Development of a Mouse Model of Coccidioidomycosis Using an Inhalation Exposure System
Abstract
1. Introduction
2. Methods
2.1. Mice
2.2. Fungal Cultures
2.3. Aerosolization of Pathogens
2.4. Intranasal Infection Model
2.5. Fungal Titers
2.6. Statistical Analysis
3. Results
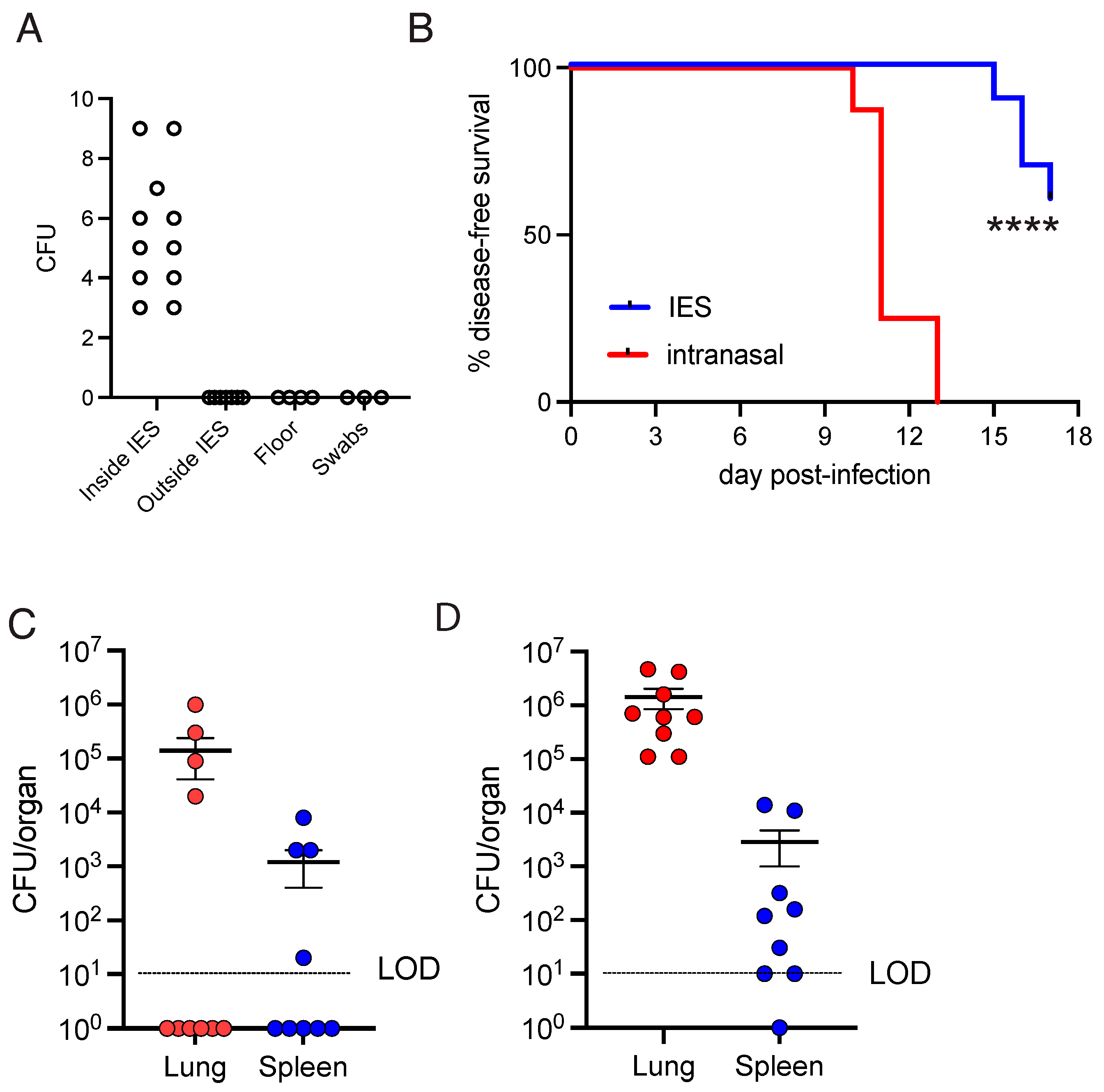
Nebulization of Coccidioides Inconsistently Infected Mice
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Brown, J.; Benedict, K.; Park, B.J.; Thompson, G.R., 3rd. Coccidioidomycosis: Epidemiology. Clin. Epidemiol. 2013, 5, 185–197. [Google Scholar] [PubMed]
- Galgiani, J.N.; Kauffman, C.A. Coccidioidomycosis and Histoplasmosis in Immunocompetent Persons. N. Engl. J. Med. 2024, 390, 536–547. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.Y.; Jerng, J.S.; Ko, J.C.; Lin, M.F.; Hsiao, C.H.; Lee, L.N.; Hsueh, P.-R.; Kuo, S.-H. Disseminated coccidioidomycosis. Emerg. Infect. Dis. 2005, 11, 177–179. [Google Scholar] [CrossRef] [PubMed]
- To, E.E.; Erlich, J.; Liong, F.; Luong, R.; Liong, S.; Bozinovski, S.; Seow, H.J.; O’lEary, J.J.; Brooks, D.A.; Vlahos, R.; et al. Intranasal and epicutaneous administration of Toll-like receptor 7 (TLR7) agonists provides protection against influenza A virus-induced morbidity in mice. Sci. Rep. 2019, 9, 2366. [Google Scholar] [CrossRef] [PubMed]
- Suarez-Alvarez, R.O.; Sahaza, J.H.; Berzunza-Cruz, M.; Becker, I.; Curiel-Quesada, E.; Perez-Torres, A.; Reyes-Montes, M.d.R.; Taylor, M.L. Dimorphism and Dissemination of Histoplasma capsulatum in the Upper Respiratory Tract after Intranasal Infection of Bats and Mice with Mycelial Propagules. Am. J. Trop. Med. Hyg. 2019, 101, 716–723. [Google Scholar] [CrossRef] [PubMed]
- Dileepan, T.; Smith, E.D.; Knowland, D.; Hsu, M.; Platt, M.; Bittner-Eddy, P.; Cohen, B.; Southern, P.; Latimer, E.; Harley, E.; et al. Group A Streptococcus intranasal infection promotes CNS infiltration by streptococcal-specific Th17 cells. J. Clin. Investig. 2016, 126, 303–317. [Google Scholar] [CrossRef] [PubMed]
- Jeon, D.; Kim, S.H.; Kim, J.; Jeong, H.; Uhm, C.; Oh, H.; Cho, K.; Cho, Y.; Park, I.H.; Oh, J.; et al. Discovery of a new long COVID mouse model via systemic histopathological comparison of SARS-CoV-2 intranasal and inhalation infection. Biochim. Biophys. Acta Mol. Basis Dis. 2024, 1870, 167347. [Google Scholar] [CrossRef] [PubMed]
- Porte, L.; Valdivieso, F.; Wilmes, D.; Gaete, P.; Diaz, M.C.; Thompson, L.; Munita, J.; Alliende, R.; Varela, C.; Rickerts, V.; et al. Laboratory exposure to Coccidioides: Lessons learnt in a non-endemic country. J. Hosp. Infect. 2019, 102, 461–464. [Google Scholar] [CrossRef] [PubMed]
- Shubitz, L.; Peng, T.; Perrill, R.; Simons, J.; Orsborn, K.; Galgiani, J.N. Protection of mice against Coccidioides immitis intranasal infection by vaccination with recombinant antigen 2/PRA. Infect. Immun. 2002, 70, 3287–3289. [Google Scholar] [CrossRef] [PubMed]
- Viriyakosol, S.; Jimenez Mdel, P.; Gurney, M.A.; Ashbaugh, M.E.; Fierer, J. Dectin-1 is required for resistance to coccidioidomycosis in mice. mBio 2013, 4, e00597-12. [Google Scholar] [CrossRef] [PubMed]
- Stollings, L.M.; Jia, L.J.; Tang, P.; Dou, H.; Lu, B.; Xu, Y. Immune Modulation by Volatile Anesthetics. Anesthesiology 2016, 125, 399–411. [Google Scholar] [CrossRef] [PubMed]
- Fumagalli, V.; Rava, M.; Marotta, D.; Di Lucia, P.; Laura, C.; Sala, E.; Grillo, M.; Bono, E.; Giustini, L.; Perucchini, C.; et al. Administration of aerosolized SARS-CoV-2 to K18-hACE2 mice uncouples respiratory infection from fatal neuroinvasion. Sci. Immunol. 2022, 7, eabl9929. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Schelle, M.W.; Jain, M.; Lin, F.L.; Petzold, C.J.; Leavell, M.D.; Leary, J.A.; Cox, J.S.; Bertozzi, C.R. PapA1 and PapA2 are acyltransferases essential for the biosynthesis of the Mycobacterium tuberculosis virulence factor sulfolipid-1. Proc. Natl. Acad. Sci. USA 2007, 104, 11221–11226. [Google Scholar] [CrossRef] [PubMed]
- Stutz, M.D.; Allison, C.C.; Ojaimi, S.; Preston, S.P.; Doerflinger, M.; Arandjelovic, P.; Whitehead, L.; Bader, S.M.; Batey, D.; Asselin-Labat, M.-L.; et al. Macrophage and neutrophil death programs differentially confer resistance to tuberculosis. Immunity 2021, 54, 1758–1771.e7. [Google Scholar] [CrossRef] [PubMed]
- Mead, H.L.; Van Dyke, M.C.C.; Barker, B.M. Proper Care and Feeding of Coccidioides: A Laboratorian’s Guide to Cultivating the Dimorphic Stages of C. immitis and C. posadasii. Curr. Protoc. Microbiol. 2020, 58, e113. [Google Scholar] [CrossRef] [PubMed]
- Kirkland, T.N.; Fierer, J. Inbred mouse strains differ in resistance to lethal Coccidioides immitis infection. Infect. Immun. 1983, 40, 912–916. [Google Scholar] [CrossRef] [PubMed]
| Dose (CFU/mL) | Nebulized Dose (CFU) | Diluent | Test | Infected |
|---|---|---|---|---|
| 5 × 103 | 2.5 × 104 | H2O | Agar plates | Growth |
| 5 × 103 | 2.5 × 104 | H2O | Mice | 1/49 |
| 5 × 104 | 2.5 × 105 | H2O | Mice | 0/50 |
| 2 × 106 | 1 × 107 | H2O | Mice | 0/50 |
| 2 × 106 | 1 × 107 | PBS | Mice | 4/5 |
| 1 × 106 | 5 × 106 | PBS | Mice | 10/19 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Erlich, J.R.; Rodriguez, P.; Yau, K.P.S.; Tate, M.; Carlin, A.F.; Fierer, J.; Kirkland, T.N.; Hoffman, H.M.; Beyhan, S.; Croker, B.A. Development of a Mouse Model of Coccidioidomycosis Using an Inhalation Exposure System. J. Fungi 2025, 11, 599. https://doi.org/10.3390/jof11080599
Erlich JR, Rodriguez P, Yau KPS, Tate M, Carlin AF, Fierer J, Kirkland TN, Hoffman HM, Beyhan S, Croker BA. Development of a Mouse Model of Coccidioidomycosis Using an Inhalation Exposure System. Journal of Fungi. 2025; 11(8):599. https://doi.org/10.3390/jof11080599
Chicago/Turabian StyleErlich, Jonathan Rodrigo, Priscila Rodriguez, Ka Pui Sharon Yau, Matthew Tate, Aaron F. Carlin, Joshua Fierer, Theo N. Kirkland, Hal M. Hoffman, Sinem Beyhan, and Ben A. Croker. 2025. "Development of a Mouse Model of Coccidioidomycosis Using an Inhalation Exposure System" Journal of Fungi 11, no. 8: 599. https://doi.org/10.3390/jof11080599
APA StyleErlich, J. R., Rodriguez, P., Yau, K. P. S., Tate, M., Carlin, A. F., Fierer, J., Kirkland, T. N., Hoffman, H. M., Beyhan, S., & Croker, B. A. (2025). Development of a Mouse Model of Coccidioidomycosis Using an Inhalation Exposure System. Journal of Fungi, 11(8), 599. https://doi.org/10.3390/jof11080599






