An Individualized, Less-Invasive Surgical Approach Algorithm Improves Outcome in Elderly Patients Undergoing Mitral Valve Surgery
Abstract
1. Introduction
2. Methods
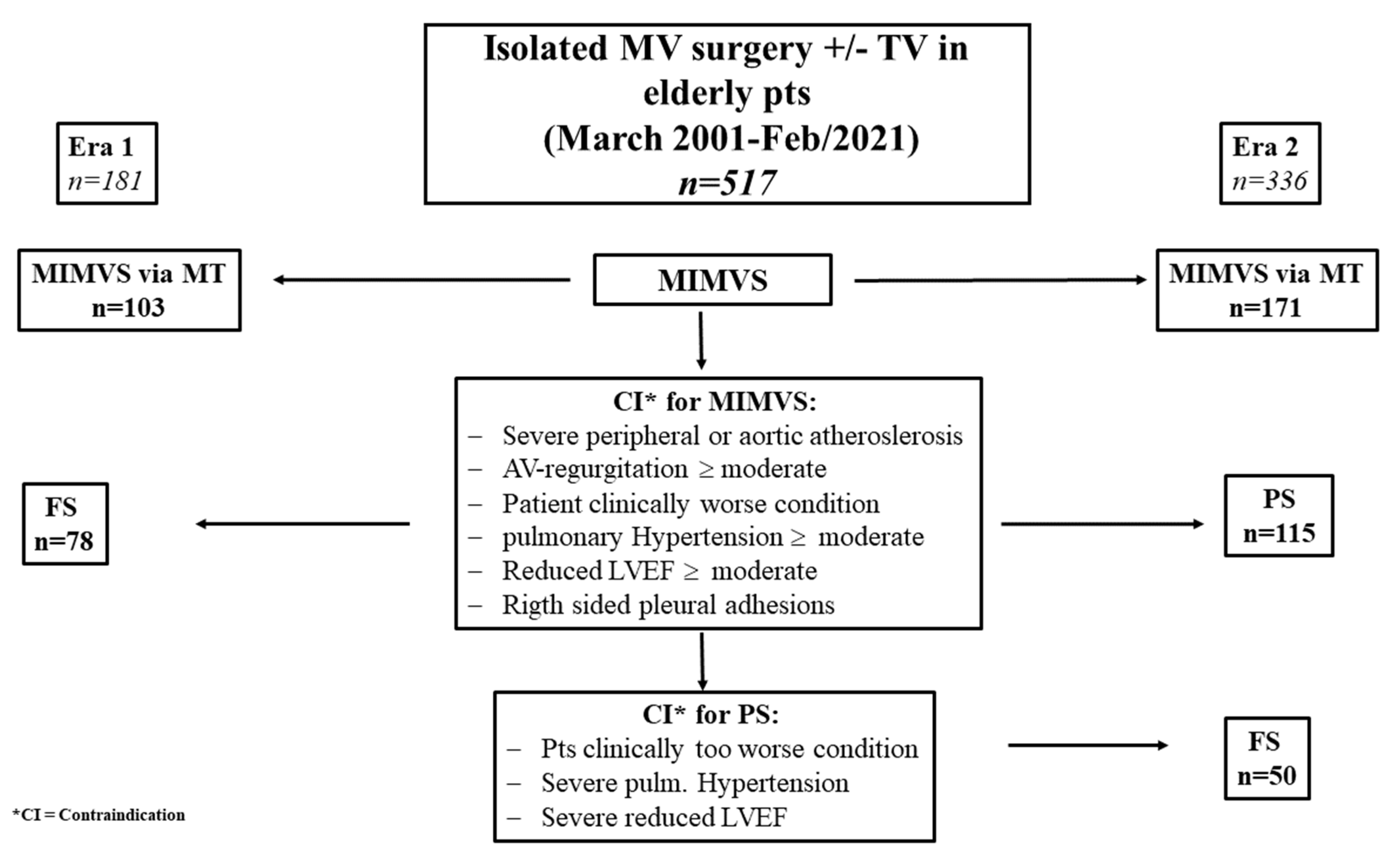
2.1. Study Design and Patients
2.2. Surgical Procedures
2.3. Definitions
3. Statistical Analysis
4. Results
4.1. Baseline Characteristics and Intraoperative Parameters
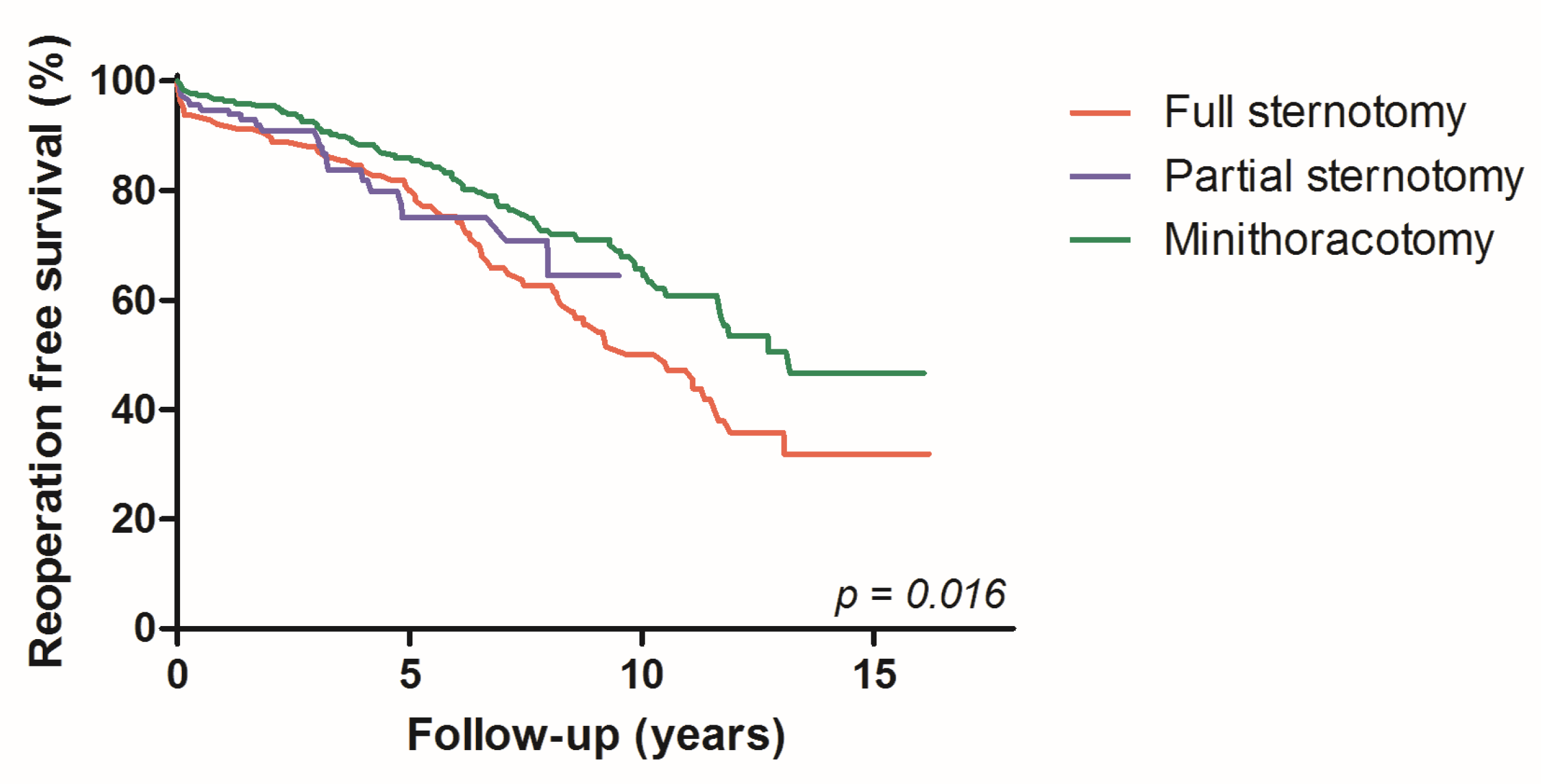
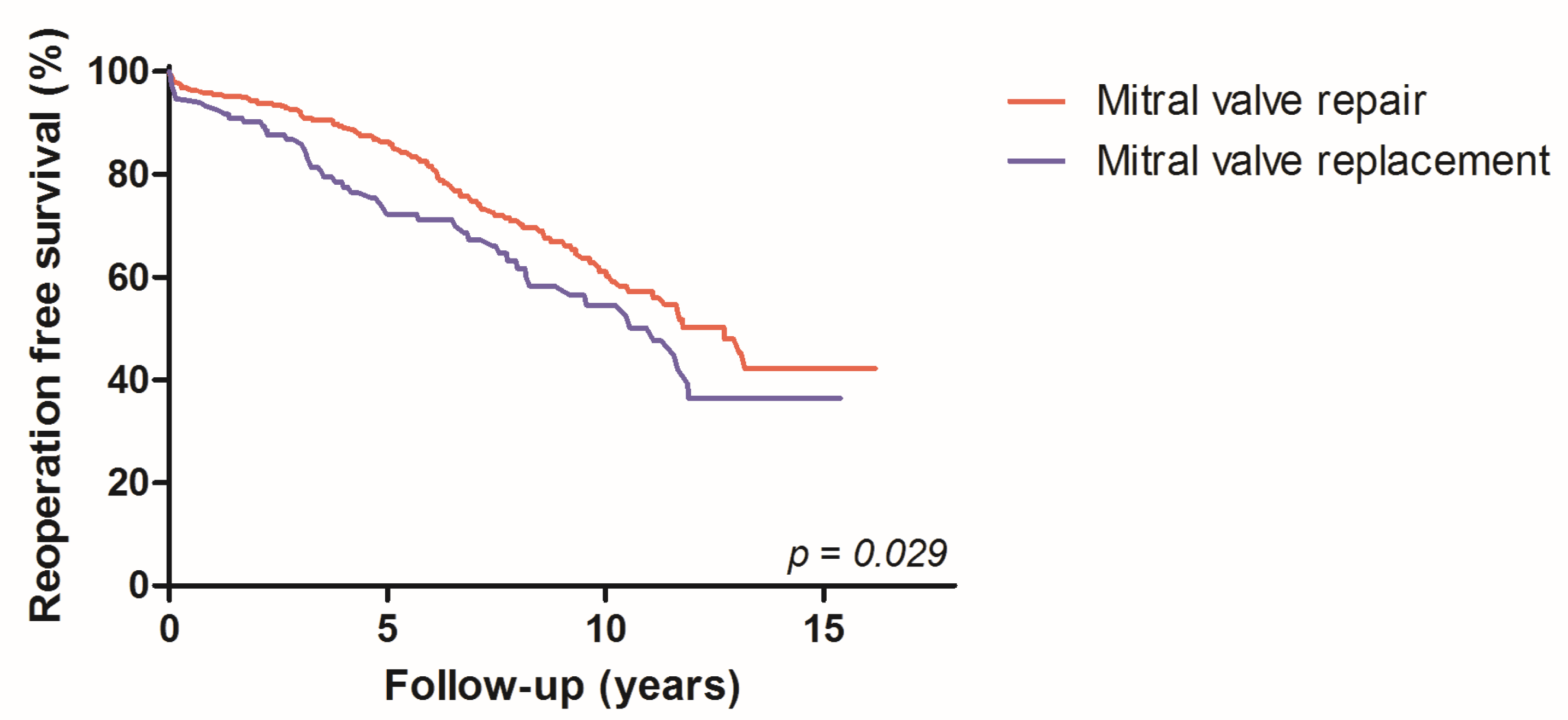
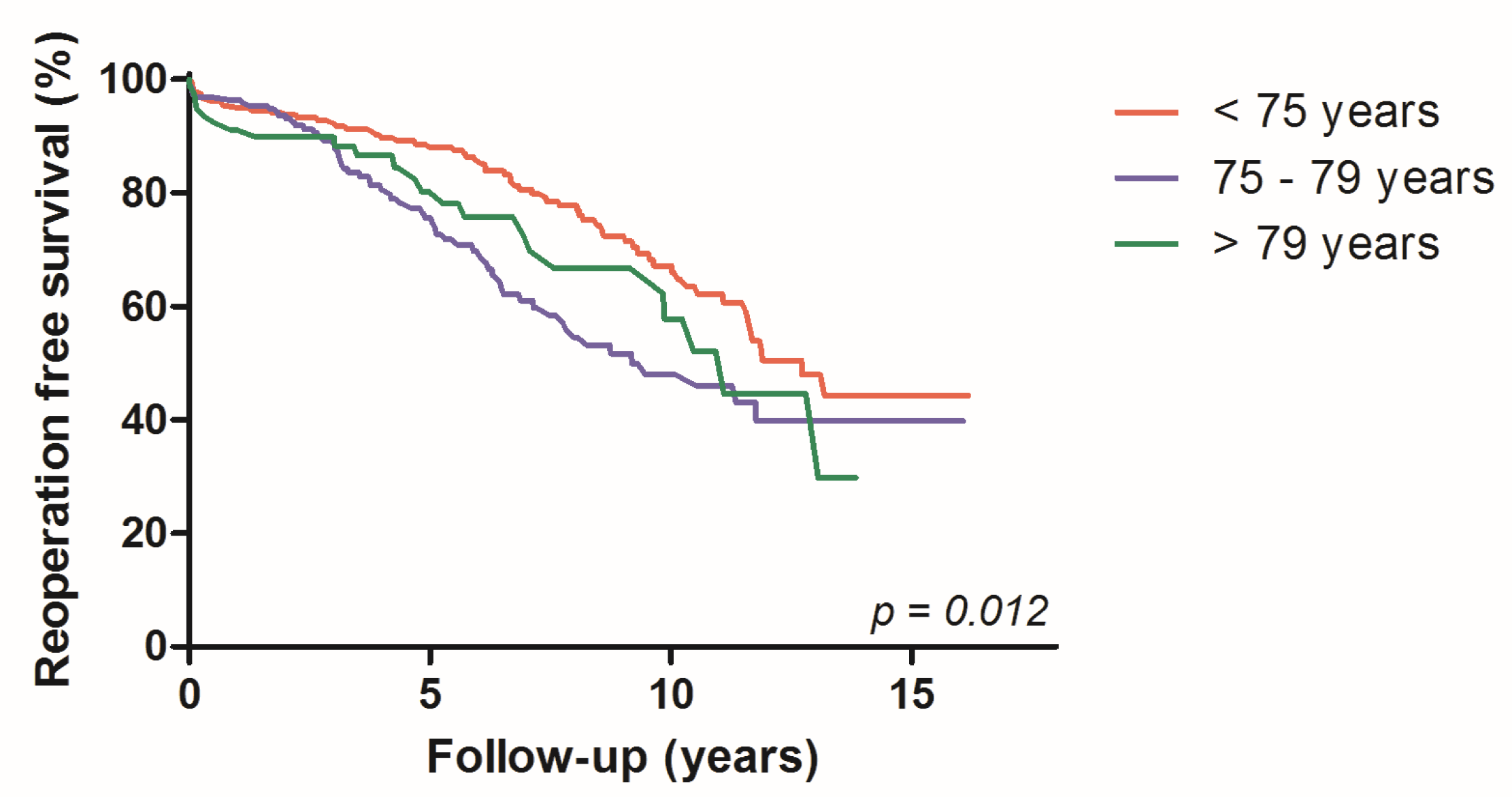
4.2. Long-Term Outcome
4.3. Operative and Perioperative Success
5. Discussion
Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nkomo, V.T.; Gardin, J.M.; Skelton, T.N.; Gottdiener, J.S.; Scott, C.G.; Enriquez-Sarano, M. Burden of valvular heart diseases: A population-based study. Lancet 2006, 368, 1005–1011. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, S.M.; Shahian, D.M.; Filardo, G.; Ferraris, V.A.; Haan, C.K.; Rich, J.B.; Normand, S.-L.T.; DeLong, E.R.; Shewan, C.M.; Dokholyan, R.S.; et al. The Society of Thoracic Surgeons 2008 cardiac surgery risk models: Part 2—Isolated valve surgery. Ann. Thorac. Surg. 2009, 88, S23–S42. [Google Scholar] [CrossRef] [PubMed]
- Grant, S.W.; Hickey, G.L.; Modi, P.; Hunter, S.; Akowuah, E.; Zacharias, J. Propensity-matched analysis of minimally invasive approach versus sternotomy for mitral valve surgery. Heart 2019, 105, 783–789. [Google Scholar] [CrossRef] [PubMed]
- Kang, D.H.; Heo, R.; Lee, S.; Baek, S.; Kim, D.-H.; Song, J.-M.; Song, J.-K.; Lee, J.W. Initial surgery versus conservative management of symptomatic severe mitral regurgitation in the elderly. Heart 2018, 104, 849–854. [Google Scholar] [CrossRef] [PubMed]
- Bonnet, V.; Boisselier, C.; Saplacan, V.; Belin, A.; Gérard, J.-L.; Fellahi, J.-L.; Hanouz, J.-L.; Fischer, M.-O. The role of age and comorbidities in postoperative outcome of mitral valve repair: A propensity-matched study. Medicine 2016, 95, e3938. [Google Scholar] [CrossRef]
- Seeburger, J.; Falk, V.; Garbade, J.; Noack, T.; Kiefer, P.; Vollroth, M.; Mohr, F.W.; Misfeld, M. Mitral valve surgical procedures in the elderly. Ann. Thorac. Surg. 2012, 94, 1999–2003. [Google Scholar] [CrossRef]
- Beckmann, A.; Meyer, R.; Lewandowski, J.; Markewitz, A.; Blassfeld, D.; Boning, A. German Heart Surgery Report 2021: The Annual Updated Registry of the German Society for Thoracic and Cardiovascular Surgery. Thorac. Cardiovasc. Surg. 2022, 70, 362–376. [Google Scholar] [CrossRef]
- Gotte, J.; Zittermann, A.; Hakim-Meibodi, K.; Hata, M.; Schramm, R.; Bleiziffer, S.; Parsa, M.A.; Gummert, J.; Renner, A. Long-Term Clinical Outcome in Elderly Patients Undergoing Mitral Valve Repair. Thorac. Cardiovasc. Surg. 2022, 70, 93–99. [Google Scholar] [CrossRef]
- Kawajiri, H.; Schaff, H.V.; Dearani, J.A.; Daly, R.C.; Greason, K.L.; Arghami, A.; Rowse, P.G.; Viehman, J.K.; Lahr, B.D.; Gallego-Navarro, C.; et al. Clinical Outcomes of Mitral Valve Repair for Degenerative Mitral Regurgitation in Elderly Patients. Eur. J. Cardiothorac. Surg. 2022, 62, ezac299. [Google Scholar] [CrossRef]
- Vollroth, M.; Seeburger, J.; Garbade, J.; Borger, M.A.; Misfeld, M.; Mohr, F.W. Conversion rate and contraindications for minimally invasive mitral valve surgery. Ann. Cardiothorac. Surg. 2013, 2, 853–854. [Google Scholar]
- Doenst, T.; Diab, M.; Sponholz, C.; Bauer, M.; Farber, G. The Opportunities and Limitations of Minimally Invasive Cardiac Surgery. Dtsch. Arztebl. Int. 2017, 114, 777–784. [Google Scholar] [CrossRef]
- Cetinkaya, A.; Geier, A.; Bramlage, K.; Hein, S.; Bramlage, P.; Schönburg, M.; Choi, Y.; Richter, M. Long-term results after mitral valve surgery using minimally invasive versus sternotomy approach: A propensity matched comparison of a large single-center series. BMC Cardiovasc. Disord. 2021, 21, 314. [Google Scholar] [CrossRef]
- Zacharias, J.; Perier, P. Seven Habits of Highly Effective Endoscopic Mitral Surgeons. Innovations 2020, 15, 11–16. [Google Scholar] [CrossRef]
- Oezpeker, U.C.; Barbieri, F.; Hoefer, D.; Bonaros, N.; Grimm, M.; Mueller, L. Partial Upper Sternotomy is a Safe Alternative in Mitral Annulus Decalcification. Semin. Thorac. Cardiovasc. Surg. 2022, 34, 502–509. [Google Scholar] [CrossRef]
- Hage, A.; Hage, F.; Al-Amodi, H.; Gupta, S.; Papatheodorou, S.I.; Hawkins, R.; Ailawadi, G.; Mittleman, M.A.; Chu, M.W.A. Minimally Invasive versus Sternotomy for Mitral Surgery in the Elderly: A Systematic Review and Meta-Analysis. Innovations 2021, 16, 310–316. [Google Scholar] [CrossRef]
- Oezpeker, C.; Barbieri, F.; Hoefer, D.; Schneider, B.; Bonaros, N.; Grimm, M.; Mueller, L. Mitral Valve Surgery via Partial Upper Sternotomy: Closing the Gap between Conventional Sternotomy and Right Lateral Minithoracotomy. Thorac. Cardiovasc. Surg. 2019, 67, 524–530. [Google Scholar] [CrossRef]
- Bonaros, N.; Hoefer, D.; Oezpeker, C.; Gollmann-Tepeköylü, C.; Holfeld, J.; Dumfarth, J.; Kilo, J.; Ruttmann-Ulmer, E.; Hangler, H.; Grimm, M.; et al. Predictors of safety and success in minimally invasive surgery for degenerative mitral disease. Eur. J. Cardio-Thorac. Surg. 2022, 61, 637–644. [Google Scholar] [CrossRef]
- Gaur, P.; Kaneko, T.; McGurk, S.; Rawn, J.D.; Maloney, A.; Cohn, L.H. Mitral valve repair versus replacement in the elderly: Short-term and long-term outcomes. J. Thorac. Cardiovasc. Surg. 2014, 148, 1400–1406. [Google Scholar] [CrossRef]
- Farid, S.; Ladwiniec, A.; Hernandez-Sanchez, J.; Povey, H.; Caruana, E.; Ali, A.; Moorjani, N.; Irons, J.; Ring, L.; Abu-Omar, Y. Early Outcomes after Mitral Valve Repair versus Replacement in the Elderly: A Propensity Matched Analysis. Heart Lung Circ. 2019, 28, 314–319. [Google Scholar] [CrossRef]
- Bonaros, N.; Hofer, D.; Holfeld, J.; Grimm, M.; Muller, L. Cannulation of the Carotid Artery for Minimally Invasive Mitral or Tricuspid Valve Surgery. Ann. Thorac. Surg. 2020, 110, e517–e519. [Google Scholar] [CrossRef]
- Al Otaibi, A.; Gupta, S.; Belley-Cote, E.P.; Alsagheir, A.; Spence, J.; Parry, D.; Whitlock, R.P. Mini-thoracotomy vs. conventional sternotomy mitral valve surgery: A systematic review and meta-analysis. J. Cardiovasc. Surg. 2017, 58, 489–496. [Google Scholar] [CrossRef] [PubMed]
- Oezpeker, C.U.; Barbieri, F.; Hoefer, D.; Bonaros, N.; Grimm, M.; Mueller, L. Upper Hemi-Sternotomy Provides Benefit for Patients with Isolated or Combined Mitral Valve Surgery. Medicina 2022, 58, 142. [Google Scholar] [CrossRef] [PubMed]
- Vlahakes, G.J. Right ventricular failure after cardiac surgery. Cardiol. Clin. 2012, 30, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Zanobini, M.; Loardi, C.; Poggio, P.; Tamborini, G.; Veglia, F.; di Minno, A.; Myasoedova, V.; Mammana, L.F.; Biondi, R.; Pepi, M.; et al. The impact of pericardial approach and myocardial protection onto postoperative right ventricle function reduction. J. Cardiothorac. Surg. 2018, 13, 55. [Google Scholar] [CrossRef]
- Chivasso, P.; Bruno, V.D.; Farid, S.; Malvindi, P.G.; Modi, A.; Benedetto, U.; Ciulli, F.; Abu-Omar, Y.; Caputo, M.; Angelini, G.D.; et al. Predictors of survival in octogenarians after mitral valve surgery for degenerative disease: The Mitral Surgery in Octogenarians study. J. Thorac. Cardiovasc. Surg. 2018, 155, 1474–1482.e2. [Google Scholar] [CrossRef]
- Moscarelli, M.; Emmanuel, S.; Athanasiou, T.; Speziale, G.; Fattouch, K.; Casula, R. The role of minimal access valve surgery in the elderly. A meta-analysis of observational studies. Int. J. Surg. 2016, 33 Pt A, 164–171. [Google Scholar] [CrossRef]
- Loulmet, D.F.; Ranganath, N.K.; Neragi-Miandoab, S.; Koeckert, M.S.; Galloway, A.C.; Grossi, E.A. Advanced experience allows robotic mitral valve repair in the presence of extensive mitral annular calcification. J. Thorac. Cardiovasc. Surg. 2019. epub ahead of print. [Google Scholar] [CrossRef]
- Helmers, M.R.; Shin, M.; Iyengar, A.; Arguelles, G.R.; Mays, J.; Han, J.J.; Patrick, W.; Altshuler, P.; Hargrove, W.C.; Atluri, P. Permanent pacemaker implantation following mitral valve surgery: A retrospective cohort study of risk factors and long-term outcomes. Eur. J. Cardiothorac. Surg. 2021, 60, 140–147. [Google Scholar] [CrossRef]
- Lukac, P.; Hjortdal, V.; Pedersen, A.K.; Jensen, H.K.; Mortensen, P.T.; Hansen, P.S. The superior transseptal surgical approach to mitral valve creates slow conduction. Pacing Clin. Electrophysiol. 2006, 29, 719–726. [Google Scholar] [CrossRef]
| Era 1 n = 181 | Era 2 n = 336 | ||
|---|---|---|---|
| FS Instead of MT n = 78 | PS Instead of MT n = 115 | FS Instead of MT n = 50 | |
| Severe peripheral or aortic atherosclerosis (%, n) | 3.3 (6) | 20.9 (24) | 3.3 (6) |
| AV regurgitation ≤ moderate (%, n) | 3.9 (10) | 7.8 (9) | 3.9 (10) |
| Patient in a clinically worse condition (%, n) | 11.6 (21) | 16.5 (19) | 11.6 (21) |
| Moderate-to-major AC (%, n) | 9.9 (18) | 34 (34) | 9.9 (18) |
| Pulmonary hypertension ≥ moderate (%, n) | 6.6 (12) | 18.3 (21) | 6.6 (12) |
| Reduced LVEF ≥ moderate | 5.0 (9) | 4.3 (5) | 5.0 (9) |
| Right-sided pleural adhesions (%, n) | 1.1 (2) | 1.7 (2) | 1.1 (2) |
| Surgical training reasons (%, n) | 0 | 0.9 (1) | 0 |
| MVS (Total) n = 517 | MT-MVS n = 274 | PS-MVS n = 115 | FS-MVS n = 128 | p-Value | |
|---|---|---|---|---|---|
| Age (years) 1 | 75 (72–78) | 74 (63–77) | 76 (72–79) | 75 (72–79) | 0.006 |
| Gender, females (%, n) | 56.5 (292) | 52.6 (144) | 58.3 (67) | 62.5(80) | 0.154 |
| Primary MV disease (%, n) | 82.6 (427) | 79.9 (219) | 87.8 (101) | 83.6 (107) | 0.163 |
| BSA (m2) | 1.80 (1.66–1.94) | 1.80 (1.70–2.0) | 1.77 (1.62–1.94) | 1.74 (1.63–1.87) | <0.001 |
| DM (%, n) | 36.2 (187) | 52.9 (145) | 18.3 (21) | 16.4 (21) | <0.001 |
| IDDM (%, n) | 4.6 (24) | 6.2 (17) | 2.6 (3) | 3.1 (4) | 0.191 |
| Art.hypertension (%, n) | 65.8 (340) | 52.9 (145) | 81.7 (94) | 78.9 (101) | <0.001 |
| COPD ≥ GOLD 2 (%, n) | 18.4 (95) | 30.5 (51) | 35.4 (58) | 30.5 (50) | <0.001 |
| PAOD (%, n) | 2.3 (12) | 0.7 (2) | 6.1 (7) | 2.3 (3) | 0.006 |
| Dialysis (%, n) | 0.4 (2) | 0 | 1.7 (2) | 0 | 0.030 |
| Smoking history (%, n) | 9.5 (49) | 5.1 (14) | 16.5 (19) | 12.5 (16) | <0.001 |
| HLP (%, n) | 39.1 (202) | 28.8 (79) | 53.9 (62) | 47.7 (61) | <0.001 |
| Prev.CVE (%, n) | 4.1 (21) | 1.5 (4) | 7 (8) | 7 (9) | 0.006 |
| EuroSCORE2 (%) 1 | 3.10 (1.80–4.73) | 2.20 (1.31–3.70) | 3.70 (2.51–5.20) | 4.21 (3.15–6.43) | <0.001 |
| LV-EF (%) 1 | 60 (51–64) | 60 (52–64) | 58 (50–65) | 57 (50–63) | 0.114 |
| NYHA III (%, n) | 56.1 (290) | 51.8 (142) | 61.7 (71) | 60.2 (77) | 0.112 |
| NYHA IV (%, n) | 5.0 (26) | 3.3 (9) | 8.7 (10) | 5.5 (7) | 0.081 |
| i-Afib (%, n) | 42.4 (219) | 37.2 (102) | 43.5 (50) | 52.3 (67) | 0.016 |
| p-Afib (%, n) | 15.3 (79) | 9.5 (26) | 25.2 (29) | 21.1 (27) | <0.001 |
| sPAP > 55 mmHg (%, n) | 15.3 (79) | 5.1 (14) | 32.1 (34) | 32 (31) | <0.001 |
| NT-proBNP (ng/l) 1 | 1218 (550–2133) | 1148 (472–1800) | 1410 (705–2979) | 1220 (723–2431) | 0.004 |
| Intraoperative Outcomes | MVS (Total) n = 517 | MT-MVS n = 274 | PS-MVS n = 115 | FS-MVS n = 128 | p-Value |
|---|---|---|---|---|---|
| MV repair (%, n) | 74.1 (383) | 88.97 (242) | 62.6 (72) | 53.9 (69) | <0.001 |
| Switch MV repair to replacement (intraoperatively) (%, n) | 2.7 (14) | 1.5 (4) | 2.6 (3) | 5.5 (7) | 0.070 |
| Additional TV repair (%, n) | 40.8 (211) | 34.3 (94) | 46.1 (53) | 50 (64) | 0.005 |
| Ablation surgical (%, n) | 15.3 (79) | 17.5 (48) | 9.6 (11) | 15.6 (20) | 0.137 |
| Cardiopulmonary bypass time (min) 1 | 168 (137–211) | 198 (158–232) | 151 (130–176) | 144 (113–170) | <0.001 |
| Aortic cross-clamp time (min) 1 | 101 (80–123) | 106 (84–126) | 94 (83–115) | 93 (71–118) | 0.004 |
| Conversion to FS (%, n) | 5.0 (26) | 4 (11) | 13 (15) | 0 | <0.001 |
| Second pump run/X-clamp (%, n) | 4.3 (22) | 3.0 (8) | 6.1 (7) | 5.5 (7) | 0.365 |
| Moderate-to-major annulus calcifications (%, n) | 17.0 (88) | 0.7 (2) | 32.2 (37) | 38.3 (49) | <0.001 |
| En bloc decalcifications (%, n) | 2.9 (15) | 0.7 (2) | 3.5 (4) | 7.0 (9) | 0.002 |
| Postoperative Outcomes | MVS (Total) n = 517 | MT-MVS n = 274 | PS-MVS n = 115 | FS-MVS n = 128 | p-Value |
|---|---|---|---|---|---|
| MV regurgitation ≥ 2 after MV-reapair * (%, n) | 4.2 (16) | 2.9 (7) | 1.4 (1) | 11.6 (8) | 0.040 |
| Mild PVL * (in the MV-replacement group) (%, n) | 2.2 (3) | 0 (0) | 4.7 (2) | 1.7 (1) | 0.113 |
| 30-days mortality (%, n) | 2.1 (11) | 0.7 (2) | 2.6 (3) | 4.7 (6) | 0.035 |
| 1-year mortality (%, n) | 4.5 (23) | 2.2 (6) | 5.2 (6) | 8.6 (11) | 0.016 |
| Extracorporeal membrane oxygenation, (%, n) | 2.5 (13) | 3.3 (9) | 2.6 (3) | 0.8 (1) | 0.327 |
| Cardiac low-output syndrome, (%, n) | 10.4 (54) | 3.3 (9) | 14.8 (17) | 21.9 (28) | <0.001 |
| Tamponade or excessive bleeding (%, n) | 6.2 (32) | 5.5 (15) | 7.8 (9) | 6.3 (8) | 0.680 |
| Hemofiltration/-dialysis (%, n) | 7.9 (41) | 1.1 (3) | 20 (23) | 11.7 (15) | <0.001 |
| Ventilation >24 hrs (%, n) | 15.3 (79) | 10.9 (30) | 19.1 (22) | 21.1 (27) | 0.013 |
| Red blood units (total) 1 | 1 (1–2) | 0 (0–2) | 1 (1–3) | 1 (1–3) | <0.001 |
| Intensive care unit length (days) 1 | 1 (1–2) | 1 (1–1) | 1 (1–4) | 2 (1–9) | <0.001 |
| Hospital stay (days) 1 | 8 (7–11) | 8 (7–9) | 8 (7–12) | 10 (8–12) | <0.001 |
| Deep wound infection (%, n) | 1.4 (7) | 0 | 1.7 (2) | 3.9 (5) | 0.006 |
| Cerebrovascular adverse event (%, n) | 0.8 (4) | 0 | 0.9 (1) | 2.3 (3) | 0.044 |
| Pacemaker implantation (%, n) | 3.4 (18) | 0.4 (1) | 8.7 (10) | 5.5 (7) | <0.001 |
| Myocardial infarction (%, n) | 0.4 (2) | 0 | 0.9 (1) | 0.8 (1) | 0.648 |
| MVS (Total) n = 517 | FS vs. PS n = 243 | p-Value | OR | CI | FS vs. MT n = 402 | p-Value | OR | CI | |
|---|---|---|---|---|---|---|---|---|---|
| Combined operative success—yes (%) | 89.0 | 85.2 | 0.155 | 0.60 | 0.29–1.22 | 91.0 | 0.188 | 1.60 | 0.80–3.22 |
| EuroSCORE2 adjusted | 0.162 | 0.60 | 0.29–1.23 | 0.373 | 1.39 | 0.67–2.84 | |||
| Combined perioperative success—yes (%) | 74.1 | 63.8 | 0.529 | 0.85 | 0.50–1.43 | 77.6 | <0.001 | 2.60 | 1.60–4.21 |
| EuroSCORE2 adjusted | 0.470 | 0.82 | 0.48–1.40 | 0.002 | 2.19 | 1.32–3.63 | |||
| 30-day survival (%) | 97.9 | 96.3 | 0.398 | 1.84 | 0.449–7.52 | 98.0 | 0.021 | 6.69 | 1.33–33.61 |
| MI (%) | 0.6 | 0.4 | 0.997 | n.a | 0.5 | 0.956 | 1.07 | 0.10–11.92 | |
| ECMO (%) | 2.5 | 1.6 | 0.292 | 0.294 | 0.030–2.87 | 2.2 | 0.168 | 0.232 | 0.3–1.85 |
| Renal failure dialysis (%) | 7.9 | 15.6 | 0.079 | 0.531 | 0.26–1.08 | 4.5 | <0.001 | 11.991 | 3.41–42.23 |
| >24 h ventilation (%) | 15.3 | 20.1 | 0.703 | 1.13 | 0.60–2.1 | 14.2 | 0.007 | 2.17 | 1.23–3.84 |
| Reoperation for any reason (%) | 7.4 | 8.6 | 0.668 | 1.22 | 0.49–3.0 | 4.2 | 0.256 | 1.56 | 0.72–3.38 |
| Reoperation bleeding (%) | 6.2 | 7.0 | 0.631 | 0.79 | 0.29–2.11 | 5.7 | 0.755 | 1.15 | 0.48–2.8 |
| PM implantation (%) | 3.5 | 7.0 | 0.329 | 0.607 | 0.223–1.652 | 2.0 | 0.01 | 15.79 | 1.9–129.8 |
| CVE (%) | 0.8 | 1.6 | 0.386 | 2.74 | 0.28–26.68 | 0 | 0.99 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oezpeker, U.C.; Barbieri, F.; Höfer, D.; Gollmann-Tepeköylü, C.; Holfeld, J.; Sommerauer, F.; Wagner, J.; Rajsic, S.; Ersahin, S.; Bonaros, N.; et al. An Individualized, Less-Invasive Surgical Approach Algorithm Improves Outcome in Elderly Patients Undergoing Mitral Valve Surgery. J. Cardiovasc. Dev. Dis. 2023, 10, 28. https://doi.org/10.3390/jcdd10010028
Oezpeker UC, Barbieri F, Höfer D, Gollmann-Tepeköylü C, Holfeld J, Sommerauer F, Wagner J, Rajsic S, Ersahin S, Bonaros N, et al. An Individualized, Less-Invasive Surgical Approach Algorithm Improves Outcome in Elderly Patients Undergoing Mitral Valve Surgery. Journal of Cardiovascular Development and Disease. 2023; 10(1):28. https://doi.org/10.3390/jcdd10010028
Chicago/Turabian StyleOezpeker, Ulvi Cenk, Fabian Barbieri, Daniel Höfer, Can Gollmann-Tepeköylü, Johannes Holfeld, Florian Sommerauer, Julian Wagner, Sasa Rajsic, Suat Ersahin, Nikolaos Bonaros, and et al. 2023. "An Individualized, Less-Invasive Surgical Approach Algorithm Improves Outcome in Elderly Patients Undergoing Mitral Valve Surgery" Journal of Cardiovascular Development and Disease 10, no. 1: 28. https://doi.org/10.3390/jcdd10010028
APA StyleOezpeker, U. C., Barbieri, F., Höfer, D., Gollmann-Tepeköylü, C., Holfeld, J., Sommerauer, F., Wagner, J., Rajsic, S., Ersahin, S., Bonaros, N., Grimm, M., & Ludwig, M. (2023). An Individualized, Less-Invasive Surgical Approach Algorithm Improves Outcome in Elderly Patients Undergoing Mitral Valve Surgery. Journal of Cardiovascular Development and Disease, 10(1), 28. https://doi.org/10.3390/jcdd10010028







