The Effect of a Single Bout of Resistance Exercise with Blood Flow Restriction on Arterial Stiffness in Older People with Slow Gait Speed: A Pilot Randomized Study
Abstract
:1. Introduction
2. Methods
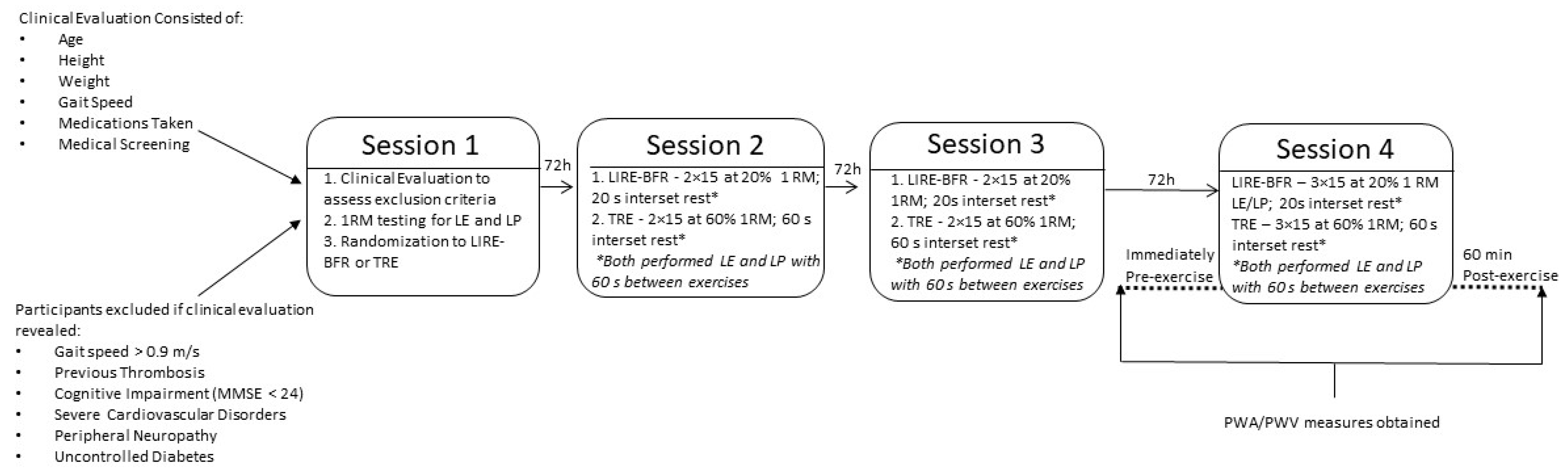
2.1. Study Design
2.2. Participants
2.3. Study Protocol Overview
2.3.1. Session One—Clinical Evaluation, 1RM Testing and Randomization
Clinical Evaluation
One-Repetition (1-RM) Maximum Assessment
Randomization
2.3.2. Session Two and Three—Familiarization
Determination of Individual Blood Flow Restriction Pressure
2.3.3. Session Four—Pilot Data Collection
Exercise Session
Assessment of Arterial Stiffness
Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Matthew, J.; Rossman, T.J.; Martens, C.R.; Seals, D.R. Healthy Lifestyle-Based Approaches for Successful Vascular Aging. J. Appl. Physiol. 2018, 125, 1888–1900. [Google Scholar]
- Vanhees, L.; Rauch, B.; Piepoli, M.; Van Buuren, F.; Takken, T.; Bo, M. Importance of characteristics and modalities of physical activity and exercise in the management of cardiovascular health in individuals with cardiovascular disease (Part III). Eur. J. Prev. Cardiol. 2012, 19, 1333–1356. [Google Scholar] [CrossRef] [PubMed]
- Carmel, M.; McEniery, Y.; Ian, R.; Hall, A.Q.; Ian, B.; Wilkinson, J.R.C. Normal Vascular Aging: Differential Effects on Wave Reflection and Aortic Pulse Wave Velocity. Aging Vasc. Funct. 2005, 46, 1753–1760. [Google Scholar] [CrossRef] [Green Version]
- Lopez, P.; Pinto, R.S.; Radaelli, R.; Rech, A.; Grazioli, R.; Izquierdo, M.; Cadore, E.L. Benefits of resistance training in physically frail elderly: A systematic review. Aging Clin. Exp. Res. 2018, 30, 889–899. [Google Scholar] [CrossRef]
- Nelson, M.E.; Rejeski, W.J.; Blair, S.N.; Duncan, P.W.; Judge, J.O.; King, A.C.; Macera, C.A.; Castaneda-Sceppa, C. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Circulation 2007, 116, 1094–1105. [Google Scholar] [CrossRef] [Green Version]
- Centner, C.; Wiegel, P.; Gollhofer, A.; König, D. Effects of Blood Flow Restriction Training on Muscular Strength and Hypertrophy in Older Individuals: A Systematic Review and Meta-Analysis. Sports Med. 2018, 49, 95–108. [Google Scholar] [CrossRef] [Green Version]
- Grigoriadis, G.; Rosenberg, A.J.; Lefferts, W.K.; Wee, S.O.; Schroeder, E.C.; Baynard, T. Similar Effects of Acute Resistance Exercise on Carotid Stiffness in Males and Females. Endoscopy 2020, 41, 82–88. [Google Scholar] [CrossRef]
- Okamoto, T.; Kobayashi, R.; Sakamaki-sunaga, M. Effect of Resistance Exercise on Arterial Stiffness during the Follicular and Luteal Phases of the Menstrual Cycle. Int. J. Sports Med. 2017, 38, 347–352. [Google Scholar] [CrossRef]
- Thiebaud, R.S.; Fahs, C.A.; Rossow, L.M.; Loenneke, J.P.; Kim, D.; Mouser, J.G.; Beck, T.W.; Bemben, D.A.; Larson, R.D.; Bemben, M.G. Effects of age on arterial stiffness and central blood pressure after an acute bout of resistance exercise. Eur. J. Appl. Physiol. 2015, 116, 39–48. [Google Scholar] [CrossRef]
- Yoon, E.S.; Jung, S.J.; Cheun, S.K. Effects of Acute Resistance Exercise on Arterial Stiffness in Young Men. Korean Soc. Cardiol. 2010, 40, 16–22. [Google Scholar] [CrossRef]
- Figueroa, A.; Okamoto, T.; Jaime, S.J.; Fahs, C.A. Impact of high- and low-intensity resistance training on arterial stiffness and blood pressure in adults across the lifespan: A review. Eur. J. Physiol. 2018, 471, 467–478. [Google Scholar] [CrossRef]
- Otsuki, T.; Maeda, S.; Iemitsu, M.; Saito, Y.; Tanimura, Y.; Ajisaka, R.; Miyauchi, T. Vascular endothelium-derived factors and arterial stiffness in strength- and endurance-trained men. Am. J. Physiol. Circ. Physiol. 2007, 292, H786–H791. [Google Scholar] [CrossRef] [Green Version]
- Vlachopoulos, C.; Aznaouridis, K.; Stefanadis, C. Prediction of Cardiovascular Events and All-Cause Mortality With Arterial Stiffness. J. Am. Coll. Cardiol. 2010, 55, 1318–1327. [Google Scholar] [CrossRef] [Green Version]
- Spranger, M.D.; Krishnan, A.C.; Levy, P.D.; O’Leary, D.S.; Smith, S.A. Blood flow restriction training and the exercise pressor reflex: A call for concern. Am. J. Physiol. Circ. Physiol. 2015, 309, H1440–H1452. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, M.; Meireles, K.; Marty, D.; Spranger, D.S.; O’Leary, H.R.; Peçanha, T. Clinical safety of blood flow restricted training? A comprehensive review of altered muscle metaboreflex in cardiovascular disease during ischemic exercise. Am. J. Physiol. Circ. Physiol. 2020, 318, H90–H109. [Google Scholar] [CrossRef]
- Uhlmann, S.; Friedrichs, U.; Eichler, W.; Hoffmann, S.; Wiedemann, P. Direct Measurement of VEGF-Induced Nitric Oxide Production by Choroidal Endothelial Cells 1. Microvasc. Res. 2001, 62, 179–189. [Google Scholar] [CrossRef]
- Diaz, M.; Parikh, V.; Ismail, S.; Maxamed, R.; Tye, E.; Austin, C.; Dew, T.; Graf, B.A.; Vanhees, L.; Degens, H.; et al. Nitric Oxide Differential effects of resveratrol on the dilator responses of femoral arteries, ex vivo. Nitric Oxide 2019, 92, 1–10. [Google Scholar] [CrossRef]
- Takano, H.; Morita, T.; Iida, H.; Asada, K.-I.; Kato, M.; Uno, K.; Hirose, K.; Matsumoto, A.; Takenaka, K.; Hirata, Y.; et al. Hemodynamic and hormonal responses to a short-term low-intensity resistance exercise with the reduction of muscle blood flow. Eur. J. Appl. Physiol. 2005, 95, 65–73. [Google Scholar] [CrossRef]
- Lanziotti, S.; Neri, A.L.; Ferrioli, E.; Lourenço, R.A. Fenótipo de fragilidade: Influência de cada item na determinação da fragilidade em idosos comunitários—Rede Fibra Phenotype of frailty: The influence of each item in determining frailty in community-dwelling elderly—The Fibra Study. Cien. Saud. Colet. 2016, 21, 3483–3492. [Google Scholar] [CrossRef] [Green Version]
- Peel, N.M.; Kuys, S.S.; Klein, K. Gait Speed as a Measure in Geriatric Assessment in Clinical Settings: A Systematic Review. J. Gerontol. Ser. 2012, 68, 39–46. [Google Scholar] [CrossRef]
- Brown, L.E.E.E.; Weir, J.P. ASEP Procedures recommendation I: Accurate assessment of muscular strength and power. JEP J. Exerc. Physiol. 2001, 4, 1–21. [Google Scholar]
- Nunes, J.P.; Grgic, J.; Cunha, P.M.; Ribeiro, A.S.; Schoenfeld, B.J.; de Salles, B.F.; Cyrino, E.S. What influence does resistance exercise order have on muscle strength gains and hypertrophy? A systematic review and meta-analysis. Sport Med. 2019, 21, 149–157. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tomeleri, C.M.; Nunes, J.P.; Souza, M.F.; Gerage, A.M.; Marcori, A.; Iarosz, K.C.; Cardoso-Júnior, C.G.; Cyrino, E.S. Resistance Exercise Order Does Not Affect the Magnitude and Duration of Postexercise Blood Pressure in Older Women. J. Strength Cond. Res. 2020, 34, 1062–1070. [Google Scholar] [CrossRef] [PubMed]
- KAATSU Global Inc. Kaatsu Equipment User Manual Including Kaatsu Protocols for Including KAATSU Protocols for; KAATSU Global Inc.: Los Angeles, CA, USA, 2017; pp. 1–139. [Google Scholar]
- Weatherholt, A.M.; VanWye, W.R.; Lohmann, J.; Owens, J.G. The Effect of Cuff Width for Determining Limb Occlusion Pressure: A Comparison of Blood Flow Restriction Devices. Int. J. Exerc. Sci. 2019, 12, 136–143. [Google Scholar]
- Shimizu, R.; Hotta, K.; Yamamoto, S.; Matsumoto, T.; Kamiya, K.; Kato, M.; Hamazaki, N.; Kamekawa, D.; Akiyama, A.; Kamada, Y.; et al. Low-intensity resistance training with blood flow restriction improves vascular endothelial function and peripheral blood circulation in healthy elderly people. Eur. J. Appl. Physiol. 2016, 116, 749–757. [Google Scholar] [CrossRef]
- Libardi, C.A.; Chacon-Mikahil, M.P.T.; Cavaglieri, C.; Tricoli, V.; Roschel, H.; Vechin, F.; Conceição, M.S.; Ugrinowitsch, C. Effect of concurrent training with blood flow restriction in the elderly. Int. J. Sports Med. 2015, 36, 395–399. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laurent, S.; Cockcroft, J.; Van Bortel, L.; Boutouyrie, P.; Giannattasio, C.; Hayoz, D.; Pannier, B.; Vlachopoulos, C.; Wilkinson, I.; Struijker-Boudier, H.; et al. Expert consensus document on arterial stiffness: Methodological issues and clinical applications. Eur. Heart J. 2006, 27, 2588–2605. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Siebenhofer, A.; Kemp, C.R.W.; Sutton, A.; Williams, B. The reproducibility of central aortic blood pressure measurements in healthy subjects using applanation tonometry and sphygmocardiography. J. Hum. Hypertens. 1999, 13, 625–629. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bortel, L.M.; Van Duprez, D.; Starmans-kool, M.J.; Safar, M.E.; Giannattasio, C.; Cockcroft, J.; Kaiser, D.R.; Thuillez, C. Clinical Apllications of Arterial Stiffness, Task Force III: Recommendations for User Procedures. Am. J. Hypertens. 2002, 7061, 445–452. [Google Scholar] [CrossRef] [Green Version]
- David, M.; Malti, O.; AlGhatrif, M.; Wright, J.; Canepa, M.; Strait, J.B. Pulse Wave Velocity Testing in the Baltimore Longitudinal Study of Aging 2. Central Blood Pressure Measurement Using Pulse Wave Analysis (PWA). J. Vis. Exp. 2014, 84, 50817. [Google Scholar] [CrossRef] [Green Version]
- Wilkinson, I.B.; Mceniery, C.M.; John, R.; Lemogoum, D.; Leeman, M.; Degaute, J.; Van de Borne, P.; Van Bortel, L.M. Pulse waveform analysis and arterial stiffness: Realism can replace evangelism and scepticism. J. Hypertens. 2005, 23, 213–215. [Google Scholar] [CrossRef]
- Miyachi, M.; Kawano, H.; Sugawara, J.; Takahashi, K.; Hayashi, K.; Yamazaki, K.; Tabata, I.; Tanaka, H. Unfavorable Effects of Resistance Training on Central Arterial Compliance. Circulation 2004, 110, 2858–2863. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kawano, H.; Tanaka, H.; Miyachi, M.; Kawano, T. Resistance training and arterial compliance keeping the benefits while minimizing the stiffening. J. Hypertens. 2006, 24, 1753–1759. [Google Scholar] [CrossRef] [Green Version]
- Okamoto, T.; Masuhara, M.; Ikuta, K. Upper but not lower limb resistance training increases arterial stiffness in humans. Eur. J. Appl. Physiol. 2009, 107, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Casey, D.P.; Beck, D.T.; Braith, R.W. Progressive Resistance Training Without Volume Increases Does Not Alter Arterial Stiffness and Aortic Wave Reflection. Exp. Biol. Med. 2007, 232, 1228–1235. [Google Scholar] [CrossRef] [PubMed]
- Collier, S.R.; Frechette, V.; Sandberg, K.; Schafer, P.; Ji, H.; Smulyan, H.; Fernhall, B. Sex differences in resting hemodynamics and arterial stiffness following 4 weeks of resistance versus aerobic exercise training in individuals with pre-hypertension to stage 1 hypertension. Biol. Sex Differ. 2011, 2, 9. [Google Scholar] [CrossRef] [Green Version]
- Ho, S.S.; Radavelli-Bagatini, S.; Dhaliwal, S.S.; Hills, A.P.; Pal, S. Resistance, Aerobic, and Combination Training on Vascular Function in Overweight and Obese Adults. J. Clin. Hypertens. 2012, 14, 848–854. [Google Scholar] [CrossRef]
- Figueroa, A.; Vicil, F. Post-exercise aortic hemodynamic responses to low-intensity resistance exercise with and without vascular occlusion. Scand. J. Med. Sci. Sports 2010, 21, 431–436. [Google Scholar] [CrossRef] [PubMed]
- Nascimento, C.; Schoenfeld, B.J.; Prestes, J. Potential Implications of Blood Flow Restriction Exercise on Vascular Health: A Brief Review. Sport Med. 2019, 50, 73–81. [Google Scholar] [CrossRef]
- Vatner, S.F.; Zhang, J.; Vyzas, C.; Mishra, K.; Graham, R.M.; Vatner, D.E. Vascular Stiffness in Aging and Disease. Front. Physiol. 2021, 12, 762437. [Google Scholar] [CrossRef] [PubMed]
- Tsaia, J.P.; Hsu, B.G. Arterial stiffness: A brief review. Tzu Chi Med. J. 2021, 33, 115–121. [Google Scholar] [CrossRef]
- Meani, P.; Maloberti, A.; Sormani, P.; Colombo, G.; Giupponi, L.; Stucchi, M.; Varrenti, M.; Vallerio, P.; Facchetti, R.; Grassi, G.; et al. Determinants of carotid-femoral pulse wave velocity progression in hypertensive patients over a 3.7 years follow-up. Blood Press. 2018, 27, 32–40. [Google Scholar] [CrossRef]
- Rossow, L.M.; Fahs, C.A.; Sherk, V.D.; Seo, D.-I.; Bemben, D.A.; Bemben, M.G. The effect of acute blood-flow-restricted resistance exercise on postexercise blood pressure. Clin. Physiol. Funct. Imaging 2011, 31, 429–434. [Google Scholar] [CrossRef] [PubMed]
- Patterson, S.D.; Hughes, L.; Warmington, S.; Burr, J.; Scott, B.R.; Owens, J.; Takashi, A.; Nielsen, J.L.; Libardi, C.A.; Laurentino, G.; et al. Blood Flow Restriction Exercise: Considerations of Methodology, Application, and Safety. Front. Physiol. 2019, 10, 00533. [Google Scholar] [CrossRef] [PubMed]
- Tai, Y.L.; Marshall, E.M.; Glasgow, A.; Parks, J.C.; Sensibello, L.; Kingsley, J.D. Pulse wave reflection responses to bench press with and without practical blood flow restriction. Appl. Physiol. Nutr. Metab. 2019, 44, 341–347. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Forde, C.; Johnston, M.; Haberlin, C.; Breen, P.; Greenan, S.; Gissane, C.; Comyns, T.; Maher, V.; Gormley, J. Low Dose Resistance Exercise: A Pilot Study Examining Effects on Blood Pressure and Augmentation Index Between Intensities. High Blood Press. Cardiovasc. Prev. 2020, 27, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Kambic, T.; Novakovi, M.; Tomažin, K.; Strojnik, V.; Borut, J. Blood Flow Restriction Resistance Exercise Improves Muscle Strength and Hemodynamics, but Not Vascular Function in Coronary Artery Disease Patients: A Pilot Randomized Controlled Trial. Front. Physiol. 2019, 10, 656. [Google Scholar] [CrossRef]
- Bianchi, S.; Maloberti, A.; Peretti, A.; Garatti, L.; Palazzini, M.; Occhi, L.; Bassi, I.; Sioli, S.; Biolcati, M.; Giani, V.; et al. Determinants of Functional Improvement After Cardiac Rehabilitation in Acute Coronary Syndrome. High Blood Press. Cardiovasc. Prev. 2021, 28, 579–587. [Google Scholar] [CrossRef]
- Guimarães, R.M. Expectativa de vida com e sem multimorbidade entre idosos brasileiros: Pesquisa Nacional de Saúde 2013. Rev. Bras. Estud. Popul. 2020, 37, 1–15.e0117. [Google Scholar] [CrossRef]

| TRE | LIRE-BFR | p-Value | |
|---|---|---|---|
| Age (years) | 82.0 (7.4) | 82.8 (5.2) | 0.796 |
| Body weight (kg) | 67.9 (14.6) | 67.3 (12.1) | 0.929 |
| Height (m) | 1.54 (0.06) | 1.55 (0.07) | 0.774 |
| Body mass index (kg/m2) | 28.5 (6.3) | 27.8 (3.9) | 0.762 |
| Gait speed (m/s) | 0.74 (0.11) | 0.61 (0.13) | 0.052 |
| 1RM test—Leg press (lb) | 110.0 (62.4) | 119.0 (35.1) | 0.709 |
| 1RM test—Leg extension (lb) | 70.0 (25.8) | 67.0 (18.9) | 0.785 |
| Anti-hypertensives | 71.4 (%) | 100.0 (%) | 0.154 |
| Anti-hypercholesterolemia | 42.9 (%) | 70.0 (%) | 0.350 |
| Anti-depressant | 42.9 (%) | 60.0 (%) | 0.637 |
| Anti-anxiety | 0.0 (%) | 20.0 (%) | 0.485 |
| Anti-psychotic | 14.3 (%) | 10.0 (%) | 0.999 |
| Platelet anti-aggregant | 42.9 (%) | 30.0 (%) | 0.644 |
| Oral Hypoglycemic | 57.1 (%) | 10.0 (%) | 0.101 |
| Dementia | 14.3 (%) | 10.0 (%) | 0.999 |
| Anti-convulsant | 14.3 (%) | 10.0 (%) | 0.999 |
| Anti-parkinson | 0.0 (%) | 20.0 (%) | 0.48 |
| Variables | Pre | Post | Effects—p-Value | ||
|---|---|---|---|---|---|
| Group × Time | Group | Time | |||
| Aortic SBP (mmHg) | 0.627 | 0.255 | 0.025 | ||
| TRE | 118 (106; 131) | 124 (110; 138) | |||
| LIRE-BFR | 126 (115; 137) | 135 (122; 148) | |||
| Aortic DBP (mmHg) | 0.373 | 0.036 | 0.945 | ||
| TRE | 63 (57; 68) | 61 (56; 67) | |||
| LIRE-BFR | 69 (64; 74) | 70 (65; 75) | |||
| Aortic pulse pressure (mmHg) | 0.790 | 0.723 | 0.007 | ||
| TRE | 55 (45; 64) | 62 (51; 73) | |||
| LIRE-BFR | 56 (48; 65) | 65 (55; 75) | |||
| Radial SBP (mmHg) | 0.623 | 0.504 | 0.017 | ||
| TRE | 129 (117; 142) | 135 (121; 150) | |||
| LIRE-BFR | 133 (122; 144) | 143 (129; 156) | |||
| Radial DBP (mmHg) | 0.262 | 0.024 | 0.843 | ||
| TRE | 62 (57; 67) | 60 (55; 66) | |||
| LIRE-BFR | 68 (64; 73) | 70 (64; 75) | |||
| Radial MAP (mmHg) | 0.437 | 0.112 | 0.189 | ||
| TRE | 84 (76; 92) | 86 (77; 95) | |||
| LIRE-BFR | 91 (84; 98) | 96 (87; 104) | |||
| Radial pulse pressure (mmHg) | 0.891 | 0.763 | 0.009 | ||
| TRE | 66 (56; 76) | 75 (63; 86) | |||
| LIRE-BFR | 64 (55; 73) | 73 (62; 84) | |||
| Augmentation pressure (mmHg) | 0.130 | 0.070 | 0.005 | ||
| TRE | 19 (13; 26) | 22 (16; 29) | |||
| LIRE-BFR | 23 (18; 29) | 33 (27; 39) | |||
| Pulse wave velocity (m/s) | 0.682 | 0.556 | 0.031 | ||
| TRE | 11.6 (8.7; 15.5) | 12.7 (9.6; 16.8) | |||
| LIRE-BFR | 10.6 (8.1; 13.8) | 11.2 (8.7; 14.5) | |||
| AIx (%) | 0.159 | 0.037 | 0.146 | ||
| TRE | 36.3 (27; 45) | 36.4 (29; 43) | |||
| LIRE-BFR | 41.9 (34; 49) | 50.2 (43; 57) | |||
| AIx75 (%) | 0.152 | 0.094 | 0.209 | ||
| TRE | 31.9 (21; 41) | 31.3 (24; 38) | |||
| LIRE-BFR | 35.9 (27; 44) | 44.3 (37; 51) | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amorim, S.; Gaspar, A.P.; Degens, H.; Cendoroglo, M.S.; de Mello Franco, F.G.; Ritti-Dias, R.M.; Cucato, G.G.; Rolnick, N.; de Matos, L.D.N.J. The Effect of a Single Bout of Resistance Exercise with Blood Flow Restriction on Arterial Stiffness in Older People with Slow Gait Speed: A Pilot Randomized Study. J. Cardiovasc. Dev. Dis. 2022, 9, 85. https://doi.org/10.3390/jcdd9030085
Amorim S, Gaspar AP, Degens H, Cendoroglo MS, de Mello Franco FG, Ritti-Dias RM, Cucato GG, Rolnick N, de Matos LDNJ. The Effect of a Single Bout of Resistance Exercise with Blood Flow Restriction on Arterial Stiffness in Older People with Slow Gait Speed: A Pilot Randomized Study. Journal of Cardiovascular Development and Disease. 2022; 9(3):85. https://doi.org/10.3390/jcdd9030085
Chicago/Turabian StyleAmorim, Samuel, Alexandra Passos Gaspar, Hans Degens, Maysa Seabra Cendoroglo, Fábio Gazelato de Mello Franco, Raphael Mendes Ritti-Dias, Gabriel Grizzo Cucato, Nicholas Rolnick, and Luciana Diniz Nagem Janot de Matos. 2022. "The Effect of a Single Bout of Resistance Exercise with Blood Flow Restriction on Arterial Stiffness in Older People with Slow Gait Speed: A Pilot Randomized Study" Journal of Cardiovascular Development and Disease 9, no. 3: 85. https://doi.org/10.3390/jcdd9030085
APA StyleAmorim, S., Gaspar, A. P., Degens, H., Cendoroglo, M. S., de Mello Franco, F. G., Ritti-Dias, R. M., Cucato, G. G., Rolnick, N., & de Matos, L. D. N. J. (2022). The Effect of a Single Bout of Resistance Exercise with Blood Flow Restriction on Arterial Stiffness in Older People with Slow Gait Speed: A Pilot Randomized Study. Journal of Cardiovascular Development and Disease, 9(3), 85. https://doi.org/10.3390/jcdd9030085






