Exploring Meal Provision and Mealtime Challenges for Aged Care Residents Consuming Texture-Modified Diets: A Mixed Methods Study
Abstract
1. Introduction
2. Methods
2.1. Participants
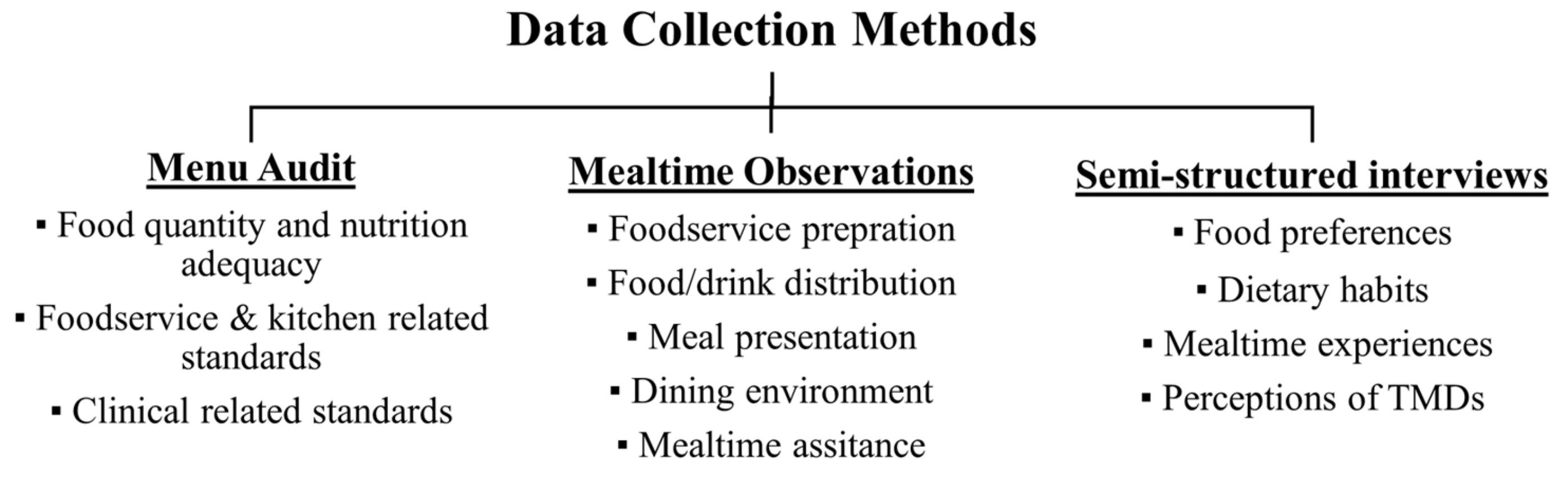
2.2. Data Collection
2.2.1. Menu Audit
2.2.2. Mealtime Observations
2.2.3. Semi-Structured Interviews
2.3. Data Analysis
3. Results
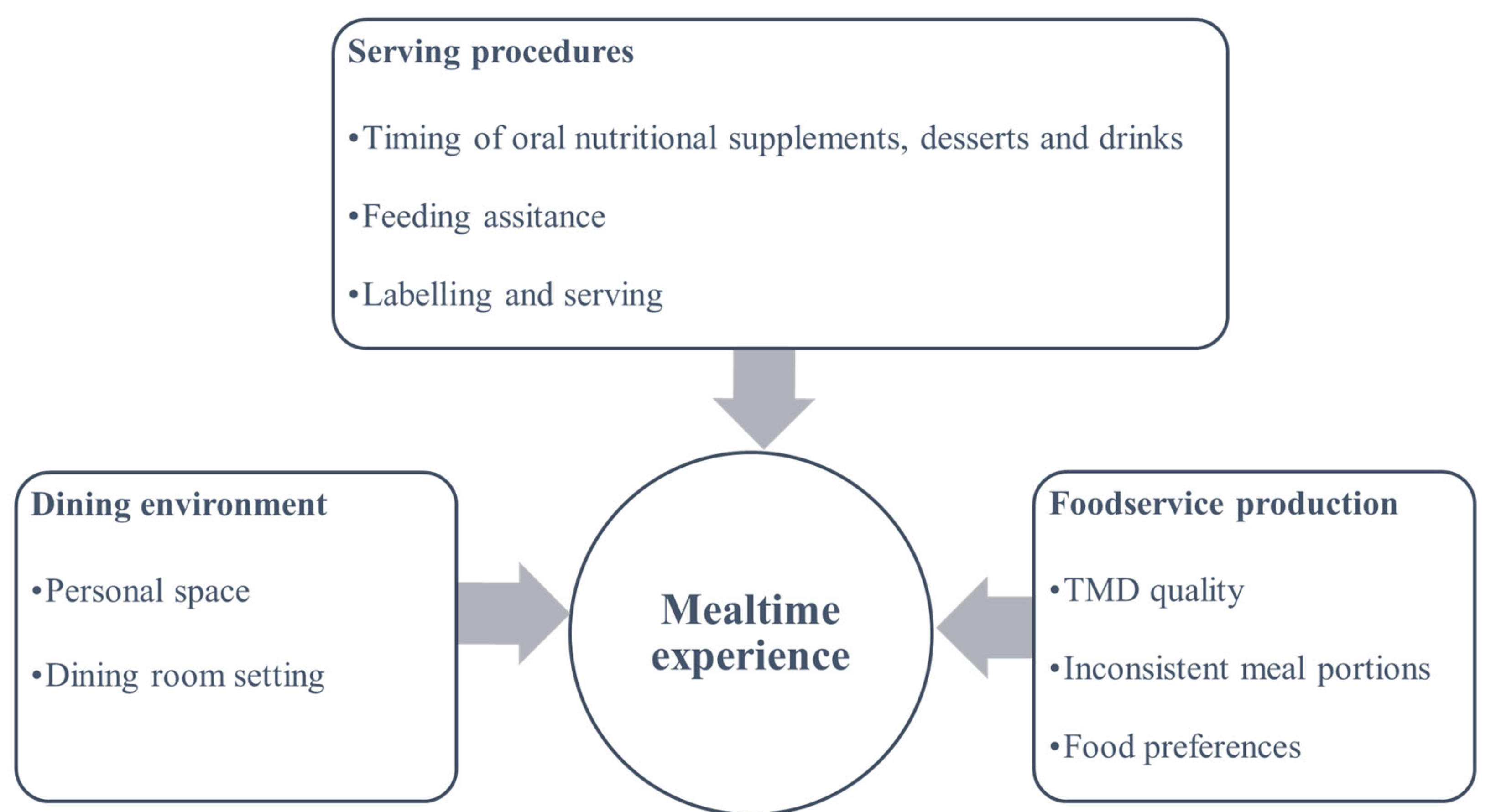
3.1. Foodservice Production
3.1.1. TMD Quality
“I miss home-cooked meals, the meals taste different here… And they don’t go well in my stomach”.(Resident 03)
“All the meals are the same, there is no variety”.Resident (04)
“At both lunch and dinner, protein component was not offered to a resident who was on a vegetarian pureed diet, but only vegetable and carbohydrate portions”.(Observation)
“The old meals (before introducing moulding) didn’t look very nice; I probably won’t eat it”.(HA 04)
“They (moulded meals) look like the real sausages, peas and corns, but sometimes I still can’t tell what meat it is”.(Resident 05)
“Even though the meal component looks like the actual food, the texture changes. It becomes flattened once the resident takes a spoonful off the plate. After they take a spoonful, the resident would realise that it is not the actual food and disappoint them”.(HA 01)
“Dinner meals served uncovered, scoops became flattened and looked unappetising”.(Observation)
3.1.2. Inconsistent Meal Portions
“I am not a fan of broccoli; they are so plain. I like tomatoes, but they don’t have it very often and I don’t know what I’m getting”(Resident 01)
“A dedicated green scoop was reported by the chef to be used for portioning protein, a smaller blue scoop for vegetable and carbohydrate portions, and an 89 mL ladle for soft and bite-sized protein or meal (e.g., macaroni and cheese) portions. However, during mealtime, there was no consistency in terms of serving portions and textures”.(Observation)
“They (residents) would usually have sliced peaches or prunes with their porridge (in the rest home dining rooms. But we don’t give those to the pureed (residents) on the other side (hospital-level). Sometimes the kitchen will have strawberry or orange puree, but not very often”.(HA 02)
“Commonly, 1/4—1/2 a cup of cut-up fruit was offered to soft and bite-sized diets, and 2–3 tablespoons of fruit purees were offered for pureed and minced and moist diets.”(Observation)
3.1.3. Food Preferences
“Sometimes he (a resident on a pureed diet) doesn’t eat anything, but when we give him ice cream, he would eat it”.(HA 05)
3.2. Serving Procedures
3.2.1. Timing of ONS, Desserts, and Drinks
“Some residents were fed ONS first, while others were fed ONS with the meal in between mouthfuls”.(Observation)
“Staff served the meals first, then prepare a jar of thickened beverages and poured a glass to those who required thickened fluids. During mid-meals, staff brought a can of thickening powder or a bottle of thickening gel on a trolley and added to pre-prepared coffee/tea”.(Observation)
“We usually make the (thickened) drinks at mealtimes. They (residents) do not often ask for drinks. We feed the drinks with foods”.(HA 04)
3.2.2. Feeding Assistance
“Some residents complain that the mash scoop is hot but other meal portions are cold”.(Nurse 02)
3.2.3. Labelling and Serving
“Pureed and minced and moist meals were sometimes observed to be tin-foiled and labelled by a marker and taken via trolley from the kitchen to dining room. However, the foil cover was occasionally removed by the chef in the kitchen when adding portions, rather than by the HAs during meal service”.(Observation)
3.3. Dining Environment
3.3.1. Personal Space
“I felt very different, like embarrassed when they gave me those soft foods (pureed meals). So, I do not like to go to the dining room”.(Resident 02)
3.3.2. Dining Room Setting
“Resident’s eating in the dining room… very noisy as staff were serving meals”.(Observation)
“Lunch was very disorganised; HAs have to work from memory when serving regular/soft and bite-sized meals as they need to consider resident preferences and whether or not they can tolerate certain foods (they also decide how much food to serve)”.(Observation)
“I don’t feel good when I see other people are eating different food. I don’t want to be different”.(Resident 04)
“He refused to have the puree and wanted the same food as the others. He eats more when he eats by himself in the room”.(Foodservice staff 03)
4. Discussion
4.1. Foodservice Production
4.2. Serving Procedures
4.3. Dining Environment
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cornwall, J.; Davey, J.A. Impact of Population Ageing in New Zealand on the Demand for Health and Disability Support Services, and Workforce Implications; A background paper completed for the Ministry of Health in June 2003 by the New Zealand Institute for Research on Ageing (NZiR); Ministry of Health: Wellington, New Zealand, 2004.
- Namasivayam, A.M.; Steele, C.M. Malnutrition and Dysphagia in Long-Term Care: A Systematic Review. J. Nutr. Gerontol. Geriatr. 2015, 34, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Carrión, S.; Cabré, M.; Monteis, R.; Roca, M.; Palomera, E.; Serra-Prat, M.; Rofes, L.; Clavé, P. Oropharyngeal dysphagia is a prevalent risk factor for malnutrition in a cohort of older patients admitted with an acute disease to a general hospital. Clin. Nutr. 2015, 34, 436–442. [Google Scholar] [CrossRef] [PubMed]
- Mann, T.; Heuberger, R.; Wong, H. The association between chewing and swallowing difficulties and nutritional status in older adults. Aust. Dent. J. 2013, 58, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Suominen, M.; Muurinen, S.; Routasalo, P.; Soni, H.; Suur-Uski, I.; Peiponen, A.; Finne-Soveri, H.; Pitkala, K.H. Malnutrition and associated factors among aged residents in all nursing homes in Helsinki. Eur. J. Clin. Nutr. 2005, 59, 578–583. [Google Scholar] [CrossRef]
- Norman, K.; Haß, U.; Pirlich, M. Malnutrition in Older Adults—Recent Advances and Remaining Challenges. Nutrients 2021, 13, 2764. [Google Scholar] [CrossRef]
- Engh, M.C.N.; Speyer, R. Management of Dysphagia in Nursing Homes: A National Survey. Dysphagia 2021, 37, 266–276. [Google Scholar] [CrossRef]
- Keller, H.H.; Chambers, L.; Niezgoda, H.; Duizer, L. Issues associated with the use of modified texture foods. J. Nutr. Health Aging 2012, 16, 195–200. [Google Scholar] [CrossRef]
- Vucea, V.; Keller, H.H.; Morrison, J.M.; Duizer, L.M.; Duncan, A.M.; Steele, C.M. Prevalence and Characteristics Associated with Modified Texture Food Use in Long Term Care: An Analysis of Making the Most of Mealtimes (M3) Project. Can. J. Diet. Pract. Res. 2019, 80, 104–110. [Google Scholar] [CrossRef]
- Miles, A.; Liang, V.; Sekula, J.; Broadmore, S.; Owen, P.; Braakhuis, A.J. Texture-modified diets in aged care facilities: Nutrition, swallow safety and mealtime experience. Australas. J. Ageing 2019, 39, 31–39. [Google Scholar] [CrossRef]
- Wu, X.S.; Braakhuis, A.J.; Miles, A. An Evaluation of Texture-Modified Diets Compliant with the International Dysphagia Diet Standardization Initiative in Aged-Care Facilities Using the Consolidated Framework for Implementation Research. Dysphagia 2022. [Google Scholar] [CrossRef]
- Curran, J.; Groher, M.E. Development and dissemination of an aspiration risk reduction diet. Dysphagia 1990, 5, 6–12. [Google Scholar] [CrossRef]
- O’Keeffe, S.T. Use of modified diets to prevent aspiration in oropharyngeal dysphagia: Is current practice justified? BMC Geriatr. 2018, 18, 167. [Google Scholar] [CrossRef]
- Wu, X.S.; Miles, A.; Braakhuis, A.J. Texture-modified diets, nutritional status and mealtime satisfaction: A systematic review. Healthcare 2021, 9, 624. [Google Scholar] [CrossRef]
- Cereda, E.; Pedrolli, C.; Klersy, C.; Bonardi, C.; Quarleri, L.; Cappello, S.; Turri, A.; Rondanelli, M.; Caccialanza, R. Nutritional status in older persons according to healthcare setting: A systematic review and meta-analysis of prevalence data using MNA ®. Clin. Nutr. 2021, 35, 1282–1290. [Google Scholar] [CrossRef]
- Tamura, B.K.; Bell, C.L.; Masaki, K.H.; Amella, E.J. Factors Associated with Weight Loss, Low BMI, and Malnutrition among Nursing Home Patients: A Systematic Review of the Literature. J. Am. Med. Dir. Assoc. 2013, 14, 649–655. [Google Scholar] [CrossRef]
- Fávaro-Moreira, N.C.; Krausch-Hofmann, S.; Matthys, C.; Vereecken, C.; Vanhauwaert, E.; Declercq, A.; Bekkering, G.E.; Duyck, J. Risk Factors for Malnutrition in Older Adults: A Systematic Review of the Literature Based on Longitudinal Data. Adv. Nutr. 2016, 7, 507–522. [Google Scholar] [CrossRef]
- Hickson, M. Malnutrition and ageing. Postgrad. Med. J. 2006, 82, 2–8. [Google Scholar] [CrossRef]
- O’Keeffe, M.; Kelly, M.; O’Herlihy, E.; O’Toole, P.W.; Kearney, P.M.; Timmons, S.; O’Shea, E.; Stanton, C.; Hickson, M.; Rolland, Y.; et al. Potentially modifiable determinants of malnutrition in older adults: A systematic review. Clin. Nutr. 2019, 38, 2477–2498. [Google Scholar] [CrossRef]
- Ministry of Health. Food and Nutrition Guidelines for Healthy Older People: A Background Paper; Minstry of Health: Wellington, New Zealand, 2013.
- Ullrich, S.; Buckley, J.; Crichton, J.; Esterman, A. An Exploratory Study of the Mealtime Experience of Older People with Dysphagia. J. Aging Res. Clin. Pract. 2014, 3, 229–236. [Google Scholar] [CrossRef]
- Wu, X.S.; Miles, A.; Braakhuis, A. Nutritional Intake and Meal Composition of Patients Consuming Texture Modified Diets and Thickened Fluids: A Systematic Review and Meta-Analysis. Healthcare 2020, 8, 579. [Google Scholar] [CrossRef]
- Niedert, K.C. Position of the American Dietetic Association: Liberalization of the diet prescription improves quality of life for older adults in long-term care. J. Am. Diet. Assoc. 2005, 105, 1955–1965. [Google Scholar] [CrossRef]
- Nijs, K.A.N.D.; De Graaf, C.; Siebelink, E.; Blauw, Y.H.; Vanneste, V.; Kok, F.J.; Van Staveren, W.A. Effect of Family-Style Meals on Energy Intake and Risk of Malnutrition in Dutch Nursing Home Residents: A Randomized Controlled Trial. J. Gerontol. 2006, 61, 935–942. [Google Scholar] [CrossRef]
- Carrier, N.; West, G.E.; Ouellet, D. Dining experience, foodservices and staffing are associated with quality of life in elderly nursing home residents. J. Nutr. Health Aging 2009, 13, 565–570. [Google Scholar] [CrossRef]
- Rowan-Robinson, K. Supportive interventions for enhancing dietary intake in malnourished or nutritionally at-risk adults. Int. J. Nurs. Pract. 2018, 24, e12580. [Google Scholar] [CrossRef]
- Reimer, H.D.; Keller, H.H. Mealtimes in nursing homes: Striving for person-centered care. J. Nutr. Elder. 2009, 28, 327–347. [Google Scholar] [CrossRef]
- Watkins, R.; Goodwin, V.A.; Abbott, R.A.; Hall, A.; Tarrant, M. Exploring residents’ experiences of mealtimes in care homes: A qualitative interview study. BMC Geriatr. 2017, 17, 141. [Google Scholar] [CrossRef]
- Spradley, J.P. Participant Observation; Holt, Rinehart and Winston: New York, NY, USA, 1980; ISBN 0030445019 9780030445019. [Google Scholar]
- Geertz, C. Thick Description: Toward an Interpretive Theory of Culture. In The Interpretation of Cultures: Selected Essays; Basic Books: New York, NY, USA, 1973; pp. 310–323. ISBN 9780786725007. [Google Scholar]
- Gilbert, G.N. Researching Social Life; Sage: London, UK; Newbury Park, CA, USA, 1993. [Google Scholar]
- Bowling, A. Research Methods in Health: Investigating Health and Health Services, 4th ed.; McGraw-Hill Education: Maidenhead, UK, 2014; ISBN 9780335262755. [Google Scholar]
- Dietitians, N.Z. Foodservice & Nutrition Audit. 2020. Available online: https://www.dietitiansboard.org.nz/wp-content/uploads/2020/12/Dietitians-Board-Annual-Report-2020-Online.pdf (accessed on 20 May 2022).
- Hsieh, H.-F.; Shannon, S.E. Three Approaches to Qualitative Content Analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef]
- Kaid, L.L. Content Analysis. In Measurement of Communication Behaviour; Emmert, P., Barker, L., Eds.; Longman: New York, NY, USA, 1989. [Google Scholar]
- Drisko, J.; Maschi, T. Qualitative Content Analysis. In Content Analysis; Oxford University Press: Oxford, UK, 2015; ISBN 9780190215491. [Google Scholar]
- Wu, X.S.; Yousif, L.; Miles, A.; Braakhuis, A. A Comparison of Dietary Intake and Nutritional Status between Aged Care Residents Consuming Texture-Modified Diets with and without Oral Nutritional Supplements. Nutrients 2022, 14, 669. [Google Scholar] [CrossRef]
- Wu, X.S.; Miles, A.; Braakhuis, A.J. The Effectiveness of International Dysphagia Diet Standardization Initiative—Tailored Interventions on Staff Knowledge and Texture-Modified Diet Compliance in Aged Care Facilities: A Pre-Post Study. Curr. Dev. Nutr. 2022, 6, nzac021. [Google Scholar] [CrossRef]
- Bauer, J.; Biolo, G.; Cederholm, T.; Cesari, M.; Cruz-Jentoft, A.J.; Morley, J.E.; Phillips, S.; Sieber, C.; Stehle, P.; Teta, D.; et al. Evidence-based recommendations for optimal dietary protein intake in older people: A position paper from the prot-age study group. J. Am. Med. Dir. Assoc. 2013, 14, 542–559. [Google Scholar] [CrossRef] [PubMed]
- Nowson, C.; O’Connell, S. Protein requirements and recommendations for older people: A review. Nutrients 2015, 7, 6874–6899. [Google Scholar] [CrossRef] [PubMed]
- Dorner, B.; Friedrich, E.K. Position of the Academy of Nutrition and Dietetics: Individualized Nutrition Approaches for Older Adults: Long-Term Care, Post-Acute Care, and other Settings. J. Acad. Nutr. Diet. 2018, 118, 724–735. [Google Scholar] [CrossRef] [PubMed]
- Seemer, J.; Kiesswetter, E.; Fleckenstein, D.; Gloning, M.; Lötzbeyer, T.M.; Ittermaier, S.; Sieber, C.; Wurm, S.; Volkert, D. Effects of an individualised nutritional intervention on dietary intake and quality of life in nursing homes residents with (risk of) malnutrition: An enable study. Clin. Nutr. ESPEN 2020, 40, 681–682. [Google Scholar] [CrossRef]
- Keller, H.; Duizer, L.M. What do consumers think of pureed food? Making the most of the indistinguishable food. J. Nutr. Gerontol. Geriatr. 2014, 33, 139–159. [Google Scholar] [CrossRef]
- Miles, A.; Dennison, K.; Amer Oad, M.; Shasha, L.; Royal, M. Consumer Satisfaction of Texture Modified Meals Served in Residential Aged-Care Facilities. Int. J. Food Sci. Nutr. Res. 2019, 1, 1. [Google Scholar] [CrossRef]
- Chisholm, A.; Jensen, J.; Field, P. Eating environment in the aged-care residential setting in New Zealand: Promoters and barriers to achieving optimum nutrition. Observations of the foodservice, menu and meals. Nutr. Diet. 2011, 68, 161–166. [Google Scholar] [CrossRef]
- Hill, C.; Clapham, R.P.; Buccheri, A.; Field, M.; Shee, A.W. Assessing adherence and exploring barriers to provision of prescribed texture modifications for dysphagia in a residential aged care facility in rural Australia. Int. J. Speech-Lang. Pathol. 2021, 24, 67–76. [Google Scholar] [CrossRef]
- Abbey, K.L.; Wright, O.R.L.; Capra, S. Menu planning in residential aged care—The level of choice and quality of planning of meals available to residents. Nutrients 2015, 7, 7580–7592. [Google Scholar] [CrossRef]
- Wang, D.; Everett, B.; Brunero, S.; Northall, T.; Villarosa, A.R.; Salamonson, Y. Perspectives of residents and staff regarding food choice in residential aged care: A qualitative study. J. Clin. Nurs. 2020, 29, 626–637. [Google Scholar] [CrossRef]
- Bennett, M.K.; Ward, E.C.; Scarinci, N.A. Mealtime management in Australian residential aged care: Comparison of documented, reported and observed care. Int. J. Speech-Lang. Pathol. 2015, 17, 451–459. [Google Scholar] [CrossRef]
- Milte, R.; Ratcliffe, J.; Chen, G.; Miller, M.; Crotty, M. Taste, choice and timing: Investigating resident and carer preferences for meals in aged care homes. Nurs. Health Sci. 2018, 20, 116–124. [Google Scholar] [CrossRef]
- Nichols, P.J.; Porter, C.; Hammond, L.; Arjmandi, B.H. Food intake may be determined by plate waste in a retirement living center. J. Am. Diet. Assoc. 2002, 102, 1142–1144. [Google Scholar] [CrossRef]
- Razalli, N.H.; Cheah, C.F.; Mohammad, N.M.A.; Abdul Manaf, Z. Plate waste study among hospitalised patients receiving texture-modified diet. Nutr. Res. Pract. 2021, 15, 655. [Google Scholar] [CrossRef]
- Crogan, N.L.; Dupler, A.E.; Short, R.; Heaton, G. Food Choice can Improve Nursing Home Resident Meal Service Satisfaction and Nutritional Status. J. Gerontol. Nurs. 2013, 39, 38–45. [Google Scholar] [CrossRef]
- Wright, O.R.L.; Connelly, L.B.; Capra, S.; Hendrikz, J. Determinants of foodservice satisfaction for patients in geriatrics/rehabilitation and residents in residential aged care. Health Expect. 2013, 16, 251–265. [Google Scholar] [CrossRef]
- Wisten, A.; Messner, T. Fruit and fibre (Pajala porridge) in the prevention of constipation. Scand. J. Caring Sci. 2005, 19, 71–76. [Google Scholar] [CrossRef]
- Ghani, H.; Motowylo, B.; Olsen, M.; Hartl, R.; Naidoo, S.; Cammer, A. Fibre Content & Fibre Fortification of Menu Items Served to Sherbrooke Community Centre Residents on Texture Modified Diets. Univ. Sask. Undergrad. Res. J. 2020, 6. [Google Scholar] [CrossRef]
- Correia, C.; Lopez, K.J.; Wroblewski, K.E.; Huisingh-Scheetz, M.; Kern, D.W.; Chen, R.C.; Schumm, L.P.; Dale, W.; McClintock, M.K.; Pinto, J.M. Global Sensory Impairment among Older Adults in the United States. J. Am. Geriatr. Soc. 2016, 64, 306–313. [Google Scholar] [CrossRef]
- Schiffman, S.S.; Graham, B.G. Taste and smell perception affect appetite and immunity in the elderly. Eur. J. Clin. Nutr. 2000, 54 (Suppl. 3), S54–S63. [Google Scholar] [CrossRef]
- Aguilera, J.M.; Park, D.J. Texture-modified foods for the elderly: Status, technology and opportunities. Trends Food Sci. Technol. 2016, 57, 156–164. [Google Scholar] [CrossRef]
- Kennewell, S.; Kokkinakos, M. Thick, cheap and easy: Fortifying texture-modified meals with infant cereal. Nutr. Diet. 2007, 64, 112–115. [Google Scholar] [CrossRef]
- Divert, C.; Laghmaoui, R.; Crema, C.; Issanchou, S.; Van Wymelbeke, V.; Sulmont-Rossé, C. Improving meal context in nursing homes. Impact of four strategies on food intake and meal pleasure. Appetite 2015, 84, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Harnett, T.; Jönson, H. Shaping nursing home mealtimes. Ageing Soc. 2017, 37, 823–844. [Google Scholar] [CrossRef]
- Cheung, G.; Pizzola, L.; Keller, H. Dietary, Food Service, and Mealtime Interventions to Promote Food Intake in Acute Care Adult Patients. J. Nutr. Gerontol. Geriatr. 2013, 32, 175–212. [Google Scholar] [CrossRef] [PubMed]
- Sossen, L.; Bonham, M.; Porter, J. Does a High-Energy High-Protein Diet Reduce Unintentional Weight Loss in Residential Aged Care Residents? J. Nutr. Gerontol. Geriatr. 2020, 39, 56–68. [Google Scholar] [CrossRef] [PubMed]
- Drewnowski, A.; Shultz, J.M. Impact of aging on eating behaviors, food choices, nutrition, and health status. J. Nutr. Health Aging 2001, 5, 75–79. [Google Scholar]
- Taylor, K.A.; Barr, S.I. Provision of small, frequent meals does not improve energy intake of elderly residents with dysphagia who live in an extended-care facility. J. Am. Diet. Assoc. 2006, 106, 1115–1118. [Google Scholar] [CrossRef]
- Logemann, J.A. Factors affecting ability to resume oral nutrition in the oropharyngeal dysphagic individual. Dysphagia 1990, 4, 202–208. [Google Scholar] [CrossRef]
- Vucea, V.; Keller, H.H.; Morrison, J.M.; Duncan, A.M.; Duizer, L.M.; Lengyel, C.O.; Slaughter, S.E. Intake and Factors Associated with Consumption of Pureed Food in Long Term Care: An Analysis of Making the Most of Mealtimes (M3) Project. J. Nutr. Gerontol. Geriatr. 2018, 37, 59–81. [Google Scholar] [CrossRef]
- Wright, L.; Cotter, D.; Hickson, M. The effectiveness of targeted feeding assistance to improve the nutritional intake of elderly dysphagic patients in hospital. J. Hum. Nutr. Diet. 2008, 21, 555–562. [Google Scholar] [CrossRef]
- Perry, L.; Hamilton, S.; Williams, J.; Jones, S. Nursing Interventions for Improving Nutritional Status and Outcomes of Stroke Patients: Descriptive Reviews of Processes and Outcomes. Worldviews Evid.-Based Nurs. 2013, 10, 17–40. [Google Scholar] [CrossRef]
- Namasivayam-MacDonald, A.M.; Steele, C.M.; Carrier, N.; Lengyel, C. The Relationship between Texture-Modified Diets, Mealtime Duration, and Dysphagia Risk in Long-Term Care. Can. J. Diet. Pract. Res. 2019, 80, 122–126. [Google Scholar] [CrossRef]
- Garcia, J.M.; Chambers, E.; Russell, E.G.; Katt, A. Modifying food textures: Practices and beliefs of staff involved in nutrition care. Am. J. Speech-Lang. Pathol. 2018, 27, 1458–1473. [Google Scholar] [CrossRef]
- Cichero, J.A.Y.; Lam, P.; Steele, C.M.; Hanson, B.; Chen, J.; Dantas, R.O.; Duivestein, J.; Kayashita, J.; Lecko, C.; Murray, J.; et al. Development of International Terminology and Definitions for Texture-Modified Foods and Thickened Fluids Used in Dysphagia Management: The IDDSI Framework. Dysphagia 2017, 32, 293–314. [Google Scholar] [CrossRef]
- Hartwell, H.J.; Edwards, J.S.A.; Beavis, J. Plate versus bulk trolley food service in a hospital: Comparison of patients’ satisfaction. Nutrition 2007, 23, 211–218. [Google Scholar] [CrossRef][Green Version]
- Abbott, R.A.; Whear, R.; Thompson-Coon, J.; Ukoumunne, O.C.; Rogers, M.; Bethel, A.; Hemsley, A.; Stein, K. Effectiveness of mealtime interventions on nutritional outcomes for the elderly living in residential care: A systematic review and meta-analysis. Ageing Res. Rev. 2013, 12, 967–981. [Google Scholar] [CrossRef]
- Rothenberg, E.; Wendin, K. Texture Modification of Food for Elderly People; Elsevier Ltd.: Amsterdam, The Netherlands, 2015; Volume 2, ISBN 9781782423522. [Google Scholar]
- West, G.E.; Ouellet, D.; Ouellette, S. Resident and staff ratings of foodservices in long-term care implications for autonomy and quality of life. J. Appl. Gerontol. 2003, 22, 57–75. [Google Scholar] [CrossRef]
- Barnes, S.; Wasielewska, A.; Raiswell, C.; Drummond, B. Exploring the mealtime experience in residential care settings for older people: An observational study. Health Soc. Care Community 2013, 21, 442–450. [Google Scholar] [CrossRef]
| Outcomes (Number of Objectives Measured in Each Category) * | Facility 1 % (n) | Facility 2 % (n) | Facility 3 % (n) | Facility 4 % (n) | Facility 5 % (n) |
|---|---|---|---|---|---|
| Overall food quantity and nutrition adequacy (26) | 74 (19) | 74 (19) | 74 (19) | 74 (19) | 74 (19) |
| Nutrition quality (12) | 92 (11) ** | 92 (11) | 92 (11) | 92 (11) | 92 (11) |
| Meat/Alternatives (3) | 100 (3) | 100 (3) | 100 (3) | 100 (3) | 100 (3) |
| Dairy (1) | 100 (1) | 100 (1) | 100 (1) | 100 (1) | 100 (1) |
| Carbohydrates (1) | 0 (1) | 0 (1) | 0 (1) | 0 (1) | 0 (1) |
| Fibre (1) | 0 (1) | 0 (1) | 0 (1) | 0 (1) | 0 (1) |
| Fruit/vegetables (3) | 67 (2) | 67 (2) | 67 (2) | 67 (2) | 67 (2) |
| Snacks (1) | 100 (1) | 100 (1) | 100 (1) | 100 (1) | 100 (1) |
| Fluids (2) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| TMD menu quality (2) | 50 (1) | 50 (1) | 50 (1) | 50 (1) | 50 (1) |
| Overall foodservice and kitchen-related standards (51) | 86 (44) | 86 (44) | 88 (45) | 80 (41) | 88 (45) |
| Dining environment (11) | 73 (8) | 73 (8) | 82 (9) | 73 (8) | 82 (9) |
| Actioning of policies and procedures (3) | 100 (3) | 100 (3) | 100 (3) | 100 (3) | 100 (3) |
| Foodservice practices (8) | 88 (7) | 88 (7) | 88 (7) | 75 (6) | 88 (7) |
| Meal quality (2) | 100 (2) | 100 (2) | 100 (2) | 100 (2) | 100 (2) |
| Hydration (2) | 100 (2) | 100 (2) | 100 (2) | 100 (2) | 100 (2) |
| Menu (6) | 83 (5) | 83 (5) | 83 (5) | 83 (5) | 83 (5) |
| Oral nutritional supplements (4) | 100 (4) | 100 (4) | 100 (4) | 75 (3) | 100 (4) |
| Portion size (5) | 80 (4) | 80 (4) | 80 (4) | 80 (4) | 80 (4) |
| TMD compliance to IDDSI (10) | 90 (9) | 90 (9) | 90 (9) | 80 (8) | 90 (9) |
| Overall clinic-related standards (16) | 81 (13) | 81 (13) | 81 (13) | 81 (13) | 81 (13) |
| Clinical practices (10) | 90 (9) | 90 (9) | 90 (9) | 90 (9) | 90 (9) |
| IDDSI practice (4) | 50 (2) | 50 (2) | 50 (2) | 50 (2) | 50 (2) |
| Training (2) | 100 (2) | 100 (2) | 100 (2) | 100 (2) | 100 (2) |
| Total compliance (93) | 82 (76) | 82 (76) | 83 (77) | 78 (73) | 83 (77) |
| Subsections * | Non-Compliant Objectives | Frequency (n/5) ** |
|---|---|---|
| Food quantity and nutrition adequacy | 1. Menu did not specify all IDDSI textures for meals and snacks | 5 |
| 2. Menu did not specify all food textures for each meal and snack (e.g., bread is not suitable for TMDs) | 5 | |
| 3. Inadequate provision of high-fibre whole-grain foods throughout the day | 5 | |
| 4. Inadequate high-fibre food offered at every meal and snack | 5 | |
| 5. Inadequate fresh fruit was offered daily | 5 | |
| 6. Fluid varieties were not specified on the menu | 5 | |
| 7. Fluid provision times were not specified | 5 | |
| Foodservice and kitchen-related standards | 1. No second helping was offered to residents who finished their meals | 5 |
| 2. Jelly was not served with high-protein/milk-based accompaniments | 5 | |
| 3. Food wastage was not monitored systematically | 5 | |
| 4. Inadequate portions of fruits were served over the day | 5 | |
| 5. Texture-modified meals were stirred together during feeding | 5 | |
| 6. TMD menus were not displayed in the dining room | 4 | |
| 7. Desserts were given before the main meal was finished | 3 | |
| 8. When residents were sleeping/sleepy during mealtime, the risk of malnutrition was not addressed to the nursing team | 1 | |
| 9. Food fortification strategies were not in place | 1 | |
| 10. Foodservice did not have high-protein, high-energy drinks available in addition to oral nutritional supplements | 1 | |
| 11. Level 4 and level 5 TMDs were not fortified | 1 | |
| Clinic-related standards | 1. Nutrition support was not always initiated for at-risk residents (e.g., wound and pressure injuries, bowel issues, respiratory disease, frequent UTIs, etc.) | 5 |
| 2. Not all healthcare assistants were able to demonstrate fluid tests for each level of fluid thickness | 5 | |
| 3. Daily fluid monitoring form was not in place for residents on thickened fluids | 5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, X.; Yousif, L.; Miles, A.; Braakhuis, A. Exploring Meal Provision and Mealtime Challenges for Aged Care Residents Consuming Texture-Modified Diets: A Mixed Methods Study. Geriatrics 2022, 7, 67. https://doi.org/10.3390/geriatrics7030067
Wu X, Yousif L, Miles A, Braakhuis A. Exploring Meal Provision and Mealtime Challenges for Aged Care Residents Consuming Texture-Modified Diets: A Mixed Methods Study. Geriatrics. 2022; 7(3):67. https://doi.org/10.3390/geriatrics7030067
Chicago/Turabian StyleWu, Xiaojing, Lina Yousif, Anna Miles, and Andrea Braakhuis. 2022. "Exploring Meal Provision and Mealtime Challenges for Aged Care Residents Consuming Texture-Modified Diets: A Mixed Methods Study" Geriatrics 7, no. 3: 67. https://doi.org/10.3390/geriatrics7030067
APA StyleWu, X., Yousif, L., Miles, A., & Braakhuis, A. (2022). Exploring Meal Provision and Mealtime Challenges for Aged Care Residents Consuming Texture-Modified Diets: A Mixed Methods Study. Geriatrics, 7(3), 67. https://doi.org/10.3390/geriatrics7030067






