The Influence of Age and Exercise Training Status on Left Ventricular Systolic Twist Mechanics in Healthy Males—An Exploratory Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Overview and Participants
2.2. Protocol and Experimental Procedures
2.2.1. Echocardiography
2.2.2. Left Ventricular Twist Mechanics
2.3. Statistical Analysis
3. Results
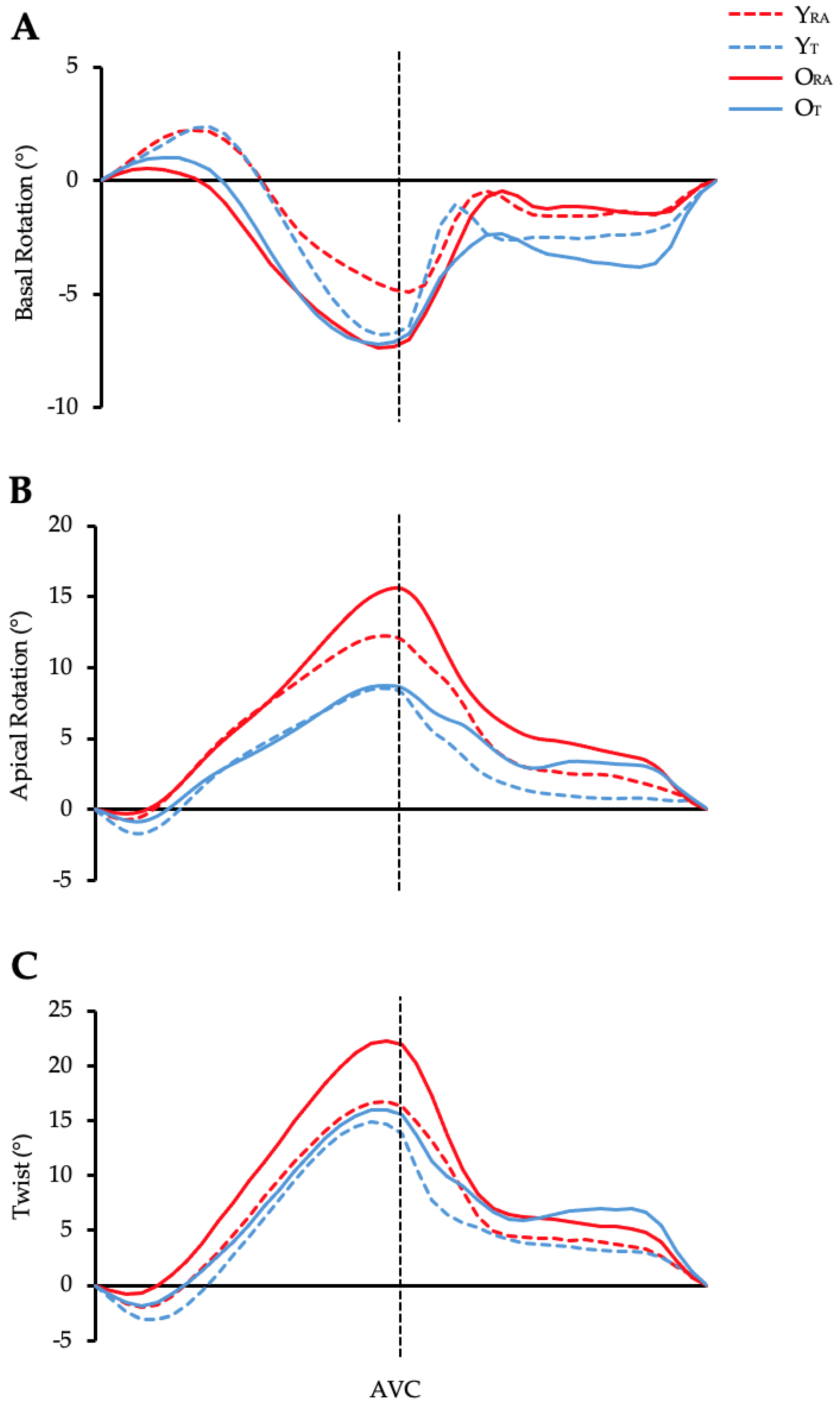
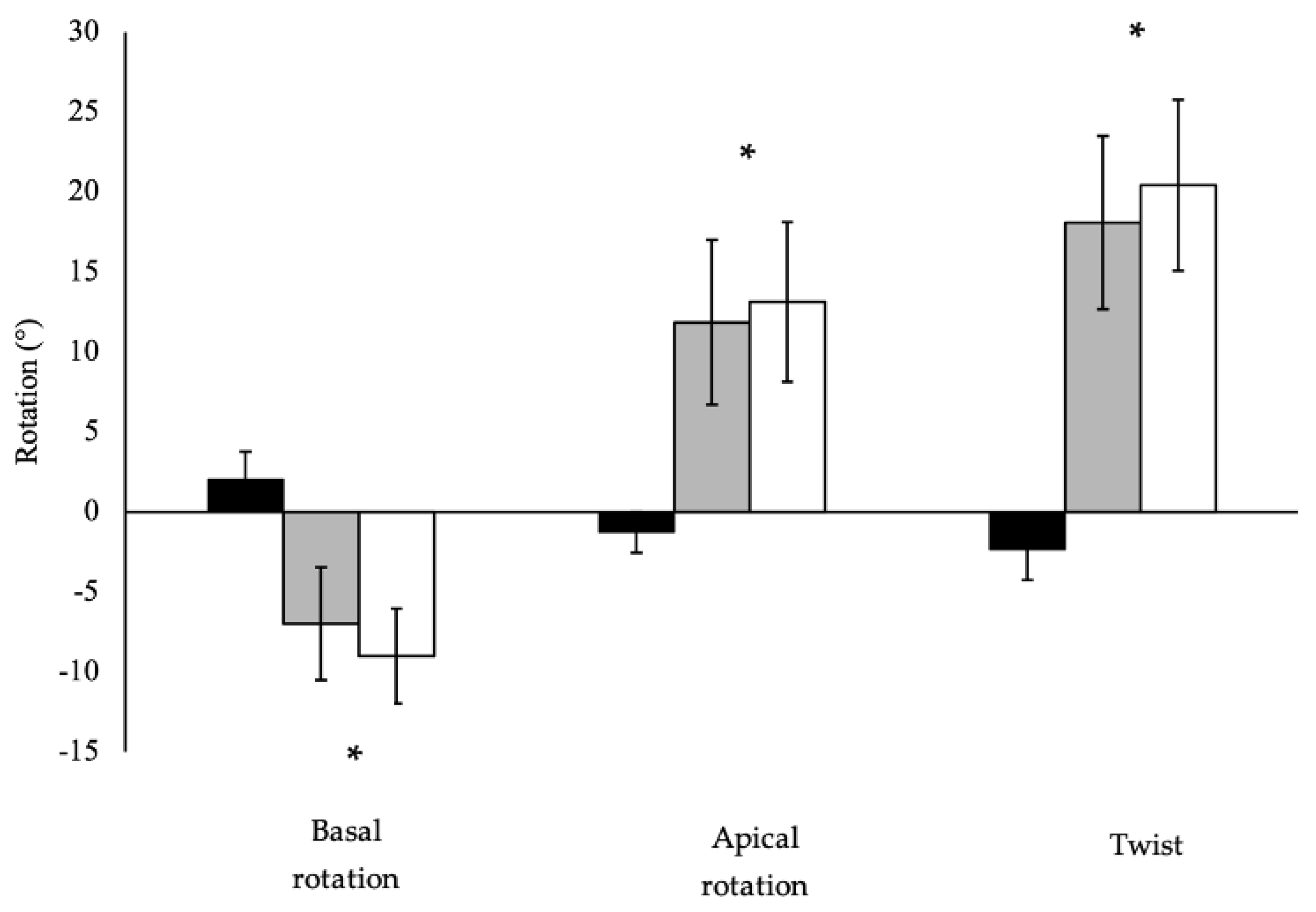
3.1. Left Ventricular Basal Rotation
3.2. Left Ventricular Apical Rotation
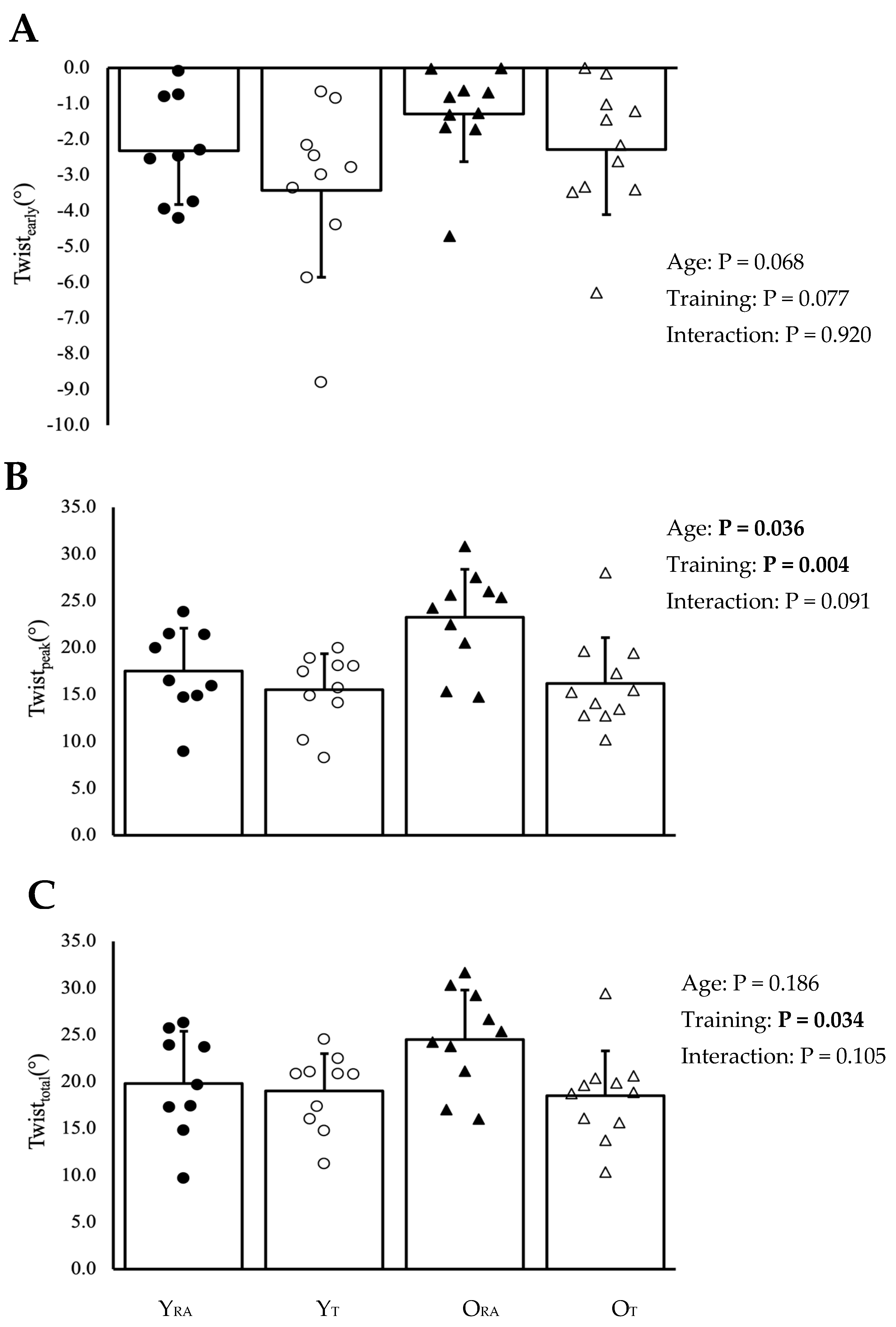
3.3. Left Ventricular Twist
4. Discussion
4.1. Age-Related Differences in LV Twist
4.2. LV Twist and Exercise Training Status
4.3. Temporal LV Systolic Twist
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chiao, Y.A.; Rabinovitch, P.S. The Aging Heart. Cold Spring Harb. Perspect. Med. 2015, 5, a025148. [Google Scholar] [CrossRef] [PubMed]
- Paneni, F.; Cañestro, C.D.; Libby, P.; Lüscher, T.F.; Camici, G.G. The Aging Cardiovascular System: Understanding It at the Cellular and Clinical Levels. J. Am. Coll. Cardiol. 2017, 69, 1952–1967. [Google Scholar] [CrossRef] [PubMed]
- Lower, R. Tractatus de Corde; Oxford University Press: London, UK, 1669; Volume 9. [Google Scholar]
- Mor-Avi, V.; Lang, R.M.; Badano, L.P.; Belohlavek, M.; Cardim, N.M.; Derumeaux, G.; Galderisi, M.; Marwick, T.; Nagueh, S.F.; Sengupta, P.P.; et al. Current and Evolving Echocardiographic Techniques for the Quantitative Evaluation of Cardiac Mechanics: ASE/EAE Consensus Statement on Methodology and Indications Endorsed by the Japanese Society of Echocardiography. Eur. J. Echocardiogr. 2011, 12, 167–205. [Google Scholar] [CrossRef]
- Nakatani, S. Left Ventricular Rotation and Twist: Why Should We Learn? J. Cardiovasc. Ultrasound 2011, 19, 1–6. [Google Scholar] [CrossRef]
- Bansal, M.; Kasliwal, R.R. How Do I Do It? Speckle-Tracking Echocardiography. Indian Heart J. 2013, 65, 117–123. [Google Scholar] [CrossRef]
- Sun, J.P.; Lam, Y.-Y.; Wu, C.-Q.; Yang, X.S.; Guo, R.; Kwong, J.S.W.; Merlino, J.D.; Yu, C.-M. Effect of Age and Gender on Left Ventricular Rotation and Twist in a Large Group of Normal Adults—A Multicenter Study. Int. J. Cardiol. 2013, 167, 2215–2221. [Google Scholar] [CrossRef]
- Kaku, K.; Takeuchi, M.; Tsang, W.; Takigiku, K.; Yasukochi, S.; Patel, A.R.; Mor-Avi, V.; Lang, R.M.; Otsuji, Y. Age-Related Normal Range of Left Ventricular Strain and Torsion Using Three-Dimensional Speckle-Tracking Echocardiography. J. Am. Soc. Echocardiogr. Off. Publ. Am. Soc. Echocardiogr. 2014, 27, 55–64. [Google Scholar] [CrossRef]
- Kocabay, G.; Muraru, D.; Peluso, D.; Cucchini, U.; Mihaila, S.; Padayattil-Jose, S.; Gentian, D.; Iliceto, S.; Vinereanu, D.; Badano, L.P. Normal Left Ventricular Mechanics by Two-Dimensional Speckle-Tracking Echocardiography. Reference Values in Healthy Adults. Rev. Espanola Cardiol. Engl. Ed. 2014, 67, 651–658. [Google Scholar] [CrossRef]
- Maufrais, C.; Schuster, I.; Doucende, G.; Vitiello, D.; Rupp, T.; Dauzat, M.; Obert, P.; Nottin, S. Endurance Training Minimizes Age-Related Changes of Left Ventricular Twist-Untwist Mechanics. J. Am. Soc. Echocardiogr. Off. Publ. Am. Soc. Echocardiogr. 2014, 27, 1208–1215. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhou, Q.; Pu, D.; Zou, L.; Tan, Y. Differences in Left Ventricular Twist Related to Age: Speckle Tracking Echocardiographic Data for Healthy Volunteers from Neonate to Age 70 Years. Echocardiogr. Mt. Kisco N 2010, 27, 1205–1210. [Google Scholar] [CrossRef]
- Tavakoli, V.; Sahba, N. Assessment of Age-Related Changes in Left Ventricular Twist by 3-Dimensional Speckle-Tracking Echocardiography. J. Ultrasound Med. 2013, 32, 1435–1441. [Google Scholar] [CrossRef] [PubMed]
- Stöhr, E.J.; Shave, R.E.; Baggish, A.L.; Weiner, R.B. Left Ventricular Twist Mechanics in the Context of Normal Physiology and Cardiovascular Disease: A Review of Studies Using Speckle Tracking Echocardiography. Am. J. Physiol. Heart Circ. Physiol. 2016, 311, H633–H644. [Google Scholar] [CrossRef] [PubMed]
- Gibson-Moore, H. UK Chief Medical Officers’ physical activity guidelines 2019: What’s new and how can we get people more active? Nutr. Bull. 2019, 44, 320–328. [Google Scholar] [CrossRef]
- Myers, J.; Prakash, M.; Froelicher, V.; Do, D.; Partington, S.; Atwood, J.E. Exercise Capacity and Mortality among Men Referred for Exercise Testing. N. Engl. J. Med. 2002, 346, 793–801. [Google Scholar] [CrossRef]
- Beaumont, A.J.; Grace, F.M.; Richards, J.C.; Campbell, A.K.; Sculthorpe, N.F. Aerobic Training Protects Cardiac Function During Advancing Age: A Meta-Analysis of Four Decades of Controlled Studies. Sports Med. 2018, 49, 199–219. [Google Scholar] [CrossRef] [PubMed]
- Howden, E.J.; Sarma, S.; Lawley, J.S.; Opondo, M.; Cornwell, W.; Stoller, D.; Urey, M.A.; Adams-Huet, B.; Levine, B.D. Reversing the Cardiac Effects of Sedentary Aging in Middle Age—A Randomized Controlled Trial: Implications For Heart Failure Prevention. Circulation 2018, 137, 1549–1560. [Google Scholar] [CrossRef]
- Santoro, A.; Alvino, F.; Antonelli, G.; Cassano, F.E.; De Vito, R.; Cameli, M.; Mondillo, S. Age Related Diastolic Function in Amateur Athletes. Int. J. Cardiovasc. Imaging 2015, 31, 567–573. [Google Scholar] [CrossRef]
- Maufrais, C.; Doucende, G.; Rupp, T.; Dauzat, M.; Obert, P.; Nottin, S.; Schuster, I. Left Ventricles of Aging Athletes: Better Untwisters but Not More Relaxed during Exercise. Clin. Res. Cardiol. 2017, 106, 884–892. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.S.; Mariani, J.A.; Sasson, Z.; Goodman, J.M. Exercise with a Twist: Left Ventricular Twist and Recoil in Healthy Young and Middle-Aged Men, and Middle-Aged Endurance-Trained Men. J. Am. Soc. Echocardiogr. Off. Publ. Am. Soc. Echocardiogr. 2012, 25, 986–993. [Google Scholar] [CrossRef]
- Sengupta, P.P.; Khandheria, B.K.; Korinek, J.; Wang, J.; Jahangir, A.; Seward, J.B.; Belohlavek, M. Apex-to-Base Dispersion in Regional Timing of Left Ventricular Shortening and Lengthening. J. Am. Coll. Cardiol. 2006, 47, 163–172. [Google Scholar] [CrossRef]
- Sengupta, P.P.; Tajik, A.J.; Chandrasekaran, K.; Khandheria, B.K. Twist Mechanics of the Left Ventricle: Principles and Application. JACC Cardiovasc. Imaging 2008, 1, 366–376. [Google Scholar] [CrossRef] [PubMed]
- Ashikaga, H.; van der Spoel, T.I.G.; Coppola, B.A.; Omens, J.H. Transmural Myocardial Mechanics during Isovolumic Contraction. JACC Cardiovasc. Imaging 2009, 2, 202–211. [Google Scholar] [CrossRef] [PubMed]
- Sengupta, P.P.; Korinek, J.; Belohlavek, M.; Narula, J.; Vannan, M.A.; Jahangir, A.; Khandheria, B.K. Left Ventricular Structure and Function: Basic Science for Cardiac Imaging. J. Am. Coll. Cardiol. 2006, 48, 1988–2001. [Google Scholar] [CrossRef] [PubMed]
- Sabatino, J.; Castaldi, B.; Di Salvo, G. How to Measure Left Ventricular Twist by Two-Dimensional Speckle-Tracking Analysis. Eur. Heart J. Cardiovasc. Imaging 2021, 22, 961–963. [Google Scholar] [CrossRef]
- Kim, H.-K.; Sohn, D.-W.; Lee, S.-E.; Choi, S.-Y.; Park, J.-S.; Kim, Y.-J.; Oh, B.-H.; Park, Y.-B.; Choi, Y.-S. Assessment of Left Ventricular Rotation and Torsion with Two-Dimensional Speckle Tracking Echocardiography. J. Am. Soc. Echocardiogr. 2007, 20, 45–53. [Google Scholar] [CrossRef] [PubMed]
- van Dalen, B.M.; Soliman, O.I.I.; Vletter, W.B.; ten Cate, F.J.; Geleijnse, M.L. Age-Related Changes in the Biomechanics of Left Ventricular Twist Measured by Speckle Tracking Echocardiography. Am. J. Physiol.-Heart Circ. Physiol. 2008, 295, H1705–H1711. [Google Scholar] [CrossRef]
- Takeuchi, M.; Otsuji, Y.; Lang, R.M. Evaluation of Left Ventricular Function Using Left Ventricular Twist and Torsion Parameters. Curr. Cardiol. Rep. 2009, 11, 225–230. [Google Scholar] [CrossRef]
- Johnson, C.; Forsythe, L.; Somauroo, J.; Papadakis, M.; George, K.; Oxborough, D. Cardiac Structure and Function in Elite Native Hawaiian and Pacific Islander Rugby Football League Athletes: An Exploratory Study. Int. J. Cardiovasc. Imaging 2018, 34, 725–734. [Google Scholar] [CrossRef]
- Beaumont, A.; Campbell, A.; Unnithan, V.; Grace, F.; Knox, A.; Sculthorpe, N. Long-Term Athletic Training Does Not Alter Age-Associated Reductions of Left-Ventricular Mid-Diastolic Lengthening or Expansion at Rest. Eur. J. Appl. Physiol. 2020, 120, 2059–2073. [Google Scholar] [CrossRef]
- Aksakal, E.; Kurt, M.; Ozturk, M.E.; Tanboga, I.H.; Kaya, A.; Nacar, T.; Sevimli, S.; Gurlertop, Y. The Effect of Incremental Endurance Exercise Training on Left Ventricular Mechanics: A Prospective Observational Deformation Imaging Study. Anadolu Kardiyol. Derg. Anatol. J. Cardiol. 2013, 13, 432. [Google Scholar] [CrossRef][Green Version]
- Donal, E.; Rozoy, T.; Kervio, G.; Schnell, F.; Mabo, P.; Carré, F. Comparison of the Heart Function Adaptation in Trained and Sedentary Men After 50 and Before 35 Years of Age. Am. J. Cardiol. 2011, 108, 1029–1037. [Google Scholar] [CrossRef] [PubMed]
- Matelot, D.; Schnell, F.; Kervio, G.; Ridard, C.; Thillaye du Boullay, N.; Wilson, M.; Carre, F. Cardiovascular Benefits of Endurance Training in Seniors: 40 Is Not Too Late to Start. Int. J. Sports Med. 2016, 37, 625–632. [Google Scholar] [CrossRef] [PubMed]
- Fujimoto, N.; Prasad, A.; Hastings, J.L.; Arbab-Zadeh, A.; Bhella, P.S.; Shibata, S.; Palmer, D.; Levine, B.D. Cardiovascular Effects of 1 Year of Progressive and Vigorous Exercise Training in Previously Sedentary Individuals Older than 65 Years of Age. Circulation 2010, 122, 1797–1805. [Google Scholar] [CrossRef] [PubMed]
- van Dalen, B.M.; Vletter, W.B.; Soliman, O.I.I.; ten Cate, F.J.; Geleijnse, M.L. Importance of Transducer Position in the Assessment of Apical Rotation by Speckle Tracking Echocardiography. J. Am. Soc. Echocardiogr. 2008, 21, 895–898. [Google Scholar] [CrossRef]
- van Dalen, B.M.; Soliman, O.I.I.; Kauer, F.; Vletter, W.B.; van der Zwaan, H.B.; Cate, F.J.T.; Geleijnse, M.L. Alterations in Left Ventricular Untwisting with Ageing. Circ. J. Off. J. Jpn. Circ. Soc. 2010, 74, 101–108. [Google Scholar] [CrossRef]
- Stöhr, E.J.; González-Alonso, J.; Pearson, J.; Low, D.A.; Ali, L.; Barker, H.; Shave, R. Effects of Graded Heat Stress on Global Left Ventricular Function and Twist Mechanics at Rest and during Exercise in Healthy Humans. Exp. Physiol. 2011, 96, 114–124. [Google Scholar] [CrossRef]
- Oxborough, D.; George, K.; Birch, K.M. Intraobserver Reliability of Two-Dimensional Ultrasound Derived Strain Imaging in the Assessment of the Left Ventricle, Right Ventricle, and Left Atrium of Healthy Human Hearts. Echocardiogr. Mt. Kisco N 2012, 29, 793–802. [Google Scholar] [CrossRef]
- The Jamovi Project Jamovi. Available online: https://www.jamovi.org (accessed on 1 August 2024).
- Lumens, J.; Delhaas, T.; Arts, T.; Cowan, B.R.; Young, A.A. Impaired Subendocardial Contractile Myofiber Function in Asymptomatic Aged Humans, as Detected Using MRI. Am. J. Physiol. Heart Circ. Physiol. 2006, 291, H1573–H1579. [Google Scholar] [CrossRef]
- Mitchell, J.H.; Haskell, W.; Snell, P.; Van Camp, S.P. Task Force 8: Classification of Sports. J. Am. Coll. Cardiol. 2005, 45, 1364–1367. [Google Scholar] [CrossRef]
- Beaumont, A.; Grace, F.; Richards, J.; Hough, J.; Oxborough, D.; Sculthorpe, N. Left Ventricular Speckle Tracking-Derived Cardiac Strain and Cardiac Twist Mechanics in Athletes: A Systematic Review and Meta-Analysis of Controlled Studies. Sports Med. 2016, 47, 1145–1170. [Google Scholar] [CrossRef]
- Forsythe, L.; MacIver, D.H.; Johnson, C.; George, K.; Somauroo, J.; Papadakis, M.; Brown, B.; Qasem, M.; Oxborough, D. The Relationship between Left Ventricular Structure and Function in the Elite Rugby Football League Athlete as Determined by Conventional Echocardiography and Myocardial Strain Imaging. Int. J. Cardiol. 2018, 261, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Nottin, S.; Doucende, G.; Schuster-Beck, I.; Dauzat, M.; Obert, P. Alteration in Left Ventricular Normal and Shear Strains Evaluated by 2D-Strain Echocardiography in the Athlete’s Heart: Left Ventricular Regional Strains in Athletes. J. Physiol. 2008, 586, 4721–4733. [Google Scholar] [CrossRef] [PubMed]
- Weiner, R.B.; DeLuca, J.R.; Wang, F.; Lin, J.; Wasfy, M.M.; Berkstresser, B.; Stöhr, E.; Shave, R.; Lewis, G.D.; Hutter, A.M.; et al. Exercise-Induced Left Ventricular Remodeling Among Competitive Athletes A Phasic Phenomenon. Circ. Cardiovasc. Imaging 2015, 8, e003651. [Google Scholar] [CrossRef] [PubMed]
- Stöhr, E.J.; McDonnell, B.; Thompson, J.; Stone, K.; Bull, T.; Houston, R.; Cockcroft, J.; Shave, R. Left Ventricular Mechanics in Humans with High Aerobic Fitness: Adaptation Independent of Structural Remodelling, Arterial Haemodynamics and Heart Rate. J. Physiol. 2012, 590, 2107–2119. [Google Scholar] [CrossRef] [PubMed]
- Taber, L.A.; Yang, M.; Podszus, W.W. Mechanics of Ventricular Torsion. J. Biomech. 1996, 29, 745–752. [Google Scholar] [CrossRef]
- van Dalen, B.M.; Kauer, F.; Vletter, W.B.; Soliman, O.I.I.; van der Zwaan, H.B.; ten Cate, F.J.; Geleijnse, M.L. Influence of Cardiac Shape on Left Ventricular Twist. J. Appl. Physiol. 2009, 108, 146–151. [Google Scholar] [CrossRef]
- Notomi, Y.; Popovic, Z.B.; Yamada, H.; Wallick, D.W.; Martin, M.G.; Oryszak, S.J.; Shiota, T.; Greenberg, N.L.; Thomas, J.D. Ventricular Untwisting: A Temporal Link between Left Ventricular Relaxation and Suction. Am. J. Physiol. Heart Circ. Physiol. 2008, 294, H505–H513. [Google Scholar] [CrossRef]
- Oxborough, D.; Heemels, A.; Somauroo, J.; McClean, G.; Mistry, P.; Lord, R.; Utomi, V.; Jones, N.; Thijssen, D.; Sharma, S.; et al. Left and Right Ventricular Longitudinal Strain-Volume/Area Relationships in Elite Athletes. Int. J. Cardiovasc. Imaging 2016, 32, 1199–1211. [Google Scholar] [CrossRef]
- Park, C.M.; March, K.; Williams, S.; Kukadia, S.; Ghosh, A.K.; Jones, S.; Tillin, T.; Chaturvedi, N.; Hughes, A.D. Feasibility and Reproducibility of Left Ventricular Rotation by Speckle Tracking Echocardiography in Elderly Individuals and the Impact of Different Software. PLoS ONE 2013, 8, e75098. [Google Scholar] [CrossRef]
- Hung, C.-L.; Gonçalves, A.; Shah, A.M.; Cheng, S.; Kitzman, D.; Solomon, S.D. Age- and Sex-Related Influences on Left Ventricular Mechanics in Elderly Individuals Free of Prevalent Heart FailureCLINICAL PERSPECTIVE. Circ. Cardiovasc. Imaging 2017, 10, e004510. [Google Scholar] [CrossRef]
- Nio, A.Q.X.; Stöhr, E.J.; Shave, R.E. Age-Related Differences in Left Ventricular Structure and Function between Healthy Men and Women. Climacteric J. Int. Menopause Soc. 2017, 20, 476–483. [Google Scholar] [CrossRef] [PubMed]

| Young | Old | p-Value | |||||
|---|---|---|---|---|---|---|---|
| Recreationally Active (YRA) | Trained (YT) | Recreationally Active (ORA) | Trained (OT) | Age | Training | Interaction | |
| Basalearly rotation (°) | 2.6 ± 2.0 | 2.7 ± 2.1 | 1.2 ± 1.1 | 1.6 ± 1.6 | 0.025 | 0.679 | 0.742 |
| Basalpeak rotation (°) | −5.4 ± 2.7 | −7.0 ± 2.5 | −7.6 ± 3.0 | −7.7 ± 4.3 | 0.164 | 0.421 | 0.482 |
| Basaltotal rotation (°) | −8.1 ± 2.8 | −9.7 ± 1.9 | −8.8 ± 3.5 | −9.3 ± 3.5 | 0.841 | 0.273 | 0.568 |
| Normalised basal rotation (°/cm) | −0.6 ± 0.3 | −0.7 ± 0.3 | −0.9 ± 0.4 | −0.9 ± 0.5 | 0.094 | 0.564 | 0.560 |
| Apicalearly rotation (°) | −0.9 ± 0.7 | −2.0 ± 1.4 | −0.9 ± 1.5 | −1.3 ± 1.2 | 0.379 | 0.069 | 0.393 |
| Apicalpeak rotation (°) | 12.6 ± 3.9 | 9.5 ± 3.0 | 16.3 ± 6.1 | 9.3 ± 4.0 | 0.206 | <0.001 | 0.173 |
| Apicaltotal rotation (°) | 13.5 ± 3.9 | 11.5 ± 2.9 | 17.2 ± 6.2 | 10.6 ± 4.0 | 0.310 | 0.004 | 0.112 |
| Normalised apical rotation (°/cm) | 1.4 ± 0.4 | 1.0 ± 0.3 | 1.9 ± 0.7 | 1.0 ± 0.5 | 0.105 | <0.001 | 0.201 |
| Torsion (°/cm) | 1.9 ± 0.5 | 1.6 ± 0.4 | 2.6 ± 0.6 | 1.8 ± 0.5 | 0.009 | 0.001 | 0.119 |
| Young | Old | p-Value | |||||
|---|---|---|---|---|---|---|---|
| Recreationally Active (YRA) | Trained (YT) | Recreationally Active (ORA) | Trained (OT) | Age | Training | Interaction | |
| Time to basalearly rotation (ms) | 272 ± 77 | 295 ± 103 | 263 ± 99 | 281 ± 125 | 0.720 | 0.534 | 0.942 |
| Time to basalpeak rotation (ms) | 348 ± 50 | 343 ± 37 | 362 ± 73 | 369 ± 48 | 0.251 | 0.937 | 0.731 |
| Time to apicalearly rotation (ms) | 215 ± 76 | 247 ± 107 | 230 ± 83 | 260 ± 93 | 0.635 | 0.295 | 0.980 |
| Time to apicalpeak rotation (ms) | 363 ± 36 | 385 ± 71 | 397 ± 48 | 397 ± 60 | 0.204 | 0.545 | 0.563 |
| Time displacement (ms) | −16 ± 52 | −42 ± 60 | −35 ± 66 | −28 ± 77 | 0.882 | 0.648 | 0.435 |
| Time to twistearly (ms) | 233 ± 72 | 260 ± 112 | 242 ± 86 | 261 ± 96 | 0.865 | 0.446 | 0.890 |
| Time to twistpeak (ms) | 350 ± 41 | 355 ± 34 | 389 ± 42 | 374 ± 31 | 0.018 | 0.710 | 0.402 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beaumont, A.J.; Campbell, A.K.; Unnithan, V.B.; Oxborough, D.; Grace, F.; Knox, A.; Sculthorpe, N.F. The Influence of Age and Exercise Training Status on Left Ventricular Systolic Twist Mechanics in Healthy Males—An Exploratory Study. J. Cardiovasc. Dev. Dis. 2024, 11, 321. https://doi.org/10.3390/jcdd11100321
Beaumont AJ, Campbell AK, Unnithan VB, Oxborough D, Grace F, Knox A, Sculthorpe NF. The Influence of Age and Exercise Training Status on Left Ventricular Systolic Twist Mechanics in Healthy Males—An Exploratory Study. Journal of Cardiovascular Development and Disease. 2024; 11(10):321. https://doi.org/10.3390/jcdd11100321
Chicago/Turabian StyleBeaumont, Alexander J., Amy K. Campbell, Viswanath B. Unnithan, David Oxborough, Fergal Grace, Allan Knox, and Nicholas F. Sculthorpe. 2024. "The Influence of Age and Exercise Training Status on Left Ventricular Systolic Twist Mechanics in Healthy Males—An Exploratory Study" Journal of Cardiovascular Development and Disease 11, no. 10: 321. https://doi.org/10.3390/jcdd11100321
APA StyleBeaumont, A. J., Campbell, A. K., Unnithan, V. B., Oxborough, D., Grace, F., Knox, A., & Sculthorpe, N. F. (2024). The Influence of Age and Exercise Training Status on Left Ventricular Systolic Twist Mechanics in Healthy Males—An Exploratory Study. Journal of Cardiovascular Development and Disease, 11(10), 321. https://doi.org/10.3390/jcdd11100321






