Allostatic Load, Social Participation, and Healthy Ageing: Longitudinal Evidence on the Impact of Chronic Stress
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
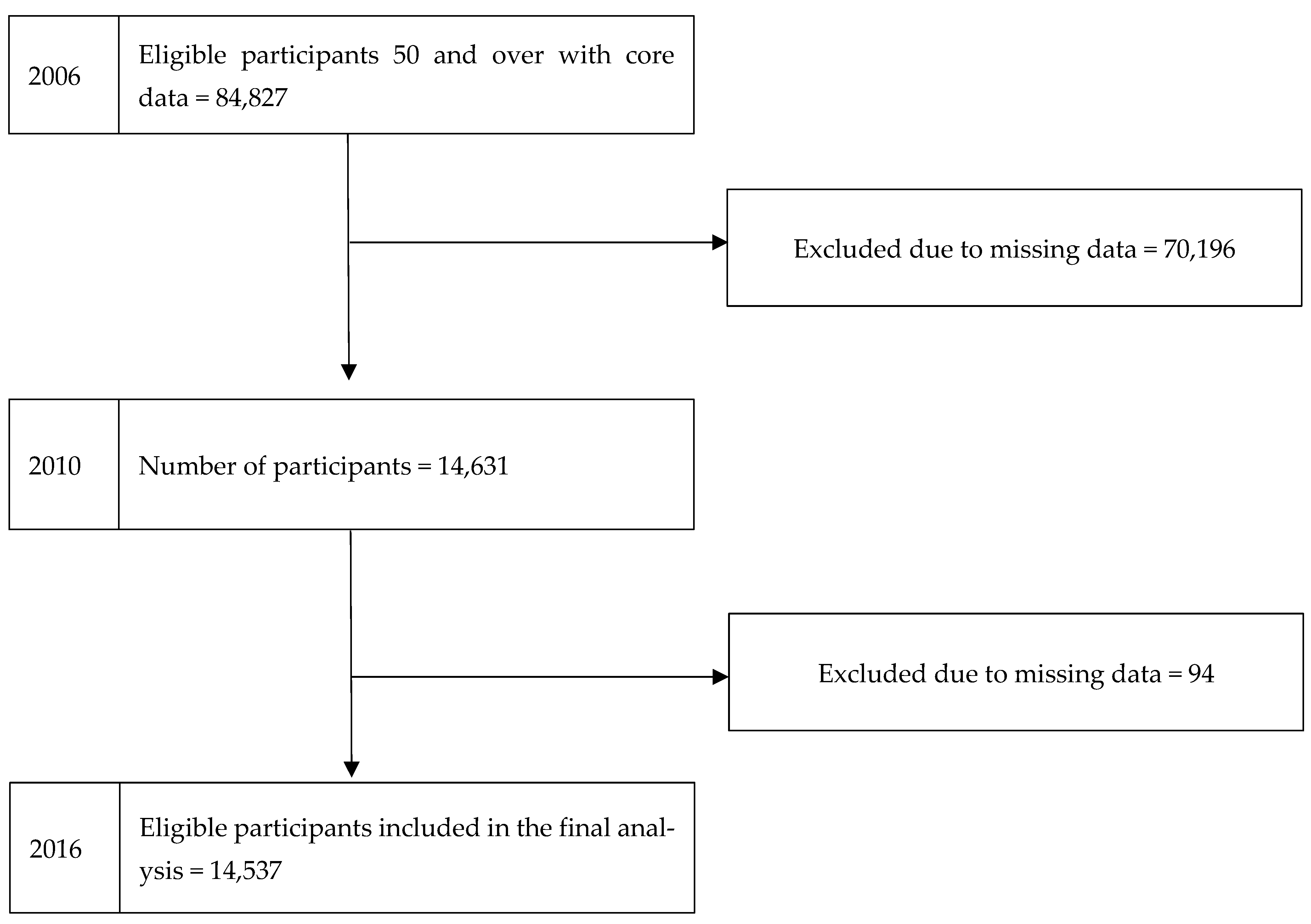
2.2. Study Design and Sample
2.3. Study Variables
2.4. Statistical Analysis
3. Results
3.1. Characteristics of the Study Sample
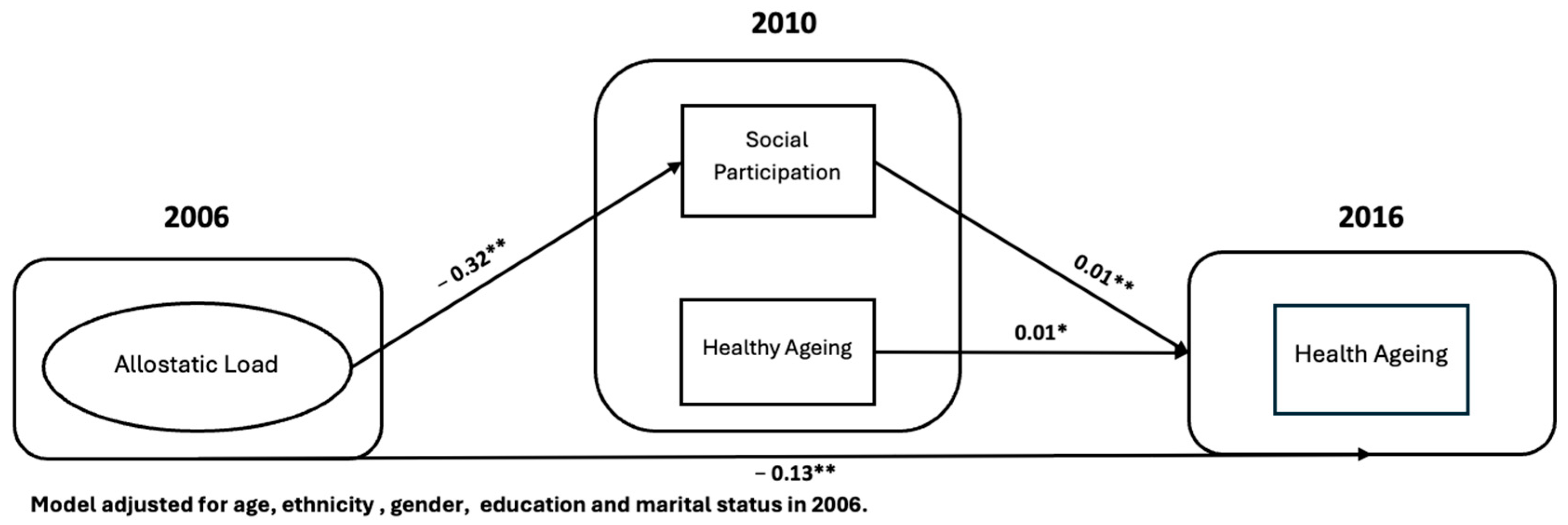
3.2. Pathways Linking Allostatic Load to Healthy Ageing
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. World Report on Ageing and Health; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Prince, J.B.; Davis, H.L.; Tan, J.; Muller-Townsend, K.; Markovic, S.; Lewis, D.M.G.; Hastie, B.; Thompson, M.B.; Drummond, P.D.; Fujiyama, H.; et al. Cognitive and neuroscientific perspectives of healthy ageing. Neurosci. Biobehav. Rev. 2024, 161, 105649. [Google Scholar] [CrossRef]
- McEwen, B.S.; Stellar, E. Stress and the individual. Mechanisms leading to disease. Arch. Intern. Med. 1993, 153, 2093–2101. [Google Scholar] [CrossRef] [PubMed]
- McEwen, B.S.; Seeman, T. Protective and damaging effects of mediators of stress. Elaborating and testing the concepts of allostasis and allostatic load. Ann. N. Y Acad. Sci. 1999, 896, 30–47. [Google Scholar] [CrossRef] [PubMed]
- Juster, R.P.; McEwen, B.S.; Lupien, S.J. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci. Biobehav. Rev. 2010, 35, 2–16. [Google Scholar] [CrossRef]
- Gouin, J.P.; Glaser, R.; Malarkey, W.B.; Beversdorf, D.; Kiecolt-Glaser, J. Chronic stress, daily stressors, and circulating inflammatory markers. Health Psychol. 2012, 31, 264–268. [Google Scholar] [CrossRef]
- Alcolea, D.; Beeri, M.S.; Rojas, J.C.; Gardner, R.C.; Lleó, A. Blood Biomarkers in Neurodegenerative Diseases. Neurology 2023, 101, 172–180. [Google Scholar] [CrossRef] [PubMed]
- Feng, L.; Ye, Z.; Du, Z.; Pan, Y.; Canida, T.; Ke, H.; Liu, S.; Chen, S.; Hong, L.E.; Kochunov, P.; et al. Association between allostatic load and accelerated white matter brain aging: Findings from the UK Biobank. medRxiv 2024, 194, 2376–2384. [Google Scholar] [CrossRef]
- Seeman, T.E.; McEwen, B.S.; Rowe, J.W.; Singer, B.H. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proc. Natl. Acad. Sci. USA 2001, 98, 4770–4775. [Google Scholar] [CrossRef]
- Danese, A.; McEwen, B.S. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol. Behav. 2012, 106, 29–39. [Google Scholar] [CrossRef]
- Mira, R.; Newton, J.T.; Sabbah, W. The Longitudinal Relationship Between Allostatic Load and Multimorbidity Among Older Americans. Geriatrics 2025, 10, 84. [Google Scholar] [CrossRef]
- Holt-Lunstad, J.; Smith, T.B.; Layton, J.B. Social relationships and mortality risk: A meta-analytic review. PLoS Med. 2010, 7, e1000316. [Google Scholar] [CrossRef]
- Cohen, S.; Wills, T.A. Stress, social support, and the buffering hypothesis. Psychol. Bull. 1985, 98, 310–357. [Google Scholar] [CrossRef]
- Sherman, S.M.; Cheng, Y.-P.; Fingerman, K.L.; Schnyer, D.M. Social support, stress and the aging brain. Soc. Cogn. Affect. Neurosci. 2016, 11, 1050–1058. [Google Scholar] [CrossRef] [PubMed]
- CDC. Healthy Weight, Nutrition, and Physical Activity. 2023. Available online: https://www.cdc.gov/healthyweight/index.html (accessed on 1 August 2025).
- Singh, B.; Goyal, A.; Patel, B.C. C-Reactive Protein: Clinical Relevance and Interpretation. In Treasure Island; StatPearls Publishing: Orlando, FL, USA, 2025. [Google Scholar]
- AHA. What Your Cholesterol Levels Mean. 2024. Available online: https://www.heart.org/en/health-topics/cholesterol/about-cholesterol/what-your-cholesterol-levels-mean (accessed on 10 August 2025).
- ADA. Understanding A 1 C Test. 2025. Available online: https://diabetes.org/about-diabetes/a1c (accessed on 10 August 2025).
- AHA. Understanding Blood Pressure Readings. 2025. Available online: https://www.heart.org/en/health-topics/high-blood-pressure/understanding-blood-pressure-readings (accessed on 10 August 2025).
- McLaughlin, S.J.; Connell, C.M.; Heeringa, S.G.; Li, L.W.; Roberts, J.S. Successful aging in the United States: Prevalence estimates from a national sample of older adults. J. Gerontol. B Psychol. Sci. Soc. Sci. 2010, 65, 216–226. [Google Scholar] [CrossRef]
- WHO. Decade of Healthy Ageing: Plan of Action; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Sahab, L.; Newton, J.T.; Sabbah, W. The Nutritional Pathway Between Tooth Loss and Healthy Ageing: A Longitudinal Study of Older American Adults. Nutrients 2025, 17, 719. [Google Scholar] [CrossRef] [PubMed]
- Seeman, T.E.; Singer, B.H.; Rowe, J.W.; Horwitz, R.I.; McEwen, B.S. Price of adaptation--allostatic load and its health consequences. MacArthur studies of successful aging. Arch. Intern. Med. 1997, 157, 2259–2268. [Google Scholar] [CrossRef]
- Tampubolon, G.; Maharani, A. Trajectories of allostatic load among older Americans and Britons: Longitudinal cohort studies. BMC Geriatr. 2018, 18, 255. [Google Scholar] [CrossRef]
- Kawachi, I.; Kennedy, B.P.; Glass, R. Social capital and self-rated health: A contextual analysis. Am. J. Public Health 1999, 89, 1187–1193. [Google Scholar] [CrossRef] [PubMed]
- Fiorillo, D.; Sabatini, F. Structural social capital and health in Italy. Econ. Hum. Biol. 2015, 17, 129–142. [Google Scholar] [CrossRef]
- Gunnar, M.R.; Hostinar, C.E. The social buffering of the hypothalamic-pituitary-adrenocortical axis in humans: Developmental and experiential determinants. Soc. Neurosci. 2015, 10, 479–488. [Google Scholar] [CrossRef]
- Smith, K.J.; Gavey, S.; NE, R.I.; Kontari, P.; Victor, C. The association between loneliness, social isolation and inflammation: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2020, 112, 519–541. [Google Scholar] [CrossRef]
- Ihara, S.; Ide, K.; Kanamori, S.; Tsuji, T.; Kondo, K.; Iizuka, G. Social participation and change in walking time among older adults: A 3-year longitudinal study from the JAGES. BMC Geriatr. 2022, 22, 238. [Google Scholar] [CrossRef]
- Schroeder, T.; Ozieh, M.N.; Thorgerson, A.; Williams, J.S.; Walker, R.J.; Egede, L.E. Social Risk Factor Domains and Preventive Care Services in US Adults. JAMA Netw. Open 2024, 7, e2437492. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.S.; Tkatch, R.; Martin, D.; MacLeod, S.; Sandy, L.; Yeh, C. Resilient Aging: Psychological Well-Being and Social Well-Being as Targets for the Promotion of Healthy Aging. Gerontol. Geriatr. Med. 2021, 7, 23337214211002951. [Google Scholar] [CrossRef]
- Clouston, S.A.P.; Smith, D.M.; Mukherjee, S.; Zhang, Y.; Hou, W.; Link, B.G.; Richards, M. Education and Cognitive Decline: An Integrative Analysis of Global Longitudinal Studies of Cognitive Aging. J. Gerontol. B Psychol. Sci. Soc. Sci. 2020, 75, e151–e160. [Google Scholar] [CrossRef]
- Markides, K.S.; Eschbach, K. Aging, Migration, and Mortality: Current Status of Research on the Hispanic Paradox. J. Gerontol. Ser. B 2005, 60, S68–S75. [Google Scholar] [CrossRef]
- Chatters, L.M.; Taylor, R.J.; Woodward, A.T.; Nicklett, E.J. Social support from church and family members and depressive symptoms among older African Americans. Am. J. Geriatr. Psychiatry 2015, 23, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Garcia, M.A.; Garcia, C.; Chiu, C.T.; Raji, M.; Markides, K.S. A Comprehensive Analysis of Morbidity Life Expectancies Among Older Hispanic Subgroups in the United States: Variation by Nativity and Country of Origin. Innov. Aging 2018, 2, igy014. [Google Scholar] [CrossRef] [PubMed]
- Banks, J.; Muriel, A.; Smith, J.P. Attrition and health in ageing studies: Evidence from ELSA and HRS. Longit. Life Course Stud. 2011, 2, 1–29. [Google Scholar]
- Beller, J.; Geyer, S.; Epping, J. Health and study dropout: Health aspects differentially predict attrition. BMC Med. Res. Methodol. 2022, 22, 31. [Google Scholar] [CrossRef]
| Year | Variables | Mean/Percentage | |
|---|---|---|---|
| Gender | Male | 41.7% | |
| Female | 58.3% | ||
| Ethnicity | Black | 13.9% | |
| Non-Black | 86.1% | ||
| Education | <High school | 22.8% | |
| High school/equivalent | 52.4% | ||
| Some college | 4.3% | ||
| College and above | 28.5% | ||
| 2006 | |||
| Age (mean) | 68.7 (95%CI: 68.5–68.8) | ||
| Marital status | Married | 64.5% | |
| Unmarried/divorced | 14.1% | ||
| Widowed | 21.4% | ||
| Waist circumference | High risk | 60.8% | |
| C-reactive protein | Elevated | 19.2% | |
| Glycated hemoglobin | Diabetic | 12.2% | |
| Blood pressure | Elevated | 17.7% | |
| High density lipoprotein | Elevated | 8.4% | |
| 2010 | |||
| Healthy ageing | 53.8% | ||
| Social participation | 78.3% | ||
| 2016 | |||
| Healthy ageing (outcome) | 50.3% | ||
| Variables | Estimate | 95% CI | p-Value | |
|---|---|---|---|---|
| Allostatic Load 2006 (Latent Variable) | ||||
| Waist circumference | 0.95 | (0.94, 0.96) | <0.001 | |
| C-reactive protein | −0.90 | (−0.90, −0.89) | <0.001 | |
| High density lipoprotein | −0.37 | (−0.38, −0.35) | <0.001 | |
| Glycated hemoglobin | −0.35 | (−0.38, −0.33) | <0.001 | |
| Blood pressure | 0.07 | (0.05, 0.09) | <0.001 | |
| Social Participation 2010 | ||||
| Allostatic load 2006 | −0.32 | (−0.34, −0.30) | <0.001 | |
| Healthy ageing 2016 | ||||
| 2006 | AL | −0.12 | (−0.14, 0.11) | <0.001 |
| Education | 0.18 | (0.17, 0.19) | <0.001 | |
| Age | 0.36 | (0.35, 0.37) | <0.001 | |
| Marital status | 0.02 | (0.00, 0.03) | NS | |
| Gender | −0.01 | (−0.02, 0.01) | NS | |
| Ethnicity | −0.11 | (−0.12, −0.10) | <0.001 | |
| 2010 | Social Participation | 0.05 | (0.04, 0.06) | <0.001 |
| Healthy ageing | 0.10 | (0.08, 0.12) | <0.001 | |
| Model fit | ||||
| RMSEA | 0.54 | <0.001 | ||
| CFI | 0.05 | |||
| TLI | 0.00 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sahab, L.; Newton, J.T.; Sabbah, W. Allostatic Load, Social Participation, and Healthy Ageing: Longitudinal Evidence on the Impact of Chronic Stress. Geriatrics 2025, 10, 157. https://doi.org/10.3390/geriatrics10060157
Sahab L, Newton JT, Sabbah W. Allostatic Load, Social Participation, and Healthy Ageing: Longitudinal Evidence on the Impact of Chronic Stress. Geriatrics. 2025; 10(6):157. https://doi.org/10.3390/geriatrics10060157
Chicago/Turabian StyleSahab, Lujain, Jonathon Timothy Newton, and Wael Sabbah. 2025. "Allostatic Load, Social Participation, and Healthy Ageing: Longitudinal Evidence on the Impact of Chronic Stress" Geriatrics 10, no. 6: 157. https://doi.org/10.3390/geriatrics10060157
APA StyleSahab, L., Newton, J. T., & Sabbah, W. (2025). Allostatic Load, Social Participation, and Healthy Ageing: Longitudinal Evidence on the Impact of Chronic Stress. Geriatrics, 10(6), 157. https://doi.org/10.3390/geriatrics10060157







