Abstract
Background: Dementia care programs have become more common due to a growing number of persons living with dementia and lack of substantial benefit from pharmacologic therapies. Cultural and language differences may present barriers to access and efficacy of these programs. In this article, we aimed to systematically review the current literature regarding outcomes of dementia care programs that included multicultural and non-English speaking populations. Methods: A systematic review was conducted using four scientific search engines. All studies included in the review are English language, randomized control trials evaluating various care coordination models. The initial search strategy focusing on studies specifically targeting multicultural and non-English speaking populations resulted in too few articles. We expanded our search to articles that included these populations although these populations may not have been the focus of the study. Results: Seven articles met inclusion criteria for final review. Measured outcomes included emergency room use, hospitalizations, provider visits, quality of life indicators, depression scores, and caregiver burden. Conclusions: Dementia care programs demonstrate significant ability to provide support and improve outcomes for those living with dementia and their caregivers. There is limited research in this field and thus opportunity for further study in underserved and safety net populations including more high-quality randomized controlled trials with larger sample sizes.
1. Introduction
According to the World Alzheimer Report, it is estimated that by 2030 the global number of persons living with dementia will be 74.7 million and increase to 131.5 million by 2050 [1]. Those living with dementia may suffer devastating outcomes including inappropriate and potentially harmful medication use, frequent hospitalizations, and aggressive end-of-life care inconsistent with their goals of care [2,3,4,5,6]. Dementia has become a public health issue that affects not only those with dementia but also those who love and care for them. Caregivers experience high levels of stress and burden, which can negatively impact their physical and emotional health [4,5,7,8].
Navigating the healthcare system for persons with dementia is a challenge and usually falls on the caregiver. To mitigate these challenges, dementia care programs and dementia care-coordinators are increasingly used to address the interdisciplinary needs of those with dementia and their caregivers [6,9]. Studies show that caregivers who can access support and resources experience benefits, including improved understanding of dementia, care plans, and reduced caregiver depression, fatigue, and feelings of isolation [8,10,11]. Whereas using dementia medications has not led to substantial improvements in clinical meaningful outcomes, dementia care programs have shown benefit [12]. However, the structure, components, and efficacy of these programs vary. Furthermore, barriers to access to these programs exist, including language, culture, and geographic disparities [6,7,8]. To better understand the components and the effectiveness of these types of programs, we conducted a systematic review and evaluation of the current published literature pertaining to dementia care programs that included multicultural and multilingual populations and their outcomes.
2. Methods
2.1. Data Sources
A systematic review was conducted to investigate outcomes of dementia support programs for persons with dementia and their caregivers. While our initial search was for studies that targeted multicultural or non-English speaking populations, there were no articles that specifically met this criterion. Therefore, we changed our search to articles that included multicultural and non-English speaking populations. Literature search was conducted using PubMed, MEDLINE, CINAHL, and PsycInfo. Key terms included dementia and care coordinator. For PubMed, the “similar articles” feature was used to expand the search. Searches were then limited to peer reviewed journal articles, which were written in English and published after 2005.
2.2. Inclusion and Exclusion Criteria
Articles were included if the article was a randomized control trial and investigated an intervention that targeted support for persons with dementia and/or their caregivers. The trial also had to include multicultural or multilingual populations. Observational studies, reviews, editorials, commentaries, and case studies were excluded. Articles published outside the United States were included.
2.3. Study Selection
The primary author reviewed the titles and abstracts of all retrieved articles to assess for relevance prior to reviewing the article in full. Articles were included for full review if it was unclear from their title or abstract if a specific intervention was used in an interventional design. During full review, articles were eliminated if they investigated the same dementia support program. Only the article that scored the highest quality based on the Modified Downs and Black checklist was included. A total of seven articles were included in the final review (Figure 1). Due to the wide range of interventions and outcomes examined it was unfeasible to pool results for a quantitative meta-analysis.
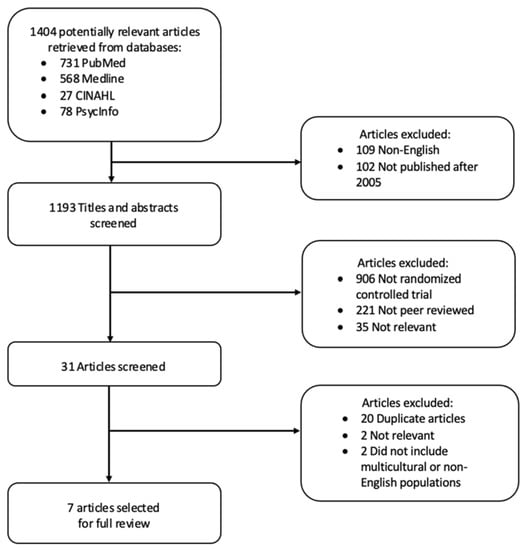
Figure 1.
Results of research strategy.
2.4. Data Abstraction
Data abstraction was performed on seven articles by the primary author and included: population, clinical setting, sample size, intervention and comparison group, measured outcome, and major findings (Table 1). The number of multicultural or non-English speaking populations included in the study was also noted.

Table 1.
Characteristics of included studies.
2.5. Quality Appraisal
The seven studies included in this review were systematically appraised using the modified Downs and Black checklist. This tool may be used to evaluate both randomized and non-randomized control trials by scoring quality of reporting, external validity, bias, confounding variables, and power, although this review article only includes randomized controlled trials [13]. The maximum score for this checklist is 28. Modified Downs and Black score ranges mirrored those reported in previous studies: ≥20 very good; 15–19 good; 11–14 fair; ≤10 poor [14].
3. Results
3.1. Article Selection
Utilizing the search strategy described above, a total of 1404 articles were initially identified. Articles were excluded if they were published prior to 2005 or not written in English. After applying these filters, 1193 articles remained. After removing articles that were not peer reviewed and not randomized controlled trials, 67 articles remained. The titles and abstracts of these 67 articles were screened and 31 articles were retained for full screening. After removing duplicates and reviewing the articles for relevance and inclusion of multicultural or non-English speaking populations, seven articles remained for full review.
3.2. Type of Studies
3.2.1. Study Design
The final review included studies that were published between 2006 and 2019. Study durations ranged from one month [8] to two years [6]. Although all studies were randomized, one study did not provide details surrounding randomization [8], one study was randomized at the level of the provider [15], another study was randomized at the level of the study site [16], while all other studies were randomized at the level of the participant [6,17,18,19]. While most studies were conducted in the US, two were conducted outside of the US including Australia [17] and Mexico [8].
3.2.2. Setting
All interventions occurred at the person’s home except for in the study conducted by Callahan et al., which included a mixture of home-based support and office visits. Support interventions included care coordination, needs assessments, linkage to resources, providing education, emotional support, or a combination of these. Additionally, these interventions were provided in varied ways including use of a culturally sensitive educational website [8], use of a therapist or certified interventionalist to teach problem solving techniques [19], or more commonly, use of a care manager to provide care coordination with needs assessments, screenings, education, and linkage to resources [6,15,16,17,18].
3.2.3. Study Population
Multicultural or multilingual participants were included in all studies. Two of the seven studies specifically targeted multicultural populations. These two studies evaluated different forms of technology to support persons with dementia. In the Czaja et al. study which evaluated a videophone technology, 50% of their study population identified as Hispanic/Latino with the other half of their population identifying as African Americans. The second study, Pagan Ortiz et al., evaluated a web-based platform in a Hispanic population. Callahan et al. had almost 50% of their study population identifying as Black/African American although multicultural populations were not specifically targeted in this study. Possin et al. included some multicultural groups, but their numbers tended to be small with only 4% identifying as African American, 10% Hispanic/Latino, and 10% Cantonese in their investigation of a phone-based support program.
Five studies reported non-English speaking dyad members. 86% of the Xiao et al. dyad population (language not specified), 7.5% in Possin et al. (2% Cantonese, 5.5% Spanish), and 100% of Pagan-Ortiz et al. (Spanish). Czaja et al. included non-English speaking populations but did not report the number of individuals who spoke Spanish.
3.2.4. Outcomes
Study outcomes fell into two groups: health care utilization or clinical outcomes. Health care utilization was evaluated in four studies, specifically emergency room use, hospitalizations, or provider visits [6,15,16,18]. Clinical outcomes, including quality of life indicators, depression scores, and caregiver burden scores, were evaluated in five studies [6,8,15,17,19].
4. Identification of Key Themes
4.1. Care Team Members
Three of the five studies used a care manager to provide care coordination used licensed clinical persons in the role of the care manager, such as social workers, registered nurses, and nurse practitioners. Only two studies used nonclinical persons as the care manager. In one study, the nonclinical person was supported by an interdisciplinary clinical team consisting of an RN and geriatric psychiatrist [18]. In the other, Possin et al. utilized an unlicensed care team manager who was provided with 40 h of training and had access to higher level clinical providers (e.g., RNs, pharmacists, social workers) if needed. While care coordination had mixed results with improvements in health care utilization, care coordination demonstrated positive clinical outcomes regardless of whether the care coordinator was a licensed clinical person.
4.2. Health Care Utilization
Five studies investigated care recipient’s health care utilization, which included number of ED visits, utilization of acute care, inpatient, outpatient, and home-and community-based services. Bass et al. found a significant decrease in both ED visits and hospitalizations in the intervention groups while Possin et al. showed a significant decrease in ED visits, but not hospitalizations. Amjad et al. showed no significant difference between number of inpatient or outpatient services. Callahan et al. did not show improvements in nursing home placement.
4.3. Clinical Outcomes
Studies evaluating clinical outcomes showed consistently positive results. Two studies resulted in less caregiver depression after participation in a dementia care program [6,8]. Three studies also found a reduction in caregiver burden [6,8,19]. Callahan et al. showed significant improvement in behavioral neuropsychiatric inventory (NPI) scores and caregiver stress and Xiao et al. reported improved quality of life measures. Of note, Czaja et al. found that almost three times as many participants in the intervention group reported significant improvements in positive aspects of caregiving after participating in an at-home, technology-based education platform for dementia care. These studies varied in their intervention from face-to-face visits [17] to virtual methods, including telephone-based [6,17], video-based [19], and web-based [6,8] visits.
4.4. Type of Educational Materials
All studies involved providing caregivers with education on how best to care for their family or loved one living with dementia. However, the type of education differed. Possin et al. educated caregivers about dementia [6] whereas four studies focused on strategies for managing challenging behaviors exhibited by persons with dementia [15,17,18,19]. Pagan-Ortiz et al. provided both types of education.
4.5. Multicultural or Non-English Speaking Participants
Although all studies included populations known to have barriers in accessing care including racial minorities or non-English speaking participants, only two studies investigated outcomes specific to these populations [8,19].
4.6. Quality of Studies
The Black and Downs scores of the seven studies included in this review ranged from 10 to 23 with a median score of 19. Based on this method of appraisal four studies received a “very good” quality rating [6,15,17,18], two studies were “good” [16,19], none were “fair”, and one study was “poor” [8].
5. Discussion
With the increasing population of older adults living in the U.S and corresponding rise in numbers of adults living with dementia, there has been a growing interest in and need for care interventions for persons with dementia (PWD) and their caregivers. Collaborative care models and multicomponent interventions have been shown to improve caregiver burden and depression, PWD quality of life, and decreases in resource utilization, such as ED visits, hospitalizations, and nursing home placement. Currently there is little information to determine whether these interventions are equally effective for multicultural populations and rural communities/communities with low resources. This review originally intended to review the efficacy of these interventions in multicultural or non-English speaking populations. However, this strategy was too limiting, and we expanded this review to evaluate studies that included these populations.
This systematic review highlights the value of dementia care programs in a variety of domains ranging from psychosocial and quality of life measures of persons with dementia and caregivers alike [6,8,17,19] to health care utilization [6,16]. A limitation identified in this review is that although most studies included for review are randomized controlled trials, not all studies were randomized at the level of the participant.
It is well established that caring for persons with dementia results in physical and psychological strain on caregivers. Challenges include helping with activities of daily living, managing psychological and behavioral symptoms of those with dementia, and perceived changes in relationship between caregivers and the person with dementia [9,10,17]. As the disease severity progresses over time, caregivers require ongoing assistance to help address challenges regarding education, daily care practices, other care services, as well as their own emotional and psychological well-being [8,11,17]. These needs may be addressed by dementia care programs.
In addition to the stressors of caring for a loved one with dementia, underrepresented multicultural populations and non-English speaking caregivers face added barriers to care. Communication barriers have been identified as a barrier to non-English speaking caregivers and families from seeking supportive services [14]. Furthermore, many resources for caregivers are designed to target the predominant culture and those who speak English [17]. Mixed race populations are understudied in trials regarding dementia care programs [15,20]. In conducting this review, it was apparent that there is limited research targeting underserved and safety net populations in this area. Although a number of studies mentioned minority populations, only two specifically targeted minority populations [8,19], further highlighting the need for more research in this area.
In the two studies that included these populations, Pagan-Ortiz et al. utilized a website to provide culturally sensitive dementia education and support for Hispanic families, and Ceja et al. used certified interventionalists to teach problem solving strategies to Hispanic and African American caregivers. The Pagan-Ortiz et al. study showed no statistically significant outcomes in self-mastery, social support, caregiver burden, or depression. Of note, study participants in Pagan-Ortiz et al. were mostly located in Mexico or Puerto Rico. Only five participants were recruited in Massachusetts. Hispanic populations in the United States face different barriers to care than in Mexico or Puerto Rico where Hispanic culture is predominant. Of the interventions listed in Table 1, use of a culturally sensitive website is the least intensive and requires more initiative on the part of the caregiver to engage with the program. Ceja et al. showed decrease caregiver burden and increased appreciation for the positive aspects of caregiving and satisfaction with social support. This more intensive intervention showed positive outcomes in underrepresented populations. This is the only article we found that showed positive outcomes specific to multicultural populations. This highlights a need for further randomized trials in populations that face barriers to accessing care in the U.S. The other studies that included multicultural or non-English speaking populations did not report outcomes specific to these specialized populations as the sample size for these populations was not large enough.
Another study, carried out by Chodosh et al., was not included as it was not a randomized control trial, but offered support for low-income Hispanic and Black communities in Los Angeles that partnered with the Alzheimer’s Association and conducted either in person or phone visits for care coordination. This study showed improved caregiver burden and problem behaviors [21], which is promising, but again highlights the need for further randomized controlled trials of dementia support programs in these populations.
Despite the lack of diversity in the trials presented here, several dementia care programs, whether through face-to-face clinical coordinators or by virtual means, have shown substantial benefit in quality of life measures. In one study conducted by Callahan et al., participants received 1 year of care management by an interdisciplinary team led by an advanced nurse practitioner integrated within the primary care setting. This study demonstrated that a comprehensive care approach resulted in clinically significant improvements in behavioral and psychological symptoms of dementia and reduction in caregiver stress. Ensuring that caregivers are properly supported has demonstrated positive outcomes for both persons with dementia and their caregivers [6].
Care coordinators may also assist in the fragmentation of medical care, provide resources, and potentially reduce healthcare costs [18]. In general, those living with dementia have higher rates of ED visits and hospitalizations, which may yield undesired consequences, including delirium, falls, medical complications, functional decline, and nursing home placement [16,22,23,24,25,26,27,28]. In a study by Bass et al., a program called Partners in Dementia, which was a collaboration between Veterans Affairs medical centers and the Alzheimer’s Association created to address the needs of persons with dementia and their caregivers, showed a reduction in hospital admissions and ED visits with corresponding healthcare costs [6,16].
As the number of individuals with dementia increases and caregivers are recognized as a precious resource, using all available tools to assist caregivers may mitigate the challenges they face [29,30]. Technology allows for the opportunity to provide tailored support and evidence-based interventions to caregivers [29,31]. Online communities are a feasible way for geographically dispersed groups to meet online for education, support, and social connection [8]. Possin et al. created a telephone based collaborative dementia care program called Ecosystem to provide education, support and care coordination to caregivers and persons with dementia. This study found that dementia care management delivered over the telephone and internet may reduce growing societal and economic burdens of dementia. In a study by Xiao et al., coaching and support provided to caregivers over the phone improved caregivers’ sense of competence in managing dementia and their mental well-being. Additionally, programs that utilize technology allow for the opportunity to reach individuals in rural areas that may otherwise not have the opportunity to participate in a dementia care program [29]. Technology is more easily accessible for persons with dementia and caregivers who otherwise would be unable to access these resources due to barriers in transportation and proximity to physical resources.
6. Conclusions
In summary, dementia care programs provide significant benefit to those living with dementia and their caregivers. Dementia care programs, whether through face-to-face coordination or virtual means, show significant promise in providing improvements in access to resources and quality of life measures for persons with dementia and caregivers alike. Furthermore, virtual based programs may be particularly helpful in underserved or safety net populations as this may improve access to dementia care programs. As research in this field is limited, more high quality studies using larger sample sizes are needed. Additionally, there is a particular need for further research in the development and efficacy of dementia care programs in multicultural and multilingual populations.
Author Contributions
Conceptualization, A.D., M.H. and K.T.W.; methodology, A.D. and M.H.; software, A.D.; validation, A.D. and M.H.; formal analysis, A.D.; data curation, A.D.; writing—original draft preparation, A.D.; writing—review and editing, A.T.W., K.T.W. and M.H.; visualization, A.D. and A.T.W.; supervision, M.H. All authors have read and agreed to the published version of the manuscript.
Funding
NIH/NCATS Grant #UL1TR001881.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Prince, M.J.; Wimo, A.; Guerchet, M.M.; Ali, G.C.; Wu, Y.T.; Prina, M. The Global Impact of Dementia: An Analysis of Prevalence, Incidence, Cost and Trends; Alzheimer’s Disease International: London, UK, 2015; p. 1. [Google Scholar]
- Hunt, L.J.; Coombs, L.A.; Stephens, C.E. Emergency Department Use by Community-Dwelling Individuals with Dementia in the United States: An Integrative Review. J. Gerontol. Nurs. 2018, 44, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Zhu, C.W.; Cosentino, S.; Ornstein, K.; Gu, Y.; Andrews, H.; Stern, Y. Use and Cost of Hospitalization in Dementia: Longitudinal Results from a Community-Based Study: Use and Cost of Hospitalization in Dementia. Int. J. Geriatr. Psychiatry 2015, 30, 833–841. [Google Scholar] [CrossRef] [PubMed]
- Etters, L.; Goodall, D.; Harrison, B.E. Caregiver Burden among Dementia Patient Caregivers: A Review of the Literature. J. Am. Acad. Nurse Pract. 2008, 20, 423–428. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, R.; Regan, C.; Katona, C.; Livingston, G. Anxiety and Depression in Family Caregivers of People with Alzheimer Disease: The LASER-AD Study. Am. J. Geriatr. Psychiatry 2005, 13, 795–801. [Google Scholar] [CrossRef]
- Possin, K.L.; Merrilees, J.J.; Dulaney, S.; Bonasera, S.J.; Chiong, W.; Lee, K.; Hooper, S.M.; Allen, I.E.; Braley, T.; Bernstein, A.; et al. Effect of Collaborative Dementia Care via Telephone and Internet on Quality of Life, Caregiver Well-Being, and Health Care Use: The Care Ecosystem Randomized Clinical Trial. JAMA Intern. Med. 2019, 179, 1658. [Google Scholar] [CrossRef]
- Papastavrou, E.; Kalokerinou, A.; Papacostas, S.S.; Tsangari, H.; Sourtzi, P. Caring for a Relative with Dementia: Family Caregiver Burden. J. Adv. Nurs. 2007, 58, 446–457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pagán-Ortiz, M.E.; Cortés, D.E.; Rudloff, N.; Weitzman, P.; Levkoff, S. Use of an Online Community to Provide Support to Caregivers of People With Dementia. J. Gerontol. Soc. Work 2014, 57, 694–709. [Google Scholar] [CrossRef] [Green Version]
- Callahan, C.M. Alzheimer’s Disease: Individuals, Dyads, Communities, and Costs. J. Am. Geriatr. Soc. 2017, 65, 892–895. [Google Scholar] [CrossRef]
- Biegel, D.E.; Sales, E.; Schulz, R. Family Caregiving in Chronic Illness: Alzheimer’s Disease, Cancer, Heart Disease, Mental Illness, and Stroke; Sage Publications: Newbury Park, CA, USA, 1991. [Google Scholar]
- Llanque, S.M.; Enriquez, M. Interventions for Hispanic Caregivers of Patients with Dementia: A Review of the Literature. Am. J. Alzheimers Dis. Dement. 2012, 27, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Buckley, J.S.; Salpeter, S.R. A Risk-Benefit Assessment of Dementia Medications: Systematic Review of the Evidence. Drugs Aging 2015, 32, 453–467. [Google Scholar] [CrossRef]
- Downs, S.H.; Black, N. The Feasibility of Creating a Checklist for the Assessment of the Methodological Quality Both of Randomised and Non-Randomised Studies of Health Care Interventions. J. Epidemiol. Community Health 1998, 52, 377–384. [Google Scholar] [CrossRef] [Green Version]
- Silva, M.D.; Genoff, M.; Zaballa, A.; Jewell, S.; Stabler, S.; Gany, F.M.; Diamond, L.C. Interpreting at the End of Life: A Systematic Review of the Impact of Interpreters on the Delivery of Palliative Care Services to Cancer Patients with Limited English Proficiency. J. Pain Symptom Manag. 2016, 51, 569–580. [Google Scholar] [CrossRef] [Green Version]
- Callahan, C.M.; Boustani, M.A.; Unverzagt, F.W.; Austrom, M.G.; Damush, T.M.; Perkins, A.J.; Fultz, B.A.; Hui, S.L.; Counsell, S.R.; Hendrie, H.C. Effectiveness of Collaborative Care for Older Adults with Alzheimer Disease in Primary Care: A Randomized Controlled Trial. JAMA 2006, 295, 2148. [Google Scholar] [CrossRef] [PubMed]
- Bass, D.M.; Judge, K.S.; Maslow, K.; Wilson, N.L.; Morgan, R.O.; McCarthy, C.A.; Looman, W.J.; Snow, A.L.; Kunik, M.E. Impact of the Care Coordination Program “Partners in Dementia Care” on Veterans’ Hospital Admissions and Emergency Department Visits. Alzheimers Dement. Transl. Res. Clin. Interv. 2015, 1, 13–22. [Google Scholar] [CrossRef] [Green Version]
- Xiao, L.D.; De Bellis, A.; Kyriazopoulos, H.; Draper, B.; Ullah, S. The Effect of a Personalized Dementia Care Intervention for Caregivers From Australian Minority Groups. Am. J. Alzheimers Dis. Dement. 2016, 31, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Amjad, H.; Wong, S.K.; Roth, D.L.; Huang, J.; Willink, A.; Black, B.S.; Johnston, D.; Rabins, P.V.; Gitlin, L.N.; Lyketsos, C.G.; et al. Health Services Utilization in Older Adults with Dementia Receiving Care Coordination: The MIND at Home Trial. Health Serv. Res. 2018, 53, 556–579. [Google Scholar] [CrossRef]
- Czaja, S.J.; Loewenstein, D.; Schulz, R.; Nair, S.N.; Perdomo, D. A Videophone Psychosocial Intervention for Dementia Caregivers. Am. J. Geriatr. Psychiatry 2013, 21, 1071–1081. [Google Scholar] [CrossRef] [PubMed]
- Sink, K.M.; Holden, K.F.; Yaffe, K. Pharmacological Treatment of Neuropsychiatric Symptoms of Dementia: A Review of the Evidence. JAMA 2005, 293, 596. [Google Scholar] [CrossRef]
- Chodosh, J.; Colaiaco, B.A.; Connor, K.I.; Cope, D.W.; Liu, H.; Ganz, D.A.; Richman, M.J.; Cherry, D.L.; Blank, J.M.; Carbone, R.d.P.; et al. Dementia Care Management in an Underserved Community: The Comparative Effectiveness of Two Different Approaches. J. Aging Health 2015, 27, 864–893. [Google Scholar] [CrossRef] [PubMed]
- Bynum, J.P.W.; Rabins, P.V.; Weller, W.; Niefeld, M.; Anderson, G.F.; Wu, A.W. The Relationship Between a Dementia Diagnosis, Chronic Illness, Medicare Expenditures, and Hospital Use. J. Am. Geriatr. Soc. 2004, 52, 187–194. [Google Scholar] [CrossRef]
- Krishnan, L.L.; Petersen, N.J.; Snow, A.L.; Cully, J.A.; Schulz, P.E.; Graham, D.P.; Morgan, R.O.; Braun, U.; Moffett, M.L.; Yu, H.-J.; et al. Prevalence of Dementia among Veterans Affairs Medical Care System Users. Dement. Geriatr. Cogn. Disord. 2005, 20, 245–253. [Google Scholar] [CrossRef]
- Maslow, K.; Mezey, M. Recognition of Dementia in Hospitalized Older Adults. AJN Am. J. Nurs. 2008, 108, 40–49. [Google Scholar] [CrossRef] [PubMed]
- Clevenger, C.K.; Chu, T.A.; Yang, Z.; Hepburn, K.W. Clinical Care of Persons with Dementia in the Emergency Department: A Review of the Literature and Agenda for Research. J. Am. Geriatr. Soc. 2012, 60, 1742–1748. [Google Scholar] [CrossRef] [PubMed]
- Kuo, S.; Rhodes, R.L.; Mitchell, S.L.; Mor, V.; Teno, J.M. Natural History of Feeding-Tube Use in Nursing Home Residents with Advanced Dementia. J. Am. Med. Dir. Assoc. 2009, 10, 264–270. [Google Scholar] [CrossRef] [Green Version]
- Sands, L.P.; Yaffe, K.; Covinsky, K.; Chren, M.-M.; Counsell, S.; Palmer, R.; Fortinsky, R.; Landefeld, C.S. Cognitive Screening Predicts Magnitude of Functional Recovery From Admission to 3 Months After Discharge in Hospitalized Elders. J. Gerontol. A Biol. Sci. Med. Sci. 2003, 58, M37–M45. [Google Scholar] [CrossRef] [Green Version]
- Bejjani, C.; Rumph, G.; Kunik, M. Addressing Psychiatric Problems of Dementia in the Emergency Room. Internet J. Emerg. Med. 2017, 7, 1–2. [Google Scholar]
- Williams, K.N.; Perkhounkova, Y.; Shaw, C.A.; Hein, M.; Vidoni, E.D.; Coleman, C.K. Supporting Family Caregivers with Technology for Dementia Home Care: A Randomized Controlled Trial. Innov. Aging 2019, 3, igz037. [Google Scholar] [CrossRef] [Green Version]
- Talley, R.C.; Crews, J.E. Framing the Public Health of Caregiving. Am. J. Public Health 2007, 97, 224–228. [Google Scholar] [CrossRef]
- Hopwood, J.; Walker, N.; McDonagh, L.; Rait, G.; Walters, K.; Iliffe, S.; Ross, J.; Davies, N. Internet-Based Interventions Aimed at Supporting Family Caregivers of People With Dementia: Systematic Review. J. Med. Internet Res. 2018, 20, e216. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).