Abstract
Spatiotemporal parameters such as gait velocity and stride length are simple indicators of functional status and can be used to predict major adverse outcomes in older adults. A smartphone can be used for gait analysis by providing spatiotemporal parameters useful for improving the diagnosis and rehabilitation processes in frail people. The aim of this study was to review articles published in the last 20 years (from 2004 to 2024) concerning the application of smartphones to assess the spatiotemporal parameters of gait in older adults. This systematic review was performed in line with Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA), and original articles were identified by searching seven electronic databases: SciVerse (ScienceDirect), Excerpta Medica Database (EMBASE), Medline, Scopus, PubMed, Web of Science and the Cochrane Library. Studies were rigorously screened using the inclusion criteria of smartphones and mobile apps, older adults and spatiotemporal gait parameters, and results were narratively synthesized. Seventy-three articles were initially identified while searching the scientific literature regarding this topic. Eleven articles were selected and included in this review. Analysis of these studies covered information about gait assessment using mobile apps recorded in 723 older adults and 164 control cases. Analysis of data related to the application of smartphones to assess spatiotemporal parameters of gait in older adults showed moderate-to-excellent test–retest reliability and validity (ICCs around 0.9) of gait speed, the most common parameter reported. Additionally, gait speeds recorded with mobile apps showed excellent agreement when compared to gold standard systems. Smartphones and mobile apps are useful, non-invasive, low-cost and objective tools that are being extensively used to perform gait analysis in older adults. Smartphones and mobile apps can reliably identify spatiotemporal parameters related to adverse outcomes, such as a slow gait speed, as predictors and outcomes in clinical practice and research involving older adults.
1. Introduction
Numerous studies have analyzed gait in older adults and its relationship with adverse outcomes, including disability, dementia, hospitalization and mortality [1,2,3,4]. Different spatiotemporal variables related to adverse outcomes have been identified in the scientific literature, such as gait speed, stride length and cadence [5]. Older adults who present a slower gait and a decrease in stride length are considered patients at risk. In particular, a gait speed lower than 0.8 m/s is a reliable cut-off for identifying subjects at increased risk of disability, and a stride length of 0.64 m accurately predicts major adverse events such as physical disability, falls, institutionalization and mortality [6,7]. With the advancement of medical and health standards, the proportion of people over 60 accounts for 12.3% of the global population, and World Health Organization studies show that by 2050 this figure will approximately double from 12% to 22% [8,9,10]. Aging is associated with physiological changes that can reduce mobility and quality of life in people aged 65 years and older, but age-related gait decline is still underdiagnosed or diagnosed at a relatively late stage, often following an injury, despite increasing evidence suggesting that a decrease in walking speed represents a key element of frailty [11]. Over the last decade, several reports have pinpointed the importance of early detection in patients with gait impairments and those at risk of falling [12,13]. The use of smartphone apps in daily life may be adapted to the early detection of older individuals with a reduced walking speed and can help identify individuals who are at higher risk of falling before an episode of fall or an advanced stage of dementia [14,15]. Smartphone apps are widely used to collect data on gait parameters such as cadence, gait speed and step length, enabling monitoring of the patient’s status in a free-living environment [16]. Older adults are increasingly using smartphones and mobile apps, which may serve as useful tools to support gait assessment [17,18]. Early detection of a decline in gait parameters may help older adults adopt timely interventions in order to improve their quality of life and predict adverse outcomes [19]. The aim of this scoping review was to provide current evidence regarding the effectiveness of gait assessment using a mobile app on a smartphone in the aged population, and results of this study highlight the importance of gait impairments and enhance our knowledge of gait assessment protocols as a simple indicator to predict major adverse outcomes in older adults.
2. Materials and Methods
2.1. Identifying the Research Question
The primary aim of this review was to synthesize all the published evidence on gait impairment evaluated with smartphones in older adults. The review question was formulated using the PCC strategy (population, concept and context), and eligibility criteria were developed based on populations, interventions or exposures, comparators, outcomes and study designs (PICOS): participants: older adults (over the age of 65 years); interventions or exposures: not applicable; comparators: data collected with a smartphone and/or mobile app; outcomes: gait assessment; study designs: cross-sectional and prospective cohort observational studies and intervention studies. The review question was as follows: are smartphone-based gait assessments in older adults a reliable method of quantifying the spatiotemporal parameters of gait and predicting adverse outcomes? The goal of this work was to provide an overview of the recent state of the art in this field, characterizing current usage and limitations.
2.2. Literature Search Methodology
The following systematic review was performed in line with Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA). The research question was developed using the PICO framework. This study analyzed every original article published up to April 2024 that met the following inclusion criteria: (1) full text in English; (2) primary articles only; and (3) presentation of identifiable data measuring gait with a smartphone in older adults. Studies were searched in the following databases: Scopus, Excerpta Medica Database (EMBASE), Medline, SciVerse (ScienceDirect), PubMed, Web of Science and the Cochrane Library. The search strategy was formulated based on a combination of controlled descriptors and keywords related to the topic. Moreover, a manual search was conducted of reference lists from initially selected studies to identify other eligible studies.
Conference proceedings and articles reporting results from fewer than twenty older patients that did not assess gait or that assessed only balance were excluded. Articles were excluded if they focused on mobility assessment for older people with neurological disorders such as Alzheimer’s disease or Parkinson’s disease.
An electronic search was performed in PubMed on 11 April 2024 using the following search string:
(“smartphone”[MeSH Terms] OR “smartphone”[All Fields] OR “smartphones”[All Fields] OR “smartphone s”[All Fields]) AND (“gait”[MeSH Terms] OR “gait”[All Fields]) AND (“aged”[MeSH Terms] OR “aged”[All Fields] OR (“older”[All Fields] AND “adults”[All Fields]) OR “older adults”[All Fields]).
(“mobile applications”[MeSH Terms] OR (“mobile”[All Fields] AND “applications”[All Fields]) OR “mobile applications”[All Fields] OR (“mobile”[All Fields] AND “app”[All Fields]) OR “mobile app”[All Fields]) AND (“gait”[MeSH Terms] OR “gait”[All Fields]) AND (“aged”[MeSH Terms] OR “aged”[All Fields] OR (“older”[All Fields] AND “adults”[All Fields]) OR “older adults”[All Fields]).
A number of articles (165) were initially identified while searching the scientific literature regarding this topic, and 11 articles were selected and included in this review. Figure 1 presents a flowchart of the review process (PRISMA diagram).
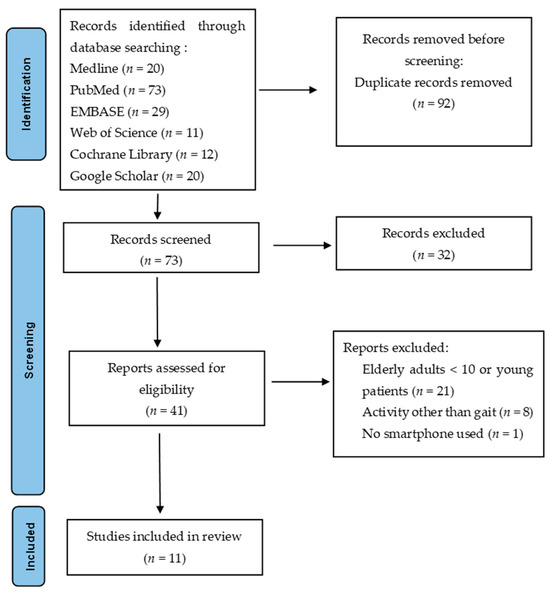
Figure 1.
PRISMA diagram: this figure represents the flow of study selection through identification, screening, eligibility and inclusion.
Finally, reference lists of all relevant articles were manually cross-referenced in order to identify any additional articles. A qualitative synthesis of data from selected studies was conducted, describing the following data: (1) characteristics of the studies (name of the study, authors, year of publication); (2) demographic information for samples (sample size, participant characteristics of mean age, gender distribution); (3) spatiotemporal parameters investigated; (4) mobile app used; (5) smartphone used and (6) main findings. These data are summarized in Table 1, which lists characteristics of mobile apps, smartphones used and spatiotemporal parameters.

Table 1.
Characteristics of mobile apps, smartphones used and gait parameters: an overview of selected studies.
3. Results
Studies included an average of 74 older patients with a sample of at least 28 participants [14] and a maximum of 163 participants [23]. The minimum average age observed in these studies was 56.12 ± 6.06 years [21], with a maximum of 75.6 years [22]. These studies had a specific sex target; in most studies, women were the most prevalent. Concerning gait spatiotemporal parameters, substantial variety was found in selected articles. Gait speed and step length are the most common parameters reported in these studies (Figure 2). Cadence, which can be particularly useful when evaluating older patients (who often may exhibit short steps), is reported in only two studies [23,27].
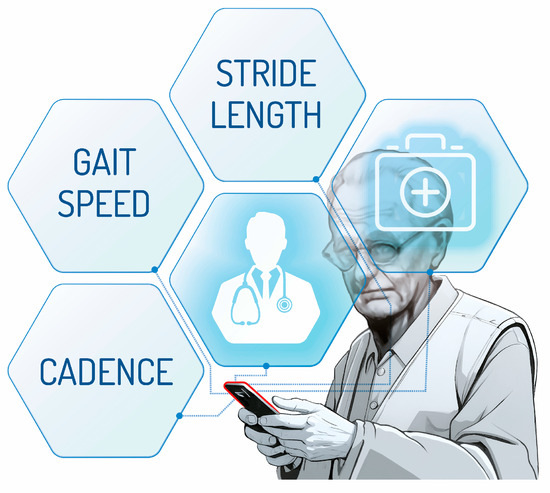
Figure 2.
Spatiotemporal parameters most frequently evaluated in selected articles.
In this review, I did not find one particular smartphone set-up that was used by most studies, but a wide variety of combinations. The most used set-up was a smartphone attached to a sacroiliac belt, which was used in 8 of 11 studies screened [20,21,22,26,27,28,29,30]. The other position was in the pant pocket [14,23,25] (Figure 3).
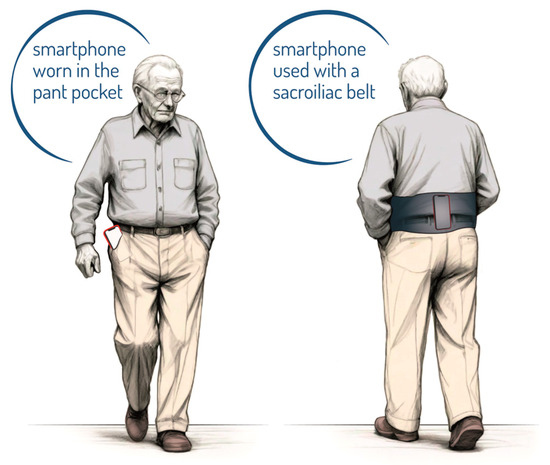
Figure 3.
Smartphone placement: the corresponding position of the smartphone reported.
Also, in terms of mobile operating systems, there was no homogeneity; 5 of the 11 studies screened used the Android operating system, and 6 of 11 used iOS. The G&B app for iOS represents the most used app, featured in 3 of 11 studies [21,26,28]. Most studies (6 of 11) reported the number of patients with a history of falls, with a maximum of 37 patients analyzed [20]; alternatively, other studies reported some motor/balance scores such as Berg Balance, the Kihon checklist score, the mini-balance evaluation system test, the functional gait assessment or the short physical performance battery. The heterogeneity of the scores used made it difficult to draw a conclusion and compare the functional ability of the sample recruited. Consensus still needs to be reached in this field; therefore, it is recommended that new studies report the history of falls in the analyzed sample.
Data Analyses
Studies analyzed gait parameters collected with smartphones using descriptive statistics and ANOVA; analysis showed that age had a significant effect on smaller step frequency (p < 0.001) [20], worse step regularity and variability [29]. Gait cadence, which is also reported as step frequency, could be a useful indicator when estimating functional capacity, with a sensitivity of 0.81 (95% CI: 0.77, 0.85) and a specificity of 0.57 (95% CI: 0.55, 0.59) [27].
Other studies explored the test reliability and construct validity of mobile app data compared with clinical measurements (Time Up and Go Test). The sensitivity of app data demonstrated moderate-to-excellent reliability for walking looking straight ahead for gait symmetry (ICC = 0.65), walking speed (ICC = 0.93), step length (ICC = 0.94) and step time (ICC = 0.84) [21,30]. Giannouli et al. showed moderate-to-excellent test–retest reliability (ICCs between 0.584 and 0.920) and validity (ICCs between 0.468 and 0.950) of walking speed measurements of 50 m [25]. Olsen et al. recently confirmed moderate-to-excellent validity for mobile app measurements of step time (rp 0.97, 95% CI [0.96, 0.98]), walking speed (rp 0.83 [0.78, 0.87]) and step length (rp 0.74, [0.66, 0.80]) [28]. In contrast, not all spatiotemporal parameters had the same validity; in fact, Olsen et al. found that step length variability (r 0.29 [0.09, 0.47]), step length asymmetry (r 0.14 [0.06, 0.34]), step time variability (r 0.49 [0.31, 0.63]) and step time asymmetry (r 0.2 [0.01, 0.39]) had poor validity [26].
Three studies compared the smartphone app analysis with gold standard methods such as 3D kinematics, video assessment and the GAITRite® system [14,26,28]. Lee P.-A. et al. showed a high correlation (r = 0.94), with minimal differences (mean = 0.07 m/s, ± 1.96 SD = 0.12) across a range of gait speeds and a high test–retest reliability (ICC values: 0.75 to 0.93) compared to video assessment analysis [14]. Results obtained by Olsen et al. showed excellent agreement between the mobile app and the GAITRite system for step time (rp 0.97, 95% CI [0.96, 0.98]), walking speed (rp 0.83, 95% CI [0.78, 0.87]) and step length (rp 0.74, 95% CI [0.66, 0.8]) [28].
4. Discussion
Biomechanical investigation allows the identification of abnormalities in gait that may also impact the quality of life and mobility of older adults [31]. One of the most important spatiotemporal parameters that seems to decline significantly in older patients is gait speed [21,22,32,33]. The emergence of technologies such as smartphones, mobile apps and artificial intelligence has provided promising avenues for gait analysis that had previously been performed in laboratories with a set of measurement systems such as stereophotogrammetry, EMG and force platforms [34]. Financial constraints and time expenditure have limited the use of these movement analysis laboratories in clinical practice; hence, the availability of cost-effective and reliable tools for gait analysis is paramount [35]. Gait analysis using smartphones and mobile apps is expected to play an increasingly important role in various clinical fields, where quantitative assessment of outcomes is crucial in achieving therapy goals [36,37,38]. Rehabilitation has significantly benefited from the development of smartphones and mobile apps [39]. In this context, quantifying the re-establishment of function is essential in the success of therapy, and this technology can be used to measure and monitor movements in order to support clinical decision-making [40,41]. Smartphones and mobile apps enable the objective and responsive assessment of physical function during functional tests, gait training or exercise programs, and the increasing use of smartphone technology in our daily lives and clinical settings will simplify patient assessment, therapy and follow-ups for health professionals [42]. Smartphones provide a cheap and accessible means of efficiently collecting large amounts of human gait data in an unconstrained environment compared to motion capture systems, electromyography or other systems that require costly equipment and trained engineers, which are only available in movement analysis research laboratories. To summarize, approaches to gait analysis in older individuals can vary regarding the type of mobile app, smartphone used, smartphone location and the type of spatiotemporal parameters assessed. The large number of patients analyzed in these studies (887 patients) suggests the feasibility of using a mobile app to quantify motor performance in older patients. This scoping review is the first to review articles concerning the application of smartphones to assessing spatiotemporal parameters of gait in older adults. Its novelty lies in providing current evidence regarding the effectiveness of gait assessment using mobile apps through smartphones in the aged population. The use of smartphones for gait analysis has been studied in patients with Parkinson’s disease, post-stroke and multiple sclerosis [43,44,45]. However, these patients have unique and variable gait patterns, so the results may not be applicable to the general elderly population. This study is not without limitations. One limitation of the present study concerns the inability to carry out a statistical analysis of results due to the heterogeneity of the control groups, mobile app used and type of gold standard chosen in order to investigate the validity of spatiotemporal gait parameters assessed with smartphones.
Consensus among the clinical research community regarding the smartphone’s location is yet to come. Looser pants with larger pockets may have led to more artifactual instrument movements and/or greater deviations from the participant’s center of mass, providing a poorer signal for data processing [46]. For this reason, the most reliable protocol to date is probably the one that involves positioning the smartphone using a sacroiliac belt. Despite the different mobile apps and smartphones used, all studies agreed on the reliability of these tools for measuring spatiotemporal parameters such as gait speed, the most investigated spatiotemporal parameter, in older adults, with excellent reliability [25,47,48,49].
5. Conclusions
This review provides strong evidence regarding the potential use of smartphone applications to assess gait impairments among older individuals. The results indicate that smartphone applications are tools with strong validity and reliability in monitoring gait dysfunctions, such as lower walking speeds and stride lengths, that are related to adverse outcomes, including disability and mortality. This study also highlights promising avenues for further research, emphasizing the importance of predictive modeling in addressing capability risks in the daily activities of the older population.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data supporting the reported results can be obtained by writing to lorenzo.brognara2@unibo.it.
Acknowledgments
Conflicts of Interest
The author declares no conflicts of interest.
References
- Veronese, N.; Stubbs, B.; Volpato, S.; Zuliani, G.; Maggi, S.; Cesari, M.; Lipnicki, D.M.; Smith, L.; Schofield, P.; Firth, J.; et al. Association Between Gait Speed with Mortality, Cardiovascular Disease and Cancer: A Systematic Review and Meta-analysis of Prospective Cohort Studies. J. Am. Med. Dir. Assoc. 2018, 19, 981–988.e7. [Google Scholar] [CrossRef]
- Montero-Odasso, M.; Schapira, M.; Soriano, E.R.; Varela, M.; Kaplan, R.; Camera, L.A.; Mayorga, L.M. Gait Velocity as a Single Predictor of Adverse Events in Healthy Seniors Aged 75 Years and Older. J. Gerontol. A Biol. Sci. Med. Sci. 2005, 60, 1304–1309. [Google Scholar] [CrossRef]
- Van Kan, G.A.; Rolland, Y.; Andrieu, S.; Bauer, J.; Beauchet, O.; Bonnefoy, M.; Cesari, M.; Donini, L.; Gillette-Guyonnet, S.; Inzitari, M.; et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J. Nutr. Health Aging 2009, 13, 881–889. [Google Scholar] [CrossRef] [PubMed]
- Verghese, J.; Holtzer, R.; Lipton, R.B.; Wang, C. Quantitative Gait Markers and Incident Fall Risk in Older Adults. J. Gerontol. A Biol. Sci. Med. Sci. 2009, 64A, 896–901. [Google Scholar] [CrossRef] [PubMed]
- Doi, T.; Nakakubo, S.; Tsutsumimoto, K.; Kurita, S.; Ishii, H.; Shimada, H. Spatiotemporal gait characteristics and risk of mortality in community-dwelling older adults. Maturitas 2021, 151, 31–35. [Google Scholar] [CrossRef]
- Studenski, S. Gait Speed and Survival in Older Adults. JAMA 2011, 305, 50. [Google Scholar] [CrossRef]
- Bytyçi, I.; Henein, M.Y. Stride Length Predicts Adverse Clinical Events in Older Adults: A Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 2670. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, E.; Walker, R. Global ageing: Successes, challenges and opportunities. Br. J. Hosp. Med. 2020, 81, 1–9. [Google Scholar] [CrossRef]
- World Health Organization. Decade of Healthy Ageing: Baseline Report; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 26 June 2024).
- Samaras, N.; Chevalley, T.; Samaras, D.; Gold, G. Older patients in the emergency department: A review. Ann. Emerg. Med. 2010, 56, 261–269. [Google Scholar] [CrossRef]
- Hardy, S.E.; Perera, S.; Roumani, Y.F.; Chandler, J.M.; Studenski, S.A. Improvement in Usual Gait Speed Predicts Better Survival in Older Adults. J. Am. Geriatr. Soc. 2007, 55, 1727–1734. [Google Scholar] [CrossRef]
- Ruiz-Ruiz, L.; Jimenez, A.R.; Garcia-Villamil, G.; Seco, F. Detecting Fall Risk and Frailty in Elders with Inertial Motion Sensors: A Survey of Significant Gait Parameters. Sensors 2021, 21, 6918. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.-A.; DuMontier, C.; Yu, W.; Ask, L.; Zhou, J.; Testa, M.A.; Kim, D.; Abel, G.; Travison, T.; Manor, B.; et al. Validity and Reliability of a Smartphone Application for Home Measurement of Four-Meter Gait Speed in Older Adults. Bioengineering 2024, 11, 257. [Google Scholar] [CrossRef] [PubMed]
- Lunardini, F.; Malavolti, M.; Pedrocchi, A.L.G.; Borghese, N.A.; Ferrante, S. A mobile app to transparently distinguish single- from dual-task walking for the ecological monitoring of age-related changes in daily-life gait. Gait Posture 2021, 86, 27–32. [Google Scholar] [CrossRef]
- Silsupadol, P.; Teja, K.; Lugade, V. Reliability and validity of a smartphone-based assessment of gait parameters across walking speed and smartphone locations: Body, bag, belt, hand, and pocket. Gait Posture 2017, 58, 516–522. [Google Scholar] [CrossRef]
- Andrea, R.; Mireia, F.-A. Smartphone usage diversity among older people. In Perspectives on Human-Computer Interaction Research with Older People; Springer Link: Berlin/Heidelberg, Germany, 2019. [Google Scholar]
- Portenhauser, A.A.; Terhorst, Y.; Schultchen, D.; Sander, L.B.; Denkinger, M.D.; Stach, M.; Waldherr, N.; Dallmeier, D.; Baumeister, H.; Messner, E.-M. Mobile Apps for Older Adults: Systematic Search and Evaluation within Online Stores. JMIR Aging 2021, 4, e23313. [Google Scholar] [CrossRef] [PubMed]
- Almada, M.; Brochado, P.; Portela, D. Prevalence of falls and associated factors among community-dwelling older adults: A cross-sectional study. J. Frailty Aging 2020, 10, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Zhong, R.; Rau, P.L.P. A mobile phone-based gait assessment app for the elderly: Development and evaluation. JMIR Mhealth Uhealth 2020, 8, e14453. [Google Scholar] [CrossRef] [PubMed]
- Shafi, H.; Awan, W.A.; Olsen, S.; Siddiqi, F.A.; Tassadaq, N.; Rashid, U.; Niazi, I.K. Assessing Gait & Balance in Adults with Mild Balance Impairment: G&B App Reliability and Validity. Sensors 2023, 23, 9718. [Google Scholar] [CrossRef] [PubMed]
- Doshi, K.B.; Moon, S.H.; Whitaker, M.D.; Lockhart, T.E. Assessment of gait and posture characteristics using a smartphone wearable system for persons with osteoporosis with and without falls. Sci. Rep. 2023, 13, 538. [Google Scholar] [CrossRef] [PubMed]
- Kawai, H.; Obuchi, S.; Ejiri, M.; Ito, K. Association between daily life walking speed and frailty measured by a smartphone application: A cross-sectional study. BMJ Open 2023, 13, e065098. [Google Scholar] [CrossRef]
- Satake, S.; Shimokata, H.; Senda, K.; Kondo, I.; Toba, K. Validity of Total Kihon Checklist Score for Predicting the Incidence of 3-Year Dependency and Mortality in a Community-Dwelling Older Population. J. Am. Med. Dir. Assoc. 2017, 18, 552.e1–552.e6. [Google Scholar] [CrossRef]
- Giannouli, E.; Kim, E.-K.; Fu, C.; Weibel, R.; Sofios, A.; Infanger, D.; Portegijs, E.; Rantanen, T.; Huang, H.; Schmidt-Trucksäss, A.; et al. Psychometric properties of the MOBITEC-GP mobile application for real-life mobility assessment in older adults. Geriatr. Nurs. 2022, 48, 273–279. [Google Scholar] [CrossRef]
- Olsen, S.; Rashid, U.; Allerby, C.; Brown, E.; Leyser, M.; McDonnell, G.; Alder, G.; Barbado, D.; Shaikh, N.; Lord, S.; et al. Smartphone-based gait and balance accelerometry is sensitive to age and correlates with clinical and kinematic data. Gait Posture 2023, 100, 57–64. [Google Scholar] [CrossRef]
- Rubin, D.S.; Ranjeva, S.L.; Urbanek, J.K.; Karas, M.; Madariaga, M.L.L.; Huisingh-Scheetz, M. Smartphone-Based Gait Cadence to Identify Older Adults with Decreased Functional Capacity. Digit. Biomark. 2022, 6, 61–70. [Google Scholar] [CrossRef]
- Olsen, S.; Rashid, U.; Barbado, D.; Suresh, P.; Alder, G.; Niazi, I.K.; Taylor, D. The validity of smartphone-based spatiotemporal gait measurements during walking with and without head turns: Comparison with the GAITRite® system. J. Biomech. 2024, 162, 111899. [Google Scholar] [CrossRef]
- Zhong, R.; Gao, T. Impact of walking states, self-reported daily walking amount and age on the gait of older adults measured with a smart-phone app: A pilot study. BMC Geriatr. 2022, 22, 259. [Google Scholar] [CrossRef]
- Pedrero-Sánchez, J.-F.; De-Rosario-Martínez, H.; Medina-Ripoll, E.; Garrido-Jaén, D.; Serra-Añó, P.; Mollà-Casanova, S.; López-Pascual, J. The Reliability and Accuracy of a Fall Risk Assessment Procedure Using Mobile Smartphone Sensors Compared with a Physiological Profile Assessment. Sensors 2023, 23, 6567. [Google Scholar] [CrossRef]
- Suri, A.; Rosso, A.L.; VanSwearingen, J.; Coffman, L.M.; Redfern, M.S.; Brach, J.S.; Sejdić, E. Mobility of Older Adults: Gait Quality Measures Are Associated With Life-Space Assessment Scores. J. Gerontol. Ser. A 2021, 76, e299–e306. [Google Scholar] [CrossRef]
- Brognara, L.; Luna, O.C.; Traina, F.; Cauli, O. Inflammatory Biomarkers and Gait Impairment in Older Adults: A Systematic Review. Int. J. Mol. Sci. 2024, 25, 1368. [Google Scholar] [CrossRef]
- Brognara, L.; Mafla-España, M.A.; Gil-Molina, I.; Castillo-Verdejo, Y.; Cauli, O. The Effects of 3D Custom Foot Orthotics with Mechanical Plantar Stimulation in Older Individuals with Cognitive Impairment: A Pilot Study. Brain Sci. 2022, 12, 1669. [Google Scholar] [CrossRef]
- Brognara, L.; Mazzotti, A.; Di Martino, A.; Faldini, C.; Cauli, O. Wearable Sensor for Assessing Gait and Postural Alterations in Patients with Diabetes: A Scoping Review. Med. B Aires 2021, 57, 1145. [Google Scholar] [CrossRef]
- Simon, S.R. Quantification of human motion: Gait analysis—Benefits and limitations to its application to clinical problems. J. Biomech. 2004, 37, 1869–1880. [Google Scholar] [CrossRef]
- Mulas, I.; Putzu, V.; Asoni, G.; Viale, D.; Mameli, I.; Pau, M. Clinical assessment of gait and functional mobility in Italian healthy and cognitively impaired older persons using wearable inertial sensors. Aging Clin. Exp. Res. 2021, 33, 1853–1864. [Google Scholar] [CrossRef]
- Mazzotti, A.; Arceri, A.; Abdi, P.; Artioli, E.; Zielli, S.O.; Langone, L.; Ramponi, L.; Ridolfi, A.; Faldini, C.; Brognara, L. An Innovative Clinical Evaluation Protocol after Total Ankle Arthroplasty: A Pilot Study Using Inertial Sensors and Baropodometric Platforms. Appl. Sci. 2024, 14, 1964. [Google Scholar] [CrossRef]
- Brognara, L.; Mazzotti, A.; Rossi, F.; Lamia, F.; Artioli, E.; Faldini, C.; Traina, F. Using Wearable Inertial Sensors to Monitor Effectiveness of Different Types of Customized Orthoses during CrossFit® Training. Sensors 2023, 23, 1636. [Google Scholar] [CrossRef]
- Song, Y.; Ren, C.; Liu, P.; Tao, L.; Zhao, W.; Gao, W. Effect of Smartphone-Based Telemonitored Exercise Rehabilitation among Patients with Coronary Heart Disease. J. Cardiovasc. Transl. Res. 2020, 13, 659–667. [Google Scholar] [CrossRef]
- Moral-Munoz, J.A.; Zhang, W.; Cobo, M.J.; Herrera-Viedma, E.; Kaber, D.B. Smartphone-based systems for physical rehabilitation applications: A systematic review. Assist. Technol. 2021, 33, 223–236. [Google Scholar] [CrossRef]
- Milani, P.; Coccetta, C.A.; Rabini, A.; Sciarra, T.; Massazza, G.; Ferriero, G. Mobile Smartphone Applications for Body Position Measurement in Rehabilitation: A Review of Goniometric Tools. PM&R 2014, 6, 1038–1043. [Google Scholar] [CrossRef]
- Lee, C.; Ahn, J.; Lee, B.-C. A Systematic Review of the Long-Term Effects of Using Smartphone- and Tablet-Based Rehabilitation Technology for Balance and Gait Training and Exercise Programs. Bioengineering 2023, 10, 1142. [Google Scholar] [CrossRef]
- Abou, L.; Wong, E.; Peters, J.; Dossou, M.S.; Sosnoff, J.J.; Rice, L.A. Smartphone applications to assess gait and postural control in people with multiple sclerosis: A systematic review. Mult. Scler. Relat. Disord. 2021, 51, 102943. [Google Scholar] [CrossRef]
- Abou, L.; Peters, J.; Wong, E.; Akers, R.; Dossou, M.S.; Sosnoff, J.J.; Rice, L.A. Gait and Balance Assessments using Smartphone Applications in Parkinson’s Disease: A Systematic Review. J. Med. Syst. 2021, 45, 87. [Google Scholar] [CrossRef]
- Peters, J.; Abou, L.; Wong, E.; Dossou, M.S.; Sosnoff, J.J.; Rice, L.A. Smartphone-based gait and balance assessment in survivors of stroke: A systematic review. Disabil. Rehabil. Assist. Technol. 2024, 19, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Werner, C.; Hezel, N.; Dongus, F.; Spielmann, J.; Mayer, J.; Becker, C.; Bauer, J.M. Validity and reliability of the Apple Health app on iPhone for measuring gait parameters in children, adults, and seniors. Sci. Rep. 2023, 13, 5350. [Google Scholar] [CrossRef] [PubMed]
- Rashid, U.; Barbado, D.; Olsen, S.; Alder, G.; Elvira, J.L.L.; Lord, S.; Niazi, I.K.; Taylor, D. Validity and Reliability of a Smartphone App for Gait and Balance Assessment. Sensors 2021, 22, 124. [Google Scholar] [CrossRef]
- Shahar, R.T.; Agmon, M. Gait Analysis Using Accelerometry Data from a Single Smartphone: Agreement and Consistency between a Smartphone Application and Gold-Standard Gait Analysis System. Sensors 2021, 21, 7497. [Google Scholar] [CrossRef]
- Vera-Remartínez, E.J.; Lázaro-Monge, R.; Casado-Hoces, S.V.; Garcés-Pina, E.; Molés-Julio, M.P. Validity and reliability of an android device for the assessment of fall risk in older adult inmates. Nurs. Open 2023, 10, 2904–2911. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).