Lower Limb Strength Profile in Elderly with Different Pathologies: Comparisons with Healthy Subjects
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Statistical Analysis
3. Results
3.1. Sociodemographic Characteristics and Baseline Comparisons
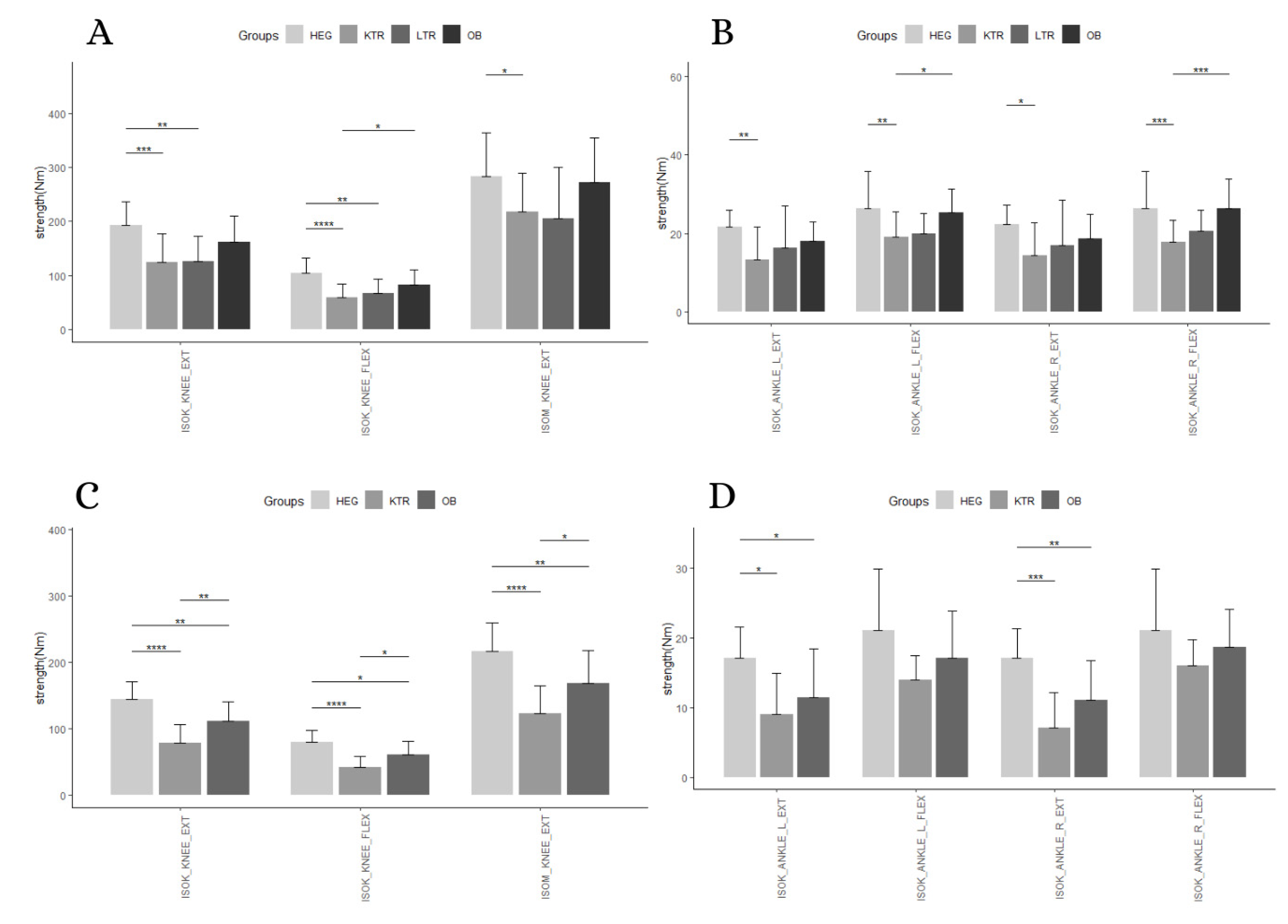
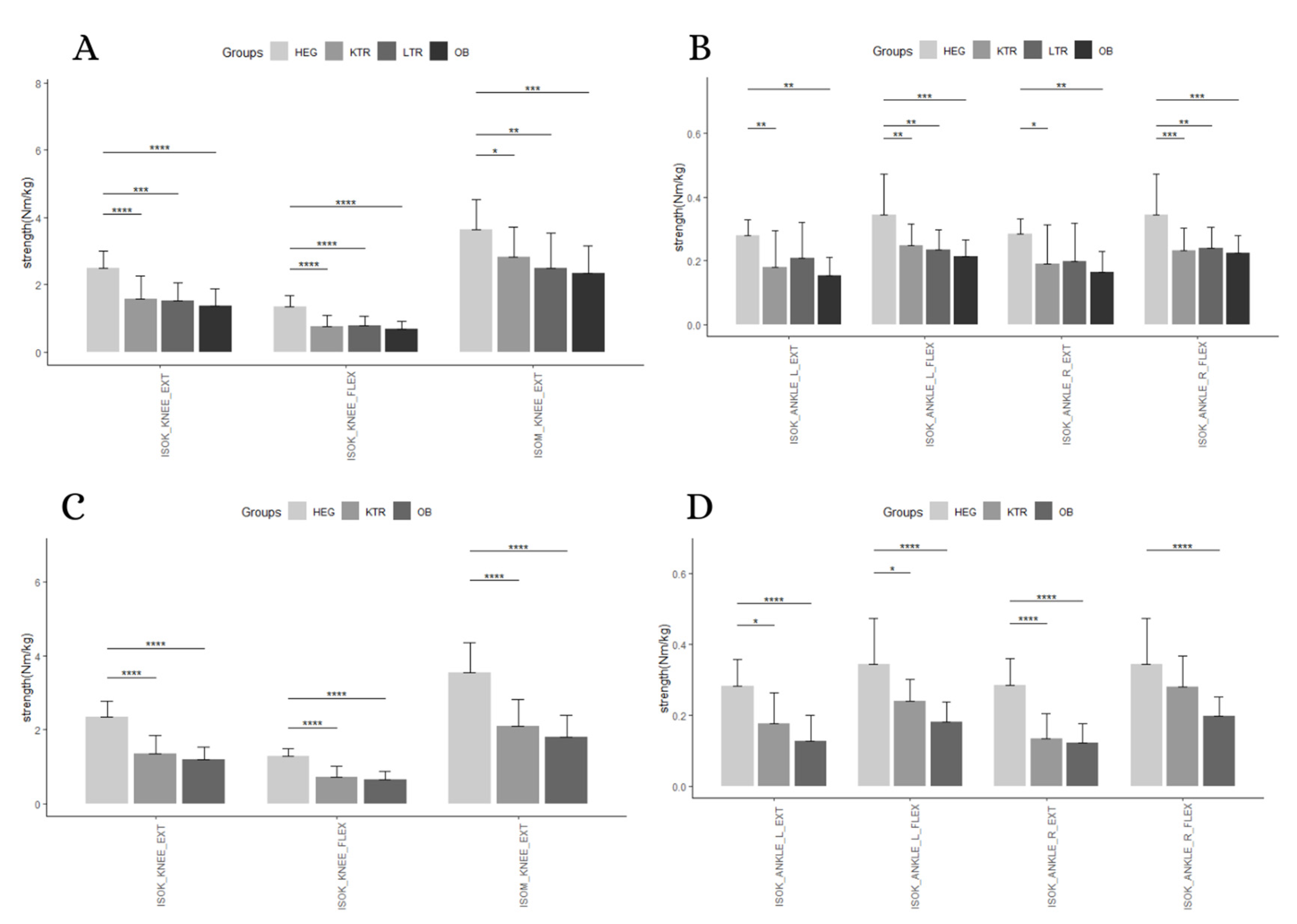
3.2. Absolute Strength
3.3. Relative Strength
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Yassierli; Nussbaum, M.A.; Iridiastadi, H.; Wojcik, L.A. The influence of age on isometric endurance and fatigue is muscle dependent: A study of shoulder abduction and torso extension. Ergonomics 2007, 50, 26–45. [Google Scholar] [CrossRef] [PubMed]
- Runge, M.; Rittweger, J.; Russo, C.R.; Schiessl, H.; Felsenberg, D. Is muscle power output a key factor in the age-related decline in physical performance? A comparison of muscle cross section, chair-rising test and jumping power. Clin. Physiol. Funct. Imaging 2004, 24, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Sapienza, C.M. Implications of expiratory muscle strength training for rehabilitation of the elderly: Tutorial. J. Rehabil. Res. Dev. 2005, 42, 211–224. [Google Scholar] [CrossRef]
- Clark, B.C.; Manini, T.M. What is dynapenia? Nutrition 2012, 28, 495–503. [Google Scholar] [CrossRef] [PubMed]
- Ryall, J.G.; Schertzer, J.D.; Lynch, G.S. Cellular and molecular mechanisms underlying age-related skeletal muscle wasting and weakness. Biogerontology 2008, 9, 213–228. [Google Scholar] [CrossRef]
- Deer, R.R.; Volpi, E. Protein intake and muscle function in older adults. Curr. Opin. Clin. Nutr. Metab. Care 2015, 18, 248–253. [Google Scholar] [CrossRef] [PubMed]
- Langhammer, B.; Bergland, A.; Rydwik, E. The Importance of Physical Activity Exercise among Older People. Biomed. Res. Int. 2018, 2018, 7856823. [Google Scholar] [CrossRef]
- Rubenstein, L.Z. Falls in older people: Epidemiology, risk factors and strategies for prevention. Age Ageing 2006, 35 (Suppl. 2), ii37–ii41. [Google Scholar] [CrossRef]
- Granacher, U.; Muehlbauer, T.; Gollhofer, A.; Kressig, R.W.; Zahner, L. An intergenerational approach in the promotion of balance and strength for fall prevention—A mini-review. Gerontology 2011, 57, 304–315. [Google Scholar] [CrossRef]
- Mitchell, W.K.; Williams, J.; Atherton, P.; Larvin, M.; Lund, J.; Narici, M. Sarcopenia, dynapenia, and the impact of advancing age on human skeletal muscle size and strength; a quantitative review. Front. Physiol. 2012, 3, 260. [Google Scholar] [CrossRef]
- Lexell, J.; Taylor, C.C.; Sjostrom, M. What is the cause of the ageing atrophy? Total number, size and proportion of different fiber types studied in whole vastus lateralis muscle from 15- to 83-year-old men. J. Neurol. Sci. 1988, 84, 275–294. [Google Scholar] [CrossRef]
- Delbono, O. Neural control of aging skeletal muscle. Aging Cell 2003, 2, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Lynch, N.A.; Metter, E.J.; Lindle, R.S.; Fozard, J.L.; Tobin, J.D.; Roy, T.A.; Fleg, J.L.; Hurley, B.F. Muscle quality. I. Age-associated differences between arm and leg muscle groups. J. Appl. Physiol. 1999, 86, 188–194. [Google Scholar] [CrossRef] [PubMed]
- Candow, D.G.; Chilibeck, P.D. Differences in size, strength, and power of upper and lower body muscle groups in young and older men. J. Gerontol. A Biol. Sci. Med. Sci. 2005, 60, 148–156. [Google Scholar] [CrossRef]
- Christensen, U.; Stovring, N.; Schultz-Larsen, K.; Schroll, M.; Avlund, K. Functional ability at age 75: Is there an impact of physical inactivity from middle age to early old age? Scand. J. Med. Sci. Sports 2006, 16, 245–251. [Google Scholar] [CrossRef]
- Saggini, R. Sarcopenia in Chronic Illness and Rehabilitative Approaches. In Frailty and Sarcopenia—Onset, Development and Clinical Challenges; Dionyssiotis, Y., Ed.; IntechOpen: Rijeka, Croatia, 2017. [Google Scholar] [CrossRef][Green Version]
- Adams, G.R.; Vaziri, N.D. Skeletal muscle dysfunction in chronic renal failure: Effects of exercise. Am. J. Physiol. Renal. Physiol. 2006, 290, F753–F761. [Google Scholar] [CrossRef]
- Jones, J.C.; Coombes, J.S.; Macdonald, G.A. Exercise capacity and muscle strength in patients with cirrhosis. Liver Transpl. 2012, 18, 146–151. [Google Scholar] [CrossRef]
- Parry, S.M.; Puthucheary, Z.A. The impact of extended bed rest on the musculoskeletal system in the critical care environment. Extrem. Physiol. Med. 2015, 4, 16. [Google Scholar] [CrossRef] [PubMed]
- Zanotto, T.; Gobbo, S.; Bullo, V.; Vendramin, B.; Duregon, F.; Cugusi, L.; Di Blasio, A.; Furian, L.; Silvestre, C.; Neunhaeuserer, D.; et al. Balance impairment in kidney transplant recipients without concurrent peripheral neuropathy. Gait Posture 2017, 55, 116–120. [Google Scholar] [CrossRef][Green Version]
- Stenholm, S.; Harris, T.B.; Rantanen, T.; Visser, M.; Kritchevsky, S.B.; Ferrucci, L. Sarcopenic obesity: Definition, cause and consequences. Curr. Opin. Clin. Nutr. Metab. Care 2008, 11, 693–700. [Google Scholar] [CrossRef]
- Stenholm, S.; Sainio, P.; Rantanen, T.; Alanen, E.; Koskinen, S. Effect of co-morbidity on the association of high body mass index with walking limitation among men and women aged 55 years and older. Aging Clin. Exp. Res. 2007, 19, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Bergamin, M.; Gobbo, S.; Bullo, V.; Vendramin, B.; Duregon, F.; Frizziero, A.; Di Blasio, A.; Cugusi, L.; Zaccaria, M.; Ermolao, A. Reliability of a device for the knee and ankle isometric and isokinetic strength testing in older adults. Muscles Ligaments Tendons J. 2017, 7, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Padulo, J.; Oliva, F.; Frizziero, A.; Maffulli, N. Muscles, Ligaments and Tendons Journal—Basic principles and recommendations in clinical and field Science Research: 2018 update. MLTJ 2018, 8, 305–307. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Tombaugh, T.N.; McIntyre, N.J. The mini-mental state examination: A comprehensive review. J. Am. Geriatr. Soc. 1992, 40, 922–935. [Google Scholar] [CrossRef]
- Tomczak, M.; Tomczak, E. The need to report effect size estimates revisited. An overview of some recommended measures of effect size. Trends Sport Sci. 2014, 1, 19–25. [Google Scholar]
- Chan, W.; Chin, S.H.; Whittaker, A.C.; Jones, D.; Kaur, O.; Bosch, J.A.; Borrows, R. The Associations of Muscle Strength, Muscle Mass, and Adiposity With Clinical Outcomes and Quality of Life in Prevalent Kidney Transplant Recipients. J. Ren. Nutr. 2019, 29, 536–547. [Google Scholar] [CrossRef]
- McAdams-DeMarco, M.A.; Ying, H.; Olorundare, I.; King, E.A.; Haugen, C.; Buta, B.; Gross, A.L.; Kalyani, R.; Desai, N.M.; Dagher, N.N.; et al. Individual Frailty Components and Mortality in Kidney Transplant Recipients. Transplantation 2017, 101, 2126–2132. [Google Scholar] [CrossRef]
- Menna Barreto, A.P.M.; Barreto Silva, M.I.; Pontes, K.; Costa, M.S.D.; Rosina, K.T.C.; Souza, E.; Bregman, R.; Klein, M. Sarcopenia and its components in adult renal transplant recipients: Prevalence and association with body adiposity. Br. J. Nutr. 2019, 122, 1386–1397. [Google Scholar] [CrossRef]
- Lai, J.C.; Segev, D.L.; McCulloch, C.E.; Covinsky, K.E.; Dodge, J.L.; Feng, S. Physical frailty after liver transplantation. Am. J. Transplant. 2018, 18, 1986–1994. [Google Scholar] [CrossRef]
- Onghena, L.; Develtere, W.; Poppe, C.; Geerts, A.; Troisi, R.; Vanlander, A.; Berrevoet, F.; Rogiers, X.; Van Vlierberghe, H.; Verhelst, X. Quality of life after liver transplantation: State of the art. World J. Hepatol. 2016, 8, 749–756. [Google Scholar] [CrossRef] [PubMed]
- A.I.S.F. Associazione Italiana per lo Studio del Fegato. Trapianto di Fegato non Urgente Dell’adulto; A.I.S.F. Associazione Italiana per lo Studio del Fegato: Roma, Italy, 2019. [Google Scholar]
- Tomlinson, D.J.; Erskine, R.M.; Morse, C.I.; Winwood, K.; Onambele-Pearson, G. The impact of obesity on skeletal muscle strength and structure through adolescence to old age. Biogerontology 2016, 17, 467–483. [Google Scholar] [CrossRef]
- Bosco, C.; Rusko, H.; Hirvonen, J. The effect of extra-load conditioning on muscle performance in athletes. Med. Sci. Sports Exerc. 1986, 18, 415–419. [Google Scholar] [CrossRef]
- Hulens, M.; Vansant, G.; Lysens, R.; Claessens, A.L.; Muls, E. Assessment of isokinetic muscle strength in women who are obese. J. Orthop. Sports Phys. Ther. 2002, 32, 347–356. [Google Scholar] [CrossRef] [PubMed]
- Maffiuletti, N.A.; Jubeau, M.; Munzinger, U.; Bizzini, M.; Agosti, F.; De Col, A.; Lafortuna, C.L.; Sartorio, A. Differences in quadriceps muscle strength and fatigue between lean and obese subjects. Eur. J. Appl. Physiol. 2007, 101, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Rolland, Y.; Lauwers-Cances, V.; Cristini, C.; Abellan van Kan, G.; Janssen, I.; Morley, J.E.; Vellas, B. Difficulties with physical function associated with obesity, sarcopenia, and sarcopenic-obesity in community-dwelling elderly women: The EPIDOS (EPIDemiologie de l’OSteoporose) Study. Am. J. Clin. Nutr. 2009, 89, 1895–1900. [Google Scholar] [CrossRef]
- Shaw, R.; Mitchell-Olds, T. Anova for Unbalanced Data: An Overview. Ecology 1993, 74, 1638–1645. [Google Scholar] [CrossRef]
- Newman, A.B.; Kupelian, V.; Visser, M.; Simonsick, E.M.; Goodpaster, B.H.; Kritchevsky, S.B.; Tylavsky, F.A.; Rubin, S.M.; Harris, T.B. Strength, but not muscle mass, is associated with mortality in the health, aging and body composition study cohort. J. Gerontol. A Biol. Sci. Med. Sci. 2006, 61, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Visser, M.; Goodpaster, B.H.; Kritchevsky, S.B.; Newman, A.B.; Nevitt, M.; Rubin, S.M.; Simonsick, E.M.; Harris, T.B. Muscle mass, muscle strength, and muscle fat infiltration as predictors of incident mobility limitations in well-functioning older persons. J. Gerontol. A Biol. Sci. Med. Sci. 2005, 60, 324–333. [Google Scholar] [CrossRef]
- Visser, M.; Newman, A.B.; Nevitt, M.C.; Kritchevsky, S.B.; Stamm, E.B.; Goodpaster, B.H.; Harris, T.B. Reexamining the sarcopenia hypothesis. Muscle mass versus muscle strength. Health, Aging, and Body Composition Study Research Group. Ann. N. Y. Acad. Sci. 2000, 904, 456–461. [Google Scholar] [CrossRef]
| Measures | Sex | KTR (46) | LTR (15) | OB (50) | HEG (30) |
|---|---|---|---|---|---|
| Number | M | 36 | 14 | 18 | 16 |
| F | 10 | 1 | 32 | 14 | |
| Age (y) | M | 66.64 ± 4.92 | 66 ± 4.39 | 65.28 ± 3.49 | 64.31 ± 4.13 |
| F | 65.9 ± 3.87 | 63.41 ± 4.22 | 63.79 ± 5.47 | ||
| Height (m) | M | 1.74 ± 0.06 | 1.7 ± 0.08 | 1.72 ± 0.05 | 1.77 ± 0.04 |
| F | 1.6 ± 0.06 | 1.57 ± 0.06 | 1.63 ± 0.06 | ||
| Weight (kg) | M | 77.44 ± 11.99 | 82.26 ± 14.91 | 120.19 ± 18.53 | 78.25 ± 13.49 |
| F | 60.09 ± 10.93 | 96.05 ± 14.8 | 62.14 ± 12.88 | ||
| BMI (kg/m2) | M | 25.63 ± 3.12 | 28.32 ± 4.07 | 40.41 ± 5.52 | 24.97 ± 4.01 |
| F | 23.44 ± 3.54 | 39.55 ± 5.27 | 23.31 ± 3.98 | ||
| MMSE | M | 28.42 ± 1.58 | 29 ± 1.41 | 29.6 ± 0.74 | 29.69 ± 0.48 |
| F | 28.41 ± 1.87 | 29.38 ± 0.74 | 29.5 ± 0.52 | ||
| Time transplant (months) | M | 34.7 ± 63.61 | 28.43 ± 43.5 | ||
| F | 5.75 ± 7.09 | ||||
| Hypertension | M | 24 | 2 | 10 | 2 |
| F | 5 | 17 | 1 | ||
| DMT2 | M | 8 | 5 | 7 | 1 |
| F | 0 | 10 | 0 | ||
| Dyslipidemia | M | 8 | 1 | 4 | 0 |
| F | 3 | 10 | 1 |
| Effect | Variables | dof, dofE | F | p | Partial η2 (90%CI) |
|---|---|---|---|---|---|
| Measure x Group | Absolute Strength | 4.47, 105.88 | 3.61 | 0.006 | 0.13 (0.02–0.2) |
| Measure | 1.49, 105.88 | 563.1 | <0.0001 | 0.89 (0.85–0.91) | |
| Group | 3.00, 71.00 | 7.31 | 0.0002 | 0.24 (0.08–0.34) | |
| Post Hoc | Variables | dof, dofE | F | p | Partial η2 (90%CI) |
| For group | ISOK_ANKLE-L_EXT | 3.00, 75 | 4.66 | 0.005 | 0.16 (0.03–0.26) |
| ISOK_ANKLE-R_EXT | 3.00, 73 | 3.63 | 0.017 | 0.13 (0.01–0.23) | |
| ISOK_KNEE_EXT | 3.00, 74 | 8.25 | 0.0001 | 0.25 (0.1–0.36) | |
| ISOK_ANKLE-L_FLEX | 3.00, 75 | 5.90 | 0.001 | 0.19 (0.05–0.29) | |
| ISOK_ANKLE-R_FLEX | 3.00, 73 | 8.45 | 0.0001 | 0.26 (0.1–0.36) | |
| ISOK_KNEE_FLEX | 3.00, 74 | 10.85 | <0.0001 | 0.31 (0.15–0.41) | |
| ISOM_KNEE_EXT | 3.00, 80 | 4.38 | 0.007 | 0.14 (0.02–0.24) | |
| For measure | HEG | 6.00, 90.00 | 176.99 | <0.0001 | 0.92 (0.89–0.93) |
| KTR | 1.44, 43.09 | 210.65 | <0.0001 | 0.88 (0.81–0.91) | |
| LTR | 1.31, 14.37 | 75.9 | <0.0001 | 0.87 (0.71–0.91) | |
| OB | 1.73, 25.88 | 154.73 | <0.0001 | 0.91 (0.84–0.94) |
| Effect | Variables | dof, dofE | F | p | Partial η2 (90%CI) |
|---|---|---|---|---|---|
| Measure x Group | Absolute Strength | 3.44, 75.62 | 8.21 | <0.0001 | 0.27 (0.11–0.37) |
| Measure | 1.72, 75,62 | 489.75 | <0.0001 | 0.92 (0.89–0.93) | |
| Group | 2, 44 | 14.05 | <0.0001 | 0.40 (0.18–0.52) | |
| Post Hoc | Variables | dof, dofE | F | p | Partial η2 (90%CI) |
| For group | ISOK_ANKLE-L_EXT | 2.00, 45 | 5.41 | 0.008 | 0.19 (0.03–0.33) |
| ISOK_ANKLE-R_EXT | 2.00, 45 | 11.04 | 0.0001 | 0.33 (0.13–0.46) | |
| ISOK_KNEE_EXT | 2.00, 47 | 15.92 | <0.0001 | 0.40 (0.21–0.53) | |
| ISOK_ANKLE-L_FLEX | 2.00, 45 | 2.76 | 0.074 | 0.11 (0–0.24) | |
| ISOK_ANKLE-R_FLEX | 2.00, 45 | 1.59 | 0.215 | 0.07 (0–0.18) | |
| ISOK_KNEE_FLEX | 2.00, 47 | 11.59 | 0.0001 | 0.33 (0.14–0.46) | |
| ISOM_KNEE_EXT | 2.00, 53 | 11.75 | 0.0001 | 0.31 (0.13–0.43) | |
| For measure | HEG | 6.00, 78.00 | 270.34 | <0.0001 | 0.95 (0.93–0.96) |
| KTR | 1.53, 10.72 | 106.72 | <0.0001 | 0.94 (0.82–0.96) | |
| OB | 1.83, 43.92 | 291.38 | <0.0001 | 0.92 (0.88–0.94) |
| Outcomes | Group 1 | Group 2 | n1 | n2 | Absolute p.adj | Relative p.adj |
|---|---|---|---|---|---|---|
| ISOK_ANKLE-L_EXT | HEG | KTR | 16 | 36 | 0.0032 | 0.005 |
| HEG | LTR | 16 | 14 | 0.402 | 0.387 | |
| HEG | OB | 16 | 18 | 1 | 0.0018 | |
| LTR | KTR | 14 | 36 | 1 | 1 | |
| LTR | OB | 14 | 18 | 1 | 0.809 | |
| KTR | OB | 36 | 18 | 0.256 | 1 | |
| ISOK_ANKLE-R_EXT | HEG | KTR | 16 | 36 | 0.012 | 0.0176 |
| HEG | LTR | 16 | 14 | 0.485 | 0.157 | |
| HEG | OB | 16 | 18 | 1 | 0.0058 | |
| LTR | KTR | 14 | 36 | 1 | 1 | |
| LTR | OB | 14 | 18 | 1 | 1 | |
| KTR | OB | 36 | 18 | 0.496 | 1 | |
| ISOK_KNEE_EXT | HEG | KTR | 16 | 36 | 0.0001 | <0.0001 |
| HEG | LTR | 16 | 14 | 0.0033 | 0.0003 | |
| HEG | OB | 16 | 18 | 0.42 | <0.0001 | |
| LTR | KTR | 14 | 36 | 1 | 1 | |
| LTR | OB | 14 | 18 | 0.349 | 1 | |
| KTR | OB | 36 | 18 | 0.0778 | 1 | |
| ISOK_ANKLE-L_FLEX | HEG | KTR | 16 | 36 | 0.0049 | 0.001 |
| HEG | LTR | 16 | 14 | 0.1 | 0.0041 | |
| HEG | OB | 16 | 18 | 1 | 0.0001 | |
| LTR | KTR | 14 | 36 | 1 | 1 | |
| LTR | OB | 14 | 18 | 0.238 | 1 | |
| KTR | OB | 36 | 18 | 0.0177 | 1 | |
| ISOK_ANKLE-R_FLEX | HEG | KTR | 16 | 36 | 0.0008 | 0.0002 |
| HEG | LTR | 16 | 14 | 0.176 | 0.009 | |
| HEG | OB | 16 | 18 | 1 | 0.0005 | |
| LTR | KTR | 14 | 36 | 1 | 1 | |
| LTR | OB | 14 | 18 | 0.166 | 1 | |
| KTR | OB | 36 | 18 | 0.0007 | 1 | |
| ISOK_KNEE_FLEX | HEG | KTR | 16 | 36 | <0.0001 | <0.0001 |
| HEG | LTR | 16 | 14 | 0.0021 | <0.0001 | |
| HEG | OB | 16 | 18 | 0.146 | <0.0001 | |
| LTR | KTR | 14 | 36 | 1 | 1 | |
| LTR | OB | 14 | 18 | 0.643 | 1 | |
| KTR | OB | 36 | 18 | 0.0291 | 1 | |
| ISOM_KNEE | HEG | KTR | 16 | 36 | 0.0488 | 0.0256 |
| HEG | LTR | 16 | 14 | 0.0578 | 0.0059 | |
| HEG | OB | 16 | 18 | 1 | 0.0004 | |
| LTR | KTR | 14 | 36 | 1 | 1 | |
| LTR | OB | 14 | 18 | 0.119 | 1 | |
| KTR | OB | 36 | 18 | 0.113 | 0.356 |
| Outcomes | Group 1 | Group 2 | n1 | n2 | Absolute p.adj | Relative p.adj |
|---|---|---|---|---|---|---|
| ISOK_ANKLE-L_EXT | HEG | KTR | 14 | 10 | 0.0163 | 0.0135 |
| HEG | OB | 14 | 32 | 0.0265 | <0.0001 | |
| KTR | OB | 10 | 32 | 1 | 0.401 | |
| ISOK_ANKLE-R_EXT | HEG | KTR | 14 | 10 | 0.0002 | <0.0001 |
| HEG | OB | 14 | 32 | 0.0029 | <0.0001 | |
| KTR | OB | 10 | 32 | 0.173 | 1 | |
| ISOK_KNEE_EXT | HEG | KTR | 14 | 10 | <0.0001 | <0.0001 |
| HEG | OB | 14 | 32 | 0.003 | <0.0001 | |
| KTR | OB | 10 | 32 | 0.0096 | 0.886 | |
| ISOK_ANKLE-L_FLEX | HEG | KTR | 14 | 10 | 0.087 | 0.0257 |
| HEG | OB | 14 | 32 | 0.308 | <0.0001 | |
| KTR | OB | 10 | 32 | 0.823 | 0.262 | |
| ISOK_ANKLE-R_FLEX | HEG | KTR | 14 | 10 | 0.254 | 0.306 |
| HEG | OB | 14 | 32 | 0.835 | <0.0001 | |
| KTR | OB | 10 | 32 | 0.92 | 0.0813 | |
| ISOK_KNEE_FLEX | HEG | KTR | 14 | 10 | 0.0001 | <0.0001 |
| HEG | OB | 14 | 32 | 0.0125 | <0.0001 | |
| KTR | OB | 10 | 32 | 0.0346 | 1 | |
| ISOM_KNEE | HEG | KTR | 14 | 10 | <0.0001 | <0.0001 |
| HEG | OB | 14 | 32 | 0.0072 | <0.0001 | |
| KTR | OB | 10 | 32 | 0.0312 | 0.625 |
| Effect | Variables | dof, dofE | F | p | Partial η2 (90%CI) |
|---|---|---|---|---|---|
| Measure x Group | Absolute Strength | 4.7, 104.23 | 5.88 | 0.0001 | 0.20 (0.08–0.28) |
| Measure | 1.49, 104.23 | 540.24 | <0.0001 | 0.89 (0.85–0.91) | |
| Group | 3.00, 70.00 | 11.2 | <0.0001 | 0.32 (0.16–0.43) | |
| Post Hoc | Variables | dof, dofE | F | p | Partial η2 (90%CI) |
| For group | ISOK_ANKLE-L_EXT | 3.00, 73 | 5.65 | 0.002 | 0.19 (0.05–0.29) |
| ISOK_ANKLE-R_EXT | 3.00, 73 | 4.56 | 0.006 | 0.16 (0.030–0.25) | |
| ISOK_KNEE_EXT | 3.00, 74 | 12.01 | <0.0001 | 0.33 (0.17–0.43) | |
| ISOK_ANKLE-L_FLEX | 3.00, 75 | 8.22 | 0.0001 | 0.25 (0.097–0.35) | |
| ISOK_ANKLE-R_FLEX | 3.00, 73 | 8.02 | 0.0001 | 0.25 (0.09–0.35) | |
| ISOK_KNEE_FLEX | 3.00, 74 | 16.77 | <0.0001 | 0.41 (0.24–0.50) | |
| ISOM_KNEE_EXT | 3.00, 80 | 6.63 | 0.0005 | 0.20 (0.06–0.30) | |
| For measure | HEG | 6.00, 90.00 | 227.606 | <0.001 | 0.94 (0.91–0.95) |
| KTR | 1.45, 45.1 | 225.901 | <0.001 | 0.88 (0.64–0.82) | |
| LTR | 1.32, 13.21 | 94.443 | <0.001 | 0.90 (0.72–0.92) | |
| OB | 1.45, 24.59 | 120.18 | <0.001 | 0.87 (0.75–0.91) |
| Effect | Variables | dof, dofE | F | p | Partial η2 (90%CI) |
|---|---|---|---|---|---|
| Measure x Group | Absolute Strength | 2.92, 59.79 | 24.87 | <0.0001 | 0.55 (0.38–0.63) |
| Measure | 1.46, 59.79 | 477.82 | <0.0001 | 0.92 (0.89–0.94) | |
| Group | 2, 41 | 45.17 | <0.0001 | 0.69 (0.53–0.76) | |
| Post Hoc | Variables | dof, dofE | F | p | Partial η2 (90%CI) |
| For group | ISOK_ANKLE-L_EXT | 2.00, 43 | 18.72 | <0.0001 | 0.47 (0.26–0.58) |
| ISOK_ANKLE-R_EXT | 2.00, 43 | 30.43 | <0.0001 | 0.59 (0.4–0.68) | |
| ISOK_KNEE_EXT | 2.00, 47 | 40.92 | <0.0001 | 0.64 (0.47–0.72) | |
| ISOK_ANKLE-L_FLEX | 2.00, 45 | 16.86 | <0.0001 | 0.43 (0.23–0.55) | |
| ISOK_ANKLE-R_FLEX | 2.00, 45 | 12.98 | <0.0001 | 0.37 (0.16–0.49) | |
| ISOK_KNEE_FLEX | 2.00, 47 | 33.67 | <0.0001 | 0.59 (0.41–0.68) | |
| ISOM_KNEE_EXT | 2.00, 52 | 33.48 | <0.0001 | 0.56 (0.39–0.65) | |
| For measure | HEG | 6.00, 78.00 | 238.24 | <0.0001 | 0.95 (0.93–0.96) |
| KTR | 1.56, 9.36 | 83.36 | <0.0001 | 0.94 (0.79–0.95) | |
| OB | 1.58, 34.83 | 237.78 | <0.0001 | 0.92 (0.86–0.94) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bullo, V.; Roma, E.; Gobbo, S.; Duregon, F.; Bergamo, M.; Bianchini, G.; Doria, E.; Cugusi, L.; di Blasio, A.; Bocalini, D.S.; et al. Lower Limb Strength Profile in Elderly with Different Pathologies: Comparisons with Healthy Subjects. Geriatrics 2020, 5, 83. https://doi.org/10.3390/geriatrics5040083
Bullo V, Roma E, Gobbo S, Duregon F, Bergamo M, Bianchini G, Doria E, Cugusi L, di Blasio A, Bocalini DS, et al. Lower Limb Strength Profile in Elderly with Different Pathologies: Comparisons with Healthy Subjects. Geriatrics. 2020; 5(4):83. https://doi.org/10.3390/geriatrics5040083
Chicago/Turabian StyleBullo, Valentina, Enrico Roma, Stefano Gobbo, Federica Duregon, Manuele Bergamo, Gioia Bianchini, Eleonora Doria, Lucia Cugusi, Andrea di Blasio, Danilo Sales Bocalini, and et al. 2020. "Lower Limb Strength Profile in Elderly with Different Pathologies: Comparisons with Healthy Subjects" Geriatrics 5, no. 4: 83. https://doi.org/10.3390/geriatrics5040083
APA StyleBullo, V., Roma, E., Gobbo, S., Duregon, F., Bergamo, M., Bianchini, G., Doria, E., Cugusi, L., di Blasio, A., Bocalini, D. S., Ermolao, A., & Bergamin, M. (2020). Lower Limb Strength Profile in Elderly with Different Pathologies: Comparisons with Healthy Subjects. Geriatrics, 5(4), 83. https://doi.org/10.3390/geriatrics5040083





