Perceptions of Burden and Preparedness for Caregiving among the Family Caregivers of Hospitalised Older Adults: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Setting, and Sample
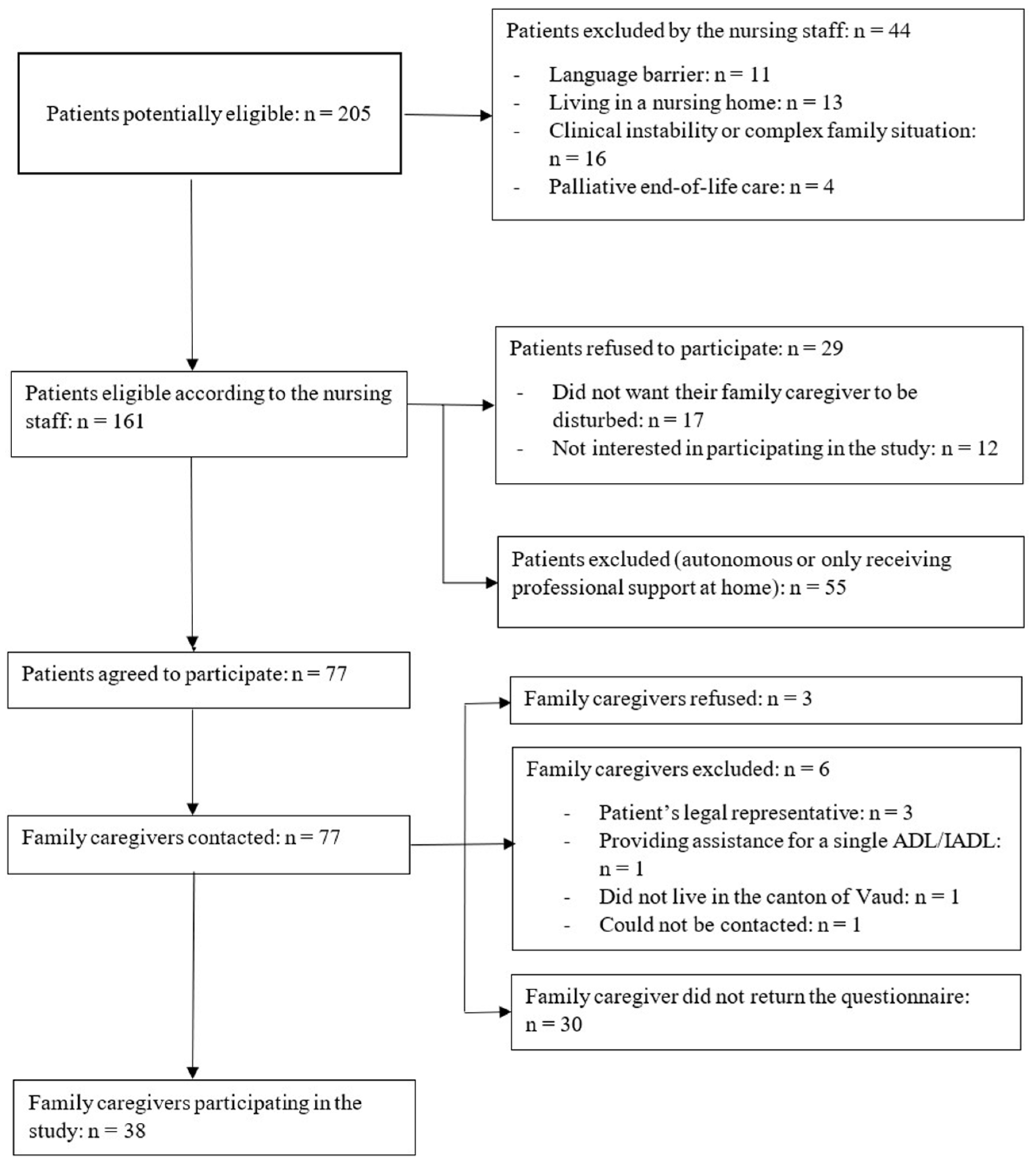
2.2. Recruitment Procedure
2.3. Measures
2.4. Statistical Analysis
3. Results
3.1. Hospitalised Older Adults’ Characteristics
3.2. Family Caregivers’ Characteristics
3.3. Family Caregivers’ Perception Levels of Preparedness for Caregiving
3.4. Associations between Preparedness for Caregiving and Older Adults’ Characteristics
3.5. Family Caregivers’ Perception of Burden
3.6. Associations between Family Caregivers’ Perceptions of Burden and the Sociodemographic and Clinical Characteristics of Their Older Adult Relatives
3.7. Associations between the Dimensions of Preparedness for Caregiving and the Dimensions of Burden
4. Discussion
4.1. Older Adults’ Sociodemographic and Clinical Characteristics
4.2. Sociodemographic Characteristics of Family Caregivers
4.3. Family Caregivers’ Perceptions of Their Level of Preparedness for Caregiving
4.4. Family Caregivers’ Perceived Levels of Burden
4.5. Associations between Preparedness for Caregiving and Perceptions of Burden
4.6. Strengths and Limitations
4.7. Recommendations for Clinical Practice, Research, and Education
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Vieillissement et Santé. Available online: http://www.who.int/mediacentre/factsheets/fs404/fr/ (accessed on 21 April 2020).
- Andreani, T.; Berrut, S.; Gazareth, P.; Hauri, D.; Kaeser, M.; Lieberherr, R.; Lindner, M.; Marquis, J.-F.; Storni, M.; Teotino, G.; et al. Statistiques de la Santé; Département fédéral de l’intérieur DFI: Neuchâtel, Switzerland, 2014.
- Silva, A.L.; Teixeira, H.J.; Teixeira, M.J.; Freitas, S. The needs of informal caregivers of elderly people living at home: An integrative review. Scand. J. Caring Sci. 2013, 27, 792–803. [Google Scholar] [CrossRef] [PubMed]
- Service des Assurances Sociales et de l’hébergement. Commission Consultative Pour le Soutien Direct des Proches Aidants Actifs à Domicile -CCSPA: Rapport D’activité 2011–2012; État de Vaud: Lausanne, Switzerland, 2011; pp. 1–26.
- World Health Organization. Supporting Informal Caregivers of People Living with Dementia; 2015. Available online: https://www.who.int/mental_health/neurology/dementia/dementia_thematicbrief_informal_care.pdf (accessed on 7 January 2022).
- Ducharme, F.; Lebel, P.; Bergman, H. Vieillissement et soins, l’urgence d’offrir des services de santé intégrés aux familles du XXIe siècle. Ruptures 2001, 8, 110–121. [Google Scholar]
- Ducharme, F. Famille et Vieillissement. Enjeux et Défis Pour Soignants Professionnels et Proches-Aidants. Perspect. Infirm. 2007, 4, 11–16. [Google Scholar]
- Criel, B.; Vanlerberghe, V.; De Koker, B.; Decraene, B.; Engels, E.; Waltens, R. Informal home care for elderly in Belgium: A study on the features and challenges of informal care at local level. Community Ment. Health J. 2014, 50, 848–853. [Google Scholar] [CrossRef] [PubMed]
- Committee on Family Caregiving for Older Adults; Board on Health Care Services; Health and Medicine Division; National Academies of Sciences, Engineering and Medicine. Families Caring for an Aging America; Schulz, R., Eden, J., Eds.; National Academies Press: Washington, DC, USA, 2016. [Google Scholar]
- Kim, E.K.; Park, H. Factors associated with Burden of Family Caregivers of Home-dwelling Elderly People with Dementia: A Systematic Review and Meta-analysis. Korean J. Adult Nurs. 2019, 31, 351–364. [Google Scholar] [CrossRef]
- Petruzzo, A.; Biagioli, V.; Durante, A.; Emberti Gialloreti, L.; D’Agostino, F.; Alvaro, R.; Vellone, E. Influence of preparedness on anxiety, depression, and quality of life in caregivers of heart failure patients: Testing a model of path analysis. Patient Educ. Couns. 2019, 102, 1021–1028. [Google Scholar] [CrossRef]
- George, L.K.; Gwyther, L.P. Caregiver well-being: A multidimensional examination of family caregivers of demented adults. Gerontologist 1986, 26, 253–259. [Google Scholar] [CrossRef]
- Thompson, E.H.; Doll, W. The Burden of Families Coping with the Mentally III: An Invisible Crisis. Fam. Relat. 1982, 31, 379–388. [Google Scholar] [CrossRef]
- Hébert, R.; Bravo, G.; Préville, M. Reliability, Validity and Reference Values of the Zarit Burden Interview for Assessing Informal Caregivers of Community-Dwelling Older Persons with Dementia. Can. J. Aging/La Rev. Can. Du Vieil. 2000, 19, 494–507. [Google Scholar] [CrossRef]
- Gibbons, C.; Creese, J.; Tran, M.; Brazil, K.; Chambers, L.; Weaver, B.; Bedard, M. The psychological and health consequences of caring for a spouse with dementia: A critical comparison of husbands and wives. J. Women Aging 2014, 26, 3–21. [Google Scholar] [CrossRef]
- Kumamoto, K.; Arai, Y. Validation of ‘personal strain’ and ‘role strain’: Subscales of the short version of the Japanese version of the Zarit Burden Interview (J-ZBI_8). Psychiatry Clin. Neurosci. 2004, 58, 606–610. [Google Scholar] [CrossRef] [PubMed]
- Whitlatch, C.J.; Zarit, S.H.; von Eye, A. Efficacy of interventions with caregivers: A reanalysis. Gerontologist 1991, 31, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Conde-Sala, J.L.; Garre-Olmo, J.; Turro-Garriga, O.; Vilalta-Franch, J.; Lopez-Pousa, S. Quality of life of patients with Alzheimer’s disease: Differential perceptions between spouse and adult child caregivers. Dement. Geriatr. Cogn. Disord. 2010, 29, 97–108. [Google Scholar] [CrossRef] [PubMed]
- Grant, M.; Sun, V.; Fujinami, R.; Sidhu, R.; Otis-Green, S.; Juarez, G.; Klein, L.; Ferrell, B. Family caregiver burden, skills preparedness, and quality of life in non-small cell lung cancer. Oncol. Nurs. Forum. 2013, 40, 337–346. [Google Scholar] [CrossRef]
- Loureiro Lde, S.; Fernandes, M.; Marques, S.; Nobrega, M.M.; Rodrigues, R.A. Burden in family caregivers of the elderly: Prevalence and association with characteristics of the elderly and the caregivers. Rev. Esc. Enferm. USP 2013, 47, 1133–1140. [Google Scholar] [CrossRef]
- Borman, P.; Gokce-Kutsal, Y.; Terzioglu, F.; Okumus, M.; Ceceli, E.; Karahan, S.; Senel, K.; Gokkaya, K.O.; Dogan, A.; Eskiyurt, N.; et al. A Multicenter Pilot Study of Burden Among Caregivers of Geriatric Rehabilitation Patients with Neuromusculoskeletal Diseases. Rehabil. Nurs. 2017, 42, 199–209. [Google Scholar] [CrossRef]
- Dauphinot, V.; Ravier, A.; Novais, T.; Delphin-Combe, F.; Mouchoux, C.; Krolak-Salmon, P. Risk Factors of Caregiver Burden Evolution, for Patients With Subjective Cognitive Decline or Neurocognitive Disorders: A Longitudinal Analysis. J. Am. Med. Dir. Assoc. 2016, 17, 1037–1043. [Google Scholar] [CrossRef]
- Girardi Paskulin, L.M.; Kottwitz Bierhals, C.C.B.; Oliveira Dos Santos, N.; Baltar Day, C.; de Oliveira Machado, D.; Pinheiro de Morais, E.; Rodrigues Goncalves, M.; Peixoto Cordova, F.; Ferreira Grillo, M.F. Depressive symptoms of the elderly people and caregiver’s burden in home care. Investig. Educ. Enferm. 2017, 35, 210–220. [Google Scholar] [CrossRef][Green Version]
- Mello, J.A.; Macq, J.; Van Durme, T.; Ces, S.; Spruytte, N.; Van Audenhove, C.; Declercq, A. The determinants of informal caregivers’ burden in the care of frail older persons: A dynamic and role-related perspective. Aging Ment. Health 2017, 21, 838–843. [Google Scholar] [CrossRef]
- Perez Marmol, J.M.; Flores Antiguedad, M.L.; Castro Sanchez, A.M.; Tapia Haro, R.M.; Garcia Rios, M.D.C.; Aguilar Ferrandiz, M.E. Inpatient dependency in activities of daily living predicts informal caregiver strain: A cross-sectional study. J. Clin. Nurs. 2018, 27, e177–e185. [Google Scholar] [CrossRef]
- Pessotti, C.F.C.; Fonseca, L.C.; Tedrus, G.; Laloni, D.T. Family caregivers of elderly with dementia Relationship between religiosity, resilience, quality of life and burden. Dement. Neuropsychol. 2018, 12, 408–414. [Google Scholar] [CrossRef] [PubMed]
- del-Pino-Casado, R.; Frias-Osuna, A.; Palomino-Moral, P.A.; Ramon Martinez-Riera, J. Gender differences regarding informal caregivers of older people. J. Nurs. Scholarsh. 2012, 44, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Chang, M.; Rose, K.; Kim, S. Predictors of caregiver burden in caregivers of individuals with dementia. J. Adv. Nurs. 2012, 68, 846–855. [Google Scholar] [CrossRef]
- Mendes, P.N.; Figueiredo, M.d.L.F.; Santos, A.M.R.d.; Fernandes, M.A.; Fonseca, R.S.B. Sobrecargas física, emocional e social dos cuidadores informais de idosos. Acta Paul. Enferm. 2019, 32, 87–94. [Google Scholar] [CrossRef]
- Reckrey, J.M.; Decherrie, L.V.; Kelley, A.S.; Ornstein, K. Health care utilization among homebound elders: Does caregiver burden play a role? J. Aging Health 2013, 25, 1036–1049. [Google Scholar] [CrossRef]
- Uei, S.L.; Sung, H.C.; Yang, M.S. Caregivers’ Self-Efficacy and Burden of Managing Behavioral Problems in Taiwanese Aged 65 and over with Dementia. Soc. Behav. Personal. 2013, 41, 1487–1496. [Google Scholar] [CrossRef]
- Friedemann, M.L.; Buckwalter, K.C. Family Caregiver Role and Burden Related to Gender and Family Relationships. J. Fam. Nurs. 2014, 20, 313–336. [Google Scholar] [CrossRef]
- Rosas-Carrasco, O.; Guerra-Silla Mde, G.; Torres-Arreola Ldel, P.; Garcia-Pena, C.; Escamilla-Jimenez, C.I.; Gonzalez-Gonzalez, C. Caregiver burden of Mexican dementia patients: The role of dysexecutive syndrome, sleep disorders, schooling and caregiver depression. Geriatr. Gerontol. Int. 2014, 14, 146–152. [Google Scholar] [CrossRef]
- Naef, R.; Hediger, H.; Imhof, L.; Mahrer-Imhof, R. Variances in family carers’ quality of life based on selected relationship and caregiving indicators: A quantitative secondary analysis. Int. J. Older People Nurs. 2017, 12, e12138. [Google Scholar] [CrossRef]
- Valente, L.E.; Truzzi, A.; Souza, W.F.; Alves, G.S.; Alves, C.E.; Sudo, F.K.; Lanna, M.E.; Moreira, D.M.; Engelhardt, E.; Laks, J. Health self-perception by dementia family caregivers: Sociodemographic and clinical factors. Arq. Neuropsiquiatr. 2011, 69, 739–744. [Google Scholar] [CrossRef]
- Wright, M.J.; Battista, M.A.; Pate, D.S.; Hierholzer, R.; Mogelof, J.; Howsepian, A.A. Domain-Specific Associations between Burden and Mood State in Dementia Caregivers. Clin. Gerontol. 2010, 33, 237–247. [Google Scholar] [CrossRef]
- Shyu, Y.I.; Yang, C.T.; Huang, C.C.; Kuo, H.C.; Chen, S.T.; Hsu, W.C. Influences of mutuality, preparedness, and balance on caregivers of patients with dementia. J. Nurs. Res. 2010, 18, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Zwicker, D. Preparedness for Caregiving Scale; Hartford Institute for Geriatric Nursing: New York, NY, USA, 2018. [Google Scholar]
- Yang, C.T.; Liu, H.Y.; Shyu, Y.I. Dyadic relational resources and role strain in family caregivers of persons living with dementia at home: A cross-sectional survey. Int. J. Nurs. Stud. 2014, 51, 593–602. [Google Scholar] [CrossRef] [PubMed]
- Ducharme, F.; Levesque, L.; Lachance, L.; Kergoat, M.J.; Coulombe, R. Challenges associated with transition to caregiver role following diagnostic disclosure of Alzheimer disease: A descriptive study. Int. J. Nurs. Stud. 2011, 48, 1109–1119. [Google Scholar] [CrossRef]
- Scherbring, M. Effect of caregiver perception of preparedness on burden in an oncology population. Oncol. Nurs. Forum. 2002, 29, E70–E76. [Google Scholar] [CrossRef]
- Wang, Y.N.; Shyu, Y.I.; Tsai, W.C.; Yang, P.S.; Yao, G. Exploring conflict between caregiving and work for caregivers of elders with dementia: A cross-sectional, correlational study. J. Adv. Nurs. 2013, 69, 1051–1062. [Google Scholar] [CrossRef] [PubMed]
- Henriksson, A.; Arestedt, K. Exploring factors and caregiver outcomes associated with feelings of preparedness for caregiving in family caregivers in palliative care: A correlational, cross-sectional study. Palliat. Med. 2013, 27, 639–646. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Bull. World Health Organ. 2007, 85, 867–872. [Google Scholar] [CrossRef]
- Wild, D.; Grove, A.; Martin, M.; Eremenco, S.; McElroy, S.; Verjee-Lorenz, A.; Erikson, P.; Translation, I.T.F.f.; Cultural, A. Principles of Good Practice for the Translation and Cultural Adaptation Process for Patient-Reported Outcomes (PRO) Measures: Report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health 2005, 8, 94–104. [Google Scholar] [CrossRef]
- Carter, J.H.; Stewart, B.J.; Archbold, P.G.; Inoue, I.; Jaglin, J.; Lannon, M.; Rost-Ruffner, E.; Tennis, M.; McDermott, M.P.; Amyot, D.; et al. Living with a person who has Parkinson’s disease: The spouse’s perspective by stage of disease. Parkinson’s Study Group. Mov. Disord. 1998, 13, 20–28. [Google Scholar] [CrossRef]
- Hudson, P.L.; Hayman-White, K. Measuring the psychosocial characteristics of family caregivers of palliative care patients: Psychometric properties of nine self-report instruments. J. Pain Symptom Manag. 2006, 31, 215–228. [Google Scholar] [CrossRef] [PubMed]
- Archbold, P.G.; Stewart, B.J.; Greenlick, M.R.; Harvath, T. Mutuality and preparedness as predictors of caregiver role strain. Res. Nurs. Health 1990, 13, 375–384. [Google Scholar] [CrossRef] [PubMed]
- Zarit, S.H.; Reever, K.E.; Bach-Peterson, J. Relatives of the impaired elderly: Correlates of feelings of burden. Gerontologist 1980, 20, 649–655. [Google Scholar] [CrossRef] [PubMed]
- Zarit, S.H. Diagnosis and management of caregiver burden in dementia. Handb. Clin. Neurol. 2008, 89, 101–106. [Google Scholar] [CrossRef] [PubMed]
- Réseau Québécois de Recherche sur le Vieillissement. Available online: http://www.rqrv.com/fr/instrument.php?i=91 (accessed on 14 April 2016).
- Katz, S.; Downs, T.D.; Cash, H.R.; Grotz, R.C. Progress in development of the index of ADL. Gerontologist 1970, 10, 20–30. [Google Scholar] [CrossRef]
- Katz, S. Assessing self-maintenance: Activities of daily living, mobility, and instrumental activities of daily living. J. Am. Geriatr. Soc. 1983, 31, 721–727. [Google Scholar] [CrossRef]
- Ludecke, D.; Mnich, E.; Kofahl, C. The impact of sociodemographic factors on the utilisation of support services for family caregivers of elderly dependents-results from the German sample of the EUROFAMCARE study. Psychosoc. Med. 2012, 9, Doc06. [Google Scholar] [CrossRef]
- Office fédéral de la statistique. Mouvement de la Population–Indicateurs-Espérance de vie; Confédération Suisse: Neuchâtel, Switzerland, 2016. [Google Scholar]
- Association Vaudoise d’Aide et de Soins à Domicile. Mission. Available online: http://www.avasad.ch/jcms/m_7010/fr/mission (accessed on 1 June 2016).
- Watson, L.C.; Lewis, C.L.; Moore, C.G.; Jeste, D.V. Perceptions of depression among dementia caregivers: Findings from the CATIE-AD trial. Int. J. Geriatr. Psychiatry 2011, 26, 397–402. [Google Scholar] [CrossRef]
- Pariel, S.; Boissieres, A.; Delamare, D.; Belmin, J. Patient education in geriatrics: Which specificities? Presse. Med. 2013, 42, 217–223. [Google Scholar] [CrossRef]
- Bureau D’information et de Communication de l’Etat de Vaud. Structures D’accompagnement Médico-Sociales: Une Nouvelle Identité pour Regrouper une Offre Croissante. 2012; Volume 1. Available online: https://www.vd.ch/themes/sante-soins-et-handicap/vivre-a-domicile/sams/ (accessed on 7 January 2022).
- Del-Pino-Casado, R.; Pastor-Bravo, M.D.; Palomino-Moral, P.A.; Frias-Osuna, A. Gender differences in primary home caregivers of older relatives in a Mediterranean environment: A cross-sectional study. Arch. Gerontol. Geriatr. 2017, 69, 128–133. [Google Scholar] [CrossRef]
- United Nations. Income Poverty in Old Age: An Emerging Development Priority; Department of Economic and Social Affairs: New York, NY, USA, 2015. [Google Scholar]
- Ennuyer, B. À quel âge est-on vieux? La catégorisation des âges: Ségrégation sociale et réification des individus. Gérontologie Et Société 2011, 34, 127–142. [Google Scholar] [CrossRef]
- WHO-World Health Organization. Ageing and health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 2 June 2021).
- Meleis, A.I. Transitions Theory: Middle-Range and Situation-Specific Theories in Nursing Research and Practice; Springer Publishing Company: New York, NY, USA, 2010; p. 664. [Google Scholar]
- Ducharme, F.; Lévesque, L.; Caron, C.D.; Hanson, E.; Magnusson, L.; Nolan, J.; Nolan, M. Validation d’un Outil Pour les Proches-Aidants. Rech. Soins. Infirm. 2009, 2, 63–73. [Google Scholar] [CrossRef]
- Akpinar, B.; Kucukguclu, O.; Yener, G. Effects of gender on burden among caregivers of Alzheimer’s patients. J. Nurs. Scholarsh. 2011, 43, 248–254. [Google Scholar] [CrossRef] [PubMed]
- Novak, M.; Guest, C. Application of a multidimensional caregiver burden inventory. Gerontologist 1989, 29, 798–803. [Google Scholar] [CrossRef]
| Age, Mean (SD) | 66.34 (16.44) |
|---|---|
| n (%) | |
| Female | 30 (79.0) |
| Nationality (n = 37) * | |
| Swiss | 28 (75.7) |
| Italian | 3 (8.1) |
| Spanish | 2 (5.4) |
| Other | 4 (10.8) |
| Marital status | |
| Married | 28 (73.7) |
| Single | 6 (15.8) |
| Other | 4 (10.5) |
| Employment status | |
| Full-time job | 7 (18.4) |
| Part-time job | 5 (13.2) |
| Retired | 23 (60.5) |
| Jobless | 3 (7.9) |
| Monthly income (CHF) (n = 35) * | |
| <2000 | 8 (22.9) |
| 2000–5000 | 12 (34.3) |
| 5001–7500 | 9 (25.7) |
| >7500 | 6 (17.2) |
| Monthly income is a source of concern (n = 37) *, n (%) | 8 (21.6) |
| Educational level | |
| Elementary school | 10 (26.3) |
| Apprenticeship or equivalent level | 13 (34.2) |
| High school | 2 (5.3) |
| University | 13 (34.2) |
| Family relationship with the older adult | |
| Spouse | 15 (39.5) |
| Child | 15 (39.5) |
| Friend | 4 (10.5) |
| Other | 4 (10.5) |
| Cohabitation with the older adult | 17 (44.7) |
| Household composition (n = 36) * | |
| One person | 4 (11.1) |
| Two persons | 27 (75.0) |
| ≥ Three persons | 5 (13.9) |
| Urban residential area | 28 (73.7) |
| Professional home care services for the family caregivers themselves (n = 37) * | |
| Yes | 4 (10.8) |
| Assistance with bathing | 1 (25.0) |
| Assistance with housekeeping | 2 (50.0) |
| Assistance with bathing and meal delivery | 1 (25.0) |
| Frequency of the assistance | |
| Once a week | 3 (75.0) |
| Three times a week | 1 (25.0) |
| No | 33 (89.2) |
| Type of Assistance | n (%) |
|---|---|
| Assistance with bathing | 13 (34.2) |
| Assistance with mobility and transfers | 15 (39.5) |
| Assistance with dressing and undressing | 11 (29.0) |
| Assistance with toileting | 5 (13.2) |
| Assistance with feeding | 16 (42.1) |
| Assistance with grocery shopping | 30 (79.0) |
| Assistance with transportation | 20 (52.6) |
| Assistance with medication | 15 (39.5) |
| Assistance with housekeeping | 17 (44.7) |
| Assistance with finances | 24 (63.2) |
| Assistance with food preparation | 25 (65.8) |
| Assistance with laundry | 23 (60.5) |
| Occasional surveillance | 18 (47.4) |
| Constant surveillance (day and night) | 6 (15.8) |
| Overall Level of Preparedness for Caregiving: Total Score (0–4) | Mean (SD) |
|---|---|
| 1.76 (0.91) | |
| n (%) | |
| 1 (2.6) |
| 16 (42.1) |
| 14 (36.8) |
| 5 (13.2) |
| 2 (5.3) |
| Dimensions | ZBI Personal Strain | ZBI Role Strain | ZBI Overall | |||
|---|---|---|---|---|---|---|
| ρ | p-Value | ρ | p-Value | ρ | p-Value | |
| PCS Physical care | −0.06 | 0.726 | −0.05 | 0.780 | −0.10 | 0.546 |
| PCS Emotional support | −0.18 | 0.289 | −0.35 * | 0.034 | −0.31 | 0.062 |
| PCS Organising in-home support services | −0.23 | 0.172 | −0.33 * | 0.047 | −0.23 | 0.164 |
| PCS Stress management | −0.18 | 0.273 | −0.23 | 0.174 | −0.19 | 0.256 |
| PCS Overall | −0.28 | 0.093 | −0.33 * | 0.041 | −0.30 | 0.067 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
da Rocha, C.G.; Perrenoud, B.; Ramelet, A.-S. Perceptions of Burden and Preparedness for Caregiving among the Family Caregivers of Hospitalised Older Adults: A Cross-Sectional Study. Geriatrics 2022, 7, 19. https://doi.org/10.3390/geriatrics7010019
da Rocha CG, Perrenoud B, Ramelet A-S. Perceptions of Burden and Preparedness for Caregiving among the Family Caregivers of Hospitalised Older Adults: A Cross-Sectional Study. Geriatrics. 2022; 7(1):19. https://doi.org/10.3390/geriatrics7010019
Chicago/Turabian Styleda Rocha, Carla Gomes, Béatrice Perrenoud, and Anne-Sylvie Ramelet. 2022. "Perceptions of Burden and Preparedness for Caregiving among the Family Caregivers of Hospitalised Older Adults: A Cross-Sectional Study" Geriatrics 7, no. 1: 19. https://doi.org/10.3390/geriatrics7010019
APA Styleda Rocha, C. G., Perrenoud, B., & Ramelet, A.-S. (2022). Perceptions of Burden and Preparedness for Caregiving among the Family Caregivers of Hospitalised Older Adults: A Cross-Sectional Study. Geriatrics, 7(1), 19. https://doi.org/10.3390/geriatrics7010019







