconazole | Death | 6 days |
| 63 | M | Chronic lymphocytic leukemia | None | Blood, CSF, Skin | Amphotericin B and fluconazole | Resolved | 32 months |
| 85 | M | Chronic lymphocytic leukemia and bladder cancer | Prednisone 5 mg daily | BAL | Itraconazole then fluconazole | Resolved but deceased 2 years later from cancer | 33 months |
| 43 | M | Acute myeloid leukemia | Cytarabine and idarubicin (1 cycle) | Sputum | Amphotericin B, and fluconazole | Resolved | 33 months |
| 84 | M | Chronic lymphocytic leukemia | No documentation | Blood | None | Death | 7 days |
| 72 | M | Chronic lymphocytic leukemia | Chlorambucil and prednisone | Blood | Amphotericin B | Death | 18 days |
| 64 | M | Kidney transplantation | Prednisone, tacrolimus and mycophenolate | Blood | None | Death | 1 day |
| 61 | F | Kidney transplantation | Prednisone, tacrolimus and mycophenolate | Blood | Fluconazole | Death | 86 days |
| 70 | F | Liver and kidney transplantation | Prednisone, tacrolimus and mycophenolate | BAL | None* | Resolved | 84 months |
| 64 | M | Kidney transplantation | Prednisone, tacrolimus and mycophenolate | CSF | Fluconazole | Resolved | 172 months |
| 53 | M | Sarcoidosis | Prednisone | BAL | Fluconazole | Resolved | 99 months |
| 72 | F | Sjogren’s syndrome and rheumatoid arthritis | Prednisone, methotrexate, and leflunomide | BAL | Fluconazole | Resolved | 32 months |
| 74 | M | Sarcoidosis | Prednisone and azathioprine | Skin | Fluconazole | Resolved | 25 months |
| 63 | M | Lung cancer | None | BAL | None** | Death from metastatic lung cancer | 45 days |
| 65 | F | Papillary thyroid cancer | None | BAL | Fluconazole | Resolved | 113 months |
| 77 | M | Asthma | Ciclesonide, Fluticasone, and Salbutamol | BAL | Fluconazole | Resolved | 40 months |
| 59 | F | Asthma | Fluticasone and Salbutamol | BAL | Fluconazole | Resolved | 131 months |
| 73 | F | End stage renal disease | Hemodialysis | Blood | None | Death | 3 days |
| 53 | M | Diabetes | Insulin glargine and insulin aspart | BAL | Fluconazole | Resolved | 62 months |
| 73 | M | End stage renal disease | Peritoneal dialysis | Peritoneal fluid | Fluconazole | Resolved | 104 months |
| 73 | M | Chronic obstructive pulmonary disease, chronic kidney disease | Fluticasone, Salbutamol, and Tiotropium | BAL | Fluconazole | Resolved but deceased later from abdominal aortic aneurysm rupture | 22 months |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patel, V.; Desjardins, M.; Cowan, J. Shift in Epidemiology of Cryptococcal Infections in Ottawa with High Mortality in Non-HIV Immunocompromised Patients. J. Fungi 2019, 5, 104. https://doi.org/10.3390/jof5040104
Patel V, Desjardins M, Cowan J. Shift in Epidemiology of Cryptococcal Infections in Ottawa with High Mortality in Non-HIV Immunocompromised Patients. Journal of Fungi. 2019; 5(4):104. https://doi.org/10.3390/jof5040104
Chicago/Turabian StylePatel, Vishesh, Marc Desjardins, and Juthaporn Cowan. 2019. "Shift in Epidemiology of Cryptococcal Infections in Ottawa with High Mortality in Non-HIV Immunocompromised Patients" Journal of Fungi 5, no. 4: 104. https://doi.org/10.3390/jof5040104
APA StylePatel, V., Desjardins, M., & Cowan, J. (2019). Shift in Epidemiology of Cryptococcal Infections in Ottawa with High Mortality in Non-HIV Immunocompromised Patients. Journal of Fungi, 5(4), 104. https://doi.org/10.3390/jof5040104





