Hormonal Homologies between Canine Mammary Cancer and Human Breast Cancer in a Series of Cases
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Sampling
2.1.1. Human Breast Samples
2.1.2. Canine Mammary Samples
2.2. Sample Processing
2.2.1. Histopathology and Immunohistochemistry
2.2.2. Assessment of Steroid Concentrations in Tumor Homogenate Samples
2.3. Statistical Study
3. Results
3.1. Histopathology
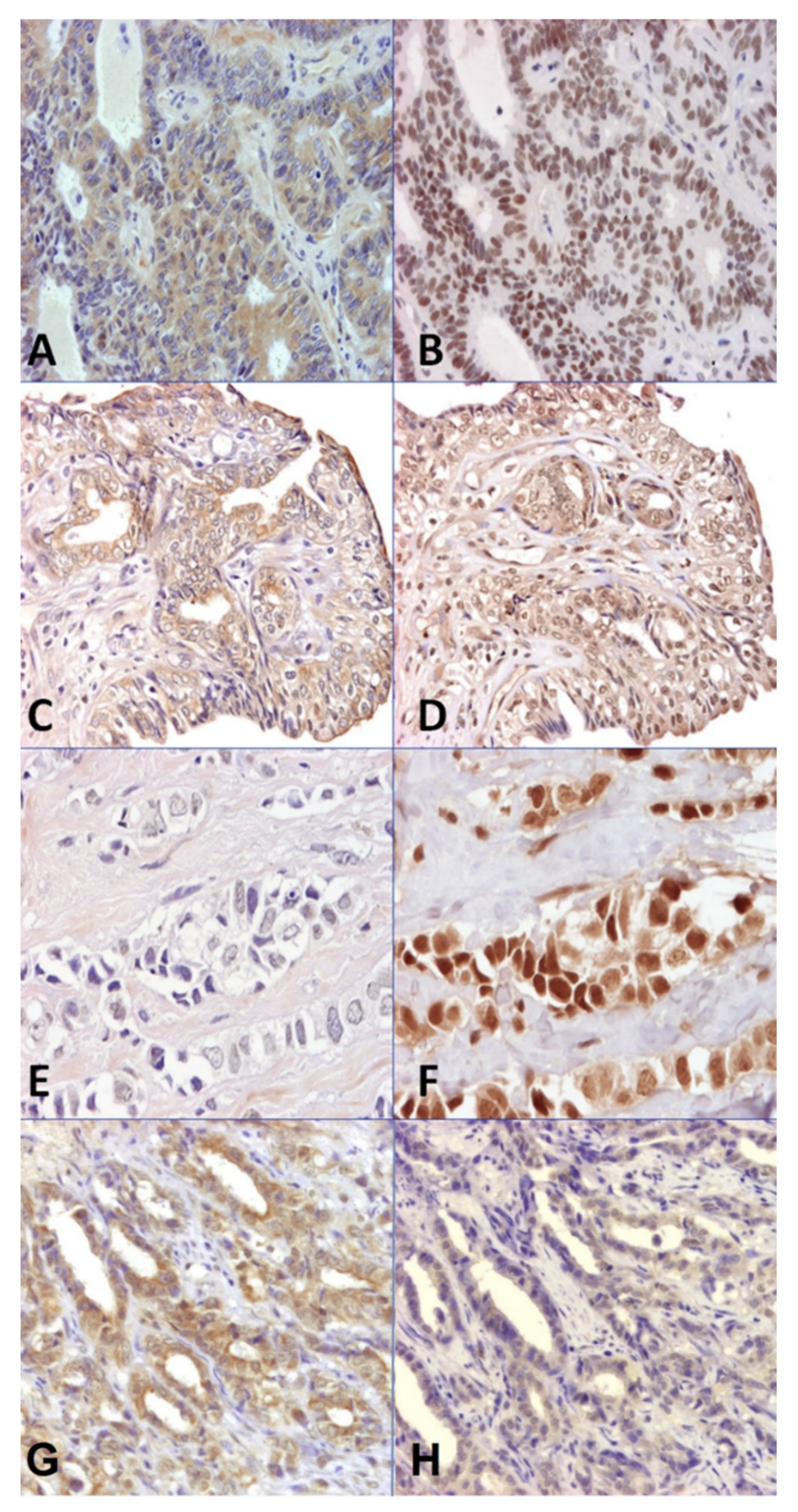
3.2. Immunoexpression of Arom, ERα, ERβ, PR, and AR
3.3. Steroid Concentrations in Tumor Homogenate Samples
3.4. Statistical Associations among Aromatase, Receptors, and Steroid Hormones
3.4.1. Arom Associations
3.4.2. Steroid Receptor Associations
3.4.3. Associations among the Different Hormonal Tissue Concentrations
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Boyle, P.; Ferlay, J. Cancer incidence and mortality in Europe, 2004. Ann. Oncol. 2005, 16, 481–488. [Google Scholar] [CrossRef] [PubMed]
- Du, X.L.; Fox, E.E.; Lai, D. Competing Causes of Death for Women with Breast Cancer and Change over Time from 1975 to 2003. Am. J. Clin. Oncol. 2008, 31, 105–116. [Google Scholar] [CrossRef] [PubMed]
- Dorn, C.R.; Taylor, D.O.; Schneider, R.; Hibbard, H.H.; Klauber, M.R. Survey of animal neoplasms in Alameda and Contra Costa Counties, California. II. Cancer morbidity in dogs and cats from Alameda County. J. Natl. Cancer Inst. 1968, 40, 307–318. [Google Scholar]
- Schneider, R.; Dorn, C.R.; Taylor, D.O.N. Factors Influencing Canine Mammary Cancer Development and Postsurgical Survival2. J. Natl. Cancer Inst. 1969, 43, 1249–1261. [Google Scholar] [CrossRef] [PubMed]
- Clemente, M.; Pérez-Alenza, M.; Peña, L. Metastasis of Canine Inflammatory versus Non-Inflammatory Mammary Tumours. J. Comp. Pathol. 2010, 143, 157–163. [Google Scholar] [CrossRef]
- Misdorp, W. Tumors of the mammary gland. In Tumors in Domestic Animals; Meuten, D.J., Ed.; Wiley-Blackwell: Ames, IA, USA, 2002; pp. 575–588. [Google Scholar]
- MacEwen, E.G. Spontaneous tumors in dogs and cats: Models for the study of cancer biology and treatment. Cancer Metastasis Rev. 1990, 9, 125–136. [Google Scholar] [CrossRef] [PubMed]
- Knapp, D.W.; Waters, D.J. Naturally occurring cancer in pet dogs: Important models for developing improved cancer therapy for humans. Mol. Med. Today 1997, 3, 8–11. [Google Scholar] [CrossRef]
- Vail, D.M.; MacEwen, E.G. Spontaneously Occurring Tumors of Companion Animals as Models for Human Cancer. Cancer Investig. 2000, 18, 781–792. [Google Scholar] [CrossRef] [PubMed]
- Antuofermo, E.; Miller, M.A.; Pirino, S.; Xie, J.; Badve, S.; Mohammed, S.I. Spontaneous Mammary Intraepithelial Lesions in Dogs—A Model of Breast Cancer. Cancer Epidemiol. Biomark. Prev. 2007, 16, 2247–2256. [Google Scholar] [CrossRef]
- Peña, L.; Perez-Alenza, M.D.; Rodriguez-Bertos, A.; Nieto, A. Canine Inflammatory Mammary Carcinoma: Histopathology, Immunohistochemistry and Clinical Implications of 21 Cases. Breast Cancer Res. Treat. 2003, 78, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Xiong, H.; Ellis, A.E.; Northrup, N.C.; Rodriguez, C.O., Jr.; O’Regan, R.M.; Dalton, S.; Zhao, S. Molecular Homology and Difference between Spontaneous Canine Mammary Cancer and Human Breast Cancer. Cancer Res. 2014, 74, 5045–5056. [Google Scholar] [CrossRef] [PubMed]
- De Andres, P.J.; Caceres, S.; Clemente, M.; Perez-Alenza, M.D.; Illera, J.C.; Pena, L. Profile of Steroid Receptors and Increased Aromatase Immunoexpression in Canine Inflammatory Mammary Cancer as a Potential Therapeutic Target. Reprod. Domest. Anim. 2016, 51, 269–275. [Google Scholar] [CrossRef] [PubMed]
- De las Mulas, J.M.D.L.; Reymundo, C. Animal models of human breast carcinoma: Canine and feline neoplasms. Rev. Oncol. 2000, 2, 274–281. [Google Scholar] [CrossRef]
- Queiroga, F.L.; Raposo, T.; Carvalho, M.; Prada, J.; Pires, I. Canine mammary tumours as a model to study human breast cancer: Most recent findings. In Vivo 2011, 25, 455–465. [Google Scholar] [PubMed]
- Abdelmegeed, S.M.; Mohammed, S. Canine mammary tumors as a model for human disease. Oncol. Lett. 2018, 15, 8195–8205. [Google Scholar] [CrossRef]
- Brandão, Y.D.O.; Toledo, M.B.; Chequin, A.; Cristo, T.G.; Sousa, R.S.; Ramos, E.A.S.; Klassen, G. DNA Methylation Status of the Estrogen Receptor α Gene in Canine Mammary Tumors. Vet. Pathol. 2018, 55, 510–516. [Google Scholar] [CrossRef]
- Goldschmidt, M.; Peña, L.; Rasotto, R.; Zappulli, V. Classification and Grading of Canine Mammary Tumors. Vet. Pathol. 2011, 48, 117–131. [Google Scholar] [CrossRef] [PubMed]
- Feldman, E.C.; Nelson, R.W. Canine and Feline Endocrinology and Reproduction, 3rd ed.; W.B. Saunders: St. Louis, MO, USA, 2004. [Google Scholar]
- Kim, N.-H.; Lim, H.-Y.; Im, K.-S.; Shin, J.-I.; Kim, H.-W.; Sur, J.-H. Evaluation of Clinicopathological Characteristics and Oestrogen Receptor Gene Expression in Oestrogen Receptor-negative, Progesterone Receptor-positive Canine Mammary Carcinomas. J. Comp. Pathol. 2014, 151, 42–50. [Google Scholar] [CrossRef] [PubMed]
- Mainenti, M.; Rasotto, R.; Carnier, P.; Zappulli, V. Oestrogen and progesterone receptor expression in subtypes of canine mammary tumours in intact and ovariectomised dogs. Vet. J. 2014, 202, 62–68. [Google Scholar] [CrossRef]
- Gama, A.; Alves, A.; Schmitt, F. Identification of molecular phenotypes in canine mammary carcinomas with clinical implications: Application of the human classification. Virchows Arch. 2008, 453, 123–132. [Google Scholar] [CrossRef]
- Yang, W.-Y.; Liu, C.-H.; Chang, C.-J.; Lee, C.-C.; Chang, K.J.; Lin, C.-T. Proliferative Activity, Apoptosis and Expression of Oestrogen Receptor and Bcl-2 Oncoprotein in Canine Mammary Gland Tumours. J. Comp. Pathol. 2006, 134, 70–79. [Google Scholar] [CrossRef] [PubMed]
- Peña, L.; Silván, G.; Pérez-Alenza, M.D.; Nieto, A.; Illera, J.C. Steroid hormone profile of canine inflammatory mammary carcinoma: A preliminary study. J. Steroid Biochem. Mol. Biol. 2003, 84, 211–216. [Google Scholar] [CrossRef]
- Kabir, F.M.L.; DeInnocentes, P.; Agarwal, P.; Mill, C.P.; Riese, D.J.; Bird, R.C. Estrogen receptor-α, progesterone receptor, and c-erbB/HER-family receptor mRNA detection and phenotype analysis in spontaneous canine models of breast cancer. J. Vet. Sci. 2017, 18, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Terzaghi, L.; Banco, B.; Groppetti, D.; Dall’Acqua, P.C.; Giudice, C.; Pecile, A.; Grieco, V.; Lodde, V.; Luciano, A.M. Progesterone receptor membrane component 1 (PGRMC1) expression in canine mammary tumors: A preliminary study. Res. Vet. Sci. 2020, 132, 101–107. [Google Scholar] [CrossRef]
- Nieto, A.; Peña, L.; Pérez-Alenza, M.D.; Sánchez, M.A.; Flores, J.M.; Castaño, M. Immunohistologic Detection of Estrogen Receptor Alpha in Canine Mammary Tumors: Clinical and Pathologic Associations and Prognostic Significance. Vet. Pathol. 2000, 37, 239–247. [Google Scholar] [CrossRef] [PubMed]
- Illera, J.C.; Pérez-Alenza, M.D.; Nieto, A.; Jiménez, M.A.; Silvan, G.; Dunner, S.; Peña, L. Steroids and receptors in canine mammary cancer. Steroids 2006, 71, 541–548. [Google Scholar] [CrossRef] [PubMed]
- Sorenmo, K.U.; Rasotto, R.; Zappulli, V.; Goldschmidt, M.H. Development, Anatomy, Histology, Lymphatic Drainage, Clinical Features, and Cell Differentiation Markers of Canine Mammary Gland Neoplasms. Vet. Pathol. 2011, 48, 85–97. [Google Scholar] [CrossRef] [PubMed]
- De Las Mulas, J.M.; Millán, Y.; Dios, R. A Prospective Analysis of Immunohistochemically Determined Estrogen Receptor α and Progesterone Receptor Expression and Host and Tumor Factors as Predictors of Disease-free Period in Mammary Tumors of the Dog. Vet. Pathol. 2005, 42, 200–212. [Google Scholar] [CrossRef] [PubMed]
- Millanta, F.; Calandrella, M.; Bari, G.; Niccolini, M.; Vannozzi, I.; Poli, A. Comparison of steroid receptor expression in normal, dysplastic, and neoplastic canine and feline mammary tissues. Res. Vet. Sci. 2005, 79, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Louis, L.R.P.; Varshney, K.C.; Nair, M.G. An Immunohistochemical Study on the Expression of Sex Steroid Receptors in Canine Mammary Tumors. ISRN Vet. Sci. 2012, 2012, 378607. [Google Scholar] [CrossRef]
- Kumaraguruparan, R.; Prathiba, D.; Nagini, S. Of humans and canines: Immunohistochemical analysis of PCNA, Bcl-2, p53, cytokeratin and ER in mammary tumours. Res. Vet. Sci. 2006, 81, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Reese, J.M.; Suman, V.J.; Subramaniam, M.; Wu, X.; Negron, V.; Gingery, A.; Pitel, K.S.; Shah, S.S.; Cunliffe, H.E.; McCullough, A.E.; et al. ERβ1: Characterization, prognosis, and evaluation of treatment strategies in ERα-positive and -negative breast cancer. BMC Cancer 2014, 14, 749. [Google Scholar] [CrossRef]
- Roger, P.; Sahla, M.E.; Mäkelä, S.; Gustafsson, J.A.; Baldet, P.; Rochefort, H. Decreased expression of estrogen receptor beta protein in proliferative preinvasive mammary tumors. Cancer Res. 2001, 61, 2537–2541. [Google Scholar] [PubMed]
- Skliris, G.P.; Carder, P.J.; Lansdown, M.R.; Speirs, V. Immunohistochemical detection of ERβ in breast cancer: Towards more detailed receptor profiling? Br. J. Cancer 2001, 84, 1095–1098. [Google Scholar] [CrossRef] [PubMed]
- Jarvinen, T.A.; Pelto-Huikko, M.; Holli, K.; Isola, J. Estrogen receptor beta is coexpressed with ERalpha and PR and associated with nodal status, grade, and proliferation rate in breast cancer. Am. J. Pathol. 2000, 156, 29–35. [Google Scholar] [CrossRef]
- Mann, S.; Laucirica, R.; Carlson, N.; Younes, P.S.; Ali, N.; Younes, A.; Li, Y.; Younes, M. Estrogen receptor beta expression in invasive breast cancer. Hum. Pathol. 2001, 32, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Martín de las Mulas, J.; Ordás, J.; Millán, M.Y.; Chacón, F.; De Lara, M.; Espinosa de los Monteros, A.; Reymundo, C.; Jover, A. Immunohistochemical Expression of Estrogen Receptor β in Normal and Tumoral Canine Mammary Glands. Vet. Pathol. 2004, 41, 269–272. [Google Scholar] [CrossRef] [PubMed]
- Shaaban, A.M.; O’Neill, P.A.; Davies, M.P.; Sibson, R.; West, C.R.; Smith, P.H.; Foster, C.S. Declining estrogen receptor-beta expression defines malignant progression of human breast neoplasia. Am. J. Surg. Pathol. 2003, 27, 1502–1512. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Peng, R.; Yuan, Z.; Wang, S.; Peng, J.; Lin, G.; Jiang, X.; Qin, T. Prognostic value of androgen receptor expression in operable triple-negative breast cancer: A retrospective analysis based on a tissue microarray. Med. Oncol. 2011, 29, 406–410. [Google Scholar] [CrossRef] [PubMed]
- Koo, J.S.; Jung, W.; Jeong, J. The Predictive Role of E-cadherin and Androgen Receptor on In Vitro Chemosensitivity in Triple-negative Breast Cancer. Jpn. J. Clin. Oncol. 2009, 39, 560–568. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pistelli, M.; Caramanti, M.; Biscotti, T.; Santinelli, A.; Pagliacci, A.; De Lisa, M.; Ballatore, Z.; Ridolfi, F.; Maccaroni, E.; Bracci, R.; et al. Androgen Receptor Expression in Early Triple-Negative Breast Cancer: Clinical Significance and Prognostic Associations. Cancers 2014, 6, 1351–1362. [Google Scholar] [CrossRef]
- Gucalp, A.; Traina, T.A. Triple-negative breast cancer: Role of the androgen receptor. Cancer J. 2010, 16, 62–65. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, B.D.; Bauer, J.A.; Schafer, J.M.; Pendleton, C.S.; Tang, L.; Johnson, K.C.; Chen, X.; Balko, J.M.; Gómez, H.; Arteaga, C.L.; et al. PIK3CA mutations in androgen receptor-positive triple negative breast cancer confer sensitivity to the combination of PI3K and androgen receptor inhibitors. Breast Cancer Res. 2014, 16, 406. [Google Scholar] [CrossRef] [PubMed]
- Luo, X.; Shi, Y.-X.; Li, Z.-M.; Jiang, W.-Q. Expression and clinical significance of androgen receptor in triple negative breast cancer. Chin. J. Cancer 2010, 29, 585–590. [Google Scholar] [CrossRef] [PubMed]
- McGhan, L.J.; McCullough, A.E.; Protheroe, C.A.; Dueck, A.C.; Lee, J.J.; Nunez-Nateras, R.; Castle, E.P.; Gray, R.J.; Wasif, N.; Goetz, M.P.; et al. Androgen Receptor-Positive Triple Negative Breast Cancer: A Unique Breast Cancer Subtype. Ann. Surg. Oncol. 2013, 21, 361–367. [Google Scholar] [CrossRef]
- McNamara, K.; Yoda, T.; Takagi, K.; Miki, Y.; Suzuki, T.; Sasano, H. Androgen receptor in triple negative breast cancer. J. Steroid Biochem. Mol. Biol. 2012, 133, 66–76. [Google Scholar] [CrossRef]
- Narayanan, R.; Ahn, S.; Cheney, M.D.; Yepuru, M.; Miller, D.D.; Steiner, M.S.; Dalton, J.T. Selective Androgen Receptor Modulators (SARMs) Negatively Regulate Triple-Negative Breast Cancer Growth and Epithelial: Mesenchymal Stem Cell Signaling. PLoS ONE 2014, 9, e103202. [Google Scholar] [CrossRef] [PubMed]
- Safarpour, D.; Tavassoli, F.A. A Targetable Androgen Receptor–Positive Breast Cancer Subtype Hidden Among the Triple-Negative Cancers. Arch. Pathol. Lab. Med. 2014, 139, 612–617. [Google Scholar] [CrossRef]
- Shah, P.D.; Gucalp, A.; Traina, T. The Role of the Androgen Receptor in Triple-Negative Breast Cancer. Women’s Health 2013, 9, 351–360. [Google Scholar] [CrossRef]
- Labrie, F.; Luu-The, V.; Labrie, C.; Beélanger, A.; Simard, J.; Lin, S.-X.; Pelletier, G. Endocrine and Intracrine Sources of Androgens in Women: Inhibition of Breast Cancer and Other Roles of Androgens and Their Precursor Dehydroepiandrosterone. Endocr. Rev. 2003, 24, 152–182. [Google Scholar] [CrossRef] [PubMed]
- Mori, M.; Tominaga, T.; Tamaoki, B.-I. Steroid Metabolism in the Normal Mammary Gland and in the Dimethylbenzanthracene-Induced Mammary Tumor of Rats. Endocrinology 1978, 102, 1387–1397. [Google Scholar] [CrossRef] [PubMed]
- Slotin, C.A.; Heap, R.B.; Christiansen, J.M.; Linzell, J.L. Synthesis of Progesterone by the Mammary Gland of the Goat. Nature 1970, 225, 385–386. [Google Scholar] [CrossRef]
- Belvedere, P.; Gabai, G.; Valle, L.D.; Accorsi, P.; Trivoletti, M.; Colombo, L.; Bono, G. Occurrence of steroidogenic enzymes in the bovine mammary gland at different functional stages. J. Steroid Biochem. Mol. Biol. 1996, 59, 339–347. [Google Scholar] [CrossRef]
- Marinelli, L.; Gabai, G.; Wolfswinkel, J.; Mol, J.A. Mammary steroid metabolizing enzymes in relation to hyperplasia and tumorigenesis in the dog. J. Steroid Biochem. Mol. Biol. 2004, 92, 167–173. [Google Scholar] [CrossRef] [PubMed]
- D’Arville, C.; Evans, B.; Borthwick, G.; Pierrepoint, C. Aspects of steroid metabolism in the normal and neoplastic mammary gland of the bitch. J. Steroid Biochem. 1980, 13, 1407–1411. [Google Scholar] [CrossRef]
- Sánchez-Archidona, A.R.; Jiménez, M.A.; Pérez-Alenza, D.; Silván, G.; Illera, J.C.; Peña, L.; Dunner, S. Steroid pathway and oestrone sulphate production in canine inflammatory mammary carcinoma. J. Steroid Biochem. Mol. Biol. 2007, 104, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Miller, W.R.; Telford, J.; Dixon, J.M.; Shivas, A.A. Androgen metabolism and apocrine differentiation in human breast cancer. Breast Cancer Res. Treat. 1985, 5, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Vihko, R.; Apter, D.; Bulbrook, R. Endogenous steroids in the pathophysiology of breast cancer. Crit. Rev. Oncol. Hematol. 1989, 9, 1–16. [Google Scholar] [CrossRef]
- Honma, N.; Takubo, K.; Sawabe, M.; Arai, T.; Akiyama, F.; Sakamoto, G.; Utsumi, T.; Yoshimura, N.; Harada, N. Estrogen-Metabolizing Enzymes in Breast Cancers from Women over the Age of 80 Years. J. Clin. Endocrinol. Metab. 2006, 91, 607–613. [Google Scholar] [CrossRef] [PubMed]
- Lykkesfeldt, A.E.; Henriksen, K.L.; Rasmussen, B.B.; Sasano, H.; Evans, D.B.; Møller, S.; Ejlertsen, B.; Mouridsen, H.T. In situaromatase expression in primary tumor is associated with estrogen receptor expression but is not predictive of response to endocrine therapy in advanced breast cancer. BMC Cancer 2009, 9, 185. [Google Scholar] [CrossRef]
- Sasano, H.; Anderson, T.J.; Silverberg, S.G.; Santen, R.J.; Conway, M.; Edwards, D.P.; Krause, A.; Bhatnagar, A.S.; Evans, D.B.; Miller, W.R. The validation of new aromatase monoclonal antibodies for immunohistochemistry—A correlation with biochemical activities in 46 cases of breast cancer. J. Steroid Biochem. Mol. Biol. 2005, 95, 35–39. [Google Scholar] [CrossRef]
- Suzuki, T.; Moriya, T.; Ishida, T.; Ohuchi, N.; Sasano, H. Intracrine mechanism of estrogen synthesis in breast cancer. Biomed. Pharmacother. 2003, 57, 460–462. [Google Scholar] [CrossRef] [PubMed]
- Esteban, J.M.; Warsi, Z.; Haniu, M.; Hall, P.; Shively, J.E.; Chen, S. Detection of intratumoral aromatase in breast carcinomas. An immunohistochemical study with clinicopathologic correlation. Am. J. Pathol. 1992, 140, 337–343. [Google Scholar]
- Shin, J.-I.; Lim, H.-Y.; Kim, H.-W.; Seung, B.-J.; Ju, J.-H.; Sur, J.-H. Analysis of Obesity-Related Factors and their Association with Aromatase Expression in Canine Malignant Mammary Tumours. J. Comp. Pathol. 2016, 155, 15–23. [Google Scholar] [CrossRef]
- Blankenstein, M.A.; van de Ven, J.; Maitimu-Smeele, I.; Donker, G.H.; de Jong, P.C.; Daroszewski, J.; Szymczak, J.; Milewicz, A.; Thijssen, J.H. Intratumoral levels of estrogens in breast cancer. J. Steroid Biochem. Mol. Biol. 1999, 69, 293–297. [Google Scholar] [CrossRef]
- Liao, D.J.; Dickson, R.B. Roles of androgens in the development, growth, and carcinogenesis of the mammary gland. J. Steroid Biochem. Mol. Biol. 2001, 80, 175–189. [Google Scholar] [CrossRef]
- Perel, E.; Davis, S.; Killinger, D.W. Androgen metabolism in male and female breast tissue. Steroids 1981, 37, 345–352. [Google Scholar] [CrossRef]
- Perel, E.; Killinger, D.W. The metabolism of androstenedione and testosterone to C19 metabolites in normal breast, breast carcinoma and benign prostatic hypertrophy tissue. J. Steroid Biochem. 1983, 19, 1135–1139. [Google Scholar] [CrossRef]
- Chetrite, G.S.; Cortes-Prieto, J.; Philippe, J.C.; Wright, F.; Pasqualini, J.R. Comparison of estrogen concentrations, estrone sulfatase and aromatase activities in normal, and in cancerous, human breast tissues. J. Steroid Biochem. Mol. Biol. 2000, 72, 23–27. [Google Scholar] [CrossRef]
- Haynes, B.P.; Straume, A.H.; Geisler, J.; A’Hern, R.; Helle, H.; Smith, I.E.; Lønning, P.E.; Dowsett, M. Intratumoral Estrogen Disposition in Breast Cancer. Clin. Cancer Res. 2010, 16, 1790–1801. [Google Scholar] [CrossRef] [PubMed]
- Lønning, P.E.; Helle, H.; Duong, N.K.; Ekse, D.; Aas, T.; Geisler, J. Tissue estradiol is selectively elevated in receptor positive breast cancers while tumour estrone is reduced independent of receptor status. J. Steroid Biochem. Mol. Biol. 2009, 117, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Queiroga, F.L.; Pérez-Alenza, M.D.; Silvan, G.; Peña, L.; Lopes, C.; Illera, J.C. Role of steroid hormones and prolactin in canine mammary cancer. J. Steroid Biochem. Mol. Biol. 2005, 94, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Perel, E.; Blackstein, M.E.; Killinger, D.W. Aromatase in human breast carcinoma. Cancer Res. 1982, 42, 3369s–3372s. [Google Scholar] [PubMed]
- Sasano, H.; Harada, N. Intratumoral Aromatase in Human Breast, Endometrial, and Ovarian Malignancies. Endocr. Rev. 1998, 19, 593–607. [Google Scholar] [CrossRef][Green Version]
- Yue, W.; Santen, R.J.; Wang, J.P.; Hamilton, C.J.; Demers, L.M. Aromatase within the breast. Endocr. Relat. Cancer 1999, 6, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Hayes, D.F.; Allred, C.; Anderson, B.O. Breast. In American Joint Committee on Cancer (AJCC) Cancer Staging Manual, 7th ed.; Edge, S.B., Byrd, D.R., Compton, C.C., Fritz, A.G., Greene, F.L., Trotti, A., Eds.; Springer: New York, NY, USA, 2010; pp. 347–376. [Google Scholar]
- Lana, S.; Rutteman, G.; Withrow, S. Tumors of the mammary gland. In Withrow and MacEwen’s Small Animal Clinical Oncology, 4th ed.; Withrow, S., Vail, D., Eds.; Saunders Elsevier: St. Louis, MO, USA, 2007; pp. 619–636. [Google Scholar] [CrossRef]
- Hoon Tan, P.H.; Ellis, I.; Allison, K.; Brogi, E.; Fox, S.B.; Lakhani, S.; Lazar, A.J.; Morris, E.A.; Sahin, A.; Salgado, R.; et al. The 2019 World Health Organization classification of tumours of the breast. Histopathology 2020, 77, 181–185. [Google Scholar] [CrossRef]
- Zappulli, V.; Peña, L.; Rasotto, R.; Goldschmidt, M.; Gama, A.; Scruggs, J.; Kiupel, M. Surgical Pathology of Tumors of Domestic Animals—Volume 2: Mammary Tumors; Kiupel, M., Ed.; Davis-Thompson DVM Foundation: Gurnee, IL, USA, 2019; Volume 2. [Google Scholar]
- Elston, C.W.; Ellis, I.O. pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: Experience from a large study with long-term follow-up. Histopathology 1991, 19, 403–410. [Google Scholar] [CrossRef]
- Peña, L.; De Andrés, P.J.; Clemente, M.; Cuesta, P.; Pérez-Alenza, M.D. Prognostic value of histological grading in noninflammatory canine mammary carcinomas in a prospective study with two-year follow-up: Relationship with clinical and histological characteristics. Vet. Pathol. 2012, 50, 94–105. [Google Scholar] [CrossRef] [PubMed]
- Allred, D.C.; Harvey, J.M.; Berardo, M.; Clark, G.M. Prognostic and predictive factors in breast cancer by immunohistochemical analysis. Mod. Pathol. 1998, 11, 155–168. [Google Scholar]
- Uva, P.; Aurisicchio, L.; Watters, J.; Loboda, A.; Kulkarni, A.; Castle, J.; Palombo, F.; Viti, V.; Mesiti, G.; Zappulli, V.; et al. Comparative expression pathway analysis of human and canine mammary tumors. BMC Genom. 2009, 10, 135. [Google Scholar] [CrossRef]
- Rasotto, R.; Goldschmidt, M.H.; Castagnaro, M.; Carnier, P.; Caliari, D.; Zappulli, V. The Dog as a Natural Animal Model for Study of the Mammary Myoepithelial Basal Cell Lineage and its Role in Mammary Carcinogenesis. J. Comp. Pathol. 2014, 151, 166–180. [Google Scholar] [CrossRef] [PubMed]
- Ghoncheh, M.; Pournamdar, Z.; Salehiniya, H. Incidence and Mortality and Epidemiology of Breast Cancer in the World. Asian Pac. J. Cancer Prev. 2016, 17, 43–46. [Google Scholar] [CrossRef] [PubMed]
- Vascellari, M.; Capello, K.; Carminato, A.; Zanardello, C.; Baioni, E.; Mutinelli, F. Incidence of mammary tumors in the canine population living in the Veneto region (Northeastern Italy): Risk factors and similarities to human breast cancer. Prev. Vet. Med. 2016, 126, 183–189. [Google Scholar] [CrossRef] [PubMed]
- Selim, A.-G.A.; El-Ayat, G.; A Wells, C. Androgen receptor expression in ductal carcinoma in situ of the breast: Relation to oestrogen and progesterone receptors. J. Clin. Pathol. 2002, 55, 14–16. [Google Scholar] [CrossRef] [PubMed]
- Moinfar, F.; Okcu, M.; Tsybrovskyy, O.; Regitnig, P.; Lax, S.F.; Weybora, W.; Ratschek, M.; Tavassoli, F.A.; Denk, H. Androgen receptors frequently are expressed in breast carcinomas: Potential relevance to new therapeutic strategies. Cancer 2003, 98, 703–711. [Google Scholar] [CrossRef] [PubMed]
- Conde, I.; Alfaro, J.M.; Fraile, B.; Ruíz, A.; Paniagua, R.; Arenas, M.I. DAX-1 expression in human breast cancer: Comparison with estrogen receptors ER-α, ER-β and androgen receptor status. Breast Cancer Res. 2004, 6, R140–R148. [Google Scholar] [CrossRef] [PubMed]
- DeVita, V.T.; Lawrence, T.S.; Rosenberg, S.A. DeVita, Hellman, and Rosenberg’s Cancer: Principles & Practice of Oncology, 8th ed.; Wolters Kluwer/Lippincott Williams & Wilkins: Philadelphia, PA, USA; London, UK, 2008; pp. 2911–3008. [Google Scholar]
- Gago, F.E.; Fanelli, M.A.; Ciocca, D.R. Co-expression of steroid hormone receptors (estrogen receptor α and/or progesterone receptors) and Her2/neu (c-erbB-2) in breast cancer: Clinical outcome following tamoxifen-based adjuvant therapy. J. Steroid Biochem. Mol. Biol. 2006, 98, 36–40. [Google Scholar] [CrossRef] [PubMed]
- Sarvilinna, N.; Eronen, H.; Miettinen, S.; Vienonen, A.; Ylikomi, T. Steroid hormone receptors and coregulators in endocrine-resistant and estrogen-independent breast cancer cells. Int. J. Cancer 2005, 118, 832–840. [Google Scholar] [CrossRef] [PubMed]
- Foster, P.A. Steroid metabolism in breast cancer. Minerva Endocrinol. 2008, 33, 27–37. [Google Scholar]
- Hong, Y.; Li, H.; Ye, J.; Miki, Y.; Yuan, Y.-C.; Sasano, H.; Evans, D.B.; Chen, S. Epitope Characterization of an Aromatase Monoclonal Antibody Suitable for the Assessment of Intratumoral Aromatase Activity. PLoS ONE 2009, 4, e8050. [Google Scholar] [CrossRef] [PubMed]
- Sasano, H.; Nagura, H.; Harada, N.; Goukon, Y.; Kimura, M. Immunolocalization of aromatase and other steroidogenic enzymes in human breast disorders. Hum. Pathol. 1994, 25, 530–535. [Google Scholar] [CrossRef]
- Shenton, K.C.; Dowsett, M.; Lu, Q.; Brodie, A.; Sasano, H.; Sacks, N.P.; Rowlands, M.G. Comparison of biochemical aromatase activity with aromatase immunohistochemistry in human breast carcinomas. Breast Cancer Res. Treat. 1998, 49 (Suppl. 1), S101–S107, discussion S109–S119. [Google Scholar] [CrossRef] [PubMed]
- Sasano, H.; Suzuki, T.; Miki, Y.; Moriya, T. Intracrinology of estrogens and androgens in breast carcinoma. J. Steroid Biochem. Mol. Biol. 2008, 108, 181–185. [Google Scholar] [CrossRef] [PubMed]
- Miller, W.R.; Anderson, T.J.; Jack, W.J. Relationship between tumour aromatase activity, tumour characteristics and response to therapy. J. Steroid Biochem. Mol. Biol. 1990, 37, 1055–1059. [Google Scholar] [CrossRef]
- Mol, J.A.; Selman, P.J.; Sprang, E.P.; van Neck, J.W.; Oosterlaken-Dijksterhuis, M.A. The role of progestins, insulin-like growth factor (IGF) and IGF-binding proteins in the normal and neoplastic mammary gland of the bitch: A review. J. Reprod. Fertil. Suppl. 1997, 51, 339–344. [Google Scholar] [PubMed]
- Lantinga-van Leeuwen, I.S.; van Garderen, E.; Rutteman, G.R.; Mol, J.A. Cloning and cellular localization of the canine progesterone receptor: Co-localization with growth hormone in the mammary gland. J. Steroid Biochem. Mol. Biol. 2000, 75, 219–228. [Google Scholar] [CrossRef]
- Guil-Luna, S.; Sánchez-Céspedes, R.; Millán, Y.; De Andrés, F.J.; Rollón, E.; Domingo, V.; Guscetti, F.; Martin de Las Mulas, J. Aglepristone Decreases Proliferation in Progesterone Receptor-Positive Canine Mammary Carcinomas. J. Vet. Intern. Med. 2011, 25, 518–523. [Google Scholar] [CrossRef] [PubMed]
| Women (n = 51) | Dogs (n = 27) | ||
|---|---|---|---|
| Age at diagnosis (y) | Age at diagnosis (y) | ||
| Range | 33–89 | Range | 6–14 |
| Mean | 63.3 | Mean | 10.2 |
| Menopausal status | Ovariectomy status | ||
| Premenopausal | 13 (25.5%) | Intact (anestrus) | 26 (96.3%) |
| Menopausal | 38 (74.5%) | Spayed | 1 (3.7%) |
| Tumor size * | Tumor size * | ||
| T0 | 0 | T1 | 11 (40.7%) |
| T1 | 32 (62.7%) | T2 | 5 (18.6%) |
| T2 | 16 (31.4%) | T3 | 11 (40.7%) |
| T3 | 3 (5.9%) | ||
| T4 | 0 | ||
| Lymphatic invasion ** | Lymphatic invasion ** | ||
| N0 | 30 (58.8%) | N0 | 20 (70.1%) |
| N1 | 16 (31.4%) | N1 | 7 (25.9%) |
| N2 | 5 (7.8%) | ||
| Distant metastases † | Distant metastases † | ||
| M0 | 49 (96%) | M0 | 22 (81.5%) |
| M1 | 2 (4%) | M1 | 5 (18.5%) |
| Clinical stage ‡ | Clinical stage ‡ | ||
| 0 | 0 | I | 11 (40.8%) |
| IA | 21 (41.2%) | II | 5 (18.5%) |
| IB | 0 | III | 4 (14.8%) |
| IIA | 13 (25.4%) | IV | 2 (7.4%) |
| IIB | 11 (21.6%) | V | 5 (18.5%) |
| IIIA | 4 (7.8%) | ||
| IIIB | 0 | ||
| IIIC | 0 | ||
| IV | 2 (4%) |
| HBC (n = 51) | CMC (n = 27) | ||
|---|---|---|---|
| Histological subtypes | Histological subtypes | ||
| Invasive ductal carcinoma | 38 (74.6%) | Tubular carcinoma | 7 (25.8%) |
| Mucinous carcinoma | 5 (9.8%) | Tubulopapillary carcinoma | 5 (18.6%) |
| Invasive lobular carcinoma | 4 (7.8%) | Solid carcinoma | 5 (18.6%) |
| Invasive papillary carcinoma | 2 (3.9%) | Complex carcinoma | 3 (11.1%) |
| Tubular carcinoma | 2 (3.9%) | Mixed-type carcinoma | 3 (11.1%) |
| Adenosquamous carcinoma | 2 (7.4%) | ||
| Lipid-rich carcinoma | 1 (3.7%) | ||
| Anaplastic carcinoma | 1 (3.7%) | ||
| HMG | HMG | ||
| 1 | 14 (27.4%) | 1 | 13 (48.2%) |
| 2 | 24 (47.1%) | 2 | 7 (25.9%) |
| 3 | 13 (25.5%) | 3 | 7 (25.9%) |
| PM-HBC ‡ (a) | a vs. c * | M-HBC ‡ (b) | b vs. c * | CMC ‡ (c) | ||
|---|---|---|---|---|---|---|
| Arom (−/+) a | Negative | 4/13 (30.8%) | p = 0.941 | 5/38 (13.2%) | p = 0.102 | 8/27 (29.6%) |
| Positive | 9/13 (69.2%) | 33/38 (86.8%) | 19/27 (70.4%) | |||
| Arom b | TS | 4.77 ± 0.76 | p = 0.696 | 5.45 ± 0.37 | p = 0.133 | 4.37 ± 0.6 |
| ERα (−/+) a | Negative | 4/13 (30.8%) | p = 0.209 | 6/38 (15.8%) | p = 0.002 | 14/27 (51.9%) |
| Positive | 9/13 (69.2%) | 32/38 (84.2%) | 13/27 (48.1%) | |||
| ERα b | TS | 4.33 ± 0.96 | p = 0.070 | 6.16 ± 0.47 | p < 0.001 | 2.44 ± 0.53 |
| ERβ (−/+) a | Negative | 0/13 (0.0%) | p = 0.144 | 2/38 (5.3%) | p = 0.190 | 4/27 (14.8%) |
| Positive | 13/13 (100%) | 36/38 (94.7%) | 23/27 (85.2%) | |||
| ERβ b | TS | 6.85 ± 0.32 | p = 0.003 | 5.42 ± 0.31 | p = 0.484 | 5.04 ± 0.48 |
| PR (−/+) a | Negative | 2/13 (15.4%) | p = 0.962 | 4/38 (10.5%) | p = 0.604 | 4/27 (14.8%) |
| Positive | 11/13 (84.6%) | 34/38 (89.5%) | 23/27 (85.2%) | |||
| PR b | TS | 5.83 ± 0.89 | p = 0.225 | 6.63 ± 0.42 | p = 0.003 | 4.74 ± 0.44 |
| AR (−/+) a | Negative | 0/13 (0.0%) | p = 0.314 | 0/38 (0.0%) | p = 0.088 | 2/27 (7.4%) |
| Positive | 13/13 (100%) | 38/38 (100%) | 25/27 (92.6%) | |||
| AR b | TS | 6.92 ± 0.35 | p = 0.001 | 6.54 ± 0.22 | p < 0.001 | 0.37 |
| Premenopausal Women | p Value * | ||
|---|---|---|---|
| Normal Breast (n = 6) | PM-HBC (n = 13) | ||
| E2 (pg/g) | 237.56 ± 118.34 | 758.81 ± 136.38 | 0.029 |
| SO4E1 (ng/g) | 233.65 ± 41.31 | 1229.18 ± 153.96 | <0.001 |
| P4 (ng/g) | 7.14 ± 0.57 | 66.04 ± 4.05 | <0.001 |
| A4 (ng/g) | 19.19 ± 2.61 | 226.76 ± 12.57 | <0.001 |
| DHEA (ng/g) | 161.46 ± 19.96 | 321.47 ± 50.51 | 0.052 |
| T (ng/g) | 9.77 ± 1.39 | 26.24 ± 2.74 | 0.001 |
| Menopausal Women | |||
| Normal Breast (n = 4) | M-HBC (n = 38) | p Value * | |
| E2 (pg/g) | 73.86 ± 15.85 | 683.93 ± 88.23 | 0.032 |
| SO4E1 (ng/g) | 226.30 ± 25.84 | 1283.13 ± 140.97 | 0.021 |
| P4 (ng/g) | 12.91 ± 3.55 | 71.45 ± 2.56 | <0.001 |
| A4 (ng/g) | 13.66 ± 1.68 | 213.79 ± 9.45 | <0.001 |
| DHEA (ng/g) | 170.07 ± 5.59 | 328.55 ± 16.39 | <0.001 |
| T (ng/g) | 8.46 ± 0.79 | 27.79 ± 1.43 | <0.001 |
| Female Dogs | |||
| Normal Mammary Gland (n = 8) | CMC (n = 30) | p Value * | |
| E2 (pg/g) | 89.74 ± 3.82 | 290.54 ± 31.8 | <0.001 |
| SO4E1 (ng/g) | 76.51 ± 5.89 | 693.44 ± 85.93 | <0.001 |
| P4 (ng/g) | 2.22 ± 0.12 | 8.69 ± 1.12 | <0.001 |
| A4 (ng/g) | 11.13 ± 2.40 | 102.55 ± 10.69 | <0.001 |
| DHEA (ng/g) | 28.24 ± 6.21 | 251.44 ± 13.80 | <0.001 |
| T (ng/g) | 0.43 ± 0.07 | 20.15 ± 2.97 | <0.001 |
| PM-HBC vs. CMC * | M-HBC vs. CMC * | |
|---|---|---|
| Immunohistochemistrya | ||
| Aromatase + | ++ | + |
| ERα + | + | − |
| ERβ + | + | + |
| PR + | ++ | ++ |
| AR + | ++ | ++ |
| Tumor steroid hormones content vs. controls b | ||
| Levels of estrogens (E2, SO4) and P4 | † | † |
| Levels of androgens (A4, DHEA and T) | ‡ | ‡ |
| Hormonal associations | ||
| Positive correlation between androgens | + | − |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Andrés, P.J.; Cáceres, S.; Illera, J.C.; Crespo, B.; Silván, G.; Queiroga, F.L.; Illera, M.J.; Pérez-Alenza, M.D.; Peña, L. Hormonal Homologies between Canine Mammary Cancer and Human Breast Cancer in a Series of Cases. Vet. Sci. 2022, 9, 395. https://doi.org/10.3390/vetsci9080395
de Andrés PJ, Cáceres S, Illera JC, Crespo B, Silván G, Queiroga FL, Illera MJ, Pérez-Alenza MD, Peña L. Hormonal Homologies between Canine Mammary Cancer and Human Breast Cancer in a Series of Cases. Veterinary Sciences. 2022; 9(8):395. https://doi.org/10.3390/vetsci9080395
Chicago/Turabian Stylede Andrés, Paloma Jimena, Sara Cáceres, Juan Carlos Illera, Belén Crespo, Gema Silván, Felisbina Luisa Queiroga, Maria José Illera, Maria Dolores Pérez-Alenza, and Laura Peña. 2022. "Hormonal Homologies between Canine Mammary Cancer and Human Breast Cancer in a Series of Cases" Veterinary Sciences 9, no. 8: 395. https://doi.org/10.3390/vetsci9080395
APA Stylede Andrés, P. J., Cáceres, S., Illera, J. C., Crespo, B., Silván, G., Queiroga, F. L., Illera, M. J., Pérez-Alenza, M. D., & Peña, L. (2022). Hormonal Homologies between Canine Mammary Cancer and Human Breast Cancer in a Series of Cases. Veterinary Sciences, 9(8), 395. https://doi.org/10.3390/vetsci9080395







