Hospitalization for Oral Health-Related Conditions of the Australian Ageing Population: Two Decades of Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics
2.2. Population Data
2.3. Hospitalisation Data
2.4. Data Analysis
2.5. Basic Model
3. Results
3.1. Descriptive Analysis
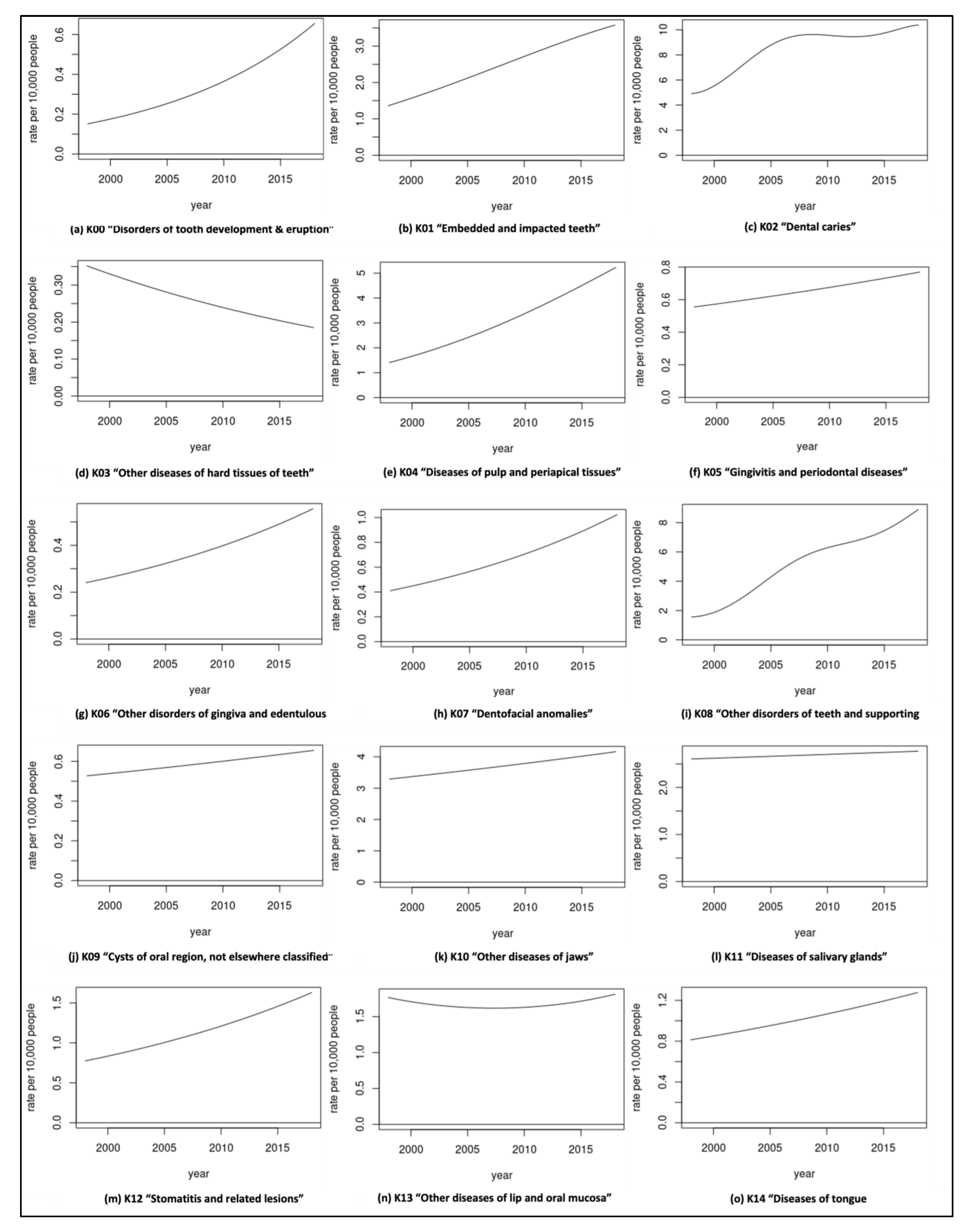
3.2. Separation Rate
3.3. Predicted Rate Increase
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Longevity Economics. Geron.org. 2018. Available online: https://www.geron.org/images/gsa/documents/gsa-longevity-economics-2018.pdf (accessed on 18 November 2021).
- Lawler, K. Aging in Place: Coordinating Housing and Health Care Provision for America’s Growing Elderly Population. Joint Center for Housing Studies of Harvard University Neighborhood Reinvestment Corporation. 2001. Available online: https://www.jchs.harvard.edu/sites/default/files/media/imp/lawler_w01-13.pdf (accessed on 6 June 2019).
- World Report on Ageing and Health. 2015. World Health Organization. Available online: https://apps.who.int/iris/bitstream/handle/10665/186463/9789240694811_eng.pdf (accessed on 8 October 2019).
- Calabrese, J.M.; Rawal, K. Demographics and Oral Health Care Utilization for Older Adults. Dent. Clin. N. Am. 2021, 65, 241–255. [Google Scholar] [CrossRef]
- Allen, F. Pragmatic care for an aging compromised dentition. Aust. Dent. J. 2019, 64, S63–S70. [Google Scholar] [CrossRef]
- Thompson, L.A.; Chen, H. Physiology of Aging of Older Adults: Systemic and Oral Health Considerations-2021 Update. Dent. Clin. N. Am. 2021, 65 (Suppl. 1), 275–284. [Google Scholar] [CrossRef]
- Thomson, W.M. Dental caries experience in older people over time: What can the large cohort studies tell us? Brit. Dent. J. 2004, 196, 89–92. [Google Scholar] [CrossRef]
- Griffin, S.O.; Griffin, P.M.; Swann, J.L.; Zlobin, N. Estimating Rates of New Root Caries in Older Adults. J. Dent. Res. 2004, 83, 634–638. [Google Scholar] [CrossRef]
- Broadbent, J.M.; Thomson, W.M.; Poulton, R. Trajectory Patterns of Dental Caries Experience in the Permanent Dentition to the Fourth Decade of Life. J. Dent. Res. 2008, 87, 69–72. [Google Scholar] [CrossRef] [PubMed]
- Karlamangla, A.; Tinetti, M.; Guralnik, J.; Studenski, S.; Wetle, T.; Reuben, D. Comorbidity in older adults: Nosology of impair-ment, diseases, and conditions. J. Gerontol. A Biol. Sci. Med. Sci. 2007, 62, 296–300. [Google Scholar] [CrossRef]
- Persson, G.R. Periodontal complications with age. Periodontol. 2000 2018, 78, 185–194. [Google Scholar] [CrossRef] [PubMed]
- Soto, A.P.; Meyer, S.L. Oral Implications of Polypharmacy in Older Adults. Dent. Clin. N. Am. 2021, 65, 323–343. [Google Scholar] [CrossRef] [PubMed]
- Kamil, W.; Kruger, E.; Tennant, M. Utilisation of Dental Services of Older People in Australia: An Economic Explanatory Model Based on Cost and Geographic Location. Geriatrics 2021, 6, 102. [Google Scholar] [CrossRef]
- Ettinger, R.L. The development of geriatric dental education programs in Canada: An update. J. Can. Dent. Assoc. 2010, 76, a1. [Google Scholar]
- Rosano, A.; Loha, C.A.; Falvo, R.; Van der Zee, J.; Ricciardi, W.; Guasticchi, G.; De Belvis, A.G. The relationship between avoidable hospitalization and accessibility to primary care: A systematic review. Eur. J. Public Health 2013, 23, 356–360. [Google Scholar] [CrossRef] [PubMed]
- Whyman, R.A.; Mahoney, E.K.; Morrison, D.; Stanley, J. Potentially preventable admissions to New Zealand public hospitals for dental care: A 20-year review. Community Dent. Oral. Epidemiol. 2014, 42, 234–244. [Google Scholar] [CrossRef] [PubMed]
- Acharya, A.; Khan, S.; Hoang, H.; Bettiol, S.; Goldberg, L.; Crocombe, L. Dental conditions associated with preventable hospital admissions in Australia: A systematic literature review. BMC Health Serv. Res. 2018, 18, 921. [Google Scholar] [CrossRef] [PubMed]
- Kruger, E.; Tennant, M. Potentially preventable hospital separations related to oral health: A 10-year analysis. Aust. Dent. J. 2015, 60, 205–211. [Google Scholar] [CrossRef]
- Crocombe, L.A.; Allen, P.; Bettiol, S.; Khan, S.; Godwin, D.; Barnett, T.; Goldberg, L.R. Geographical variation in preventable hospital ad-missions for dental conditions: An Australia-wide analysis. Aust. J. Rural. Health 2019, 27, 520–526. [Google Scholar] [CrossRef]
- Kruger, E.; Tennant, M. Hospital admissions of older people for oral health-related conditions: Implications for the future. Gerodontology 2016, 33, 490–498. [Google Scholar] [CrossRef]
- Thygesen, L.C.; Ersbøll, A.K. When the entire population is the sample: Strengths and limitations in register-based epidemiology. Eur. J. Epidemiol. 2014, 29, 551–558. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare Hospitals. Principal Diagnosis Data Cubes. Available online: https://www.aihw.gov.au/reports/hospitals/principal-diagnosis-data-cubes/contents/data-cubes (accessed on 25 February 2021).
- Australian Institute of Health and Welfare. Dental & Oral Health. Oral Health and Dental Care in Australia. Hospitalisations. Available online: https://www.aihw.gov.au/reports/dental-oral-health/oral-health-and-dental-care-in-australia/contents/hospitalisations (accessed on 15 November 2021).
- Independent Hospital Pricing Authority. Classification of Diseases and Interventions. Available online: https://www.ihpa.gov.au/what-we-do/classification-of-diseases-and-interventions (accessed on 15 November 2021).
- Thomson, W.M. Epidemiology of oral health conditions in older people. Gerodontology 2014, 31 (Suppl. 1), 9–16. [Google Scholar] [CrossRef]
- Do, L.G.; Luzzi, L. Oral health status 38. In ARCPOH. Australia’s Oral Health; National Study of Adult Oral Health 2017–2018; The University of Adelaide: Adelaide, Australia, 2019. [Google Scholar]
- Australian Institute of Health and Welfare. Older Australia at a Glance. Cat. No. AGE 87. Canberra: AIHW. Viewed 26 May 2021. 2018. Available online: https://www.aihw.gov.au/reports/older-people/older-australia-at-a-glance/contents/summary (accessed on 26 May 2021).
- Slack-Smith, L.M.; Hearn, L.; Wilson, D.F.; Wright, F. Geriatric dentistry, teaching and future directions. Aust. Dent. J. 2015, 60 (Suppl. 1), 125–130. [Google Scholar] [CrossRef]
- Tennant, M.; Namjoshi, D.; Silva, D.; Codde, J. Oral health and hospitalization in Western Australian children. Aust. Dent. J. 2000, 45, 204–207. [Google Scholar] [CrossRef] [PubMed]
- Kruger, E.; Dyson, K.; Tennant, M. Hospitalization of Western Australian children for oral health related conditions: A 5–8 year follow-up. Aust. Dent. J. 2006, 51, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.; Kruger, E.; Tennant, M. A four-year retrospective study of adult hospitalization for oral diseases in Western Australia. Aust. Dent. J. 2006, 51, 312–317. [Google Scholar] [CrossRef]
- Alsharif, A.T.; Kruger, E.; Tennant, M. Dental hospitalization trends in Western Australian children under the age of 15 years: A decade of population-based study. Int. J. Paediatr. Dent. 2015, 25, 35–42. [Google Scholar] [CrossRef]
- Oluwagbemigun, K.; Dietrich, T.; Pischon, N.; Bergmann, M.; Boeing, H. Association between Number of Teeth and Chronic Systemic Diseases: A Cohort Study Followed for 13 Years. PLoS ONE 2015, 10, e0123879. [Google Scholar] [CrossRef] [PubMed]
- Kovačić, I.; Zlatarić, D.K.; Čelebić, A. Residual ridge atrophy in complete denture wearers and relationship with densitometric values of a cervical spine: A hierarchical regression analysis. Gerodontology 2012, 29, e935–e947. [Google Scholar] [CrossRef]
- Chalmers, J.M. Geriatric oral health issues in Australia. Int. Dent. J. 2001, 51 (Suppl. 3), 188–199. [Google Scholar] [CrossRef]
- Johnstone, M.; Parashos, P. Endodontics and the ageing patient. Aust. Dent. J. 2015, 60 (Suppl. 1), 20–27. [Google Scholar] [CrossRef]
- Brennan, D.S.; Spencer, A.J. Diagnostic and preventive service trends in private general practice: 1983–1984 to 1998–1999. Aust. Dent. J. 2003, 48, 43–49. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ghezzi, E.M.; Niessen, L.C.; Jones, J.A. Innovations in Geriatric Oral Health Care. Dent. Clin. N. Am. 2021, 65, 393–407. [Google Scholar] [CrossRef]
- Akinbami, B.O.; Akadiri, O.; Gbujie, D.C. Spread of odontogenic infections in Port Harcourt, Nigeria. J. Oral. Maxillofac. Surg. 2010, 68, 2472–2477. [Google Scholar] [CrossRef]
- Jevon, P.; Abdelrahman, A.; Pigadas, N. Management of odontogenic infections and sepsis: An update. Br Dent. J. 2020, 229, 363–370. [Google Scholar] [CrossRef]
- George, R.P.; Kruger, E.; Tennant, M. The geographic and socioeconomic distribution of in-hospital treatment of impacted teeth in Western Australia: A 6-year retrospective analysis. Oral. Health Prev. Dent. 2011, 9, 131–136. [Google Scholar] [PubMed]
- Trybek, G.; Chruściel-Nogalska, M.; Machnio, M.; Smektała, T.; Malinowski, J.; Tutak, M.; Sporniak-Tutak, K. Surgical extraction of impacted teeth in elderly patients. A retrospective analysis of perioperative complications—The experience of a single institution. Gerodontology 2016, 33, 410–415. [Google Scholar] [CrossRef] [PubMed]
- Thomson, W.M.; Ma, S. An ageing population poses dental challenges. Singap. Dent. J. 2014, 35, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Kamil, W.; Kruger, E.; McGeachie, J.; Jean, G.; Tennant, M. Distribution of Australian dental practices in relation to the ageing population. Gerodontology 2021, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Australian Institute of Health and Welfare. AIHW Media Releases. Hospital Activity Low during Early Months of COVID-19 Pandemic. 2021. Available online: https://www.aihw.gov.au/news-media/media-releases/2021-1/june/hospital-activity-low-during-early-months-of-covid (accessed on 11 November 2021).



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kamil, W.; Kruger, E.; Turlach, B.; Tennant, M. Hospitalization for Oral Health-Related Conditions of the Australian Ageing Population: Two Decades of Analysis. Geriatrics 2022, 7, 2. https://doi.org/10.3390/geriatrics7010002
Kamil W, Kruger E, Turlach B, Tennant M. Hospitalization for Oral Health-Related Conditions of the Australian Ageing Population: Two Decades of Analysis. Geriatrics. 2022; 7(1):2. https://doi.org/10.3390/geriatrics7010002
Chicago/Turabian StyleKamil, Wisam, Estie Kruger, Berwin Turlach, and Marc Tennant. 2022. "Hospitalization for Oral Health-Related Conditions of the Australian Ageing Population: Two Decades of Analysis" Geriatrics 7, no. 1: 2. https://doi.org/10.3390/geriatrics7010002
APA StyleKamil, W., Kruger, E., Turlach, B., & Tennant, M. (2022). Hospitalization for Oral Health-Related Conditions of the Australian Ageing Population: Two Decades of Analysis. Geriatrics, 7(1), 2. https://doi.org/10.3390/geriatrics7010002






