Effects of the Prescription of Physical Exercises Mediated by Mobile Applications on the Health of Older Adults: A Systematic Review
Abstract
1. Introduction
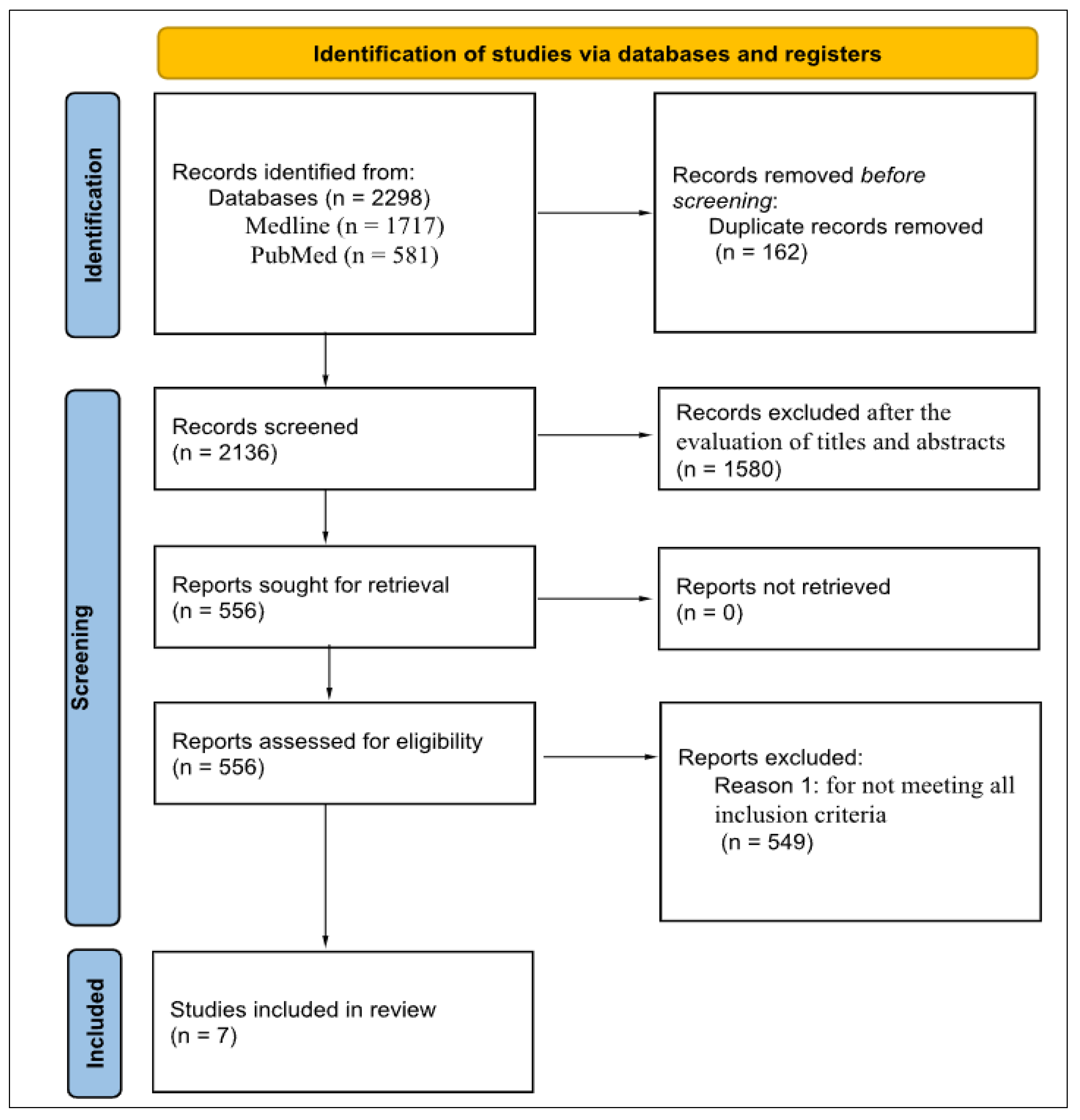
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Database and Search Strategy
2.3. Data Selection and Collection Process
2.4. Assessment of the Risk of Bias in Studies
2.5. Summary of Results
3. Results
Characteristics of the Included Studies
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- de Azeredo Passos, V.M.; Champs, A.P.S.; Teixeira, R.; Lima-Costa, M.F.F.; Kirkwood, R.; Veras, R.; Nascimento, B.R.; Nogales, A.M.; Schmidt, M.I.; Duncan, B.B.; et al. The burden of disease among Brazilian older adults and the challenge for health policies: Results of the Global Burden of Disease Study 2017. Popul. Health Metr. 2020, 18, 14. [Google Scholar] [CrossRef] [PubMed]
- Ferla, A.; Nicoli, M.A.; Funghetto, S.S. Comparação do envelhecimento populacional no Brasil e na Itália. Rev. Diálogos Gerontol. 2024, 1, 26–35. Available online: https://revista.redegeronto.com.br/index.php/dialogos/article/view/9 (accessed on 25 June 2025).
- World Health Organization (WHO). World Health Statistics 2019: Monitoring Health for the SDGs, Sustainable Development Goals; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- Länsitie, M.; Kangas, M.; Jokelainen, J.; Venojärvi, M.; Timonen, M.; Keinänen-Kiukaanniemi, S.; Korpelainen, R. Cardiovascular disease risk and all-cause mortality associated with accelerometer-measured physical activity and sedentary time—A population-based prospective cohort study in older adults. BMC Geriatr. 2022, 22, 729. [Google Scholar] [CrossRef] [PubMed]
- Frota, R.S.; Spaziani, A.O.; Alves, A.F.R.F.B.; Alves, B.R.F.B.; Azerêdo, L.; Santos, M.V.F.; Netto, E.S.S.; Spaziani, L.C. The Interference of Sedentarism in Elderly People with Chronic Noncommunicable Diseases. Braz. J. Health Rev. 2020, 3, 10518–10529. [Google Scholar] [CrossRef]
- Fong, J.H. Disability incidence and functional decline among older adults with major chronic diseases. BMC Geriatr. 2019, 19, 323. [Google Scholar] [CrossRef]
- Parra-Rizo, M.A.; Sanchís-Soler, G. Physical activity and improvement of autonomy, functional ability, subjective health, and social relationships in women over the age of 60. Int. J. Environ. Res. Public Health 2021, 18, 6926. [Google Scholar] [CrossRef]
- Socoloski, T.S.; Rech, C.R.; Correa Junior, J.A.; Lopes, R.M.; Hino, A.A.F.; Guerra, P.H. Barriers to physical activity in elderly: Scoping review of Brazilian studies. Rev. Bras. Ativ. Fís. Saúde 2021, 26, 1–8. [Google Scholar] [CrossRef]
- Zhang, M.; Wang, W.; Li, M.; Sheng, H.; Zhai, Y. Efficacy of mobile health applications to improve physical activity and sedentary behavior: A systematic review and meta-analysis for physically inactive individuals. Int. J. Environ. Res. Public Health 2022, 19, 4905. [Google Scholar] [CrossRef]
- Kunitake, A.I.; Dias, K.S.; Vegh, H.P.; Ramos, L.G.; Bossert, V.G.; Bezerra, H.S.; Solai, M.J.S.; Corrêa, F.I. Effects of the exercise mobile app and distance supervision on the functional performance of the older adults. Protocol of a clinical, randomized, controlled trial. Rev. Ciênc. Saúde 2022, 12, 61–65. [Google Scholar] [CrossRef]
- Lorenzi, L.J.; Belo, L.F.; Frohlich, D.M.; Dourado, V.Z.; Castro, P.C.; Gomes, G.A.O. Factors related to the adoption and adherence of physical activity mobile applications by older people: A scoping review protocol. BMJ Open 2021, 11, e052414. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. PLoS Med. 2021, 18, e1003583. [Google Scholar] [CrossRef]
- Santos, C.M.C.; Pimenta, C.A.M.; Nobre, M.R.C. The PICO strategy for the research question construction and evidence search. Rev. Lat.-Am. Enferm. 2007, 15, 508–511. [Google Scholar] [CrossRef] [PubMed]
- JBI. Joanna Briggs Institute. JBI Levels of Evidence. Available online: https://jbi.global/sites/default/files/2019-05/JBI-Levels-of-evidence_2014_0.pdf (accessed on 5 May 2025).
- Loh, K.P.; Sanapala, C.; Di Giovanni, G.; Klepin, H.D.; Janelsins, M.; Schnall, R.; Culakova, E.; Vertino, P.; Susiarjo, M.; Mendler, J.H.; et al. Developing and adapting a mobile health exercise intervention for older patients with myeloid neoplasms: A qualitative study. J. Geriatr. Oncol. 2021, 12, 909–914. [Google Scholar] [CrossRef] [PubMed]
- Snoek, J.A.; Prescott, E.I.; van der Velde, A.E.; Eijsvogels, T.M.H.; Mikkelsen, N.; Prins, L.F.; Bruins, W.; Meindersma, E.; González-Juanatey, J.R.; Peña-Gil, C.; et al. Effectiveness of home-based mobile guided cardiac rehabilitation as alternative strategy for nonparticipation in clinic-based cardiac rehabilitation among elderly patients in Europe: A randomized clinical trial. JAMA Cardiol. 2021, 6, 463–468. [Google Scholar] [CrossRef] [PubMed]
- Bonato, M.; Marmondi, F.; Mastropaolo, C.; Inzaghi, C.; Cerizza, C.; Galli, L.; Banfi, G.; Cinque, P. A digital platform for home-based exercise prescription for older people with sarcopenia. Sensors 2024, 24, 4788. [Google Scholar] [CrossRef]
- Ahn, J.H.; Shin, D.F.; Lee, D.; Kim, H.Y.; Youn, J.; Cho, J.W. Increasing exercise with a mobile app in people with Parkinson’s disease: A pilot study. Brain Impair. 2024, 25, IB23061. [Google Scholar] [CrossRef]
- Kim, A.; Yun, S.J.; Sung, K.S.; Kim, Y.; Jo, J.Y.; Cho, H.; Park, K.; Oh, B.M.; Seo, H.G. Exercise management using a mobile app in patients with Parkinsonism: Prospective, open-label, single-arm pilot study. JMIR mHealth uHealth 2021, 9, e27662. [Google Scholar] [CrossRef]
- Phillips, S.M.; Conroy, D.E.; Keadle, S.K.; Pellegrini, C.A.; Lloyd, G.R.; Penedo, F.J.; Spring, B. Breast cancer survivors’ preferences for technology-supported exercise interventions. Support. Care Cancer 2017, 25, 3243–3252. [Google Scholar] [CrossRef]
- Daly, R.M.; Gianoudis, J.; Hall, T.; Mundell, N.L.; Maddison, R. Feasibility, usability, and enjoyment of a home-based exercise program delivered via an exercise app for musculoskeletal health in community-dwelling older adults: Short-term prospective pilot study. JMIR mHealth uHealth 2021, 9, e21094. [Google Scholar] [CrossRef]
- Chung, C.; Lee, J.W.; Lee, S.W.; Jo, M.W. Clinical efficacy of mobile app–based, self-directed pulmonary rehabilitation for patients with chronic obstructive pulmonary disease: Systematic review and meta-analysis. JMIR mHealth uHealth 2024, 12, e41753. [Google Scholar] [CrossRef]
- Soto-Bagaria, L.; Eis, S.; Pérez, L.M.; Villa-García, L.; Solà-Morales, O.; Carrion, C.; Giné-Garriga, M.; Inzitari, M. Mobile applications to prescribe physical exercise in frail older adults: Review of the available tools in app stores. Age Ageing 2023, 52, afad227. [Google Scholar] [CrossRef]
- McGarrigle, L.; Boulton, E.; Todd, C. Map the apps: A rapid review of digital approaches to support the engagement of older adults in strength and balance exercises. BMC Geriatr. 2020, 20, 483. [Google Scholar] [CrossRef]
| Author and Year | Level of Evidence |
|---|---|
| Ahn, et al. (2024) [18] | LEVEL III.1 |
| Daly, et al. (2021) [20] | LEVEL III.2 |
| Phillips, et al. (2017) [21] | LEVEL III.2 |
| Loh, et al. (2021) [15] | LEVEL II |
| Kim, et al. (2021) [19] | LEVEL III.2 |
| Snoek, et al. (2020) [16] | LEVEL II |
| Bonato, et al. (2024) [17] | LEVEL II |
| Author, Year and Country | Design | Objective | Sample/Methodology | Results | Outcomes |
|---|---|---|---|---|---|
| Ahn, et al. (2024) [18]; Republic of Korea | Non-randomized clinical trial | Evaluate the effectiveness of the APP in increasing PA, ↓ cost barriers to exercise, and ↑ QOL. | N = 41, mean age 64.1 years; multicomponent PE with moderate intensity (15 to 20 min with APP: Parkinson Exercise) | ↑ Moderate PA, ↑ QOL | 25 individuals completed the 2-week program |
| Daly, et al. (2021) [21]; Australia | Prospective pilot study | Evaluate the functionality and ease of use of the PE prescription APP | N = 20, ≥65 years; multicomponent PE with Physitrack APP (3x/week) | ↑ Walking (78 min), ↑ Moderate/vigorous PA (41 min) | Safe and viable for older people monitored by professionals |
| Author, Year and Country | Design | Objective | Sample/Methodology | Results | Outcomes |
|---|---|---|---|---|---|
| Phillips et al. (2017) [20]; Germany | Cross-sectional observational | To explore interest in technology-mediated PE programs for breast cancer survivors | N = 279, average age 60.7; Survey on preferences and interests in technology-mediated PE | ↑ Advice, ↑ PE remotely | Interventions with technology can be viable and acceptable |
| Loh et al. (2021) [15]; USA | Randomized clinical trial | Informing the design of an APP-based exercise intervention for patients with myeloid neoplasms | N = 13, mean age 71.6 ± 8.5 years, medication use; PE in weeks 2 and 4 of the treatment cycle, using the EXCAP program and PointClickCare APP | ↑ Acceptance of the intervention for the preservation of functional capacity/habitual activity | ↑ feasibility of the intervention, ↓ resistance to the use of technology |
| Kim et al. (2021) [19]; Republic of Korea | Open prospective single-arm study | Evaluating the effects of home PE with a personalized mobile APP on the amount of exercise, PA, QOL and depression in people with Parkinson’s disease | N = 28, average age ≥ 72 years; individualized multimodal PE for 8 weeks with personalized mobile APP | ↑ Total exercise time, ↑ Functional components, ↑ BP, ↓ Depression | ↑ EP adherence, ↑ QOL, ↓ Depression |
| Snoek et al. (2020) [16]; 5 European countries | Randomized clinical trial | Evaluate the effectiveness of a home-based rehabilitation program with remote monitoring and motivational coaching to achieve PE goals | N = 179, ≥65 years; Home cardiac rehabilitation for 6 months with smartphone (moderate PE, 5x/week, 30 min) | ↑ VO2, ↓ Incidence of complications | ↑ Motivation, Insurance, ↑ Membership |
| Bonato et al. (2024) [17]; Italy | Randomized clinical trial | Evaluating the effectiveness of a digital platform for prescribing home exercises for elderly people with sarcopenia, including people living with HIV | N = 188, ≥60 years or ≥50 years for PHIV+ sarcopenia; 48-week intervention using the Gym-Grow platform for prescribing home PE | 83% adherence, ↑ Muscle strength, ↓ Difficulties finding the APP | ↑ Efficiency in prescribing, ↑ Adherence |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Costa, D.V.S.D.; Dourado, E.P.; Fernandes, M.B.; Fernandes, E.V.; de Oliveira, D.M. Effects of the Prescription of Physical Exercises Mediated by Mobile Applications on the Health of Older Adults: A Systematic Review. Geriatrics 2025, 10, 122. https://doi.org/10.3390/geriatrics10050122
Costa DVSD, Dourado EP, Fernandes MB, Fernandes EV, de Oliveira DM. Effects of the Prescription of Physical Exercises Mediated by Mobile Applications on the Health of Older Adults: A Systematic Review. Geriatrics. 2025; 10(5):122. https://doi.org/10.3390/geriatrics10050122
Chicago/Turabian StyleCosta, Débora Vanessa Santos Dias, Evellin Pereira Dourado, Mayara Bocchi Fernandes, Eduardo Vignoto Fernandes, and David Michel de Oliveira. 2025. "Effects of the Prescription of Physical Exercises Mediated by Mobile Applications on the Health of Older Adults: A Systematic Review" Geriatrics 10, no. 5: 122. https://doi.org/10.3390/geriatrics10050122
APA StyleCosta, D. V. S. D., Dourado, E. P., Fernandes, M. B., Fernandes, E. V., & de Oliveira, D. M. (2025). Effects of the Prescription of Physical Exercises Mediated by Mobile Applications on the Health of Older Adults: A Systematic Review. Geriatrics, 10(5), 122. https://doi.org/10.3390/geriatrics10050122








