Return to Play after SARS-CoV-2 Infection in Competitive Athletes of Distinct Sport Disciplines in Italy: A FMSI (Italian Federation of Sports Medicine) Study
Abstract
:1. Introduction
2. Methods
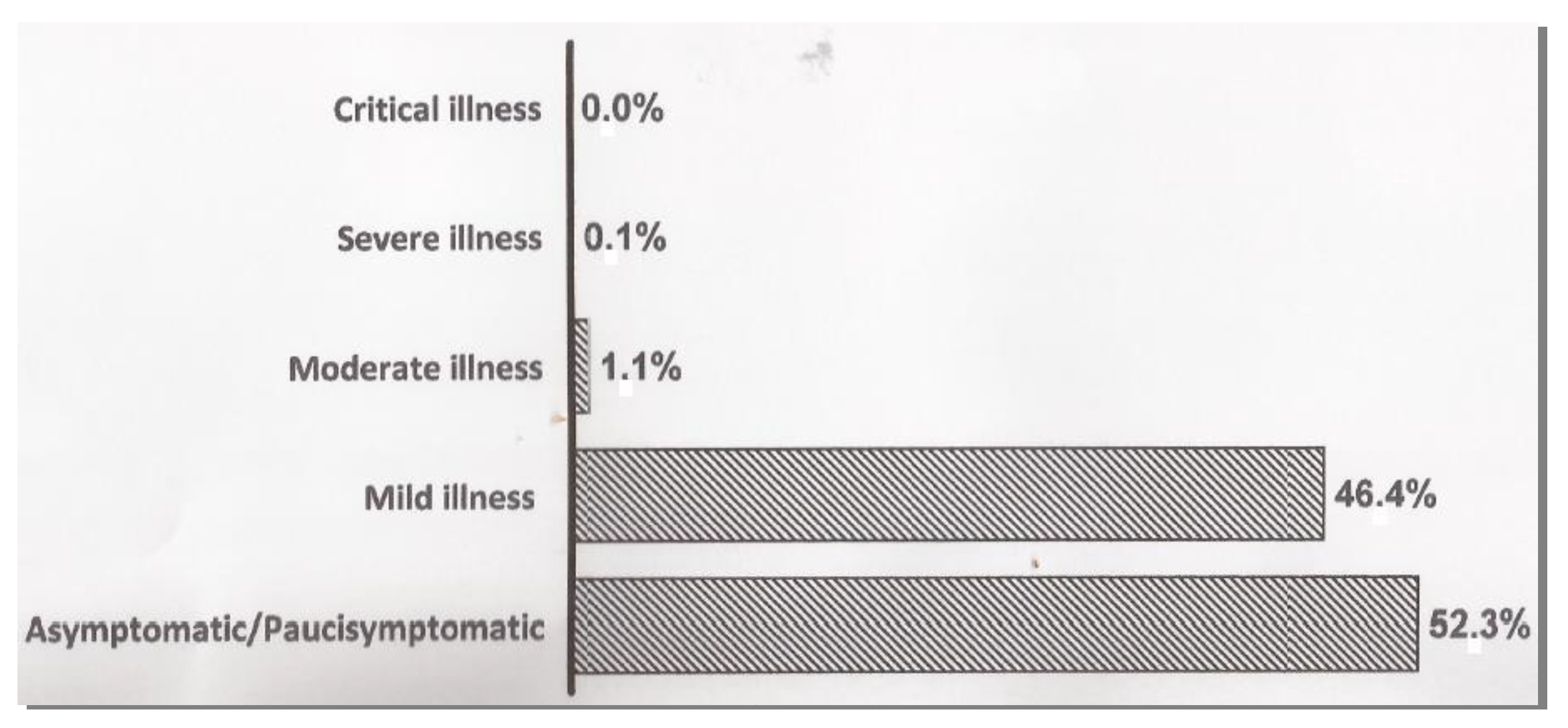
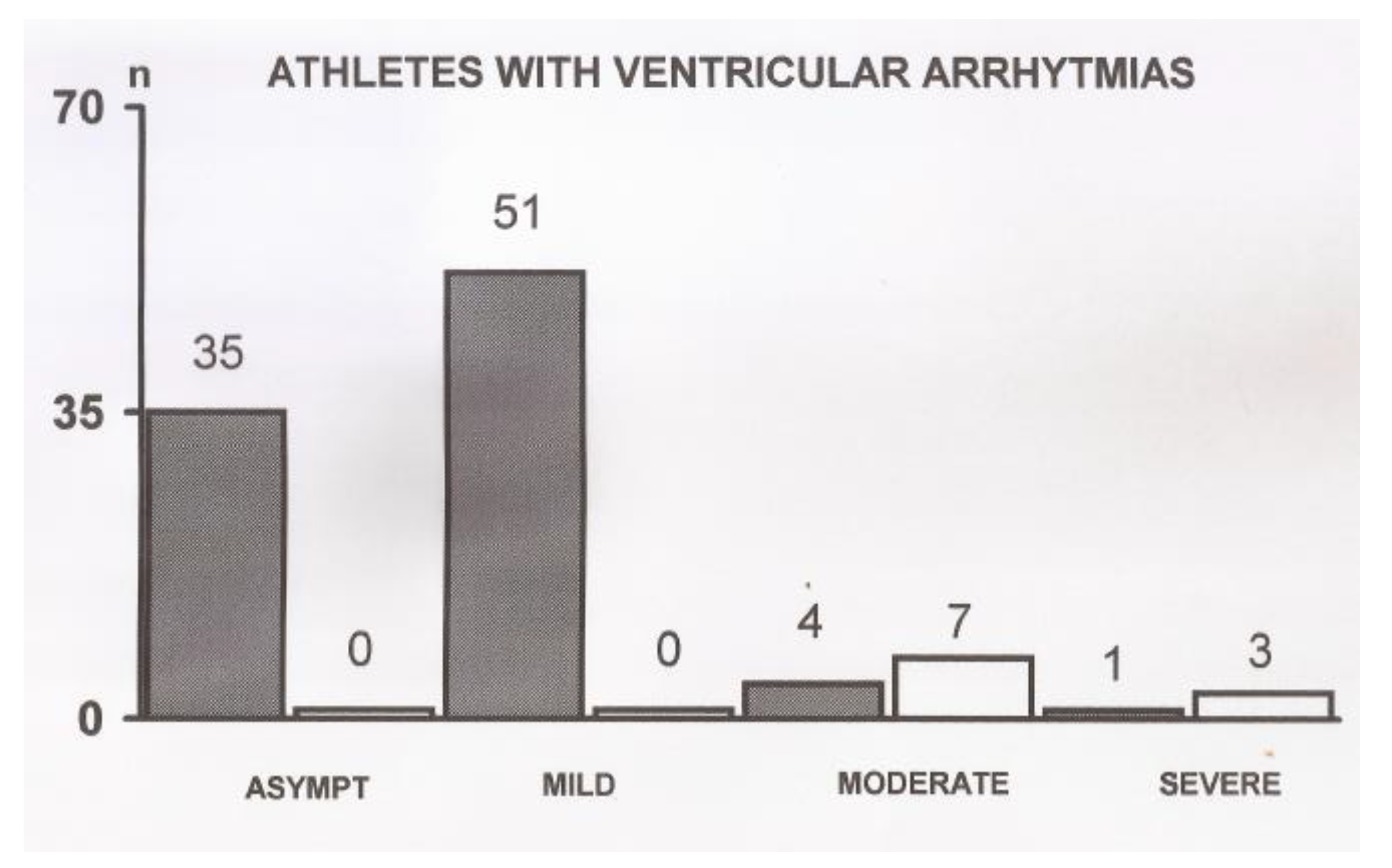
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Clerkin, K.J.; Fried, J.A.; Raikhelkar, J. Coronavirus disease 2019 (COVID-19) and cardiovascular disease. Circulation 2020, 14, 1648–1655. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moulson, N.; Petek, B.J.; Drezner, J.A.; Harmon, K.G.; Kliethermes, S.A.; Patel, M.R.; Baggish, A.L. SARS-CoV-2 Cardiac Involvement in Young Competitive Athletes. Circulation 2021, 144, 256–266. [Google Scholar] [CrossRef] [PubMed]
- Martinez, M.W.; Tucker, A.M.; Bloom, O.J.; Green, G.; DiFiori, J.P.; Solomon, G.; Phelan, D.; Kim, J.H.; Meeuwisse, W.; Sills, A.K.; et al. Prevalence of Inflammatory Heart Disease among Professional Athletes with Prior COVID-19 Infection Who Received Systematic Return-to-Play Cardiac Screening. JAMA Cardiol. 2021, 6, 745–752. [Google Scholar] [CrossRef] [PubMed]
- Gervasi, S.F.; Pengue, L.; Damato, L.; Monti, R.; Pradella, S.; Pirronti, T.; Bartoloni, A.; Epifani, F.; Saggese, A.; Cuccaro, F.; et al. Is extensive cardiopulmonary screening useful in athletes with previous asymptomatic or mild SARS-CoV-2 infection? Br. J. Sports Med. 2021, 55, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Daniels, C.J.; Rajpal, S.; Greenshields, J.T.; Rosenthal, G.L.; Chung, E.H.; Terrin, M.; Jeudy, J.; Mattson, S.E.; Law, I.H.; Borchers, J.; et al. Prevalence of Clinical and Subclinical Myocarditis in Competitive Athletes with Recent SARS-CoV-2 Infection. Results from the Big Ten COVID-19 Cardiac Registry. JAMA Cardiol. 2021, 6, 1078–1087. [Google Scholar] [CrossRef] [PubMed]
- Cavigli, L.; Frascaro, F.; Turchini, F.; Mochi, N.; Sarto, P.; Bianchi, S.; Parri, A.; Carraro, N.; Valente, S.; Focardi, M.; et al. A prospective study on the consequences of SARS-CoV-2 infection on the heart of young adult competitive athletes: Implications for a safe return-to-play. Int. J. Cardiol. 2021, 336, 130–136. [Google Scholar] [CrossRef]
- Starekova, J.; Bluemke, D.A.; Bradham, W.S.; Eckhardt, L.L.; Grist, T.M.; Kusmirek, J.E.; Purtell, C.S.; Schiebler, M.L.; Reeder, S.B. Evaluation for Myocarditis in Competitive Student Athletes Recovering from Coronavirus Disease 2019 with Cardiac Magnetic Resonance Imaging. JAMA Cardiol. 2021, 6, 945–950. [Google Scholar] [CrossRef] [PubMed]
- Hendrickson, B.S.; Stephens, R.E.; Chang, J.V.; Amburn, J.M.; Pierotti, L.L.; Johnson, J.L.; Hyden, J.C.; Johnson, J.N.; Philip, R.R. Cardiovascular evaluation after COVID-19 in 137 collegiate athletes. Results of an algorithm-guided screening. Circulation 2021, 143, 1926–1928. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.sport.governo.it/media/2422/circolare-idoneita-sportiva-np-covid-13-1-20.pdf (accessed on 10 December 2021).
- Drezner, J.A.; Sharma, S.; Baggish, A.; Papadakis, M.; Wilson, M.G.; Prutkin, J.M.; La Gerche, A.; Ackerman, M.J.; Borjesson, M.; Salerno, J.C.; et al. International criteria for electrocardiographic interpretation in athletes: Consensus statement. Br. J. Sports Med. 2017, 51, 704–731. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, R.T.; Lynch, J.B.; Del Rio, C. Mild or moderate COVID-19. N. Engl. J. Med. 2020, 383, 1757–1766. [Google Scholar] [CrossRef]
- Baggish, A.; Drezner, J.A.; Kim, J.; Martinez, M.; Prutkin, J.M. Resurgence of sport in the wake of COVID-19: Cardiac considerations in competitive athletes. Br. J. Sports Med. 2020, 54, 1130–1131. [Google Scholar] [CrossRef] [PubMed]
- Phelan, D.; Kim, J.H.; Elliott, M.D.; Wasfy, M.M.; Cremer, P.; Johri, A.M.; Emery, M.S.; Sengupta, P.P.; Sharma, S.; Martinez, M.W.; et al. Screening of potential cardiac involvement in competitive athletes recovering from COVID-19. An expert consensus statement. JACC Cardiovasc. Imaging 2020, 13, 2635–2652. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H. Screening Athletes for Miocardities with Cardiac Magnetic Resonance Imaging After COVID-19 Infection-Lessons from an English Philosopher. JAMA Cardiol. 2021, 6, 950–951. [Google Scholar] [CrossRef] [PubMed]
- Brito, D.; Meester, S.; Yanamala, N.; Patel, H.B.; Balcik, B.J.; Casaclang-Verzosa, G.; Seetharam, K.; Riveros, D.; Beto, R.J.; Balla, S.; et al. High Prevalence of Pericardial Involvement in College Student Athletes Recovering from COVID-19. JACC Cardiovasc. Imaging 2021, 14, 541–555. [Google Scholar] [CrossRef] [PubMed]
- Rajpal, S.; Tong, M.S.; Borchers, J.; Zareba, K.M.; Obarski, T.P.; Simonetti, O.P.; Daniels, C.J. Cardiovascular magnetic resonance findings in competitive athletes recovering from COVID-19 infection. JAMA Cardiol. 2021, 6, 116–118. [Google Scholar] [CrossRef] [PubMed]
| Males | Females | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Under 18 | 18–35 | Over 35 | Overall Males | Under 18 | 18–35 | Over 35 | Overall Females | Overall Athletes | |
| SOCCER | 631 | 342 | 43 | 1016 | 41 | 29 | 3 | 73 | 1089 |
| BASKETBALL | 282 | 107 | 7 | 396 | 42 | 17 | 0 | 59 | 455 |
| VOLLEY | 52 | 32 | 10 | 94 | 264 | 92 | 4 | 360 | 454 |
| ATHLETICS | 57 | 72 | 113 | 242 | 40 | 36 | 34 | 110 | 352 |
| GYMNASTICS | 13 | 15 | 6 | 34 | 166 | 18 | 8 | 192 | 226 |
| TENNIS | 30 | 36 | 80 | 146 | 15 | 5 | 28 | 48 | 194 |
| SWIMMING | 54 | 15 | 24 | 93 | 60 | 15 | 15 | 90 | 183 |
| CYCLING | 21 | 35 | 89 | 145 | 1 | 2 | 6 | 9 | 154 |
| SPORT DANCE | 13 | 5 | 8 | 26 | 63 | 19 | 10 | 92 | 118 |
| RUGBY | 40 | 21 | 2 | 63 | 4 | 4 | 1 | 9 | 72 |
| FIGURE SKATING | 8 | 1 | 0 | 9 | 53 | 8 | 1 | 62 | 71 |
| BOXING | 8 | 26 | 6 | 40 | 2 | 1 | 1 | 4 | 44 |
| ICE HOCKEY | 17 | 20 | 3 | 40 | 1 | 1 | 0 | 2 | 42 |
| TRIATHLON | 0 | 9 | 27 | 36 | 0 | 2 | 2 | 4 | 40 |
| WATER POLO | 22 | 11 | 1 | 34 | 1 | 2 | 0 | 3 | 37 |
| WEIGHTLIFTING | 2 | 13 | 12 | 27 | 1 | 4 | 4 | 9 | 36 |
| BASEBALL | 20 | 9 | 3 | 32 | 1 | 0 | 0 | 1 | 33 |
| EQUESTRIAN SPORTS | 0 | 1 | 1 | 2 | 21 | 8 | 1 | 30 | 32 |
| ALPINE SKIING | 5 | 10 | 7 | 22 | 6 | 2 | 2 | 10 | 32 |
| KARATE | 8 | 9 | 4 | 21 | 4 | 2 | 0 | 6 | 27 |
| MOTORCYCLING | 5 | 12 | 9 | 26 | 0 | 0 | 1 | 1 | 27 |
| KICK BOXING | 5 | 8 | 5 | 18 | 2 | 3 | 0 | 5 | 23, |
| JUDO | 7 | 8 | 2 | 17 | 2 | 3 | 0 | 5 | 22 |
| ROWING | 5 | 2 | 4 | 11 | 3 | 2 | 2 | 7 | 18 |
| FENCING | 9 | 2 | 1 | 12 | 4 | 2 | 0 | 6 | 18 |
| SPORT CLIMBING | 4 | 3 | 3 | 10 | 5 | 0 | 1 | 6 | 16 |
| TAEKWON-DO | 6 | 3 | 3 | 12 | 3 | 0 | 1 | 4 | 16 |
| CANOEING/KAYAK | 4 | 5 | 1 | 10 | 4 | 0 | 1 | 5 | 15 |
| GOLF | 1 | 2 | 9 | 12 | 0 | 0 | 1 | 1 | 13 |
| FIELD HOCKEY | 3 | 2 | 0 | 5 | 3 | 4 | 1 | 8 | 13 |
| SYNCHRONIZED SWIMMING | 0 | 0 | 0 | 0 | 9 | 2 | 0 | 11 | 11 |
| SPEED SKATING | 3 | 1 | 0 | 4 | 6 | 1 | 0 | 7 | 11 |
| SOFTBALL | 0 | 0 | 0 | 0 | 8 | 3 | 0 | 11 | 11 |
| ICE FIGURE SKATING | 0 | 1 | 0 | 1 | 7 | 2 | 0 | 9 | 10 |
| TABLE TENNIS | 3 | 2 | 2 | 7 | 2 | 0 | 1 | 3 | 10 |
| Males | Females | |||||||
|---|---|---|---|---|---|---|---|---|
| Age | <18 | 18–35 | >35 | sub-set | <18 | 18–35 | >35 | sub-set |
| Nr of athletes with Arrhythmias | 42 | 68 | 79 | 189 | 10 | 20 | 20 | 50 |
| % on the cohort | 17.6% | 28.5% | 33.1% | 79.1% | 4.2% | 8.4% | 8.4% | 20.9% |
| Of which with pre-infection history | 0 | 5 | 14 | 19 | 1 | 1 | 7 | 9 |
| % on the cohort | 0% | 2.1% | 5.9% | 7.9% | 0.4% | 0.4% | 2.9% | 3.8% |
| Supraventricular premature beats | ||||||||
| Males | Females | |||||||
| <18 | 18–35 | >35 | sub-set | <18 | 18–35 | >35 | sub-set | |
| Nr of athletes with SPBs | 21 | 27 | 43 | 91 | 3 | 8 | 6 | 17 |
| % on the cohort | 19.4% | 25.0% | 39.8% | 84.3% | 2.8% | 7.4% | 5.5% | 15.7% |
| Of which with pre-infection history | 0 | 1 | 8 | 9 | 0 | 1 | 2 | 3 |
| % on the cohort | 0 % | 0.9% | 7.4% | 8.3% | 0 % | 0.9% | 1.8% | 2.8% |
| Premature ventricular beats | ||||||||
| Males | Females | |||||||
| Age | <18 | 18–35 | >35 | sub-set | <18 | 18–35 | >35 | sub-set |
| Nr of athletes with PVBs | 12 | 35 | 34 | 81 | 3 | 8 | 9 | 20 |
| % on the cohort | 11.9% | 34.7% | 33.7% | 80.2% | 2.9% | 7.9% | 8.9% | 19.8% |
| Of which with pre-infection history | 0 | 3 | 8 | 11 | 1 | 0 | 2 | 3 |
| % on the cohort | 0 % | 2.9% | 7.9% | 10.9% | 0.9% | 0% | 1.9% | 2.9% |
| Complexity | ||||||||
| Isolated | 9 | 28 | 27 | 64 | 3 | 3 | 6 | 12 |
| 8.9% | 27.7% | 26.7% | 63.4% | 2.9% | 2.9% | 5.9% | 11.9% | |
| Bigeminy | 1 | 1 | 1 | 3 | 0 | 2 | 2 | 4 |
| 0.9% | 0.9% | 0.9% | 2.9% | 0% | 1.9% | 1.9% | 3.9% | |
| Trigeminy | 1 | 0 | 1 | 2 | 0 | 1 | 0 | 1 |
| 0.9% | 0% | 0.9% | 1.9% | 0% | 0.9% | 0% | 0.9% | |
| Couples | 0 | 5 | 5 | 10 | 0 | 2 | 1 | 3 |
| 0 % | 4.9% | 4.9% | 9,9% | 0% | 1.9% | 0.9% | 2.9% | |
| Runs | 1 | 1 | 2 | 0 | ||||
| 0.9% | 0.9% | 0.00% | 1.9% | 0% | 0% | 0% | 0% | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Casasco, M.; Iellamo, F.; Scorcu, M.; Parisi, A.; Tavcar, I.; Brugin, E.; Martini, B.; Fossati, C.; Pigozzi, F. Return to Play after SARS-CoV-2 Infection in Competitive Athletes of Distinct Sport Disciplines in Italy: A FMSI (Italian Federation of Sports Medicine) Study. J. Cardiovasc. Dev. Dis. 2022, 9, 59. https://doi.org/10.3390/jcdd9020059
Casasco M, Iellamo F, Scorcu M, Parisi A, Tavcar I, Brugin E, Martini B, Fossati C, Pigozzi F. Return to Play after SARS-CoV-2 Infection in Competitive Athletes of Distinct Sport Disciplines in Italy: A FMSI (Italian Federation of Sports Medicine) Study. Journal of Cardiovascular Development and Disease. 2022; 9(2):59. https://doi.org/10.3390/jcdd9020059
Chicago/Turabian StyleCasasco, Maurizio, Ferdinando Iellamo, Marco Scorcu, Attilio Parisi, Irena Tavcar, Erica Brugin, Barbara Martini, Chiara Fossati, and Fabio Pigozzi. 2022. "Return to Play after SARS-CoV-2 Infection in Competitive Athletes of Distinct Sport Disciplines in Italy: A FMSI (Italian Federation of Sports Medicine) Study" Journal of Cardiovascular Development and Disease 9, no. 2: 59. https://doi.org/10.3390/jcdd9020059
APA StyleCasasco, M., Iellamo, F., Scorcu, M., Parisi, A., Tavcar, I., Brugin, E., Martini, B., Fossati, C., & Pigozzi, F. (2022). Return to Play after SARS-CoV-2 Infection in Competitive Athletes of Distinct Sport Disciplines in Italy: A FMSI (Italian Federation of Sports Medicine) Study. Journal of Cardiovascular Development and Disease, 9(2), 59. https://doi.org/10.3390/jcdd9020059








