Effects of Chronic Mild Stress on Cardiac Autonomic Activity, Cardiac Structure and Renin–Angiotensin–Aldosterone System in Male Rats
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
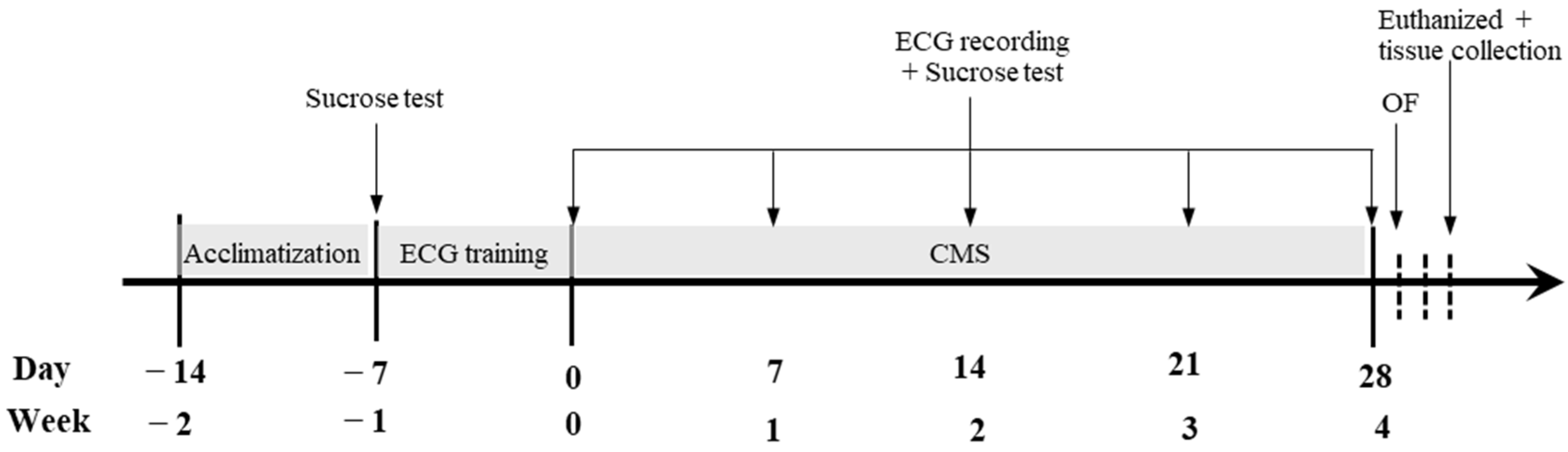
2.2. Experimental Procedures
2.3. Chronic Mild Stress Procedure
2.4. ECG Recording and HRV Measurement
2.5. Sucrose Intake Test
2.6. Open-Field Test
2.7. Histomorphometric Analysis
2.8. Left-Ventricular ANP, BNP, AT1R, AT2R, ACE and ACE2 mRNA Expressions
2.9. Plasma B-Type Natriuretic Peptide (BNP) and Serum Ang II Concentration Measurements
2.10. Statistical Analysis
3. Results
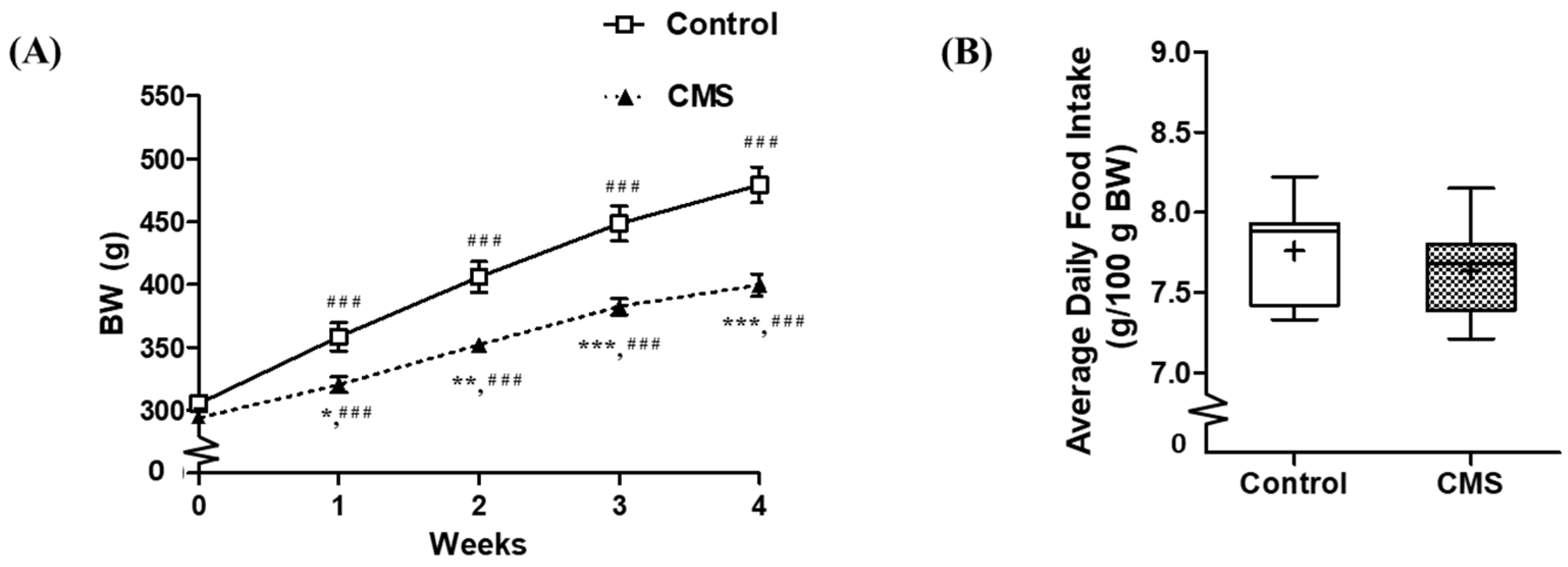
3.1. Effects of CMS on Body Weight, Food Intake and Organ Weights
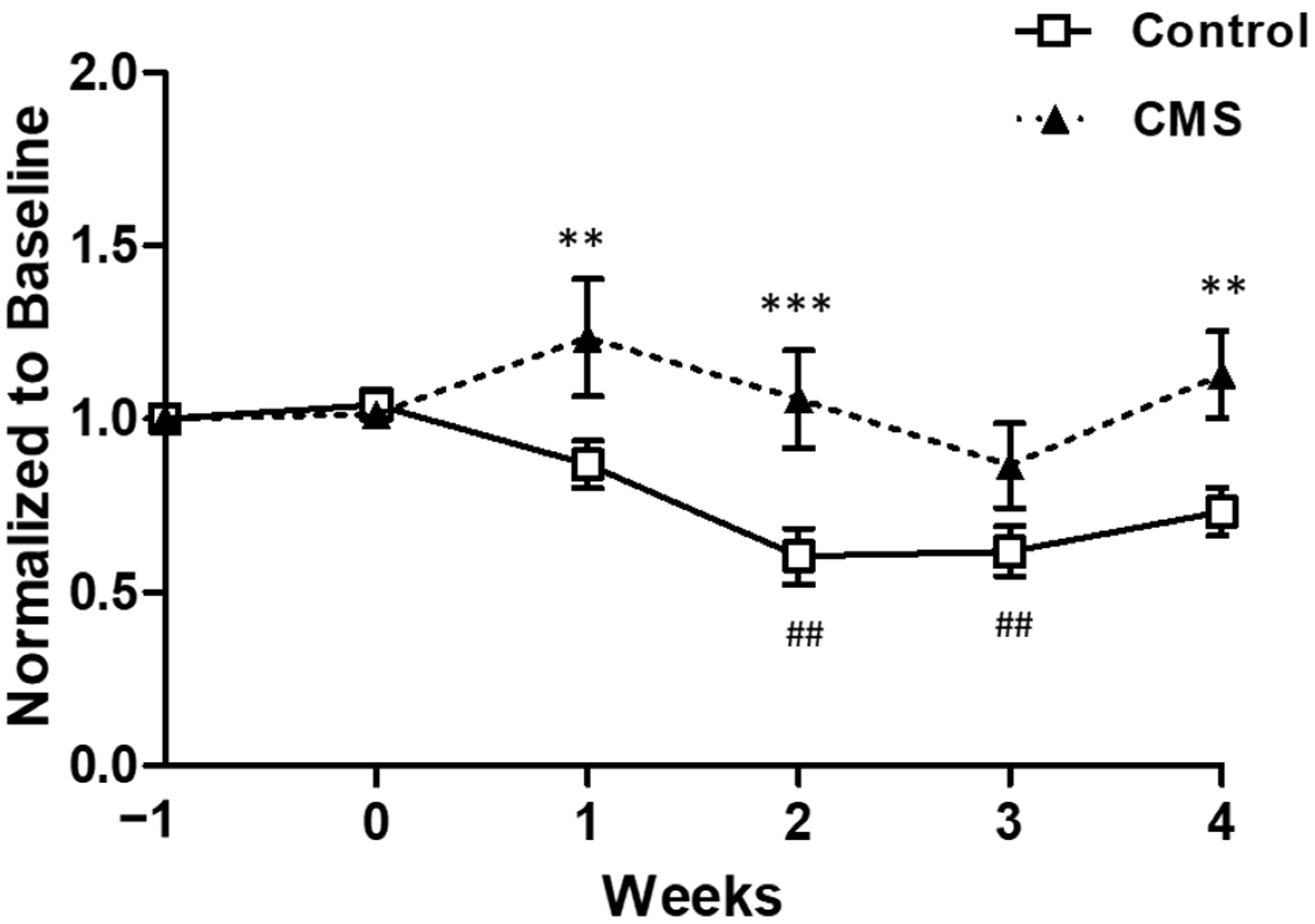
3.2. Effects of CMS on Emotional State
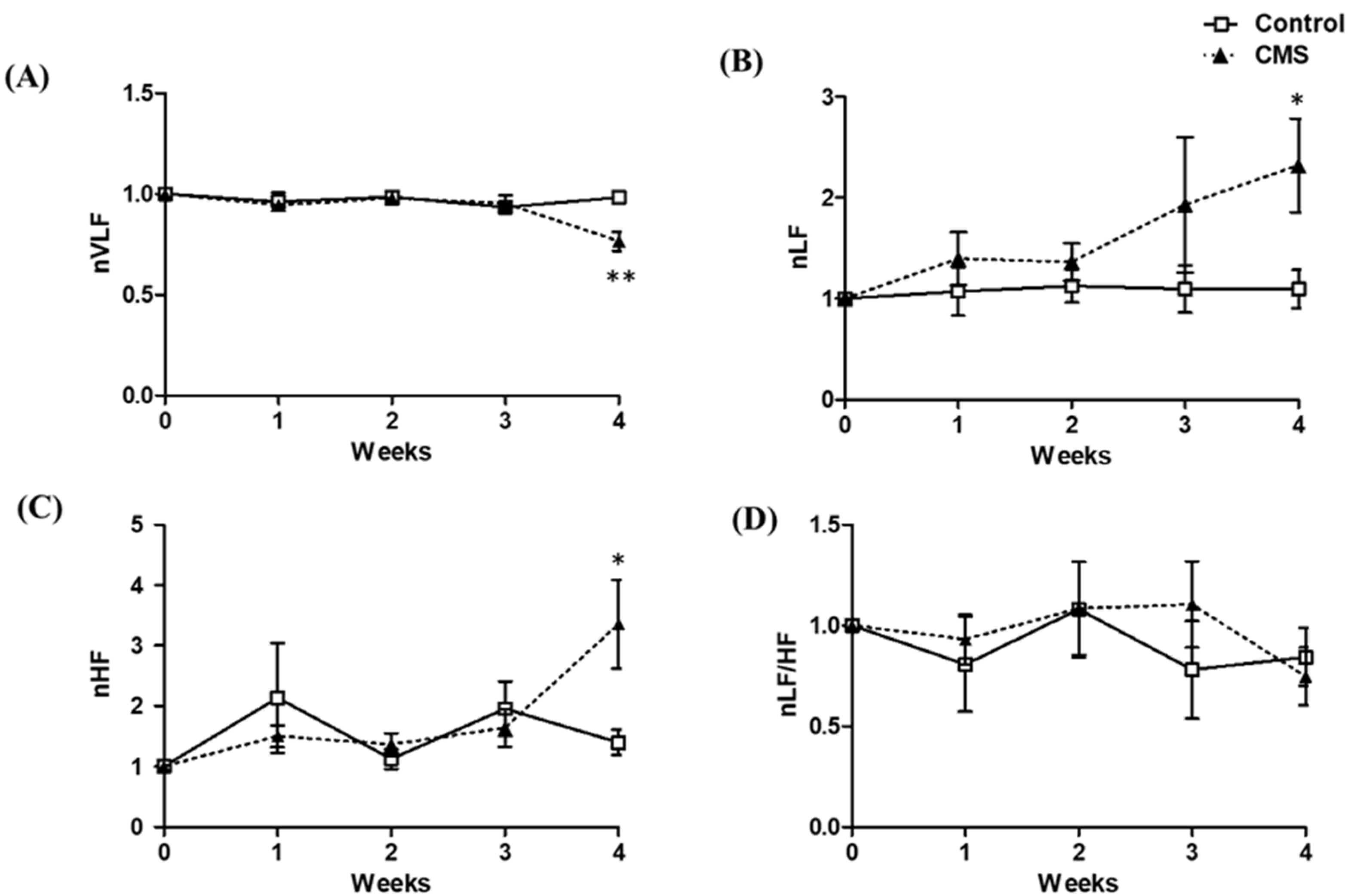
3.3. Effects of CMS on Cardiac Autonomic Activity
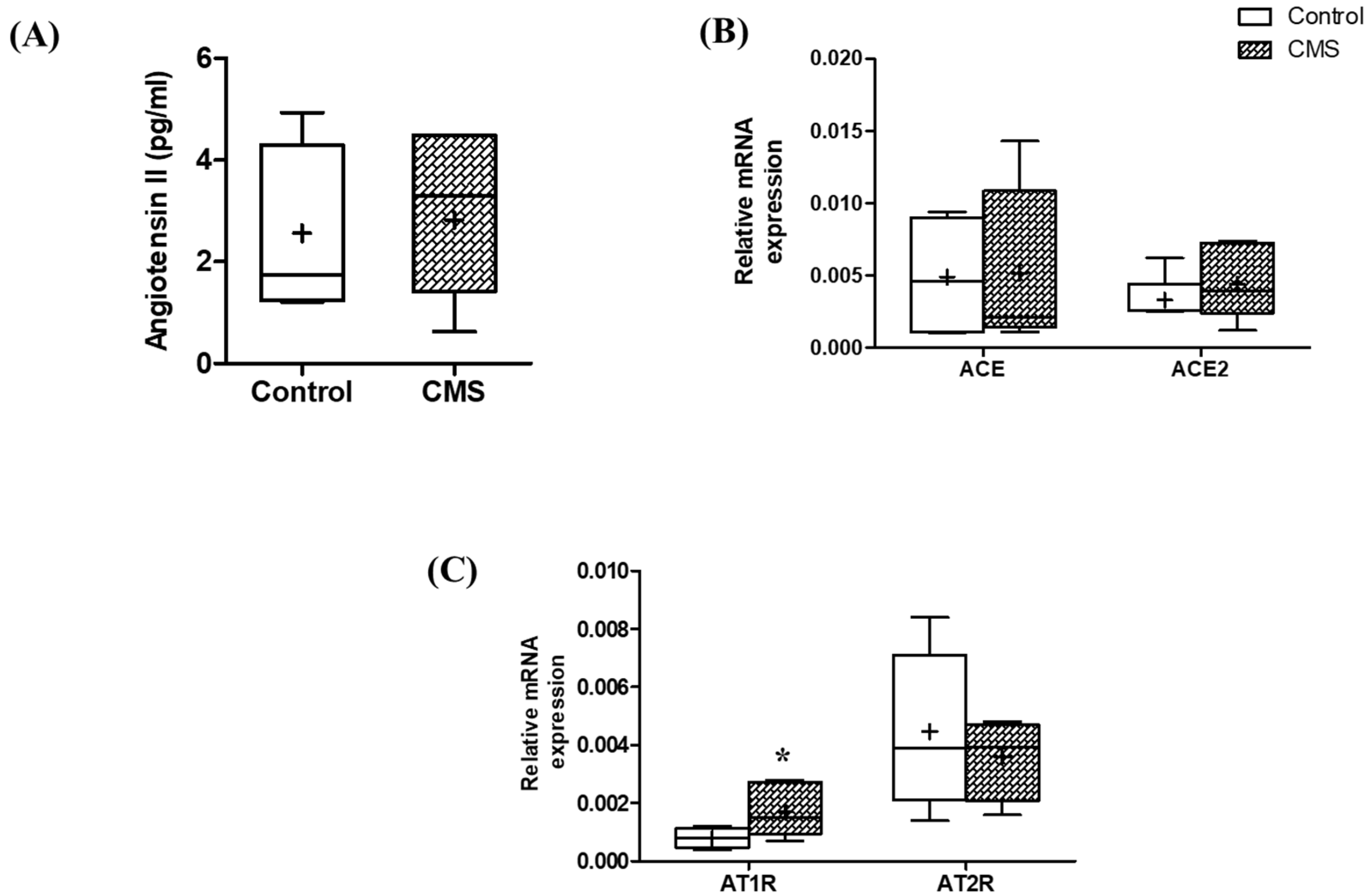
3.4. Effects of CMS on Cardiac- and RAAS-Related Parameters
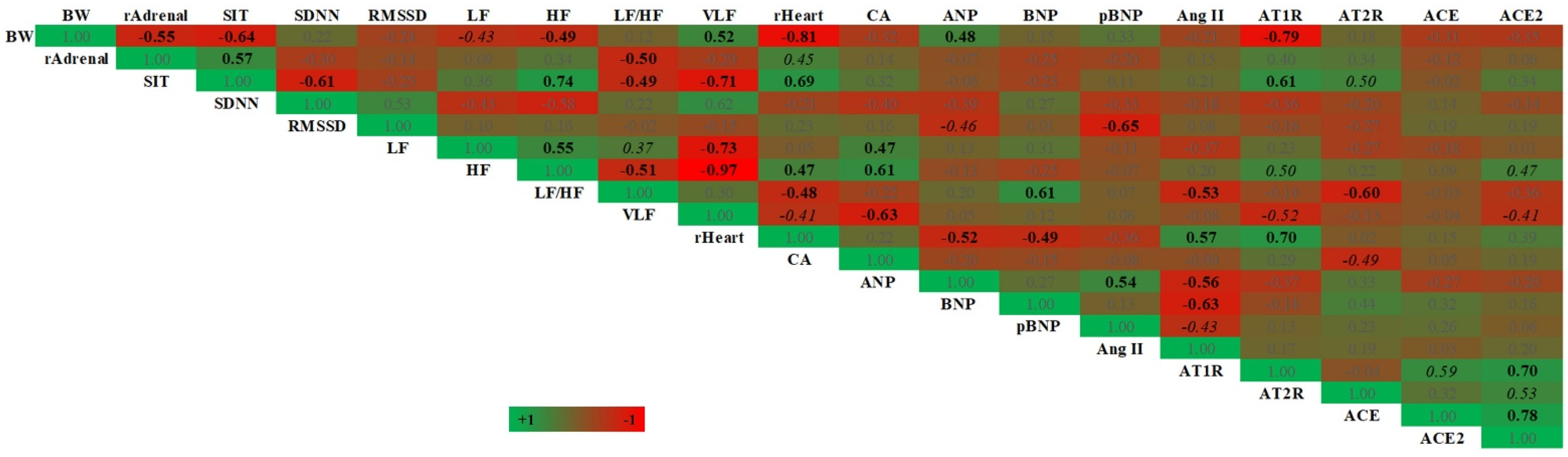
3.5. The Correlation between Stress-, HRV-, Cardiac- and RAAS-Related Parameters
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Steptoe, A.; Kivimäki, M. Stress and cardiovascular disease. Nat. Rev. Cardiol. 2012, 9, 360–370. [Google Scholar] [CrossRef]
- WHO. The Top 10 Causes of Death; World Health Organization: Geneva, Switzerland, 2020.
- Mucci, N.; Giorgi, G.; De Pasquale Ceratti, S.; Fiz-Pérez, J.; Mucci, F.; Arcangeli, G. Anxiety, stress-related factors, and blood pressure in young adults. Front. Psychol. 2016, 7, 1682. [Google Scholar] [CrossRef]
- Sara, J.D.; Prasad, M.; Eleid, M.F.; Zhang, M.; Widmer, R.J.; Lerman, A. Association between work-related stress and coronary heart disease: A review of prospective studies through the job strain, effort-reward balance, and organizational justice models. J. Am. Heart Assoc. 2018, 7, e008073. [Google Scholar] [CrossRef]
- Buckley, U.; Shivkumar, K. Stress-induced cardiac arrhythmias: The heart-brain interaction. Trends Cardiovasc. Med. 2016, 26, 78–80. [Google Scholar] [CrossRef]
- Liu, M.C.; Tester, M.A.; Franciosi, S.; Krahn, A.D.; Gardner, M.J.; Roberts, J.D.; Sanatani, S. Potential role of life stress in unexplained sudden cardiac arrest. CJC Open 2021, 3, 285–291. [Google Scholar] [CrossRef]
- Renzaho, A.M.; Houng, B.; Oldroyd, J.; Nicholson, J.M.; D’Esposito, F.; Oldenburg, B. Stressful life events and the onset of chronic diseases among Australian adults: Findings from a longitudinal survey. Eur. J. Public Health 2014, 24, 57–62. [Google Scholar] [CrossRef]
- Liu, W.; Wang, X.; Mei, Z.; Gong, J.; Gao, X.; Zhao, Y.; Ma, J.; Xie, F.; Qian, L. Chronic stress promotes the progression of pressure overload-induced cardiac dysfunction through inducing more apoptosis and fibrosis. Physiol. Res. 2015, 64, 325–334. [Google Scholar] [CrossRef]
- Costoli, T.; Bartolomucci, A.; Graiani, G.; Stilli, D.; Laviola, G.; Sgoifo, A. Effects of chronic psychosocial stress on cardiac autonomic responsiveness and myocardial structure in mice. Am. J. Physiol. Heart Circ. Physiol. 2004, 286, H2133–H2140. [Google Scholar] [CrossRef]
- Floras, J.S.; Ponikowski, P. The sympathetic/parasympathetic imbalance in heart failure with reduced ejection fraction. Eur. Heart J. 2015, 36, 1974–1982. [Google Scholar] [CrossRef]
- Thayer, J.F.; Yamamoto, S.S.; Brosschot, J.F. The relationship of autonomic imbalance, heart rate variability and cardiovascular disease risk factors. Int. J. Cardiol. 2010, 141, 122–131. [Google Scholar] [CrossRef]
- Carnevali, L.; Trombini, M.; Graiani, G.; Madeddu, D.; Quaini, F.; Landgraf, R.; Neumann, I.D.; Nalivaiko, E.; Sgoifo, A. Low vagally-mediated heart rate variability and increased susceptibility to ventricular arrhythmias in rats bred for high anxiety. Physiol. Behav. 2014, 128, 16–25. [Google Scholar] [CrossRef]
- Morais-Silva, G.; Costa-Ferreira, W.; Gomes-de-Souza, L.; Pavan, J.C.; Crestani, C.C.; Marin, M.T. Cardiovascular outcomes related to social defeat stress: New insights from resilient and susceptible rats. Neurobiol. Stress 2019, 11, 100181. [Google Scholar] [CrossRef]
- Grippo, A.J.; Beltz, T.G.; Johnson, A.K. Behavioral and cardiovascular changes in the chronic mild stress model of depression. Physiol. Behav. 2003, 78, 703–710. [Google Scholar] [CrossRef]
- Grippo, A.J.; Santos, C.M.; Johnson, R.F.; Beltz, T.G.; Martins, J.B.; Felder, R.B.; Johnson, A.K. Increased susceptibility to ventricular arrhythmias in a rodent model of experimental depression. Am. J. Physiol. Heart Circ. Physiol. 2004, 286, H619–H626. [Google Scholar] [CrossRef]
- Park, S.E.; Park, D.; Song, K.I.; Seong, J.K.; Chung, S.; Youn, I. Differential heart rate variability and physiological responses associated with accumulated short- and long-term stress in rodents. Physiol. Behav. 2017, 171, 21–31. [Google Scholar] [CrossRef]
- Park, D.; Lee, M.; Park, S.E.; Seong, J.K.; Youn, I. Determination of optimal heart rate variability features based on SVM-recursive feature elimination for cumulative stress monitoring using ECG Sensor. Sensors 2018, 18, 2387. [Google Scholar] [CrossRef]
- Willner, P. Chronic mild stress (CMS) revisited: Consistency and behavioural-neurobiological concordance in the effects of CMS. Neuropsychobiology 2005, 52, 90–110. [Google Scholar] [CrossRef]
- Willner, P. The chronic mild stress (CMS) model of depression: History, evaluation and usage. Neurobiol. Stress 2017, 6, 78–93. [Google Scholar] [CrossRef]
- Nakamura, M.; Sadoshima, J. Mechanisms of physiological and pathological cardiac hypertrophy. Nat. Rev. Cardiol. 2018, 15, 387–407. [Google Scholar] [CrossRef]
- Dorn, G.W.; Force, T. Protein kinase cascades in the regulation of cardiac hypertrophy. J. Clin. Investig. 2005, 115, 527–537. [Google Scholar] [CrossRef]
- Schlaich, M.P.; Kaye, D.M.; Lambert, E.; Sommerville, M.; Socratous, F.; Esler, M.D. Relation between cardiac sympathetic activity and hypertensive left ventricular hypertrophy. Circulation 2003, 108, 560–565. [Google Scholar] [CrossRef] [PubMed]
- Touyz, R.; Berry, C. Recent advances in angiotensin II signaling. Braz. J. Med. Biol. Res. 2002, 35, 1001–1015. [Google Scholar] [CrossRef] [PubMed]
- Raizada, M.K.; Ferreira, A.J. ACE2: A new target for cardiovascular disease therapeutics. J. Cardiovasc. Pharmacol. 2007, 50, 112–119. [Google Scholar] [CrossRef]
- Bernardi, S.; Michelli, A.; Zuolo, G.; Candido, R.; Fabris, B. Update on RAAS modulation for the treatment of diabetic cardiovascular disease. J. Diabetes Res. 2016, 2016, 8917578. [Google Scholar] [CrossRef]
- Akselrod, S.; Gordon, D.; Ubel, F.A.; Shannon, D.C.; Berger, A.C.; Cohen, R.J. Power spectrum analysis of heart rate fluctuation: A quantitative probe of beat-to-beat cardiovascular control. Science 1981, 213, 220–222. [Google Scholar] [CrossRef] [PubMed]
- Nishikimi, T.; Maeda, N.; Matsuoka, H. The role of natriuretic peptides in cardioprotection. Cardiovasc. Res. 2006, 69, 318–328. [Google Scholar] [CrossRef]
- Sergeeva, I.A.; Christoffels, V.M. Regulation of expression of atrial and brain natriuretic peptide, biomarkers for heart development and disease. Biochim. Biophys. Acta (BBA)—Mol. Basis Dis. 2013, 1832, 2403–2413. [Google Scholar] [CrossRef]
- Ueyama, T. Emotional stress-induced Tako-tsubo cardiomyopathy: Animal model and molecular mechanism. Ann. N. Y. Acad. Sci. 2004, 1018, 437–444. [Google Scholar] [CrossRef]
- Slavikova, J.; Mistrova, E.; Klenerova, V.; Kruzliak, P.; Caprnda, M.; Hynie, S.; Sida, P.; Dvorakova, M.C. Effects of immobilizations stress with or without water immersion on the expression of atrial natriuretic peptide in the hearts of two rat strains. Am. J. Transl. Res. 2016, 8, 3148–3158. [Google Scholar]
- Wann, B.P.; Audet, M.-C.; Anisman, H. Impact of acute and chronic stressor experiences on heart atrial and brain natriuretic peptides in response to a subsequent stressor. Horm. Behav. 2010, 58, 907–916. [Google Scholar] [CrossRef]
- Boggiano, M.; Cavigelli, S.A.; Dorsey, J.; Kelley, C.; Ragan, C.; Chandler-Laney, P. Effect of a cage divider permitting social stimuli on stress and food intake in rats. Physiol. Behav. 2008, 95, 222–228. [Google Scholar] [CrossRef] [PubMed]
- Grønli, J.; Murison, R.; Bjorvatn, B.; Sørensen, E.; Portas, C.M.; Ursin, R. Chronic mild stress affects sucrose intake and sleep in rats. Behav. Brain Res. 2004, 150, 139–147. [Google Scholar] [CrossRef]
- Pereira-Junior, P.P.; Marocolo, M.; Rodrigues, F.P.; Medei, E.; Nascimento, J.H. Noninvasive method for electrocardiogram recording in conscious rats: Feasibility for heart rate variability analysis. An. Acad. Bras. Cienc. 2010, 82, 431–437. [Google Scholar] [CrossRef] [PubMed]
- Rowan, W.H.; Campen, M.J.; Wichers, L.B.; Watkinson, W.P. Heart rate variability in rodents: Uses and caveats in toxicological studies. Cardiovasc. Toxicol. 2007, 7, 28–51. [Google Scholar] [CrossRef]
- Silva, L.E.V.; Geraldini, V.R.; De Oliveira, B.P.; Silva, C.A.A.; Porta, A.; Fazan, R. Comparison between spectral analysis and symbolic dynamics for heart rate variability analysis in the rat. Sci. Rep. 2017, 7, 8428. [Google Scholar] [CrossRef]
- Freitas, S.C.F.; Dos Santos, C.P.; Arnold, A.; Stoyell-Conti, F.F.; Dutra, M.R.H.; Veras, M.; Irigoyen, M.C.; De Angelis, K. A method to assess heart rate variability in neonate rats: Validation in normotensive and hypertensive animals. Braz. J. Med. Biol. Res. 2020, 53, e9493. [Google Scholar] [CrossRef]
- Trombini, M.; Hulshof, H.; Graiani, G.; Carnevali, L.; Meerlo, P.; Quaini, F.; Sgoifo, A. Early maternal separation has mild effects on cardiac autonomic balance and heart structure in adult male rats. Stress 2012, 15, 457–470. [Google Scholar] [CrossRef]
- Aubert, A.E.; Ramaekers, D.; Beckers, F.; Breem, R.; Denef, C.; Van de Werf, F.; Ector, H. The analysis of heart rate variability in unrestrained rats. Validation of method and results. Comput. Methods Programs Biomed. 1999, 60, 197–213. [Google Scholar] [CrossRef]
- McCarthy, M.M.; Felzenberg, E.; Robbins, A.; Pfaff, D.W.; Schwartz-Giblin, S. Infusions of diazepam and allopregnanolone into the midbrain central gray facilitate open-field behavior and sexual receptivity in female rats. Horm. Behav. 1995, 29, 279–295. [Google Scholar] [CrossRef]
- Smolinsky, A.N.; Bergner, C.L.; LaPorte, J.L.; Kalueff, A.V. Analysis of grooming behavior and its utility in studying animal stress, anxiety, and depression. In Mood and Anxiety Related Phenotypes in Mice; Springer: New York, NY, USA, 2009; pp. 21–36. [Google Scholar]
- Schmittgen, T.D.; Livak, K.J. Analyzing real-time PCR data by the comparative CT method. Nat. Protoc. 2008, 3, 1101–1108. [Google Scholar] [CrossRef]
- Gutte, H.; Oxbøl, J.; Kristoffersen, U.S.; Mortensen, J.; Kjær, A. Gene expression of ANP, BNP and ET-1 in the heart of rats during pulmonary embolism. PLoS ONE 2010, 5, e11111. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sabatino, L.; Costagli, C.; Lapi, D.; Del Seppia, C.; Federighi, G.; Balzan, S.; Colantuoni, A.; Iervasi, G.; Scuri, R. Renin-angiotensin system responds to prolonged hypotensive effect induced by mandibular extension in spontaneously hypertensive rats. Front. Physiol. 2018, 9, 1613. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Lee, Y.H.; Jung, S.W.; Kim, D.J.; Park, S.H.; Song, S.J.; Jeong, K.H.; Moon, J.Y.; Ihm, C.G.; Lee, T.W.; et al. Sex-related differences in the intratubular renin-angiotensin system in two-kidney, one-clip hypertensive rats. Am. J. Physiol. Renal Physiol. 2019, 317, F670–F682. [Google Scholar] [CrossRef] [PubMed]
- Kamilic, J.; Hamming, I.; Kreutz, R.; Bolbrinker, J.; Siems, W.-E.; Nassar, I.; Sluimer, J.C.; Walther, T.; Navis, G.J.; van Goor, H. Renal ACE2 expression and activity is unaltered during established hypertension in adult SHRSP and TGR (mREN2) 27. Hypertens. Res. 2010, 33, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Chen, X.; Liu, B.; Han, J. MicroRNA-124-3p directly targets PDCD6 to inhibit metastasis in breast cancer. Oncol. Lett. 2018, 15, 984–990. [Google Scholar] [CrossRef]
- Duncko, R.; Kiss, A.; Skultétyová, I.; Rusnák, M.; Jezová, D. Corticotropin-releasing hormone mRNA levels in response to chronic mild stress rise in male but not in female rats while tyrosine hydroxylase mRNA levels decrease in both sexes. Psychoneuroendocrinology 2001, 26, 77–89. [Google Scholar] [CrossRef]
- Konkle, A.T.; Baker, S.L.; Kentner, A.C.; Barbagallo, L.S.; Merali, Z.; Bielajew, C. Evaluation of the effects of chronic mild stressors on hedonic and physiological responses: Sex and strain compared. Brain Res. 2003, 992, 227–238. [Google Scholar] [CrossRef]
- Garcia, L.S.; Comim, C.M.; Valvassori, S.S.; Réus, G.Z.; Stertz, L.; Kapczinski, F.; Gavioli, E.C.; Quevedo, J. Ketamine treatment reverses behavioral and physiological alterations induced by chronic mild stress in rats. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2009, 33, 450–455. [Google Scholar] [CrossRef]
- Bielajew, C.; Konkle, A.T.; Merali, Z. The effects of chronic mild stress on male Sprague-Dawley and Long Evans rats: I. Biochemical and physiological analyses. Behav. Brain Res. 2002, 136, 583–592. [Google Scholar] [CrossRef]
- Sévoz-Couche, C.; Brouillard, C.; Camus, F.; Laude, D.; De Boer, S.F.; Becker, C.; Benoliel, J.J. Involvement of the dorsomedial hypothalamus and the nucleus tractus solitarii in chronic cardiovascular changes associated with anxiety in rats. J. Physiol. 2013, 591, 1871–1887. [Google Scholar] [CrossRef]
- Everds, N.E.; Snyder, P.W.; Bailey, K.L.; Bolon, B.; Creasy, D.M.; Foley, G.L.; Rosol, T.J.; Sellers, T. Interpreting stress responses during routine toxicity studies: A review of the biology, impact, and assessment. Toxicol. Pathol. 2013, 41, 560–614. [Google Scholar] [CrossRef] [PubMed]
- Solomon, M.B.; Jankord, R.; Flak, J.N.; Herman, J.P. Chronic stress, energy balance and adiposity in female rats. Physiol. Behav. 2011, 102, 84–90. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Živković, I.; Rakin, A.; Petrović-Djergović, D.; Miljković, B.; Mićić, M. The effects of chronic stress on thymus innervation in the adult rat. Acta Histochem. 2005, 106, 449–458. [Google Scholar] [CrossRef] [PubMed]
- Fortunato, J.J.; Réus, G.Z.; Kirsch, T.R.; Stringari, R.B.; Fries, G.R.; Kapczinski, F.; Hallak, J.E.; Zuardi, A.W.; Crippa, J.A.; Quevedo, J. Effects of β-carboline harmine on behavioral and physiological parameters observed in the chronic mild stress model: Further evidence of antidepressant properties. Brain Res. Bull. 2010, 81, 491–496. [Google Scholar] [CrossRef] [PubMed]
- Silveira, P.P.; Xavier, M.H.; Souza, F.H.; Manoli, L.P.; Rosat, R.M.; Ferreira, M.B.; Dalmaz, C. Interaction between repeated restraint stress and concomitant midazolam administration on sweet food ingestion in rats. Braz. J. Med. Biol. Res. 2000, 33, 1343–1350. [Google Scholar] [CrossRef]
- Ely, D.R.; Dapper, V.; Marasca, J.; Corrêa, J.B.; Gamaro, G.D.; Xavier, M.H.; Michalowski, M.B.; Catelli, D.; Rosat, R.; Ferreira, M.B. Effect of restraint stress on feeding behavior of rats. Physiol. Behav. 1997, 61, 395–398. [Google Scholar] [CrossRef]
- Inagaki, H.; Kuwahara, M.; Tsubone, H. Effects of psychological stress on autonomic control of heart in rats. Exp. Anim. 2004, 53, 373–378. [Google Scholar] [CrossRef][Green Version]
- Kurjanova, E.V.; Teplyj, D.L. Influence of central neurotransmitters on heart rate variability in outbred rats at rest and during acute stress: Nature of very-low-wave spectrum component revisited. Bull. Exp. Biol. Med. 2010, 149, 10–13. [Google Scholar] [CrossRef]
- Chapman, B.J.; Brooks, D.P.; Munday, K.A. Half-life of angiotensin II in the conscious and barbiturate-anaesthetized rat. Br. J. Anaesth. 1980, 52, 389–393. [Google Scholar] [CrossRef]
- Abdulla, M.; Johns, E. Renin-angiotensin and sympathetic nervous system interactions in the control of blood pressure in fructose-induced metabolic syndrome. J. Autacoids 2012, 1, e105. [Google Scholar] [CrossRef]

| Gene | Forward Primer | Reverse Primer | References |
|---|---|---|---|
| ANP | GAGGAGAAGATGCCGGTAG | CTAGAGAGGGAGCTAAGTG | [43] |
| BNP | TGATTCTGCTCCTGCTTTTC | GTGGATTGTTCTGGAGACTG | [43] |
| AT1R | TCTGGATAAATCACACAACCCTC | GAGTTGGTCTCAGACACTATTCG | [44] |
| AT2R | CTGGCAAGCATCTTATGTAGTTC | ACAAGCATTCACACCTAAGTATTC | [44] |
| ACE | TCCTATTCCCGCTCATCT | CCAGCCCTTCTGTACCATT | [45] |
| ACE2 | GAGGAGAATGCCCAAAAGATGA | GAAATTTTGGGCGATCTTGGA | [46] |
| β-actin | AGGGAAATCGTGCGTGAC | CGCTCATTGCCGATAGTG | [47] |
| Parameters | Week 0 | Week 1 | Week 2 | Week 3 | Week 4 |
|---|---|---|---|---|---|
| RR interval (ms) | |||||
| Control | 124.39 ± 2.62 | 122.69 ± 2.41 | 129.47 ± 2.92 | 132.24 ± 4.07 | 132.14 ± 5.88 |
| CMS | 118.86 ± 3.23 | 124.49 ± 4.26 | 127.64 ± 4.15 | 131.43 ± 3.27 | 123.99 ± 2.00 |
| HR (bpm) | |||||
| Control | 484.80 ± 9.71 | 491.06 ± 9.88 | 467.00 ± 9.99 | 456.97 ± 13.04 | 460.47 ± 19.20 |
| CMS | 508.11 ± 13.07 | 473.86 ± 14.96 | 473.86 ± 14.96 | 459.64 ± 11.50 | 485.29 ± 7.91 |
| nSDNN | |||||
| Control | 1 | 0.85 ± 0.05 | 1.19 ± 0.14 | 0.98 ± 0.15 | 1.14 ± 0.12 |
| CMS | 1 | 1.04 ± 0.17 | 1.01 ± 0.14 | 1.26 ± 0.17 | 0.83 ± 0.10 * |
| nRMSSD | |||||
| Control | 1 | 1.08 ± 0.17 | 1.01 ± 0.16 | 1.27 ± 0.23 | 1.08 ± 0.15 |
| CMS | 1 | 1.09 ± 0.08 | 1.10 ± 0.08 | 1.38 ± 0.09 | 1.39 ± 0.25 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bangsumruaj, J.; Kijtawornrat, A.; Kalandakanond-Thongsong, S. Effects of Chronic Mild Stress on Cardiac Autonomic Activity, Cardiac Structure and Renin–Angiotensin–Aldosterone System in Male Rats. Vet. Sci. 2022, 9, 539. https://doi.org/10.3390/vetsci9100539
Bangsumruaj J, Kijtawornrat A, Kalandakanond-Thongsong S. Effects of Chronic Mild Stress on Cardiac Autonomic Activity, Cardiac Structure and Renin–Angiotensin–Aldosterone System in Male Rats. Veterinary Sciences. 2022; 9(10):539. https://doi.org/10.3390/vetsci9100539
Chicago/Turabian StyleBangsumruaj, Janpen, Anusak Kijtawornrat, and Sarinee Kalandakanond-Thongsong. 2022. "Effects of Chronic Mild Stress on Cardiac Autonomic Activity, Cardiac Structure and Renin–Angiotensin–Aldosterone System in Male Rats" Veterinary Sciences 9, no. 10: 539. https://doi.org/10.3390/vetsci9100539
APA StyleBangsumruaj, J., Kijtawornrat, A., & Kalandakanond-Thongsong, S. (2022). Effects of Chronic Mild Stress on Cardiac Autonomic Activity, Cardiac Structure and Renin–Angiotensin–Aldosterone System in Male Rats. Veterinary Sciences, 9(10), 539. https://doi.org/10.3390/vetsci9100539







