Elevated All-Cause Mortality among Overweight Older People: AI Predicts a High Normal Weight Is Optimal
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Participants, Measurements, and AI Analysis
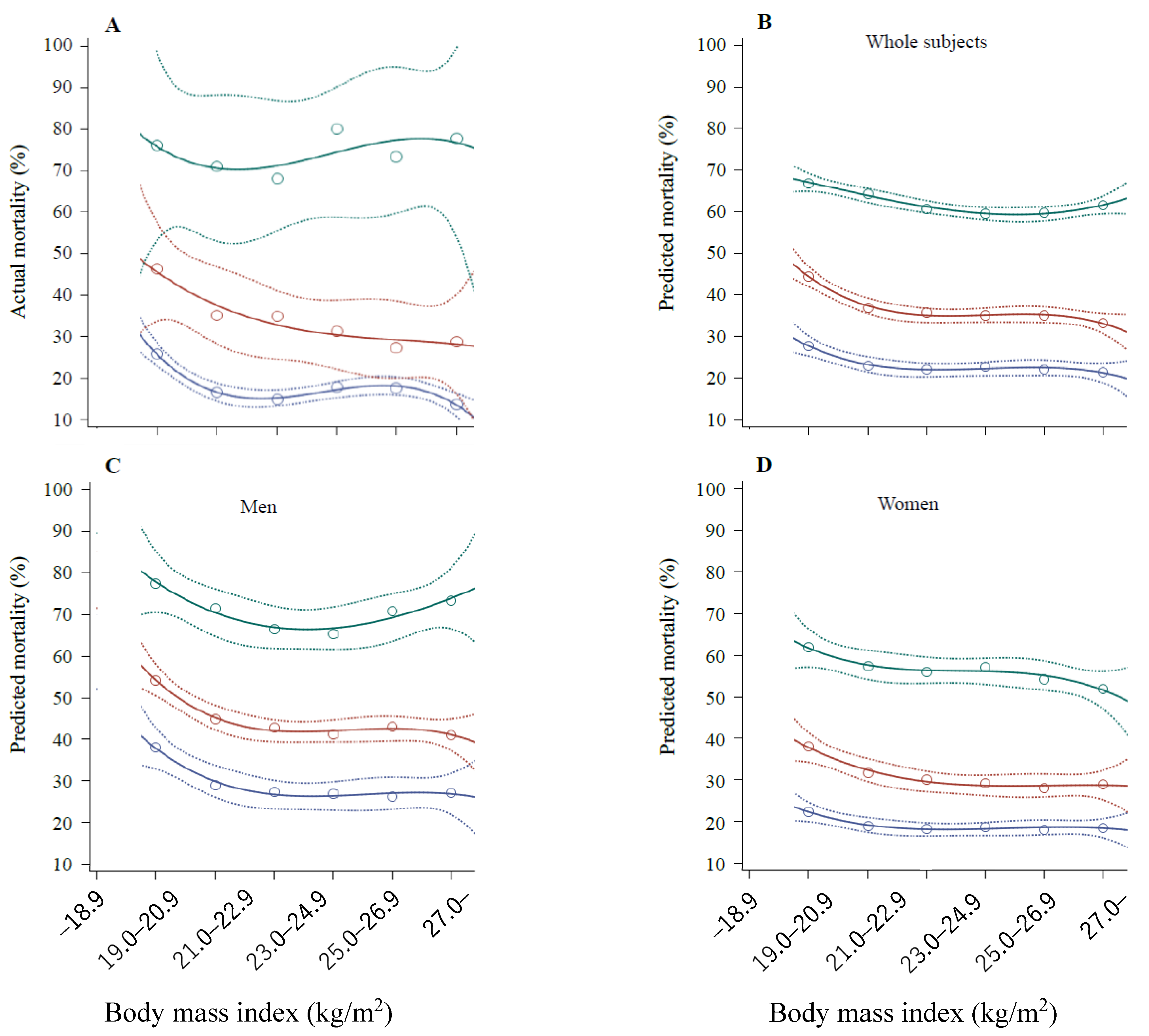
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Flegal, K.M.; Kit, B.K.; Orpana, H.; Graubard, B.I. Association of all-cause mortality with overweight and obesity using standard body mass index categories: A systematic review and meta-analysis. JAMA 2013, 309, 71–82. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.S.; Auyeung, T.W.; Chau, P.P.; Hui, E.; Chan, F.; Chi, I.; Woo, J. Obesity can benefit survival-a 9-year prospective study in 1614 Chinese nursing home residents. J. Am. Med. Dir. Assoc. 2014, 15, 342–348. [Google Scholar] [CrossRef] [PubMed]
- Veronese, N.; Cereda, E.; Solmi, M.; Fowler, S.A.; Manzato, E.; Maggi, S.; Manu, P.; Abe, E.; Hayashi, K.; Allard, J.P.; et al. Inverse relationship between body mass index and mortality in older nursing home residents: A meta-analysis of 19,538 elderly subjects. Obes. Rev. 2015, 16, 1001–1015. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karampela, I.; Chrysanthopoulou, E.; Christodoulatos, G.S.; Dalamaga, M. Is There an Obesity Paradox in Critical Illness? Epidemiologic and Metabolic Considerations. Curr. Obes. Rep. 2020, 9, 231–244. [Google Scholar] [CrossRef] [PubMed]
- Bosello, O.; Vanzo, A. Obesity paradox and aging. Eat Weight Disord. 2021, 26, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; Van Iterson, E.H.; Laffin, L.J. The obesity paradox in heart failure: What is the role of cardiorespiratory fitness? Cleve. Clin. J. Med. 2021, 88, 449–458. [Google Scholar] [CrossRef] [PubMed]
- Hasanzad, M.; Aghaei Meybodi, H.R.; Sarhangi, N.; Larijani, B. Artificial intelligence perspective in the future of endocrine diseases. J. Diabetes Metab. Disord. 2022, 21, 971–978. [Google Scholar] [CrossRef] [PubMed]
- Corti, C.; Cobanaj, M.; Marian, F.; Dee, E.C.; Lloyd, M.R.; Marcu, S.; Dombrovschi, A.; Biondetti, G.P.; Batalini, F.; Celi, L.A.; et al. Artificial intelligence for prediction of treatment outcomes in breast cancer: Systematic review of design, reporting standards, and bias. Cancer Treat. Rev. 2022, 108, 102410. [Google Scholar] [CrossRef] [PubMed]
- Antonelli, G.; Badalamenti, M.; Hassan, C.; Repici, A. Impact of artificial intelligence on colorectal polyp detection. Best Pract. Res. Clin. Gastroenterol. 2021, 52–53, 101713. [Google Scholar] [CrossRef] [PubMed]
- Kodera, S.; Akazawa, H.; Morita, H.; Komuro, I. Prospects for cardiovascular medicine using artificial intelligence. J. Cardiol. 2022, 79, 319–325. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.kuhs.ac.jp/research/news/details_00248.htmlYamato (accessed on 16 April 2022).
- Available online: http://www.city.yamato.lg.jp/web/kouhou/n20181218-2.html (accessed on 16 April 2022).
- Nakajima, K.; Yuno, M.; Tanaka, K.; Nakamura, T. High Aspartate Aminotransferase/Alanine Aminotransferase Ratio May Be Associated with All-Cause Mortality in the Elderly: A Retrospective Cohort Study Using Artificial Intelligence and Conventional Analysis. Healthcare 2022, 10, 674. [Google Scholar] [CrossRef] [PubMed]
- Sony Network Communications, Prediction One. 2022. Available online: https://predictionone.sony.biz (accessed on 10 March 2022).
- Casola, S. What is Explainable Artificial Intelligence, and Why Is It Important for Predictive Models? 2021. Available online: https://www.explorium.ai/blog/what-is-explainable-artificial-intelligence-and-why-is-it-important-for-predictive-models/ (accessed on 1 April 2022).
- Gupta, A.; Kulkarni, M.; Mukherjee, A. Accurate prediction of B-form/A-form DNA conformation propensity from primary sequence: A machine learning and free energy handshake. Patterns 2021, 2, 100329. [Google Scholar] [CrossRef] [PubMed]
- Reps, J.M.; Ryan, P.; Rijnbeek, P.R. Investigating the impact of development and internal validation design when training prognostic models using a retrospective cohort in big US observational healthcare data. BMJ Open 2021, 11, e050146. [Google Scholar] [CrossRef] [PubMed]
- Hozawa, A.; Hirata, T.; Yatsuya, H.; Murakami, Y.; Kuriyama, S.; Tsuji, I.; Sugiyama, D.; Satoh, A.; Tanaka-Mizuno, S.; Miura, K.; et al. Association Between Body Mass Index and All-Cause Death in Japanese Population: Pooled Individual Participant Data Analysis of 13 Cohort Studies. J. Epidemiol. 2019, 29, 457–463. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsugane, S. Why has Japan become the world’s most long-lived country: Insights from a food and nutrition perspective. Eur. J. Clin. Nutr. 2021, 75, 921–928. [Google Scholar] [CrossRef] [PubMed]
- Schooling, C.M.; Lam, T.H.; Li, Z.B.; Ho, S.Y.; Chan, W.M.; Ho, K.S.; Tham, M.K.; Cowling, B.J.; Leung, G.M. Obesity, physical activity, and mortality in a prospective chinese elderly cohort. Arch. Intern. Med. 2006, 166, 1498–1504. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Contribution Order | Range of BMI (kg/m2) | Feature Importance 1 * | Feature Importance 2 ** |
|---|---|---|---|
| No-cross-validation model | |||
| Negative (protective) | 0.087 | ||
| 1 | 25.9–28.4 | 0.033 | |
| 2 | 22.7–23.6 | 0.032 | |
| 3 | 24.6–25.9 | 0.027 | |
| Positive (advancing) | |||
| 1 | 12.8–18.7 | 0.087 | |
| 2 | 23.6–24.6 | 0.026 | |
| 3 | 18.7–20.0 | 0.017 | |
| Total classification accuracy (AUC) 58.4% | |||
| Cross-validation model | |||
| Negative (protective) | 0.101 | ||
| 1 | 21.0–21.9 | 0.060 | |
| 2 | 22.7–23.6 | 0.049 | |
| 3 | 25.8–28.2 | 0.039 | |
| Positive (advancing) | |||
| 1 | 12.8–18.7 | 0.087 | |
| 2 | 18.7–20.0 | 0.019 | |
| 3 | 20.0–21.0 | 0.014 | |
| Total classification accuracy (AUC) 53.7% |
| Contribution Order | Range of BMI (kg/m2) | Feature Importance 1 * | Feature Importance 2 ** | Feature Importance 3 *** |
|---|---|---|---|---|
| No-cross-validation model | ||||
| Negative (protective) | 0.080 | Age: 0.192 Sex (men): 0.133 | ||
| 1 | 22.7–23.6 | 0.037 | ||
| 2 | 25.9–28.4 | 0.029 | ||
| 3 | 24.6–25.9 | 0.023 | ||
| Positive (advancing) | ||||
| 1 | 12.8–18.7 | 0.080 | ||
| 2 | 23.6–24.6 | 0.020 | ||
| 3 | 20.0–21.0 | 0.007 | ||
| Total classification accuracy (AUC) 73.7% | ||||
| Cross-validation model | ||||
| Negative (protective) | 0.099 | Age: 0.253 Sex (men): 0.129 | ||
| 1 | 22.7–23.6 | 0.046 | ||
| 2 | 25.8–28.2 | 0.035 | ||
| 3 | 24.6–25.8 | 0.025 | ||
| Positive (advancing) | ||||
| 1 | 12.8–18.7 | 0.091 | ||
| 2 | 23.6–24.6 | 0.024 | ||
| 3 | 18.7–20.0 | 0.018 | ||
| Total classification accuracy (AUC) 69.6% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nakajima, K.; Yuno, M. Elevated All-Cause Mortality among Overweight Older People: AI Predicts a High Normal Weight Is Optimal. Geriatrics 2022, 7, 68. https://doi.org/10.3390/geriatrics7030068
Nakajima K, Yuno M. Elevated All-Cause Mortality among Overweight Older People: AI Predicts a High Normal Weight Is Optimal. Geriatrics. 2022; 7(3):68. https://doi.org/10.3390/geriatrics7030068
Chicago/Turabian StyleNakajima, Kei, and Mariko Yuno. 2022. "Elevated All-Cause Mortality among Overweight Older People: AI Predicts a High Normal Weight Is Optimal" Geriatrics 7, no. 3: 68. https://doi.org/10.3390/geriatrics7030068
APA StyleNakajima, K., & Yuno, M. (2022). Elevated All-Cause Mortality among Overweight Older People: AI Predicts a High Normal Weight Is Optimal. Geriatrics, 7(3), 68. https://doi.org/10.3390/geriatrics7030068






