Use of Echocardiography Under Hypoxic Stress Without Exercise to Assess Right to Left Shunting
Abstract
1. Introduction
2. Materials and Methods
2.1. Hypoxic Simulation Testing Without Exercise—Transthoracic Echocardiography
2.2. Statistical Analysis
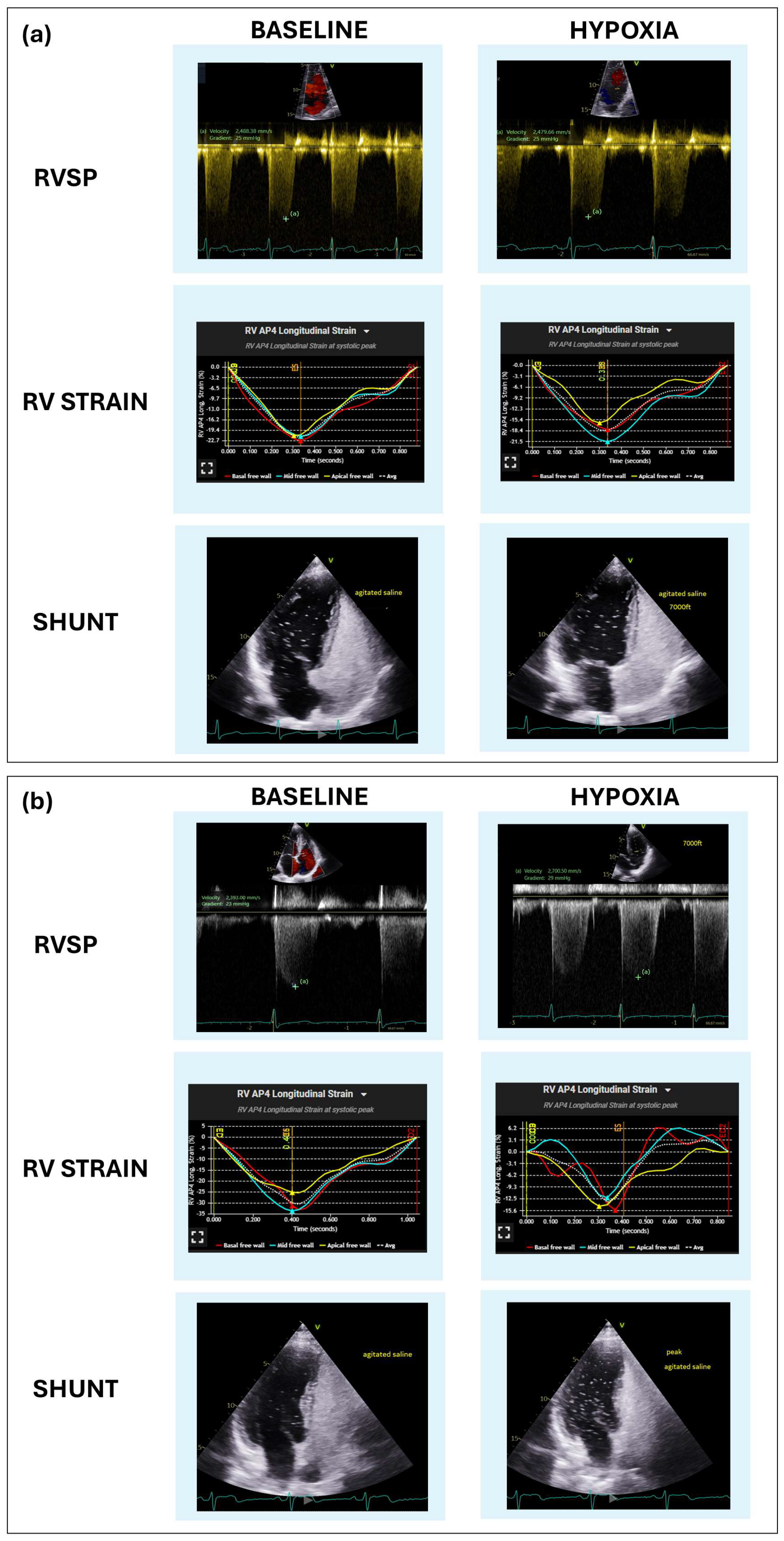
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| RV | Right ventricle |
| HST | Hypoxic simulation testing |
| TTE | Transthoracic echocardiography |
| RVSP | Right ventricular systolic pressure |
| TAPSE | Tricuspid annular plane systolic excursion |
| PFO | Patent foramen ovale |
| FiO2 | Fraction of inhaled oxygen |
| S wave | Lateral tricuspid annulus during systole |
| ASE | American Society of Echocardiography |
| SD | Standard deviations |
| P25-P75 | The 25th and 75th percentiles |
| LVEF | Left ventricle ejection fraction |
| HAPE | High-altitude pulmonary edema |
| TEE | transesophageal echocardiography |
| TCD | transcranial Doppler |
| CMR | cardiac magnetic resonance |
| V/Q | ventilation-perfusion |
| SVC | Superior vena cava |
References
- Merz, T.M.; Pichler Hefti, J. Humans at extreme altitudes. BJA Educ. 2021, 21, 455–461. [Google Scholar] [CrossRef]
- Martin-Gill, C.; Doyle, T.J.; Yealy, D.M. In-Flight Medical Emergencies: A Review. JAMA 2018, 320, 2580–2590. [Google Scholar] [CrossRef]
- Bagshaw, M.; Illig, P. The Aircraft Cabin Environment. In Travel Medicine; Elsevier: Amsterdam, The Netherlands, 2019; pp. 429–436. [Google Scholar]
- Heinonen, I.H.; Boushel, R.; Kalliokoski, K.K. The Circulatory and Metabolic Responses to Hypoxia in Humans—With Special Reference to Adipose Tissue Physiology and Obesity. Front. Endocrinol. 2016, 7, 116. [Google Scholar] [CrossRef] [PubMed]
- Crystal, G.J. Carbon Dioxide and the Heart: Physiology and Clinical Implications. Anesth. Analg. 2015, 121, 610–623. [Google Scholar] [CrossRef]
- Bartsch, P.; Gibbs, J.S. Effect of altitude on the heart and the lungs. Circulation 2007, 116, 2191–2202. [Google Scholar] [CrossRef] [PubMed]
- Allemann, Y.; Hutter, D.; Lipp, E.; Sartori, C.; Duplain, H.; Egli, M.; Cook, S.; Scherrer, U.; Seiler, C. Patent foramen ovale and high-altitude pulmonary edema. JAMA 2006, 296, 2954–2958. [Google Scholar] [CrossRef]
- Godart, F.; Rey, C.; Prat, A.; Vincentelli, A.; Chmaït, A.; Francart, C.; Porte, H. Atrial right-to-left shunting causing severe hypoxaemia despite normal right-sided pressures. Report of 11 consecutive cases corrected by percutaneous closure. Eur. Heart J. 2000, 21, 483–489. [Google Scholar] [CrossRef]
- Tobis, J.M.; Narasimha, D.; Abudayyeh, I. Patent Foramen Ovale Closure for Hypoxemia. Interv. Cardiol. Clin. 2017, 6, 547–554. [Google Scholar] [CrossRef] [PubMed]
- Dine, C.J.; Kreider, M.E. Hypoxia altitude simulation test. Chest 2008, 133, 1002–1005. [Google Scholar] [CrossRef]
- Stepanek, J.; Farina, J.M.; Mahmoud, A.K.; Chao, C.J.; Alsidawi, S.; Ayoub, C.; Barry, T.; Pereyra, M.; Scalia, I.G.; Abbas, M.T.; et al. Identifying the Causes of Unexplained Dyspnea at High Altitude Using Normobaric Hypoxia with Echocardiography. J. Imaging 2024, 10, 38. [Google Scholar] [CrossRef]
- Silvestry, F.E.; Cohen, M.S.; Armsby, L.B.; Burkule, N.J.; Fleishman, C.E.; Hijazi, Z.M.; Lang, R.M.; Rome, J.J.; Wang, Y.; American Society of Echocardiography; et al. Guidelines for the Echocardiographic Assessment of Atrial Septal Defect and Patent Foramen Ovale: From the American Society of Echocardiography and Society for Cardiac Angiography and Interventions. J. Am. Soc. Echocardiogr. 2015, 28, 910–958. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, M.; Rudski, L.G.; Addetia, K.; Afilalo, J.; D’Alto, M.; Freed, B.H.; Friend, L.B.; Gargani, L.; Grapsa, J.; Hassoun, P.M.; et al. Guidelines for the Echocardiographic Assessment of the Right Heart in Adults and Special Considerations in Pulmonary Hypertension: Recommendations from the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 2025, 38, 141–186, Correction in J. Am. Soc. Echocardiogr. 2025, 38, 641. [Google Scholar] [CrossRef]
- DiMarco, K.G.; Beasley, K.M.; Shah, K.; Speros, J.P.; Elliott, J.E.; Laurie, S.S.; Duke, J.W.; Goodman, R.D.; Futral, J.E.; Hawn, J.A.; et al. No effect of patent foramen ovale on acute mountain sickness and pulmonary pressure in normobaric hypoxia. Exp. Physiol. 2022, 107, 122–132. [Google Scholar] [CrossRef]
- West, B.H.; Fleming, R.G.; Al Hemyari, B.; Banankhah, P.; Meyer, K.; Rozier, L.H.; Murphy, L.S.; Coluzzi, A.C.; Rusheen, J.L.; Kumar, P.; et al. Relation of Patent Foramen Ovale to Acute Mountain Sickness. Am. J. Cardiol. 2019, 123, 2022–2025. [Google Scholar] [CrossRef]
- Meier, B.; Kalesan, B.; Mattle, H.P.; Khattab, A.A.; Hildick-Smith, D.; Dudek, D.; Andersen, G.; Ibrahim, R.; Schuler, G.; Walton, A.S.; et al. Percutaneous closure of patent foramen ovale in cryptogenic embolism. N. Engl. J. Med. 2013, 368, 1083–1091. [Google Scholar] [CrossRef]
- Sposato, L.A.; Albin, C.S.W.; Elkind, M.S.V.; Kamel, H.; Saver, J.L. Patent Foramen Ovale Management for Secondary Stroke Prevention: State-of-the-Art Appraisal of Current Evidence. Stroke 2024, 55, 236–247. [Google Scholar] [CrossRef]
- Lovering, A.T.; Elliott, J.E.; Davis, J.T. Physiological impact of patent foramen ovale on pulmonary gas exchange, ventilatory acclimatization, and thermoregulation. J. Appl. Physiol. (1985) 2016, 121, 512–517. [Google Scholar] [CrossRef][Green Version]
- Dunham-Snary, K.J.; Wu, D.; Sykes, E.A.; Thakrar, A.; Parlow, L.R.G.; Mewburn, J.D.; Parlow, J.L.; Archer, S.L. Hypoxic Pulmonary Vasoconstriction: From Molecular Mechanisms to Medicine. Chest 2017, 151, 181–192. [Google Scholar] [CrossRef] [PubMed]
- Naeije, R.; Chesler, N. Pulmonary circulation at exercise. Compr. Physiol. 2012, 2, 711–741. [Google Scholar] [CrossRef]
- Strange, G.; Stewart, S.; Celermajer, D.S.; Prior, D.; Scalia, G.M.; Marwick, T.H.; Gabbay, E.; Ilton, M.; Joseph, M.; Codde, J.; et al. Threshold of Pulmonary Hypertension Associated With Increased Mortality. J. Am. Coll. Cardiol. 2019, 73, 2660–2672. [Google Scholar] [CrossRef] [PubMed]
- Mojadidi, M.K.; Zaman, M.O.; Elgendy, I.Y.; Mahmoud, A.N.; Patel, N.K.; Agarwal, N.; Tobis, J.M.; Meier, B. Cryptogenic Stroke and Patent Foramen Ovale. J. Am. Coll. Cardiol. 2018, 71, 1035–1043. [Google Scholar] [CrossRef]
- De Cuyper, C.; Pauwels, T.; Derom, E.; De Pauw, M.; De Wolf, D.; Vermeersch, P.; Van Berendoncks, A.; Paelinck, B.; Vermeersch, G. Percutaneous Closure of PFO in Patients with Reduced Oxygen Saturation at Rest and during Exercise: Short- and Long-Term Results. J. Interv. Cardiol. 2020, 2020, 9813038. [Google Scholar] [CrossRef]
- Fenster, B.E.; Nguyen, B.H.; Buckner, J.K.; Freeman, A.M.; Carroll, J.D. Effectiveness of percutaneous closure of patent foramen ovale for hypoxemia. Am. J. Cardiol. 2013, 112, 1258–1262. [Google Scholar] [CrossRef]
- Song, J.K. Pearls and Pitfalls in the Transesophageal Echocardiographic Diagnosis of Patent Foramen Ovale. J. Am. Soc. Echocardiogr. 2023, 36, 895–905.e3. [Google Scholar] [CrossRef] [PubMed]
- Marriott, K.; Manins, V.; Forshaw, A.; Wright, J.; Pascoe, R. Detection of right-to-left atrial communication using agitated saline contrast imaging: Experience with 1162 patients and recommendations for echocardiography. J. Am. Soc. Echocardiogr. 2013, 26, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Deng, J.; Luo, Y.; Luo, S.; Zhan, H.; Zhou, F.; Li, S. Contrast-enhanced transcranial Doppler for the detection of right-to-left shunt: A new provocation method with a syringe-modified Valsalva maneuver. Brain Behav. 2024, 14, e3304. [Google Scholar] [CrossRef] [PubMed]
- Hamilton-Craig, C.; Sestito, A.; Natale, L.; Meduri, A.; Santangeli, P.; Infusino, F.; Pilato, F.; Di Lazzaro, V.; Crea, F.; Lanza, G.A. Contrast transoesophageal echocardiography remains superior to contrast-enhanced cardiac magnetic resonance imaging for the diagnosis of patent foramen ovale. Eur. J. Echocardiogr. 2011, 12, 222–227. [Google Scholar] [CrossRef]
- Meissner, I.; Khandheria, B.K.; Heit, J.A.; Petty, G.W.; Sheps, S.G.; Schwartz, G.L.; Whisnant, J.P.; Wiebers, D.O.; Covalt, J.L.; Petterson, T.M.; et al. Patent foramen ovale: Innocent or guilty? Evidence from a prospective population-based study. J. Am. Coll. Cardiol. 2006, 47, 440–445. [Google Scholar] [CrossRef]
- Agrawal, A.; Palkar, A.; Talwar, A. The multiple dimensions of Platypnea-Orthodeoxia syndrome: A review. Respir. Med. 2017, 129, 31–38. [Google Scholar] [CrossRef]
| Overall Population n = 125 | No Shunt n = 68 (54.4%) | Shunt n = 57 (45.6%) | p-Value | |
|---|---|---|---|---|
| Age (years) | 66 (50–74) | 67.00 (55.0–75.00) | 65.00 (48.0–72.00) | 0.306 |
| Sex Female n (%) Male n (%) | 63 (50.4) 62 (49.6) | 34 (50.7%) 33 (49.3%) | 27 (49.1%) 28 (50.9%) | 0.9 |
| BMI (kg/m2) | 28.8 (26.6–32.4) | 28.9 (26.8–32.8) | 28.70 (26.6–32.1) | 0.668 |
| Hematocrit (%) | 43.4 ± 5.02 | 43.1 ± 5.5 | 43.9 ± 4.5 | 0.395 |
| Hb (g/dL) | 14.3 ± 1.8 | 14.3 ± 1.7 | 14.4 ± 1.9 | 0.675 |
| SBP (mmHg) | 128.5 ± 15.3 | 129.1 ± 15.9 | 127.7 ± 14.7 | 0.597 |
| DBP (mmHg) | 77.9 ± 10 | 77.5 ± 9.4 | 78.4 ± 10.7 | 0.872 |
| HR (bpm) | 70 ± 11.9 | 70.4 ± 12.4 | 70.2 ± 11.3 | 0.919 |
| Rhythm Sinus Rhythm n (%) Non-Sinus Rhythm n (%) Pacemaker n (%) Atrial fibrillation n (%) | 77 (61.6) 43 (34.4) 2 (1.6) 3 (2.4) | 40 (58.8%) 25 (36.8%) - 3 (4.4%) | 37 (64.9%) 18 (31.6%) 2 (3.5%) - | 0.149 |
| TTE baseline parameters | ||||
| LVEF (%) | 62.0 (59.0–65.0) | 62.0 (59.0–65.0) | 62.00 (59.0–65.0) | 0.661 |
| LA Volume Index (mL/m2) | 25.6 ± 9.8 | 24.6 ± 9.1 | 26.8 ± 10.5 | 0.347 |
| LVIVS (mm) | 9.8 ± 1.6 | 9.8 ± 1.7 | 9.9 ± 1.4 | 0.749 |
| LVPW (mm) | 9.3 ± 1.3 | 9.5 ± 1.3 | 9.4 ± 1.1 | 0.692 |
| LVEDV (mL) | 92.2 ± 26.8 | 88.7 ± 22.3 | 94.9 ± 30.4 | 0.228 |
| LVESV (mL) | 36.2 ± 12.2 | 35.2 ± 10.8 | 37.1 ± 13.8 | 0.413 |
| E-Wave (m/s) | 0.6 ± 0.17 | 0.66 ± 0.2 | 0.61 ± 0.2 | 0.117 |
| A-Wave (m/s) | 0.62 ± 0.2 | 0.63 ± 0.2 | 0.63 ± 0.2 | 0.944 |
| E/A Ratio | 1.1 ± 0.5 | 1.1 ± 0.5 | 1.1 ± 0.4 | 0.304 |
| E/e’ medial | 8.0 (6.3–10.0) | 8.33 (6.7–11.1) | 7.69 (6.3–8.7) | 0.0.08 |
| E/e’ lateral | 6.2 (5–7.9) | 6.5 (5.0–8.6) | 5.8 (5.0–7.1) | 0.042 |
| RVSP (mmHg) | 26.0 (23–30.5) | 27.0 (23.0–32.0) | 26.0 (23.0–28.0) | 0.169 |
| TAPSE | 20.0 (18.0–23.0) | 20.0 (18.0–23.0) | 20.5 (19.0–23.0) | 0.126 |
| S wave | 0.12 (0.11–0.14) | 0.13 (0.10–0.14) | 0.12 (0.10–0.14) | 0.360 |
| RV strain | −19.6 ± 3.9 | −19.4 ± 4.2 | −19.9 ± 3.8 | 0.525 |
| HSTs Target altitude | ||||
| Target Altitude, ft (mean) | 8236.8 ± 1252.5 | 8260.29 ± 1479.2 | 8208.77 ± 924.3 | 0.813 |
| Target Altitude, n (%) More than 8000 ft 8000 ft Less than 8000 ft | 15 (12.0%) 100 (80.0%) 10 (8.0%) | 6 (8.8%) 55 (80.9%) 7 (10.3%) | 9 (15.8%) 45 (78.9%) 3 (5.3%) | 0.325 |
| Baseline n = 125 | Hypoxia n = 125 | p-Value | |
|---|---|---|---|
| Sat O2 (%) | 97 (95–98) | 88 (82–92) | <0.001 |
| RVSP (mmHg) | 26 (23–30.5) | 29 (25–36.5) | <0.001 |
| TAPSE (mm) | 20 (18–23) | 20 (19–24) | 0.7 |
| S wave (cm/s) | 0.12 (0.11–0.14) | 0.13 (0.12–0.14) | 0.2 |
| RV strain (%) | −19.6 ± 3.99 | −17.37 ± 4.17 | <0.01 |
| Shunt presence | 57 (45.6%) | 66 (52.8%) | <0.01 |
| Shunt grade | |||
| Intrapulmonary Intracardiac
| 6 (10.5%) 51 (89.5%) 40 (78.4%) 5 (9.8%) 6 (11.8%) | 7 (12.3%) 59 (89.4%) 46 (78%) 7 (11.8%) 6 (10.2%) | <0.01 |
| Hypoxia | |||
|---|---|---|---|
| No Shunt n = 59 (47.2%) | Shunt * n = 66 (52.8%) | p-Value | |
| Sat O2 (%) | 89 (83–93) | 87 (81–91) | 0.177 |
| RVSP (mmHg) | 30 (24–39) | 29 (26–34) | 0.860 |
| TAPSE (mm) | 20 (18–22) | 21 (19–24) | 0.159 |
| S wave (cm/s) | 13.1 (11–14.2) | 13.2 (12.4–15.1) | 0.302 |
| RV strain (%) | −17.25 ± 3.6 | −17.48 ± 4.62 | 0.672 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Villa Etchegoyen, C.; Wraith, R.E.; Brown, L.S.; Breznak, K.K.; Mital, R.; Lester, S.J.; Ayoub, C.; Alsidawi, S.; Shipman, J.N.; Farina, J.M.; et al. Use of Echocardiography Under Hypoxic Stress Without Exercise to Assess Right to Left Shunting. J. Cardiovasc. Dev. Dis. 2025, 12, 435. https://doi.org/10.3390/jcdd12110435
Villa Etchegoyen C, Wraith RE, Brown LS, Breznak KK, Mital R, Lester SJ, Ayoub C, Alsidawi S, Shipman JN, Farina JM, et al. Use of Echocardiography Under Hypoxic Stress Without Exercise to Assess Right to Left Shunting. Journal of Cardiovascular Development and Disease. 2025; 12(11):435. https://doi.org/10.3390/jcdd12110435
Chicago/Turabian StyleVilla Etchegoyen, Cecilia, Rachel E. Wraith, Lisa S. Brown, Karen K. Breznak, Rohit Mital, Steven J. Lester, Chadi Ayoub, Said Alsidawi, Justin N. Shipman, Juan M. Farina, and et al. 2025. "Use of Echocardiography Under Hypoxic Stress Without Exercise to Assess Right to Left Shunting" Journal of Cardiovascular Development and Disease 12, no. 11: 435. https://doi.org/10.3390/jcdd12110435
APA StyleVilla Etchegoyen, C., Wraith, R. E., Brown, L. S., Breznak, K. K., Mital, R., Lester, S. J., Ayoub, C., Alsidawi, S., Shipman, J. N., Farina, J. M., Arsanjani, R., & Stepanek, J. (2025). Use of Echocardiography Under Hypoxic Stress Without Exercise to Assess Right to Left Shunting. Journal of Cardiovascular Development and Disease, 12(11), 435. https://doi.org/10.3390/jcdd12110435






