Abstract
To ensure that older adults (aged 65 years or older) can experience a healthy life, they should use medical services that are appropriate, both quantitatively and qualitatively. This study aimed to identify the factors affecting outpatient service use by older adult women with degenerative arthritis using Andersen’s model. A survey was conducted among 232 older adult women with degenerative arthritis in two university hospitals in Seoul. The Korean Activities of Daily Living, Korean Instrumental Activities of Daily Living, and the Geriatric Depression Scale Short Form were used. Data were analyzed using descriptive statistics, χ2-test, t-test, and multiple logistic regression analysis. Among the participants, 69.8% used outpatient services and 30.2% did not. In the univariate analyses, age, marital status, residency, household income, chronic diseases, subjective health status, and disability were significant. Age (odds ratio [OR] = 5.53, p < 0.001), annual household income (OR = 5.64, p < 0.001), chronic diseases (OR = 11.06, p < 0.001), and disability (OR = 3.56, p = 0.016) significantly affected outpatient service use. The results suggest that health promotion interventions for Korean older adult women should focus on predicting outpatient service use according to the patient’s characteristics.
1. Introduction
With the extension of life expectancy in Korea, the proportion of older adults (aged 65 years or older) has increased by five times since 1970, having reached 14.9% in 2019, and is expected to reach 24.3% by 2030 and 46.5% by 2067 [1]. Moreover, by 2025, Korea is expected to become a super-aged society: that is, adults aged 65 or older will exceed 20% of the population [2]. Thus, the prospective demand for medical services will steadily increase because of the physical and mental changes that older adults experience through the aging process [3,4]. Indeed, older adults often incur health problems that negatively affect their quality of life, such as chronic diseases and their related symptoms and limitations in physical functions [5,6]. Moreover, globally, the number of older adults living longer and with various chronic diseases is increasing [7,8]. Therefore, to ensure that people can experience healthy old age, older adults should use medical services that are appropriate, both quantitatively and qualitatively, to their unique characteristics.
Degenerative arthritis is one of the most common chronic diseases in older people; it causes gradual damage or degenerative changes in the cartilage that protect the joints, thereby damaging the bones and ligaments of a joint and leading to inflammation and pain [9]. In South Korea, the prevalence of degenerative arthritis has increased in those aged 50 years or older, appearing in 25.3% of those in their 60s and 41.5% of those in their 70s; the prevalence of this disease in women is about four times higher than that in men [10]. This disease can easily be deemed a serious health problem for older people as it limits movements in daily living, degrades the quality of life owing to physical changes, and generates high medical expenses [11,12].
Outpatient service use by older adults in Korea has increased 3.8 times from 1990 to 2010 (i.e., from 6.8% to 25.7%), indicating that this population has grown to account for about a quarter of all outpatient service use nationwide [13]. Given the rapid aging phenomenon, the steady increase in medical service use, and the remarks of prior research [14,15], it seems that identifying the influencing factors of outpatient service use in Korean older people may increase our general understanding of medical service use. It also has the potential of providing valuable data for political and managerial policymakers that help to reduce the inequality in access to healthcare nationwide.
The literature shows that Andersen’s behavioral model is a widely used framework for examining the determinants of medical service use in older adults [16]; it categorizes the influencing factors of medical service use into predisposing, enabling, and need factors [17]. Specifically, this model is useful for identifying the health, sociodemographic, and economic characteristics associated with older adults’ health status [17]. Despite the utility of this model for research, there seems to be a lack of studies applying it to predicting medical service use in Korea, and this lack becomes most evident when contrasted with the number of international studies on the topic [18,19,20,21].
One of the few domestic studies that used Andersen’s model on an older adult sample showed that, in the short term, the need factors (e.g., chronic diseases and disabilities) have particularly significant effects, with chronic disease being a causative factor increasing outpatient service use [14]. Lee [22] conducted a longitudinal study using a Korean sample and showed that the predisposing factors (e.g., not living with children, the female sex, and face-to-face contact with others) and enabling factors (e.g., household income and residency in urban areas) were associated with high medical service use. Subsequently, a study published in 2018 showed that outpatient service use rates increased with a negative subjective perception of one’s health status and with the presence of multiple chronic diseases [3]. Another study on outpatient service use and health behavior in Korea showed that living in urban areas, being overweight, having a higher income, and drinking alcohol led to higher medical service use rates [23].
Particularly, some domestic studies have shown that sex affects outpatient service use in older people [15,22]. In 2015, in Korea, older adult women aged 65 or older accounted for 71.7% of the older adult population, showing that there is a higher proportion of older adult women than men, that they are aging faster than men, and that their life expectancy is 4.4 years higher than that of men [24]. Concomitantly, Korean older adult women were reported to have lower values for physical, mental, and economical factors when compared to men [25]. Furthermore, older adult women reportedly have a higher prevalence of chronic diseases and a higher risk of cognitive impairment than older adult men [26]; this last cited study also showed that depressive symptoms and morbidity rates were about two times higher, and mobility limitation was three times higher, in older adult women than in their male counterparts. Moreover, older adult women use outpatient services more than older adult men because they are more vulnerable to low economic income, poor physical and mental health, react more sensitively to stress, and perceive their health conditions more negatively [26].
In summary, thus far, few studies have analyzed medical service use in Korean older adult women using Andersen’s model. Nonetheless, against the increasing importance of the health of this population owing to the aging population phenomenon, we have been observing a steady surge in the number of studies on older adult health. Despite such augmentation, few studies have been devoted to examining the factors associated with outpatient service use within the context of specific chronic diseases [16].
Therefore, this study aimed to analyze the factors affecting outpatient service use by Korean older adult women with degenerative arthritis using Andersen’s model. The final aim of this study was to help enable Korean older adult women to lead healthier lives and experience greater societal equality regarding access to healthcare. In addition, data on outpatient service use patterns may prove useful for stakeholders in the development of interventions for improving the health of older adult women with degenerative arthritis, as well as assist those interested in improving resource allocation in medical settings in Korea. In this study, a conceptual framework for outpatient service use based on Andersen’s model was proposed, which is shown in Figure 1.
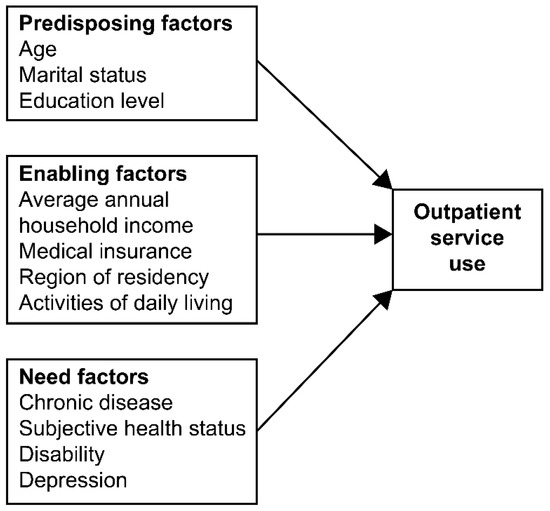
Figure 1.
The modified model based on Andersen’s model.
2. Methods
2.1. Study Design
This was a descriptive, cross-sectional study.
2.2. Samples
The inclusion criteria of this study were being of the female sex, aged 65 years or older, having degenerative arthritis, and having visited the outpatient department of two university hospitals in Seoul, Korea. Those under 65 years of age were excluded. To determine the number of participants required for logistic regression analysis, the G*power version 3.1 program (Heinrich Heine Universität Düsselforf, Schwaderer, Germany) was used with the significance level set to 0.05, an effect size for odds ratio (OR) of 1.72, and the power set at 0.8. The results showed an ideal sample size of 177. The final valid sample of 232 participants was deemed sufficient to ensure statistical power.
2.3. Data Collection
The researchers submitted a research plan to the institutional review boards of the two university hospitals with information on the study purpose and procedures. The study was reviewed and approved by the Biomedical Research Institute of the Seoul National University Hospital and the Institutional Review Board of the Chung-Ang University Hospital (approval numbers: H-1703-019-836, 1740-006-278, respectively).
Data were collected from 3 April to 27 May 2017. Prior to participation, all potential study participants received explanations of the study’s purposes and procedures, the fact that all personal information collected would be kept confidential, and that participation was voluntary. All participants provided verbal informed consent. This research used a self-reported questionnaire, but whenever participants presented any difficulties in filling out the questionnaire, the researcher read the questions to them aloud, to which study participants answered. In total, 250 questionnaires were distributed, 248 (99%) were returned, and 232 (93%) were finally used for data analysis. Data from 16 questionnaires were deleted because they had items left blank, hindering the ability to use them in the statistical analysis process.
2.4. Measurements
The questionnaire used in this study comprised 43 questions: 9 on sociodemographic characteristics, 7 on activities of daily living (ADL), 10 on instrumental activities of daily living (IADL), 15 on depression, and 2 on outpatient service use.
2.4.1. Activities of Daily Living
The 7-item K-ADL, a tool modified by Won et al. [27] for suitability with the Korean culture based on Katz et al. [28], was used to assess ADL. It includes one item each for dressing, bathing, eating, toileting, transfer, continence, and washing the face and hands, and it is answered on a 3-point scale (1, perfect self-reliance; 2, partial dependence; 3, complete dependence). Total scores range from 7 to 21 points, where the higher the score, the higher the dependence. In Won et al.’s [27] study, the Cronbach’s α of this scale was 0.94; in this study, it was 0.78.
2.4.2. Instrumental Activities of Daily Living
The 10-item K-IADL, a tool modified by Won et al. [27] for suitability with the Korean culture based on Lawton and Brody [29], was used to assess I-ADL. It includes one item each for grooming, housework, preparing meals, laundry, short trips, using transportation, shopping, managing money, using the telephone, and taking medicine, and it is answered on a 3-point scale (1, perfect self-reliance; 2, partial dependence; 3, complete dependence). Total scores range from 10 to 30 points, where the higher the score, the higher the dependence. In Won et al.’s [27] study, the Cronbach’s α of this scale was 0.94; in this study, it was 0.91.
2.4.3. Depression
To measure the level of depression in older adults, the 15-item Korean version of the Geriatric Depression Scale, which was adapted by Kee [30] based on the Short Form Geriatric Depression Scale developed by Yesavage et al. [31], was used. Items are answered on a dichotomous scale (1, yes; 0, no), with total scores ranging from 0 to 15 points. For this tool, a score within the range of 0–4 points is considered as indicating a healthy mental status, 5–9 points as mild depression, and 10–15 points as severe depression. Moreover, 5 of the 15 questions were negative, so they required reverse coding, with an answer of “no” counting as 1 point. In Kee’s [30] study, the Cronbach’s α of this scale was 0.88; in this study, it was 0.63.
Of note, in this study, the participants’ responses regarding their mood conditions may not be consistent because of the varying severity of the disease in the sample, which comprised older adult female outpatients with degenerative arthritis. However, the Cronbach’s α of the scale for this study was still deemed as a valid descriptor of the reliability of the scale.
2.5. Data Analysis
For data analysis, the SPSS program, version 24.0 (IBM Corp., Armonk, NY, USA), was used. The predisposing, enabling, and need factors were analyzed using frequency, percentage, mean, and standard deviation. The differences in outpatient service use according to the three factors were analyzed using χ2 test or t-test. To analyze the factors affecting outpatient service use by the three types of factors, multiple logistic regression analysis was used. In this study, the variance inflation factor among independent variables was checked. It confirmed that there were no multicollinearity problems among the study variables.
3. Results
3.1. Demographic Characteristics
In total, there were 232 participants, and all were older adult women; 162 (69.8%) of them used outpatient services from 1 March 2016 to 28 February 2017. The average frequency of outpatient service use in the past year was eight times.
The results of analyzing the participants’ sociodemographic characteristics according to the predisposing, enabling, and need factors are shown in Table 1. Regarding age, there were 168 (72.4%) younger-older adults (i.e., aged 65–75 years) and 64 (27.6%) older-older adults (i.e., aged 75 years or older); the average age was 72.11 years. For average annual household income, 126 (54.3%) participants earned less than 30 million won, with an average of 33.5 million won. In total, 182 (78.4%) participants had other chronic diseases aside from degenerative arthritis.

Table 1.
Participants’ sociodemographic characteristics.
3.2. Differences in the Predisposing, Enabling, and Need Factors Related to Outpatient Service Use
The results of analyzing differences in outpatient service use by the participants’ predisposing, enabling, and need factors are shown in Table 2. Among the predisposing factors, regarding age, 73.8% of the younger-older adults and 59.4% of the older-older adults used outpatient services; the difference between them was statistically significant (χ2 = 4.58, p = 0.038).

Table 2.
Differences in outpatient service use by predisposing, enabling, and need factors.
Among the enabling factors, regarding the region of residency, 76.7% of those living in Seoul and 60.6% of those in other metropolitan cities/provinces used outpatient services; the difference between them was statistically significant (χ2 = 6.97, p = 0.009).
Among the need factors, regarding other chronic diseases aside from degenerative arthritis, 75.8% of those with other chronic diseases and 48.0% of those without other chronic diseases used outpatient services; the difference between them was statistically significant (χ2 = 14.41, p < 0.001).
Regarding disability, 75.1% of those without a disability and 35.5% of those with a disability used outpatient services; the difference between these groups was statistically significant (χ2 = 20.03, p < 0.001).
Finally, there was no significant difference between groups in terms of depression (t = 0.58, p = 0.566), with a mean score of 8.57 (±3.20) for those who used outpatient services and a score of 8.31 (±2.78) for those who did not.
3.3. Factors Influencing Outpatient Service Use
The results of the multivariate logistic regression analyses for the factors affecting the participants’ outpatient service use are shown in Table 3. The result regarding −2 log-likelihood was 179.87, and the explanatory power of the data, demonstrated using Nagelkerke R2, was 0.36.

Table 3.
Multiple logistic regression analysis results for the factors affecting outpatient service use.
In Model 3, being a younger-older adult (OR = 5.53, p < 0.001) and having an average annual household income of more than 30 million won (OR = 5.64, p < 0.001), other chronic diseases aside from degenerative arthritis (OR = 11.06, p < 0.001), and no disability (OR = 3.56, p = 0.016) showed a significant effect on outpatient service use. Moreover, those with other chronic diseases aside from degenerative arthritis had an OR of 11.06 times higher than that of participants without other chronic diseases, and participants without disabilities had an OR of 3.56 times higher than that of individuals with a disability.
4. Discussion
Using Andersen’s model, this study analyzed the effects of predisposing, enabling, and need factors on outpatient service use by Korean older adult women with degenerative arthritis. The results showed that age (predisposing factor), average annual household income (enabling factor), and other chronic diseases aside from degenerative arthritis and disability (need factors) affected outpatient service use.
First, the difference between age groups was statistically significant, with 73.8% of the younger-older adults and 59.4% of the older-older adults using outpatient services. This is consistent with prior studies, which showed that outpatient service use rates were higher among younger-older adults [32,33]. Hence, it is expected that the younger the older adult, the better the health functioning, and the higher the outpatient service use rate; this may owe to younger-older adult women with degenerative arthritis experiencing less physical discomfort amid the processes required for using outpatient services (e.g., traveling to the medical institution).
Research has shown that as people age (mean age 76.0 ± 6.9), the fewer preventive services they utilize, and the less they talk about their health problems to medical staff, which may be because of the patient’s acceptance of their health deterioration, deeming it as a natural aging phenomenon and that health status restoration is a non-important issue [34]. Therefore, it seems necessary to encourage older adult women with degenerative arthritis to reduce their medical costs by implementing preventive efforts, which can be operationalized using the delivery of health checkup services to help them recognize the seriousness of the disease.
Second, married participants showed higher outpatient service use rates. This finding is similar to prior evidence, which showed that the higher the support from the family, the higher the use of outpatient services [35,36]. Nevertheless, the finding of the current study differs from prior research that applied Andersen’s model and that was conducted with Korean older adults, which showed that people who do not live with their children are more likely to use outpatient services [3]. These results may be because, although older adult women may desire to receive medical services, those who lack family support may be left unattended because they are hindered in their accessibility to healthcare services. Therefore, it may be necessary to increase accessibility support for outpatient services among Korean older adult women with degenerative arthritis who do not live with their spouses or children.
Third, the region of residency had a statistically significant effect on outpatient service use. Prior research showed that the reason behind the influence of the region of residency on medical service use may lie in its relationship with the medical environment, including the reasons why people access and search for medical institutions, the area of residency, and the number of hospitals in the region [37]. This finding is also consistent with the finding that older adult women with degenerative arthritis who live in urban areas spend more money on healthcare [21].
Fourth, the results showed that an average annual household income of 30 million won or more had a statistically significant effect on outpatient service use, as those with such income showed higher use. This finds consistency with the results of a study that applied Andersen’s model [3]. In another study, it was shown that older women with higher average annual household income actively accepted health information and were more willing to directly practice the information they received, while their counterparts with lower average income more restrictively engaged in changing their health behaviors owing to daily life-related limitations and stress [38].
Fifth, a major variable affecting outpatient service use in the current study was having other chronic diseases aside from degenerative arthritis, as those with multiple chronic diseases showed higher outpatient service use. This finding concurs with the literature, which shows that older adult women with various chronic diseases have higher outpatient service use rates [3,21,39,40]. The fact that older adults have many chronic diseases may lead them to desire to receive various, and often complex, medical services, making a higher outpatient service use rate a natural consequence of such desire/services [33,41]. Therefore, older adult women with degenerative arthritis may require the delivery of continuous health checkup services, personalized treatment, and disease management. For this, it may be necessary to provide them with preventive medical services and long-term disease management, which can be operationalized using the promotion of a continuous connection between patients and outpatient services at medical institutions.
Sixth, older adult women with degenerative arthritis who did not have a disability showed higher outpatient service use, and this was a major affecting variable. It is assumed that the outpatient service use rate was low among those with disabilities because they may feel more uncomfortable performing their ADL. In a study using Andersen’s model, conducted with pre-older adults with disability, outpatient service use was found to be very high in patients with chronic diseases [42]. Although a direct comparison between the current study and this cited study is difficult owing to sample differences, this still indicates that the need factor has a significant effect on outpatient service use.
Lastly, our study showed that older women with degenerative arthritis who used outpatient services had slightly higher depression levels than those who did not. A meta-analysis reported that some chronic diseases including arthritis were related to risk factors for depression in older adults [43]. This is believed to be because the proportion of older adult women with chronic disease who used outpatient services was higher than those who did not. Depression is associated with chronic diseases and is one of the major factors in healthcare utilization and costs [44]. Therefore, more attention needs to be diverted toward preventing and managing chronic diseases in older adults.
In Model 3 of the logistic regression analysis of the current study, the influencing factors of outpatient service use were age, average annual household income, having other chronic diseases aside from degenerative arthritis, and disability. Moreover, the need factors had more influence than the predisposing factors and enabling factors. These results were consistent with those from two other studies, which showed chronic disease as an important factor influencing medical service use in older adults [3,21].
4.1. Limitations
First, as this cross-sectional study surveyed only older adult women who frequented two university hospitals in Seoul, generalizations should be made with caution. Second, because this study included a self-reported questionnaire, attention should be paid to potential objectification. Future research should use qualitative (e.g., interviews and participant observation) and quantitative research methods concomitantly, as this will enable a more comprehensive understanding of the studied phenomena and enrich the current findings. Finally, this cross-sectional survey study collected data over a specific, short-term period; future studies should longitudinally analyze the factors affecting outpatient service use.
4.2. Theoretical Implications
Since Andersen’s model is an integrated model that considers internal and external factors at the individual level, it has been frequently applied in research on medical service use, as mentioned beforehand. In this study, its use was meaningful in that it allowed for the identification of the factors affecting outpatient service use in Korean older adult women with chronic diseases, a setting in which the application of this model for the analyses of the aforementioned variables has rarely occurred. These data may be useful for stakeholders who research the variables related to healthy living in Korean older adult women and may eventually translate into actual healthier lives for this population.
4.3. Practical Implications
The findings and discussions in this study suggest the need for improvements in interventional strategies regarding access to outpatient service use for those who are underprivileged. First, the national government should come up with measures to improve the medical service support system, allowing older-older adults to receive continuous health checkups and individualized disease management services. Second, among older adults with disabilities, it may be necessary to expand policy support for hospital accompaniment services in order to ensure that this population can access outpatient care.
Third, it seems essential to expand the policies on visiting care for chronic disease prevention and/or to develop and apply nursing intervention programs related to such prevention measures. Finally, the data from this paper may prove meaningful to help older adult women in Korea experience greater social equality in access to healthcare.
5. Conclusions
In this study conducted with 232 Korean older adult women with degenerative arthritis, Andersen’s model was used to analyze the factors affecting outpatient service use. In particular, the factors with the largest influence were the need factors. Hence, and confirming prior literature [16], the need factors in Andersen’s model were major factors influencing outpatient service use. This scientific assumption may also be applicable to Korean older adult women with degenerative arthritis.
The results of this study suggest that health promotion interventions for Korean older adult women should be devoted to predicting outpatient service use according to the patient’s characteristics. For the future, we recommend studies that can reproduce our analyses while using larger samples and longitudinally analyzing the study variables.
Author Contributions
Conceptualization, E.E.S. and S.J.; methodology, S.J.; software, S.J.; validation, E.E.S.; formal analysis, S.J.; investigation, S.J.; resources, S.J.; data curation, S.J.; writing—original draft preparation, S.J.; writing—review and editing, E.E.S.; visualization, E.E.S.; supervision, E.E.S.; funding acquisition, E.E.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by the BK21 four project (Center for Human-Caring Nurse Leaders for the Future); the Ministry of Education (MOE, Korea); and the National Research Foundation of Korea (NRF).
Institutional Review Board Statement
This study was reviewed and approved by the Biomedical Research Institute of the Seoul National University Hospital and the Institutional Review Board of the Chung-Ang University Hospital (approval numbers: H-1703-019-836, 1740-006-278).
Informed Consent Statement
Informed consent was obtained from all participants involved in the study.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
We give thanks to the patients who participated in the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Statistics Korea. Population Status and Prospects of the World and Korea. Available online: http://kostat.go.kr/portal/korea/kor_nw/1/1/index.board?bmode=read&aSeq=377226 (accessed on 10 March 2022).
- Kim, B.R.; Hwang, H.H. Analysis of Major Factors Affecting the Quality of Life of the Elderly in Korea in Preparation for a Super-Aged Society. Int. J. Environ. Res. Public Health 2022, 19, 9618. [Google Scholar] [CrossRef]
- Lee, W.S. A longitudinal study on the use of medical services. Soc. Welf. Policy 2018, 45, 5–37. [Google Scholar]
- Considine, J.; Smith, R.; Hill, K.; Gannon, J.; Behm, C.; Wellington, P. Older peoples’ experience of accessing emergency care. Australas. Emerg. Nurs. J. 2010, 13, 61–69. [Google Scholar] [CrossRef]
- Chin, Y.R.; Lee, I.S.; Lee, H.Y. Effects of hypertension, diabetes, and/or cardiovascular disease on health-related quality of life in elderly Korean individuals: A population-based cross-sectional survey. Asian Nurs. Res. 2014, 8, 267–273. [Google Scholar] [CrossRef]
- Zheng, D.D.; Loewenstein, D.A.; Christ, S.L.; Feaster, D.J.; Lam, B.L.; McCollister, K.E.; Curiel-Cid, R.E.; Lee, D.J. Multimorbidity patterns and their relationship to mortality in the US older adult population. PLoS ONE 2021, 16, e0245053. [Google Scholar] [CrossRef] [PubMed]
- Huber, M.; Knottnerus, J.A.; Green, L.; van der Horst, H.; Jadad, A.R.; Kromhout, D.; Leonard, B.; Lorig, K.; Loureiro, M.I.; van der Meer, J.W.; et al. How should we define health? BMJ 2011, 343, d4163. [Google Scholar] [CrossRef]
- Fu, X.; Sun, N.; Xu, F.; Li, J.; Tang, Q.; He, J.; Wang, D.; Sun, C. Influencing factors of inequity in health services utilization among the elderly in China. Int. J. Equity Health 2018, 17, 144. [Google Scholar] [CrossRef] [PubMed]
- Shane Anderson, A.; Loeser, R.F. Why is osteoarthritis an age-related disease? Best Pract. Res. Clin. Rheumatol. 2010, 24, 15–26. [Google Scholar] [CrossRef] [PubMed]
- Oh, J.H.; Yi, M.S. Structural equation modeling on quality of life in older adults with osteoarthritis. J. Korean Acad. Nurs. 2014, 44, 75–85. [Google Scholar] [CrossRef]
- Ayis, S.; Dieppe, P. The natural history of disability and its determinants in adults with lower limb musculoskeletal pain. J. Rheumatol. 2009, 36, 583–591. [Google Scholar] [CrossRef]
- Rosemann, T.; Grol, R.; Herman, K.; Wensing, M.; Szecsenyi, J. Association between obesity, quality of life, physical activity, and health service utilization in primary care patients osteoarthritis. Int. J. Behav. Nutr. Phys. Act. 2008, 5, 4. [Google Scholar] [CrossRef]
- Do, S.R.; Shin, E.S. Increased use of medical care by the elderly and the implications. Health Welf. Issue Focus 2012, 167, 1–8. [Google Scholar]
- Kahng, S.K. The trajectory of outpatient medical service use and its predictors: Focusing on age variations. Korean Acad. Soc. Welf. 2010, 62, 83–108. [Google Scholar] [CrossRef]
- Song, T.M. An Anderson model approach to the mediation effect of stress-vulnerability factors affecting the use of outpatient care by the elderly. Health Soc. Welf. Rev. 2013, 33, 547–576. [Google Scholar]
- Soleimanvandiazar, N.; Mohaqeqi Kamal, S.H.; Sajjadi, H.; Ghaedamini Harouni, G.; Karimi, S.E.; Djalalinia, S.; Setareh Forouzan, A. Determinants of outpatient health service utilization according to Andersen’s behavioral model: A systematic scoping review. Iran. J. Med. Sci. 2020, 45, 405–424. [Google Scholar]
- Andersen, R.M. Revisiting the behavioral model and access to medical care: Does it matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Andersen, R.; Newman, J.F. Societal and individual determinants of medical care utilization in the United States. Milbank Meml. Fund Q. 1973, 51, 95–124. [Google Scholar] [CrossRef]
- Brown, C.; Barner, J.; Bohman, T.; Richards, K. A multivariate test of an expanded Andersen Health Care utilization model for complementary and alternative medicine (CAM) use in African Americans. J. Altern. Complement. Med. 2009, 15, 911–919. [Google Scholar] [CrossRef]
- Liu, L.F. The health heterogeneity of and health care utilization by the elderly in Taiwan. Int. J. Environ. Res. Public Health 2014, 11, 1384–1397. [Google Scholar] [CrossRef]
- Lo, T.K.; Parkinson, L.; Cunich, M.; Byles, J. Factors associated with the health care cost in older Australian women with arthritis: An application of the Andersen’s Behavioural Model of Health Services Use. Public Health 2016, 134, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.S. A Longitudinal Study on the Use of Medical Services for the Elderly Based on the Anderson Behavioral Model. Doctoral Dissertation, University of Konkuk, Seoul, Republic of Korea, 2015. [Google Scholar]
- Shin, M.S.; Lee, W.J. Health behavior associated with outpatient utilization. J. Korea Contents Assoc. 2013, 13, 342–353. [Google Scholar] [CrossRef]
- Statistics Korea. Women’s Life through Statistics. Available online: https://kostat.go.kr/portal/korea/kor_nw/1/1/index.board?bmode=read&aSeq=346959 (accessed on 8 July 2022).
- Kim, E.J.; Kim, Y.H. Predictors of successful aging in Korean older women based on successful aging theory (SAT). Korean J. Women Health Nurs. 2011, 17, 378–387. [Google Scholar] [CrossRef]
- Zunzunegui, M.V.; Alvarado, B.E.; Béland, F.; Vissandjee, B. Explaining health differences between men and women in later life: A cross-city comparison in Latin America and the Caribbean. Soc. Sci. Med. 2009, 68, 235–242. [Google Scholar] [CrossRef]
- Won, C.W.; Rho, Y.G.; Sunwoo, D.; Lee, Y.S. The validity and reliability of Korean Instrumental Activities of Daily Living (K-IADL) scale. J. Korean Geriatr. Soc. 2002, 6, 273–280. [Google Scholar]
- Katz, S.J.; Kessler, R.C.; Lin, E.; Wells, K.B. Medication management of depression in the United States and Ontario. J. Gen. Intern. Med. 1998, 13, 77–85. [Google Scholar] [CrossRef]
- Lawton, M.P.; Brody, E.M. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Kee, B.S. A preliminary study for the standardization of Geriatric Depression Scale Short Form-Korea Version. J. Korean Neuropsychiatr. Assoc. 1996, 35, 298–306. [Google Scholar]
- Yesavage, J.A.; Brink, T.L.; Rose, T.L.; Lum, O.; Huang, V.; Adey, M.; Leirer, V.O. Development and validation of a geriatric depression screening scale: A preliminary report. J. Psychiatr. Res. 1982, 17, 37–49. [Google Scholar] [CrossRef] [PubMed]
- Jeon, H.S.; Kahng, S.K. The effects of medical service utilizations on life satisfaction among the elderly: Focusing on the moderating effects of the presence of chronic illnesses. J. Korea Gerontol. Soc. 2011, 31, 1247–1264. [Google Scholar]
- Lee, M.J. A longitudinal study on older adults’ use of medical services. Soc. Welf. Policy 2009, 36, 201–223. [Google Scholar]
- Sarkisian, C.A.; Hays, R.D.; Mangione, C.M. Do older adults expect to age successfully? The association between expectations regarding aging and beliefs regarding healthcare seeking among older adults. J. Am. Geriatr. Soc. 2002, 50, 1837–1843. [Google Scholar] [PubMed]
- Kang, S.H.; Wallace, N.T.; Hyun, J.K.; Morris, A.; Coffman, J.; Bloom, J.R. Social networks and their relationship to mental health service use and expenditures among Medicaid beneficiaries. Psychiatr. Serv. 2007, 58, 689–695. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.K.; Lee, M. Factors associated with health services utilization between the years 2010 and 2012 in Korea: Using Andersen’s Behavioral model. Osong Public Health Res. Perspect. 2016, 7, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Chi, I.; Zhang, K.; Guo, P. Comparison of health services use by Chinese urban and older rural adults in Yunnan Province. Geriatr. Gerontol. Int. 2006, 6, 260–269. [Google Scholar] [CrossRef]
- Rhee, C.W. Health status and self-management barriers in people with diabetes—A comparison by Medicaid Beneficiary Status. Korean Acad. Soc. Welf. 2008, 60, 231–251. [Google Scholar] [CrossRef]
- Baik, O.M. Factors associated with functional health outcomes in community-dwelling older adults: Applying Andersen’s revised model. J. Commun. Welf. 2011, 38, 1–27. [Google Scholar]
- Zhang, X.; Wu, Q.; Shao, Y.; Fu, W.; Liu, G.; Coyte, P.C. Socioeconomic inequities in health care utilization in China. Asia Pac. J. Public Health 2015, 27, 429–438. [Google Scholar] [CrossRef] [PubMed]
- Jang, Y.; Kim, G.; Chiriboga, D.A. Health, healthcare utilization, and satisfaction with service: Barriers and facilitators for older Korean Americans. J. Am. Geriatr. Soc. 2005, 53, 1613–1617. [Google Scholar] [CrossRef] [PubMed]
- Yoon, J.S. Analysis on the differences in outpatient service use among the pre-elderly with disability applying the Anderson model. DCS 2019, 20, 973–980. [Google Scholar] [CrossRef]
- Huang, C.Q.; Dong, B.R.; Lu, Z.C.; Yue, J.R.; Liu, Q.X. Chronic diseases and risk for depression in old age: A meta-analysis of published literature. Ageing Res. Rev. 2010, 9, 131–141. [Google Scholar] [CrossRef]
- Luber, M.P.; Meyers, B.S.; Williams-Russo, P.G.; Hollenberg, J.P.; DiDomenico, T.N.; Charlson, M.E.; Alexopoulos, G.S. Depression and service utilization in elderly primary care patients. Am. J. Geriatr. Psychiatry 2001, 9, 169–176. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).