Chronic Pulmonary Aspergillosis in Patients with Underlying Respiratory Disorders in Cuba—A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Clinical Samples
2.3. Isolates Identification
2.4. Serology
2.5. Treatment
2.6. Statistical Analysis
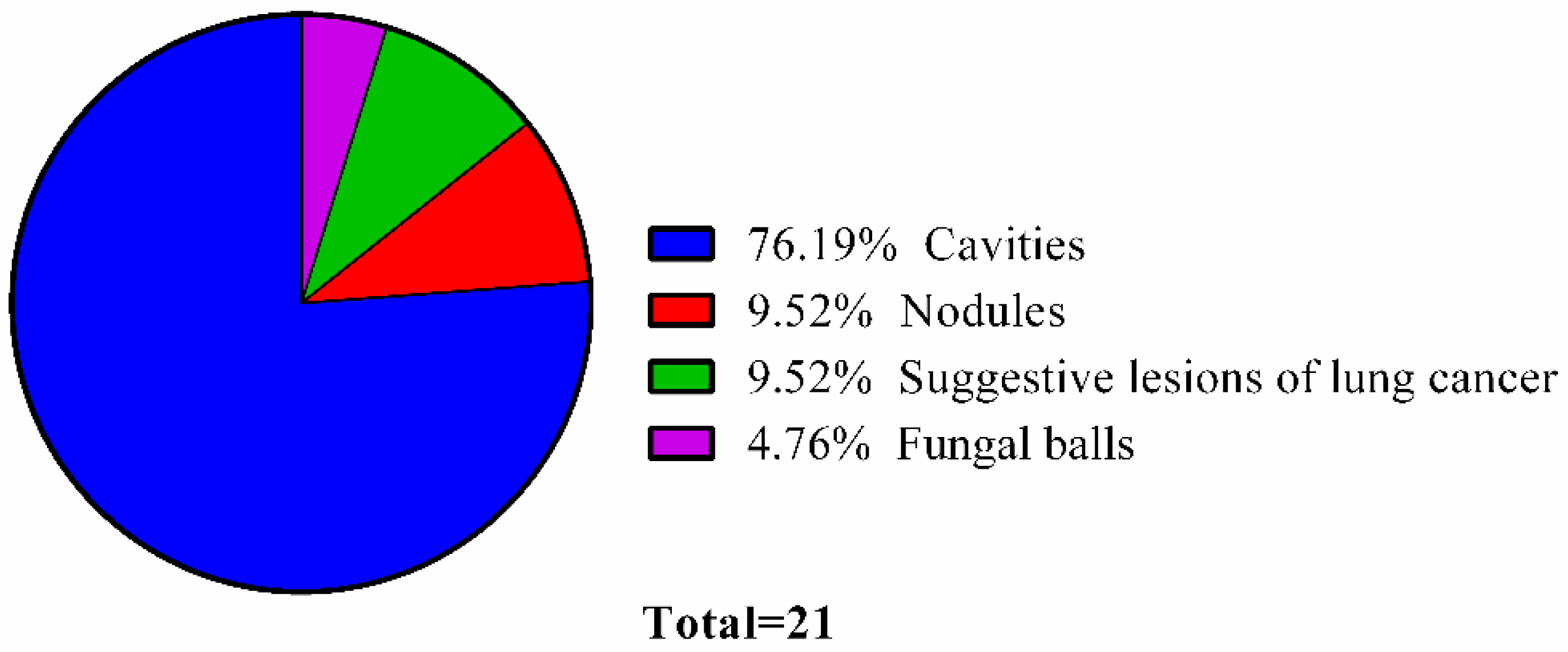
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Denning, D.W. Global Action Fund for Fungal Infections. Available online: www.gaffi.org (accessed on 19 January 2016).
- Webster, J.; Weber, R. Introduction to Fungi, 3rd ed.; Press, C.U., Ed.; Cambridge University Press: Cambridge, UK, 2007; pp. 297–314. [Google Scholar]
- Hayes, G.E.; Novak-Frazer, L. Chronic Pulmonary Aspergillosis—Where Are We? and Where Are We Going? J. Fungi 2016, 2, 18. [Google Scholar] [CrossRef]
- Gorbea, M.B.; Varona, P.; La Rosa, M.C.; Rocha, R.G.G.; Medina, R.S.; Montes de Oca, N.A.; León, A.A.; Sánchez, M.E.D.; Acosta, S.J.; Fernández, S.V.; et al. III Encuesta Nacional de Factores de Riesgo y Actividades Preventivas de Enfermedades no Trasmisibles. Cuba 2010–2011; Editorial Ciencias Médicas: La Habana, Cuba, 2014; p. 289. [Google Scholar]
- Bess-Constantén, S.; Alonso-Alomá, I.; Sánchez-Sordo, E.; López-Nistal, L.M.; Torres-Vidal, R.M.; Martínez-Morales, M.A.; Ledesma-Batista, M.; Podadera-Valdés, X.; Paredes-Esponda, E.; Pérez-Leyva, M.E.; et al. Anuario Estadístico de Salud; Ministerio de Salud Pública: La Habana, Cuba, 2018; p. 191. [Google Scholar]
- Denning, D.W.; Cadranel, J.; Beigelman-Aubry, C.; Ader, F.; Chakrabarti, A.; Blot, S.; Ullman, A.J.; Dimopoulos, G.; Lange, C.; European Society for Clinical Microbiology and Infectious Diseases and European Respiratory Society. Chronic pulmonary aspergillosis: Rationale and clinical guidelines for diagnosis and management. Eur. Respir. J. 2016, 47, 45–68. [Google Scholar] [CrossRef] [PubMed]
- Samson, R.A.; Visagie, C.M.; Houbraken, J.; Hong, S.B.; Hubka, V.; Klaassen, C.H.W.; Perrone, G.; Seifert, K.A.; Susca, A.; Tanney, J.B.; et al. Phylogeny, identification and nomenclature of the genus Aspergillus. Stud. Mycol. 2014, 78, 141–173. [Google Scholar] [CrossRef] [PubMed]
- De Hoog, G.S.; Guarro, J.; Gené, J.; Figueras, M.J. Atlas of Clinical Fungi; CBS: Utrecht, The Netherlands, 2011. [Google Scholar]
- Muldoon, E.G.; Sharman, A.; Page, L.; Bishop, P.; Denning, D.W. Aspergillus nodules, another presentation of chronic pulmonary aspergillosis. BMC Pulm. Med. 2016, 16, 123. [Google Scholar] [CrossRef] [PubMed]
- Hedayati, M.T.; Azimi, Y.; Droudinia, A.; Mousavi, B.; Khalilian, A.; Hedayati, N.; Denning, D.W. Prevalence of chronic pulmonary aspergillosis in patients with tuberculosis from Iran. Eur. J. Clin. Microbiol. Infect. Dis. 2015, 34, 1759–1765. [Google Scholar] [CrossRef] [PubMed]
- Chawla, K.; Kosaraju, K.; Rayasam, S.; Mukhopadhyay, C. Clinico-microbiological profile of chronic pulmonary aspergillosis from a tertiary care centre in southern India. J. Clin. Diagn. Res. 2013, 7, 2712–2715. [Google Scholar] [CrossRef] [PubMed]
- Denning, D.W.; Riniotis, K.; Dobrashian, R.; Sambatakou, H. Chronic cavitary and fibrosing pulmonary and pleural aspergillosis: Case series, proposed nomenclature change, and review. Clin. Infect. Dis. 2003, 37, 265–280. [Google Scholar] [CrossRef] [PubMed]
- Sharma, G.; Goodwin, J. Effect of aging on respiratory system physiology and immunology. Clin. Interv. Aging 2006, 1, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Everaerts, S.; Lagrou, K.; Vermeersch, K.; Dupont, L.J.; Vanaudenaerde, B.M.; Janssens, W. Aspergillus fumigatus detection and risk factors in patients with COPD-bronchiectasis overlap. Int. J. Mol. Sci. 2018, 19, 523. [Google Scholar] [CrossRef] [PubMed]
- Tong, X.; Cheng, A.; Xu, H.; Jin, J.; Yang, Y.; Zhu, S.; Li, Y. Aspergillus fumigatus during COPD exacerbation: A pair-matched retrospective study. BMC Pulm. Med. 2018, 18, 55. [Google Scholar] [CrossRef] [PubMed]
- Bafadhel, M.; Mckenna, S.; Agbetile, J.; Fairs, A.; Dhananjay, D.; Mistry, V.; Morley, J.P.; Pancholi, M.; Pavord, I.D.; Wardlaw, A.J.; et al. Aspergillus fumigatus during stable state and exacerbations of chronic obstructive pulmonary disease. Eur. Respir. J. 2013. [Google Scholar] [CrossRef]
- Shahi, M.; Ayatollahi-Mousavi, S.A.; Nabili, M.; Aliyali, M.; Khodavaisy, S.; Badali, H. Aspergillus colonization in patients with chronic obstructive pulmonary disease. Curr. Med. Mycol. 2015, 1, 45–51. [Google Scholar] [CrossRef] [PubMed]
- TBFACTS.ORG. Available online: https://www.tbfacts.org/tb-statistics/ (accessed on 14 January 2019).
- Denning, D.W.; Page, I.D.; Chakaya, J.; Jabeen, K.; Jude, C.M.; Cornet, M.; Alastruey-Izquierdo, A.; Bongomin, F.; Bowyer, P.; Chakrabarti, A.; et al. Case Definition of Chronic Pulmonary Aspergillosis in Resource-Constrained Settings. Emerg. Infect. Dis. 2018, 24. [Google Scholar] [CrossRef] [PubMed]
- Maghrabi, F.; Denning, D.W. The management of chronic pulmonary aspergillosis: The UK National Centre approach. Curr. Fungal Infect. Rep. 2017, 11, 242–251. [Google Scholar] [CrossRef] [PubMed]
- Panse, P.; Smith, M.; Cummings, K.; Jensen, E.; Gotway, M.; Jokerst, C. The many faces of pulmonary aspergillosis: Imaging findings with pathologic correlation. Radiol. Infect. Dis. 2016, 3, 192–200. [Google Scholar] [CrossRef]
- Sah, S.K.; Li, Y.; Ganganah, O.; Shi, X.; Li, Y. An update of clinical characteristics and imaging findings of pulmonary aspegillosis. Int. J. Diagn. Imaging 2016, 3, 8–18. [Google Scholar] [CrossRef]
- Prasad, A.; Agarwal, K.; Deepak, D.; Atwal, S.S. Pulmonary aspergillosis: What CT can offer before it is too late! J. Clin. Diagn. Res. 2016, 10, TE01–TE05. [Google Scholar] [CrossRef] [PubMed]
- Richardson, M.D.; Page, I.D. Aspergillus serology: Have we arrived yet? Med. Mycol. 2017, 55, 48–55. [Google Scholar] [CrossRef]
- Page, I.D.; Richardson, M.D.; Denning, D.W. Comparison of six Aspergillus—Specific IgG assays for the diagnosis of chronic pulmonary aspergillosis (CPA). J. Infect. 2016, 72, 240–249. [Google Scholar] [CrossRef]
- Bowyer, P.; Blightman, O.; Denning, D.W. Relative reactivity of Aspergillus allergens used in serological tests. Med. Mycol. 2006, 44, S23–S28. [Google Scholar] [CrossRef]
- Gbaja-Biamila, T.; Bongomin, F.; Irurhe, N.; Nwosu, A.O.; Oladele, R.O. Chronic pulmonary aspergillosis misdiagnosed as smear-negative pulmonary tuberculosis in a TB clinic in Nigeria. JAMMR 2018, 21, 1056–1061. [Google Scholar] [CrossRef]
- Denning, D.W.; Pleuvry, A.; Cole, D.C. Global burden of chronic pulmoanry aspergillosis as a sequel to pulmonary tuberculosis. Bull. World Health Org. 2011, 89, 864–872. [Google Scholar] [CrossRef] [PubMed]
- Patterson, T.F.; Thompson, G.R., III; Denning, D.W.; Fishman, J.A.; Hadley, S.; Herbercht, R.; Kontoyiannis, D.P.; Marr, K.A.; Morrison, V.A.; Nguyen, M.H.; et al. Practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2016, 63, 1–60. [Google Scholar] [CrossRef] [PubMed]
- Underhill, D.M.; Iliev, I.D. The mycobiota: Interactions between commensal fungi and the host immune system. Nat. Rev. 2014, 14, 405–416. [Google Scholar] [CrossRef] [PubMed]
- Pashley, C.H.; Fairs, A.; Morley, J.P.; Tailor, S.; Agbetile, J.; Bafadhel, M.; Brightling, C.E.; Wardlaw, A.J. Routine processing procedures for isolating filamentous fungi from respiratory sputum samples may underestimate fungal prevalence. Med. Mycol. 2012, 50, 433–438. [Google Scholar] [CrossRef] [PubMed]
- Hedayati, M.T.; Pasqualotto, A.C.; Warn, P.A.; Bowyer, P.; Denning, D.W. Aspergillus flavus: Human pathogen, allergen and mycotoxin producer. Microbiology 2007, 153, 1677–1692. [Google Scholar] [CrossRef] [PubMed]
- Park, S.J.; Chung, C.R.; Rhee, Y.K.; Lee, H.B.; Lee, Y.C.; Kweon, E.Y. Chronic pulmonary aspergillosis due to Aspergillus niger. Am. J. Respir. Crit. Care Med. 2012, 186, 16–17. [Google Scholar] [CrossRef]
- Aira, M.J.; Rojas, T.I.; Jato, V. Fungi associated with three houses in Havana (Cuba). Grana 2002, 41, 114–118. [Google Scholar] [CrossRef]
- Almaguer, M.; Rojas-Flores, T.I. Aeromicota viable de la atmósfera de La Habana, Cuba. NACC 2013, 20, 35–45. [Google Scholar]
- Rojas, T.I.; LLanes, N.; Benitez, M.; Aira, M.J.; Malagón, H. El género Aspergillus en la atmósfera de la Habana (Cuba). Bol. Micol. 2007, 22, 41–46. [Google Scholar] [CrossRef]
- Pasqualotto, A.C. Aspergillosis: From Diagnosis to Prevention, 1st ed.; Pasqualotto, A.C., Ed.; Springer: London, UK, 2010; pp. 9–15. [Google Scholar] [CrossRef]
| Co-Morbidities | No. of Patients (%) |
|---|---|
| COPD | 4 (19.05) |
| Lung cancer | 4 (19.05) |
| Idiopathic bronchiectasis | 5 (23.81) |
| Pleural abscess | 1 (4.76) |
| PTB | 1 (4.76) |
| Without diagnostic conclusion | 6 (28.57) |
| Clinical Signs and Symptoms | No. of Patients (%) |
|---|---|
| Productive cough | 21 (100) |
| Dyspnea | 9 (42.86) |
| Hemoptysis | 5 (23.81) |
| Chest discomfort | 5 (23.81) |
| Weight loss | 5 (23.81) |
| Tiredness | 3 (14.29) |
| Anorexia | 2 (9.52) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beltrán Rodríguez, N.; San Juan-Galán, J.L.; Fernández Andreu, C.M.; María Yera, D.; Barrios Pita, M.; Perurena Lancha, M.R.; Velar Martínez, R.E.; Illnait Zaragozí, M.T.; Martínez Machín, G.F. Chronic Pulmonary Aspergillosis in Patients with Underlying Respiratory Disorders in Cuba—A Pilot Study. J. Fungi 2019, 5, 18. https://doi.org/10.3390/jof5010018
Beltrán Rodríguez N, San Juan-Galán JL, Fernández Andreu CM, María Yera D, Barrios Pita M, Perurena Lancha MR, Velar Martínez RE, Illnait Zaragozí MT, Martínez Machín GF. Chronic Pulmonary Aspergillosis in Patients with Underlying Respiratory Disorders in Cuba—A Pilot Study. Journal of Fungi. 2019; 5(1):18. https://doi.org/10.3390/jof5010018
Chicago/Turabian StyleBeltrán Rodríguez, Nathalie, Javier Luis San Juan-Galán, Carlos Manuel Fernández Andreu, Dulce María Yera, Miriam Barrios Pita, Mayda Rosa Perurena Lancha, Rosario Esperanza Velar Martínez, María Teresa Illnait Zaragozí, and Gerardo Félix Martínez Machín. 2019. "Chronic Pulmonary Aspergillosis in Patients with Underlying Respiratory Disorders in Cuba—A Pilot Study" Journal of Fungi 5, no. 1: 18. https://doi.org/10.3390/jof5010018
APA StyleBeltrán Rodríguez, N., San Juan-Galán, J. L., Fernández Andreu, C. M., María Yera, D., Barrios Pita, M., Perurena Lancha, M. R., Velar Martínez, R. E., Illnait Zaragozí, M. T., & Martínez Machín, G. F. (2019). Chronic Pulmonary Aspergillosis in Patients with Underlying Respiratory Disorders in Cuba—A Pilot Study. Journal of Fungi, 5(1), 18. https://doi.org/10.3390/jof5010018





