Biofilm Formation and Resistance to Fungicides in Clinically Relevant Members of the Fungal Genus Fusarium
Abstract
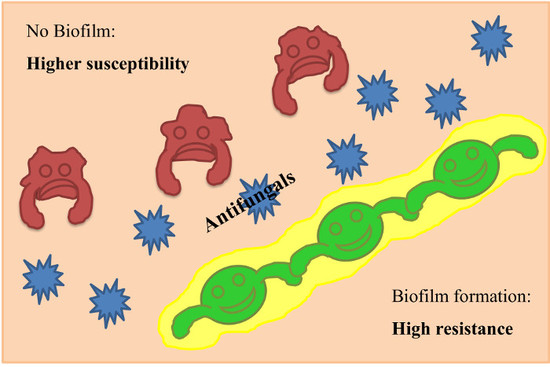
:1. Introduction
2. Materials and Methods
2.1. Fungal Strains
2.2. Antifungal Susceptibility Testing of Planktonic Cells
2.3. In Vitro Biofilm Formation Assay
2.4. Antifungals Susceptibility of Pre-Formed Biofilms
2.5. Data Analysis
3. Results
3.1. Antifungal Susceptibility Profile of Planktonic Cells
3.2. Biofilm Formation
3.3. Sessile Susceptibilities of Fusarium Strains
4. Discussion
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Van Diepeningen, A.D.; de Hoog, G.S. Challenges in Fusarium, a Trans-Kingdom Pathogen. Mycopathologia 2016, 181, 161–163. [Google Scholar] [CrossRef] [PubMed]
- Kebabci, N.; van Diepeningen, A.D.; Ener, B.; Ersal, T.; Meijer, M.; Al-Hatmi, A.M.S.; Ozkocaman, V.; Ursavas, A.; Cetinoglu, E.D.; Akalin, H. Fatal breakthrough infection with Fusarium andiyazi: New multi-resistant aetiological agent cross-reacting with Aspergillus galactomannan enzyme immunoassay. Mycoses 2014, 57, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Al-Hatmi, A.M.; Meis, J.F.; de Hoog, G.S. Fusarium: Molecular Diversity and Intrinsic Drug Resistance. PLoS Pathog. 2016, 12, e1005464. [Google Scholar] [CrossRef] [PubMed]
- Van Diepeningen, A.D.; Feng, P.; Ahmed, S.; Sudhadham, M.; Bunyaratavej, S.; de Hoog, G.S. Spectrum of Fusarium infections in tropical dermatology evidenced by multilocus sequencing typing diagnostics. Mycoses 2015, 58, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Guarro, J. Fusariosis, a complex infection caused by a high diversity of fungal species refractory to treatment. Eur. J. Clin. Microbiol. Infect. Dis. 2013, 32, 1491–1500. [Google Scholar] [CrossRef] [PubMed]
- Dalyan Cilo, B.; Al-Hatmi, A.M.; Seyedmousavi, S.; Rijs, A.J.; Verweij, P.E.; Ener, B.; de Hoog, G.S.; van Diepeningen, A.D. Emergence of fusarioses in a university hospital in Turkey during a 20-year period. Eur. J. Clin. Microbiol. Infect. Dis. 2015, 34, 1683–1691. [Google Scholar] [CrossRef] [PubMed]
- Migheli, Q.; Balmas, V.; Harak, H.; Sanna, S.; Scherm, B.; Aoki, T.; O’Donnell, K. Molecular phylogenetic diversity of dermatologic and other human pathogenic fusarial isolates from hospitals in northern and central Italy. J. Clin. Microbiol. 2010, 48, 1076–1084. [Google Scholar] [CrossRef] [PubMed]
- Taj-Aldeen, S.J.; Salah, H.; Al-Hatmi, A.M.; Hamed, M.; Theelen, B.; van Diepeningen, A.D.; Boekhout, T.; Lass-Florl, C. In vitro resistance of clinical Fusarium species to amphotericin B and voriconazole using the EUCAST antifungal susceptibility method. Diagn. Microbiol. Infect. Dis. 2016, 85, 438–443. [Google Scholar] [CrossRef] [PubMed]
- Al-Hatmi, A.M.; Meletiadis, J.; Curfs-Breuker, I.; Bonifaz, A.; Meis, J.F.; De Hoog, G.S. In vitro combinations of natamycin with voriconazole, itraconazole and micafungin against clinical Fusarium strains causing keratitis. J. Antimicrob. Chemother. 2016, 71, 953–955. [Google Scholar] [CrossRef] [PubMed]
- Guevara-Suarez, M.; Cano-Lira, J.F.; de Garcia, M.C.; Sopo, L.; De Bedout, C.; Cano, L.E.; Garcia, A.M.; Motta, A.; Amezquita, A.; Cardenas, M.; et al. Genotyping of Fusarium Isolates from Onychomycoses in Colombia: Detection of Two New Species Within the Fusarium solani Species Complex and In Vitro Antifungal Susceptibility Testing. Mycopathologia 2016, 181, 165–174. [Google Scholar] [CrossRef] [PubMed]
- Cuenca-Estrella, M.; Gomez-Lopez, A.; Mellado, E.; Buitrago, M.J.; Monzon, A.; Rodriguez-Tudela, J.L. Head-to-head comparison of the activities of currently available antifungal agents against 3,378 Spanish clinical isolates of yeasts and filamentous fungi. Antimicrob. Agents Chem. 2006, 50, 917–921. [Google Scholar] [CrossRef] [PubMed]
- Xie, L.; Zhai, H.; Zhao, J.; Sun, S.; Shi, W.; Dong, X. Antifungal susceptibility for common pathogens of fungal keratitis in Shandong Province, China. Am. J. Ophthalmol. 2008, 146, 260–265. [Google Scholar] [CrossRef] [PubMed]
- Gupta, C.; Jongman, M.; Das, S.; Snehaa, K.; Bhattacharya, S.N.; Seyedmousavi, S.; van Diepeningen, A.D. Genotyping and In Vitro Antifungal Susceptibility Testing of Fusarium Isolates from Onychomycosis in India. Mycopathologia 2016, 181, 497–504. [Google Scholar] [CrossRef] [PubMed]
- Ramage, G.; Saville, S.P.; Thomas, D.P.; Lopez-Ribot, J.L. Candida biofilms: An update. Eukaryot. Cell 2005, 4, 633–638. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, P.K.; Chandra, J.; Kuhn, D.A.; Ghannoum, M.A. Mechanism of fluconazole resistance in Candida albicans biofilms: Phase-specific role of efflux pumps and membrane sterols. Infect. Immun. 2003, 71, 4333–4340. [Google Scholar] [CrossRef] [PubMed]
- Seidler, M.J.; Salvenmoser, S.; Muller, F.M. Aspergillus fumigatus forms biofilms with reduced antifungal drug susceptibility on bronchial epithelial cells. Antimicrob. Agents Chemother. 2008, 52, 4130–4136. [Google Scholar] [CrossRef] [PubMed]
- Erdem, E.; Yagmur, M.; Boral, H.; Ilkit, M.; Ersoz, R.; Seyedmousavi, S. Aspergillus flavus Keratitis: Experience of a Tertiary Eye Clinic in Turkey. Mycopathologia 2017, 182, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Chandra, J.; Kuhn, D.M.; Mukherjee, P.K.; Hoyer, L.L.; McCormick, T.; Ghannoum, M.A. Biofilm formation by the fungal pathogen Candida albicans: Development, architecture, and drug resistance. J. Bacteriol. 2001, 183, 5385–5394. [Google Scholar] [CrossRef] [PubMed]
- Kaur, S.; Singh, S. Biofilm formation by Aspergillus fumigatus. Med. Mycol. 2014, 52, 2–9. [Google Scholar] [PubMed]
- Zhang, X.; Sun, X.; Wang, Z.; Zhang, Y.; Hou, W. Keratitis-associated fungi form biofilms with reduced antifungal drug susceptibility. Investig. Ophthalmol. Vis. Sci. 2012, 53, 7774–7778. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, P.K.; Chandra, J.; Yu, C.; Sun, Y.; Pearlman, E.; Ghannoum, M.A. Characterization of Fusarium keratitis outbreak isolates: Contribution of biofilms to antimicrobial resistance and pathogenesis. Investig. Ophthalmol. Vis. Sci. 2012, 53, 4450–4457. [Google Scholar] [CrossRef] [PubMed]
- Imamura, Y.; Chandra, J.; Mukherjee, P.K.; Lattif, A.A.; Szczotka-Flynn, L.B.; Pearlman, E.; Lass, J.H.; O’Donnell, K.; Ghannoum, M.A. Fusarium and Candida albicans biofilms on soft contact lenses: Model development, influence of lens type, and susceptibility to lens care solutions. Antimicrob. Agents Chemother. 2008, 52, 171–182. [Google Scholar] [CrossRef] [PubMed]
- Sav, H.; Ozdemir, H.G.; Altinbas, R.; Kiraz, N.; Ilkit, M.; Seyedmousavi, S. Virulence Attributes and Antifungal Susceptibility Profile of Opportunistic Fungi Isolated from Ophthalmic Infections. Mycopathologia 2016, 181, 653–661. [Google Scholar] [CrossRef] [PubMed]
- Chang, D.C.; Grant, G.B.; O’Donnell, K.; Wannemuehler, K.A.; Noble-Wang, J.; Rao, C.Y.; Jacobson, L.M.; Crowell, C.S.; Sneed, R.S.; Lewis, F.M.T.; et al. Multistate outbreak of Fusarium keratitis associated with use of a contact lens solution. JAMA 2006, 296, 953–963. [Google Scholar] [CrossRef] [PubMed]
- Clinical and Laboratory Standards Institute (CLSI). Reference Method for Broth Dilution Antifungal SusceptibilityTesting of Filamentous Fungi; Approved standard-Second Edition.CLSI Document. M38-A2; CLSI: Wane, PA, USA, 2008; Volume 28, No. 16. [Google Scholar]
- Toledo-Arana, A.; Valle, J.; Solano, C.; Arrizubieta, M.J.; Cucarella, C.; Lamata, M.; Amorena, B.; Leiva, J.; Penades, J.R.; Lasa, I. The enterococcal surface protein, Esp, is involved in Enterococcus faecalis biofilm formation. Appl. Environ. Microb. 2001, 67, 4538–4545. [Google Scholar] [CrossRef]
- Kim, D.J.; Lee, M.W.; Choi, J.S.; Lee, S.G.; Park, J.Y.; Kim, S.W. Inhibitory activity of hinokitiol against biofilm formation in fluconazole-resistant Candida species. PLoS ONE 2017, 12, e0171244. [Google Scholar] [CrossRef] [PubMed]
- Seyedmousavi, S.; Meletiadis, J.; Melchers, W.J.; Rijs, A.J.; Mouton, J.W.; Verweij, P.E. In vitro interaction of voriconazole and anidulafungin against triazole-resistant Aspergillus fumigatus. Antimicrob. Agents Chemother. 2013, 57, 796–803. [Google Scholar] [CrossRef] [PubMed]
- Seneviratne, C.J.; Jin, L.J.; Samaranayake, Y.H.; Samaranayake, L.P. Cell density and cell aging as factors modulating antifungal resistance of Candida albicans biofilms. Antimicrob. Agents Chemother. 2008, 52, 3259–3266. [Google Scholar] [CrossRef] [PubMed]
- Rollin-Pinheiro, R.; de Meirelles, J.V.; Vila, T.V.M.; Fonseca, B.B.; Alves, V.; Frases, S.; Rozental, S.; Barreto-Bergter, E. Biofilm Formation by Pseudallescheria/Scedosporium Species: A Comparative Study. Front. Microbiol. 2017, 8, 1568. [Google Scholar] [CrossRef] [PubMed]
- Vila, T.V.; Ishida, K.; de Souza, W.; Prousis, K.; Calogeropoulou, T.; Rozental, S. Effect of alkylphospholipids on Candida albicans biofilm formation and maturation. J. Antimicrob. Chemother. 2013, 68, 113–125. [Google Scholar] [CrossRef] [PubMed]
- Blankenship, J.R.; Mitchell, A.P. How to build a biofilm: A fungal perspective. Curr. Opin. Microbiol. 2006, 9, 588–594. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, K.; Sutton, D.A.; Rinaldi, M.G.; Magnon, K.C.; Cox, P.A.; Revankar, S.G.; Sanche, S.; Geiser, D.M.; Juba, J.H.; van Burik, J.A.; et al. Genetic diversity of human pathogenic members of the Fusarium oxysporum complex inferred from multilocus DNA sequence data and amplified fragment length polymorphism analyses: Evidence for the recent dispersion of a geographically widespread clonal lineage and nosocomial origin. J. Clin. Microbiol. 2004, 42, 5109–5120. [Google Scholar] [PubMed]
- Short, D.P.; O’Donnell, K.; Zhang, N.; Juba, J.H.; Geiser, D.M. Widespread occurrence of diverse human pathogenic types of the fungus Fusarium detected in plumbing drains. J. Clin. Microbiol. 2011, 49, 4264–4272. [Google Scholar] [CrossRef] [PubMed]
- Becher, R.; Weihmann, F.; Deising, H.B.; Wirsel, S.G. Development of a novel multiplex DNA microarray for Fusarium graminearum and analysis of azole fungicide responses. BMC Genom. 2011, 12, 52. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Wang, K.; Yu, X.; Liu, J.; Zhang, H.; Zhou, F.; Xie, B.; Li, S. Transcription factor CCG-8 as a new regulator in the adaptation to antifungal azole stress. Antimicrob. Agents Chemother. 2014, 58, 1434–1442. [Google Scholar] [CrossRef] [PubMed]
- Abou Ammar, G.; Tryono, R.; Doll, K.; Karlovsky, P.; Deising, H.B.; Wirsel, S.G. Identification of ABC transporter genes of Fusarium graminearum with roles in azole tolerance and/or virulence. PLoS ONE 2013, 8, e79042. [Google Scholar] [CrossRef] [PubMed]
- Fan, J.; Urban, M.; Parker, J.E.; Brewer, H.C.; Kelly, S.L.; Hammond-Kosack, K.E.; Fraaije, B.A.; Liu, X.; Cools, H.J. Characterization of the sterol 14alpha-demethylases of Fusarium graminearum identifies a novel genus-specific CYP51 function. New Phytol. 2013, 198, 821–835. [Google Scholar] [CrossRef] [PubMed]
- Ramage, G.; Rajendran, R.; Sherry, L.; Williams, C. Fungal biofilm resistance. Int. J. Microbiol. 2012, 2012, 528521. [Google Scholar] [CrossRef] [PubMed]
- Baillie, G.S.; Douglas, L.J. Matrix polymers of Candida biofilms and their possible role in biofilm resistance to antifungal agents. J. Antimicrob. Chemother. 2000, 46, 397–403. [Google Scholar] [CrossRef] [PubMed]
- LaFleur, M.D.; Kumamoto, C.A.; Lewis, K. Candida albicans biofilms produce antifungal-tolerant persister cells. Antimicrob. Agents Chemother. 2006, 50, 3839–3846. [Google Scholar] [CrossRef] [PubMed]
- Rajendran, R.; Williams, C.; Lappin, D.F.; Millington, O.; Martins, M.; Ramage, G. Extracellular DNA release acts as an antifungal resistance mechanism in mature Aspergillus fumigatus biofilms. Eukaryot. Cell 2013, 12, 420–429. [Google Scholar] [CrossRef] [PubMed]
| No | CBS No | Species | Source | Country | Underlying Disease | AMB | 5-FC | FLC | ITR | VRC | POS | AND | CAS | Biofilm Formation | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Planktonic MIC/MEC (μg/mL) | |||||||||||||||
| 1 | Fusarium dimerum species complex | 139002 | F. dimerum | Skin biopsy | Turkey | Paraplegia | 0.5 | >64 | >64 | >64 | 4 | >16 | >16 | >16 | − |
| 2 | Fusarium fujikuroi species complex | 139195 | F. andiyazi | Blood | Turkey | Acute myeloid leukemia | 8 | >64 | 16 | 8 | 2 | 1 | >16 | 8 | − |
| 3 | 138998 | F. proliferatum | Blood | Turkey | Acute lymphoblastic leukemia | 0.5 | >64 | >64 | >64 | 4 | >16 | >16 | >16 | − | |
| 4 | 138924 | F. proliferatum | Nasal biopsy | Turkey | Acute myeloid leukemia | 0.125 | >64 | >64 | >64 | 4 | >16 | >16 | >16 | − | |
| 5 | 138925 | F. proliferatum | Skin biopsy | Turkey | Chronic renal failure | 0.125 | >64 | >64 | >64 | 4 | >16 | >16 | >16 | − | |
| 6 | 139000 | F. proliferatum | BAL | Turkey | Aplastic anemia | 0.25 | >64 | >64 | >64 | 1 | 0.125 | >16 | >16 | − | |
| 7 | 139001 | F. proliferatum | Skin biopsy | Turkey | Acute lymphoblastic leukemia | 1 | >64 | >64 | >64 | 4 | 1 | >16 | >16 | − | |
| 8 | 139003 | F. proliferatum | Blood | Turkey | Acute lymphoblastic leukemia | 1 | >64 | >64 | >64 | 4 | >16 | >16 | >16 | − | |
| 9 | 139004 | F. proliferatum | Sputum | Turkey | Lung cancer | 0.5 | >64 | >64 | >64 | 4 | >16 | >16 | >16 | − | |
| 10 | 138929 | F. proliferatum | Cornea scraping | Turkey | Keratitis | 1 | >64 | >64 | >64 | 4 | >16 | >16 | >16 | − | |
| 11 | 138930 | F. proliferatum | Nasal biopsy | Turkey | Aplastic anemia | 1 | >64 | >64 | >64 | 4 | 1 | >16 | >16 | − | |
| 12 | 138928 | F. proliferatum | Blood | Turkey | Malign melanoma | 1 | >64 | >64 | >64 | 2 | 0.5 | >16 | >16 | − | |
| 13 | 139198 | F. proliferatum | Nasal biopsy | Turkey | Acute myeloid leukemia | 1 | >64 | >64 | >64 | 8 | >16 | >16 | >16 | − | |
| 14 | 138933 | F. proliferatum | Nasal biopsy | Turkey | Acute lymphoblastic leukemia | 1 | >64 | >64 | >64 | 4 | 0.5 | >16 | >16 | − | |
| 15 | 138930 | F. proliferatum | Nasal biopsy | Turkey | Aplastic anemia | 1 | >64 | >64 | >64 | 4 | 1 | >16 | >16 | − | |
| 16 | 480.77 | F. proliferatum | Banana, bud rot | the Netherlands | - | 1 | >64 | >64 | >16 | 2 | 1 | >16 | >16 | − | |
| 17 | 133030 | F. proliferatum | Nail scraping | Iran | Onychomycosis | 0.5 | >64 | >64 | >16 | 8 | >16 | >16 | >16 | − | |
| 18 | 131391 | F. proliferatum | Wheat root | Australia | - | 0.5 | >64 | >64 | >16 | 8 | >16 | >16 | >16 | − | |
| 19 | 130179 | F. proliferatum | Blood | USA | - | 1 | >64 | >64 | >64 | 4 | 2 | >16 | >16 | − | |
| 20 | 139015 | F. verticillioides | Blood | Turkey | Acute myeloid leukemia | 2 | >64 | >64 | >64 | 1 | 0.25 | >16 | >16 | − | |
| 21 | 139018 | F. verticillioides | Blood | Turkey | T-cell lymphoma | 4 | >64 | >64 | >64 | 1 | 0.125 | >16 | >16 | − | |
| 22 | 139202 | F. verticillioides | Blood | Turkey | Acute lymphoblastic leukemia | 4 | >64 | >64 | >64 | 1 | 0.25 | >16 | >16 | − | |
| 23 | 579.78 | F. verticillioides | Leg ulcer | USA | Left leg ulcer | 2 | >64 | >64 | 16 | 1 | 0.25 | >16 | >16 | − | |
| 24 | 123670 | F. verticillioides | Maize | USA | - | 2 | >64 | 64 | 16 | 2 | 1 | >16 | >16 | − | |
| 25 | 115135 | F. verticillioides | Blood | Sweden | - | 2 | >64 | >64 | >16 | 2 | 0.5 | >16 | >16 | − | |
| 26 | 108922 | F. verticillioides | Urine | Germany | - | 2 | >64 | >64 | >16 | 1 | 0.25 | >16 | >16 | − | |
| 27 | Fusarium oxysporum species complex | 138926 | F. oxysporum | Sputum | Turkey | Hepatic cirrhosis | 0.5 | >64 | >64 | >64 | 2 | >16 | >16 | >16 | − |
| 28 | Fusarium solani species complex | 139005 | F. keratoplasticum | Nail scraping | Turkey | Onychomycosis | 2 | >64 | >64 | >64 | 8 | 0.125 | >16 | >16 | + |
| 29 | 139017 | F. keratoplasticum | Nail scraping | Turkey | Onychomycosis | 2 | >64 | >64 | >64 | 8 | >16 | >16 | >16 | + | |
| 30 | 139006 | F. petroliphilum | Blood | Turkey | Acute myeloid leukemia | 0.25 | >64 | >64 | >64 | 16 | >16 | >16 | >16 | + | |
| 31 | 138932 | F. petroliphilum | Nasal biopsy | Turkey | Myelodysplastic syndrome | 0.5 | >64 | >64 | >64 | 8 | >16 | >16 | >16 | + | |
| 32 | 139011 | F. petroliphilum | Blood | Turkey | Acute lymphoblastic leukemia | 1 | >64 | >64 | >64 | 8 | >16 | >16 | >16 | + | |
| 33 | 139324 | F. petroliphilum | Blood | Turkey | Acute lymphoblastic leukemia | 0.5 | >64 | >64 | >64 | 8 | >16 | >16 | >16 | + | |
| 34 | 139013 | F. petroliphilum | Blood | Turkey | Acute lymphoblastic leukemia | 1 | >64 | >64 | >64 | 8 | >16 | >16 | >16 | + | |
| 35 | 139016 | F. petroliphilum | Nail scraping | Turkey | Onychomycosis | 1 | >64 | >64 | >64 | 8 | >16 | >16 | >16 | − | |
| 36 | 139205 | F. solani | Sputum | Turkey | Larynx cancer | 1 | >64 | >64 | >64 | 4 | >16 | >16 | >16 | − | |
| 37 | 139007 | F. solani | Skin scraping | Turkey | Diabetes | 1 | >64 | >64 | >64 | 8 | >16 | >16 | >16 | − | |
| 38 | 139008 | F. solani | Nasal biopsy | Turkey | Acute myeloid leukemia | 1 | >64 | >64 | >64 | 2 | >16 | >16 | >16 | − | |
| 39 | 139012 | F. solani | Cornea scraping | Turkey | Keratitis | 0.25 | >64 | >64 | >64 | 2 | >16 | >16 | >16 | − | |
| 40 | 139200 | F. solani | Cornea scraping | Turkey | Keratitis | 1 | >64 | >64 | >64 | 8 | >16 | >16 | >16 | − | |
| 41 | 139197 | F. solani | Skin biopsy | Turkey | Acute myeloid leukemia | 2 | >64 | >64 | >64 | 2 | >16 | >16 | >16 | − | |
| CBS No | Species | Biofilm Formation | AMB | ITC | VRC | POS | AND | CAS | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PMIC | SMIC | PMIC | SMIC | PMIC | SMIC | PMIC | SMIC | PMIC | SMIC | PMIC | SMIC | |||
| (μg/mL) | ||||||||||||||
| 139005 | F. keratoplasticum | + | 2 | 2 | >16 | >16 | 8 | >16 | 0.125 | 0.5 | >16 | >16 | >16 | >16 |
| 139017 | F. keratoplasticum | + | 2 | 8 | >16 | >16 | 8 | >16 | >16 | >16 | >16 | >16 | >16 | >16 |
| 139006 | F. petroliphilum | + | 0.25 | 2 | >16 | >16 | 16 | >16 | >16 | >16 | >16 | >16 | >16 | >16 |
| 138932 | F. petroliphilum | + | 0.5 | 4 | >16 | >16 | 8 | >16 | >16 | >16 | >16 | >16 | >16 | >16 |
| 139011 | F. petroliphilum | + | 1 | 2 | >16 | >16 | 8 | >16 | >16 | >16 | >16 | >16 | >16 | >16 |
| 139324 | F. petroliphilum | + | 0.5 | 4 | >16 | >16 | 8 | >16 | >16 | >16 | >16 | >16 | >16 | >16 |
| 139013 | F. petroliphilum | + | 1 | 2 | >16 | >16 | 8 | >16 | >16 | >16 | >16 | >16 | >16 | >16 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sav, H.; Rafati, H.; Öz, Y.; Dalyan-Cilo, B.; Ener, B.; Mohammadi, F.; Ilkit, M.; Van Diepeningen, A.D.; Seyedmousavi, S. Biofilm Formation and Resistance to Fungicides in Clinically Relevant Members of the Fungal Genus Fusarium. J. Fungi 2018, 4, 16. https://doi.org/10.3390/jof4010016
Sav H, Rafati H, Öz Y, Dalyan-Cilo B, Ener B, Mohammadi F, Ilkit M, Van Diepeningen AD, Seyedmousavi S. Biofilm Formation and Resistance to Fungicides in Clinically Relevant Members of the Fungal Genus Fusarium. Journal of Fungi. 2018; 4(1):16. https://doi.org/10.3390/jof4010016
Chicago/Turabian StyleSav, Hafize, Haleh Rafati, Yasemin Öz, Burcu Dalyan-Cilo, Beyza Ener, Faezeh Mohammadi, Macit Ilkit, Anne D. Van Diepeningen, and Seyedmojtaba Seyedmousavi. 2018. "Biofilm Formation and Resistance to Fungicides in Clinically Relevant Members of the Fungal Genus Fusarium" Journal of Fungi 4, no. 1: 16. https://doi.org/10.3390/jof4010016
APA StyleSav, H., Rafati, H., Öz, Y., Dalyan-Cilo, B., Ener, B., Mohammadi, F., Ilkit, M., Van Diepeningen, A. D., & Seyedmousavi, S. (2018). Biofilm Formation and Resistance to Fungicides in Clinically Relevant Members of the Fungal Genus Fusarium. Journal of Fungi, 4(1), 16. https://doi.org/10.3390/jof4010016