Knowledge, Attitude, and Practices on Antimicrobial Use and Antimicrobial Resistance among Poultry Drug and Feed Sellers in Bangladesh
Abstract
1. Introduction
2. Materials and Methods
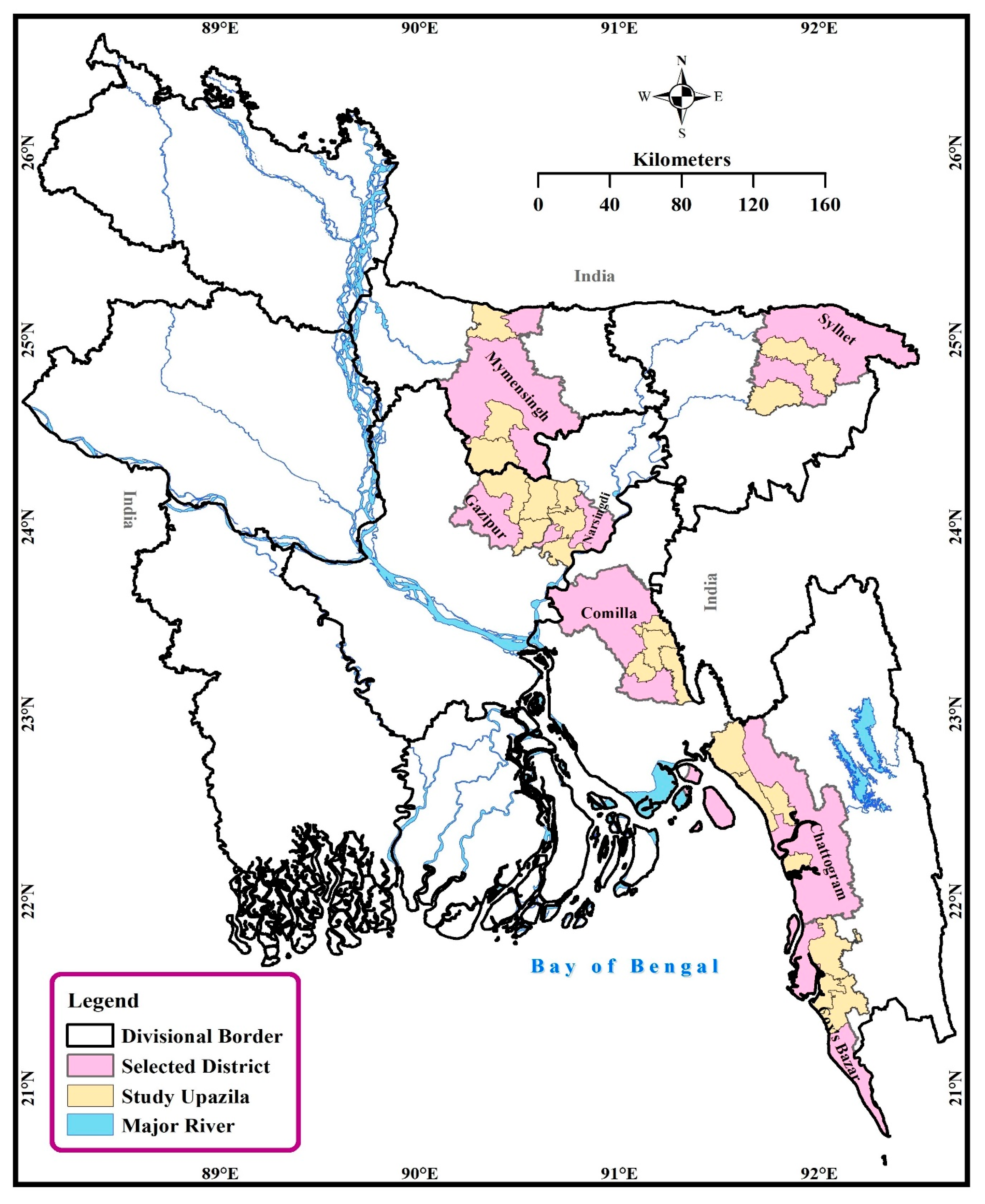
2.1. Study Period and Areas
2.2. Study Area and Sampling
2.3. Data Instrument and Collection
2.4. Data Analyses
3. Results
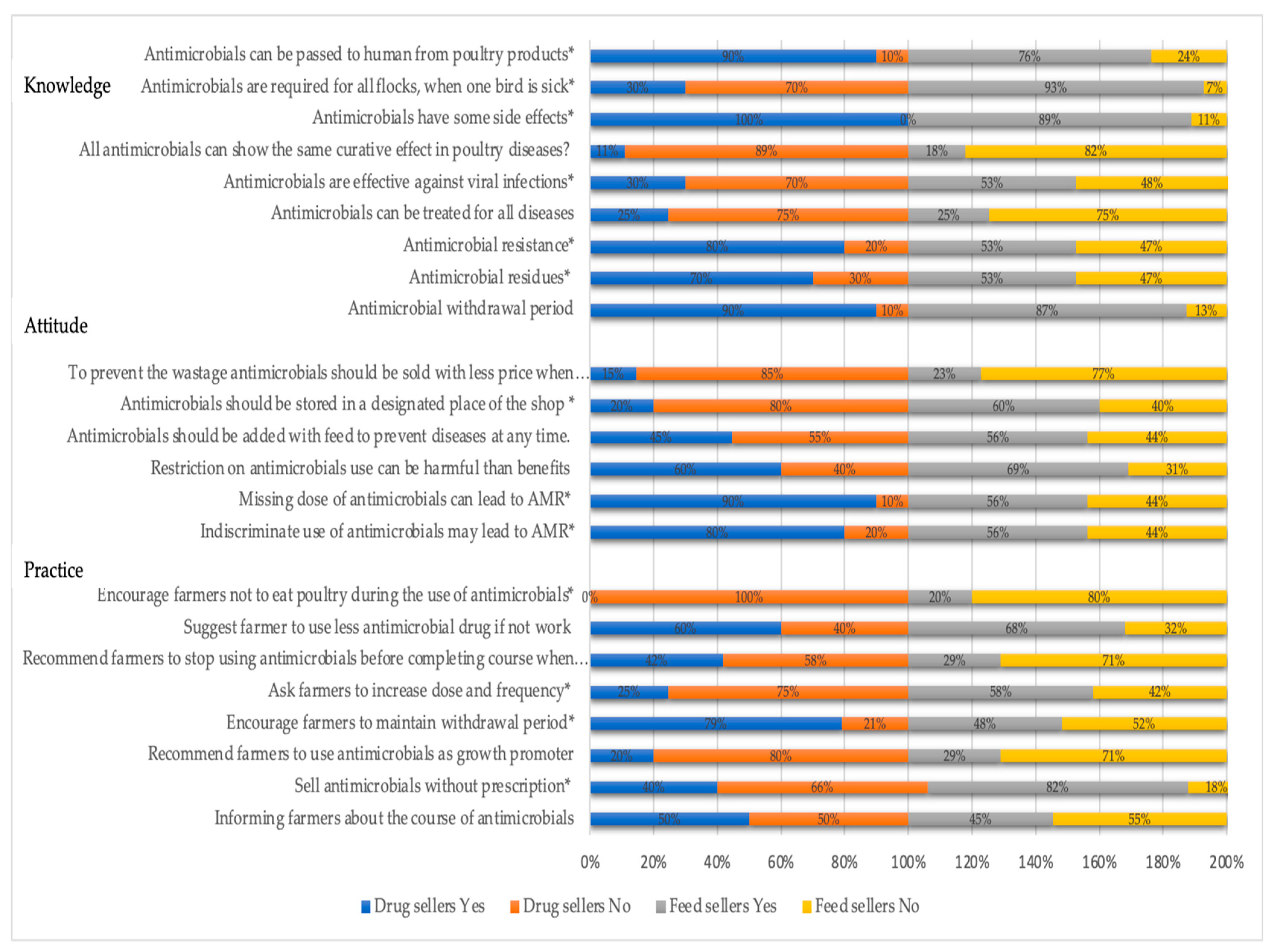
3.1. Knowledge, Attitudes, and Practices of Poultry Drug and Feed Sellers on AMU and AMR
3.2. Differences in Respondents’ Knowledge, Attitudes, and Practices
3.3. Relationship between Knowledge, Attitudes and Practices on AMU and AMR
4. Discussion
5. Conclusions and Recommendations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Davis, C.C.; Willis, C.G.; Primack, R.B.; Miller-Rushing, A.J. The importance of phylogeny to the study of phenological response to global climate change. Philos. Trans. R. Soc. B Biol. Sci. 2010, 365, 3201–3213. [Google Scholar] [CrossRef] [PubMed]
- Livestock Economy at a Glance, Directorate of Livestock Services (DLS). Available online: http://dls.portal.gov.bd/sites/default/files/files/dls.portal.gov.bd/page/ee5f4621_fa3a_40ac_8bd9_898fb8ee4700/2020-07-22-19-34-e4cd5ed65f45419ee038e00b8939c1a0.pdf (accessed on 9 May 2021).
- Das, S.; Chowdhury, S.; Khatun, M.; Nishibori, M.; Isobe, N.; Yoshimura, Y. Poultry production profile and expected future projection in Bangladesh. World Poult. Sci. J. 2008, 64, 99–118. [Google Scholar] [CrossRef]
- Raihan, S.; Mahmud, M.T. Trade and Poverty Linkages: A Case Study of the Poultry Industry in Bangladesh; CUTS International: Geneva, Switzerland, 2008. [Google Scholar]
- Agyare, C.; Boamah, V.E.; Zumbi, C.N.; Osei, F.B. Antibiotic Use in Poultry Production and Its Effects on Bacterial Resistance. In Antimicrobial Resistance—A Global Threat; IntechOpen: London, UK, 2019. [Google Scholar]
- Hassan, M.M. Scenario of Antibiotic Resistance in Developing Countries. In Antimicrobial Resistance—A One Health Perspective; IntechOpen: London, UK, 2020. [Google Scholar]
- Caudell, M.A.; Dorado-Garcia, A.; Eckford, S.; Creese, C.; Byarugaba, D.K.; Afakye, K.; Chansa-Kabali, T.; Fasina, F.O.; Kabali, E.; Kiambi, S.; et al. Towards a bottom-up understanding of antimicrobial use and resistance on the farm: A knowledge, attitudes, and practices survey across livestock systems in five African countries. PLoS ONE 2020, 15, e0220274. [Google Scholar] [CrossRef]
- Hassan, M.M.; El Zowalaty, M.E.; Lundkvist, Å.; Järhult, J.D.; Nayem, R.K.; Tanzin, A.Z.; Badsha, R.; Khan, S.A.; Ashour, H.M. Residual antimicrobial agents in food originating from animals. Trends Food Sci. Technol. 2021, 111, 141–150. [Google Scholar] [CrossRef]
- Agmas, B.; Adugna, M. Antimicrobial residue occurrence and its public health risk of beef meat in Debre Tabor and Bahir Dar, Northwest Ethiopia. Vet. World 2018, 11, 902–908. [Google Scholar] [CrossRef] [PubMed]
- Moreno, L.; Lanusse, C. Veterinary drug residues in meat-related edible tissues. In New Aspects of Meat Quality; Elsevier: Amsterdam, The Netherlands, 2017; pp. 581–603. [Google Scholar]
- Chowdhury, S.; Hassan, M.M.; Alam, M.; Sattar, S.; Bari, M.S.; Saifuddin, A.; Hoque, M.A. Antibiotic residues in milk and eggs of commercial and local farms at Chittagong, Bangladesh. Vet. World 2015, 8, 467. [Google Scholar] [CrossRef]
- Sattar, S.; Hassan, M.M.; Islam, S.K.M.A.; Alam, M.; Al Faruk, S.; Chowdhury, S.; Saifuddin, A.K.M. Antibiotic residues in broiler and layer meat in Chittagong district of Bangladesh. Vet. World 2014, 7, 7. [Google Scholar] [CrossRef]
- Islam, A.; Saifuddin, A.; Al Faruq, A.; Islam, S.; Shano, S.; Alam, M.; Hassan, M.M. Antimicrobial residues in tissues and eggs of laying hens at Chittagong, Bangladesh. Int. J. One Health 2016, 2, 75–80. [Google Scholar] [CrossRef]
- Heuer, O.E.; Kruse, H.; Grave, K.; Collignon, P.; Karunasagar, I.; Angulo, F.J.J.C.I.D. Human health consequences of use of antimicrobial agents in aquaculture. Clin. Infect. Dis. 2009, 49, 1248–1253. [Google Scholar] [CrossRef]
- Asaduzzaman, M. Livestock sector, economic development and poverty alleviation in Bangladesh. In Changing Rural Economy of Bangladesh; Bangladesh Economic Association: Dhaka, Bangladesh, 2000; pp. 42–53. [Google Scholar]
- Butaye, P.; Devriese, L.A.; Haesebrouck, F.J.C. Antimicrobial growth promoters used in animal feed: Effects of less well known antibiotics on gram-positive bacteria. Clin. Microbiol. Rev. 2003, 16, 175–188. [Google Scholar] [CrossRef] [PubMed]
- Imam, T.; Gibson, J.S.; Foysal, M.; Das, S.B.; Gupta, S.D.; Fournié, G.; Hoque, M.A.; Henning, J. A cross-sectional study of antimicrobial usage on commercial broiler and layer chicken farms in Bangladesh. Front. Vet. Sci. 2020, 7, 7. [Google Scholar] [CrossRef]
- Khan, S.A.; Imtiaz, M.A.; Sayeed, M.A.; Shaikat, A.H.; Hassan, M.M. Antimicrobial resistance pattern in domestic animal-wildlife-environmental niche via the food chain to humans with a Bangladesh perspective; a systematic review. BMC Vet. Res. 2020, 16, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Peeling, D.; Holden, S. The effectiveness of community-based animal health workers, for the poor, for communities and for public safety. Rev. Sci. Tech. 2004, 23, 253–276. [Google Scholar] [CrossRef]
- Roess, A.A.; Afroz, D.; Winch, P.J.; Darmstadt, G.L.; Ali, N.A.; Baqui, A.H.; El Arifeen, S.; Akhter, A.; the Bangladesh Projahnmo Study Group. Animal Husbandry Practices in Rural Bangladesh: Potential Risk Factors for Antimicrobial Drug Resistance and Emerging Diseases. Am. J. Trop. Med. Hyg. 2013, 89, 965–970. [Google Scholar] [CrossRef] [PubMed]
- McEwen, S.A.; Fedorka-Cray, P. Antimicrobial use and resistance in animals. Clin. Infect. Dis. 2002, 34, S93–S106. [Google Scholar] [CrossRef]
- Maron, D.F.; Smith, T.J.; Nachman, K.E. Restrictions on antimicrobial use in food animal production: An international regulatory and economic survey. Glob. Health 2013, 9, 48. [Google Scholar] [CrossRef]
- Olivier, C.; Williams-Jones, B.; Doize, B.; Ozdemir, V. Containing global antibiotic resistance: Ethical drug promotion in the developing world. In Antimicrobial Resistance in Developing Countries; Springer: Berlin/Heidelberg, Germany, 2010; pp. 505–524. [Google Scholar]
- Al Masud, A.; Rousham, E.K.; Islam, M.A.; Alam, M.-U.; Rahman, M.; Al Mamun, A.; Sarker, S.; Asaduzzaman, M.; Unicomb, L. Drivers of antibiotic use in poultry production in Bangladesh: Dependencies and dynamics of a patron-client relationship. Front. Vet. Sci. 2020, 7, 78. [Google Scholar] [CrossRef]
- Lembke, A. Drug Dealer, MD: How Doctors Were Duped, Patients Got Hooked, and Why It’s so Hard to Stop; JHU Press: Baltimore, MD, USA, 2016. [Google Scholar]
- Van Cuong, N.; Nhung, N.T.; Nghia, N.H.; Hoa, N.T.M.; Trung, N.V.; Thwaites, G.; Carrique-Mas, J. Antimicrobial consumption in medicated feeds in Vietnamese pig and poultry production. Ecohealth 2016, 13, 490–498. [Google Scholar] [CrossRef]
- Landoni, M.; Albarellos, G. The use of antimicrobial agents in broiler chickens. Vet. J. 2015, 205, 21–27. [Google Scholar] [CrossRef]
- Knoop, K.A.; McDonald, K.G.; Kulkarni, D.H.; Newberry, R. Antibiotics promote inflammation through the translocation of native commensal colonic bacteria. Gut 2016, 65, 1100–1109. [Google Scholar] [CrossRef]
- van den Bogaard, A.E.; Stobberingh, E. Epidemiology of resistance to antibiotics: Links between animals and humans. Int. J. Antimicrob. Agents 2000, 14, 327–335. [Google Scholar] [CrossRef]
- Hassan, M.M.; Amin, K.B.; Ahaduzzaman, M.; Alam, M.; Faruk, M.S.; Uddin, I. Antimicrobial resistance pattern against E. coli and Salmonella in layer poultry. Res. J. Vet. Pract. 2014, 2, 30–35. [Google Scholar] [CrossRef]
- Micallef, C.; Kildonaviciute, K.; Castro-Sánchez, E.; Scibor-Stepien, A.; Santos, R.; Aliyu, S.H.; Cooke, F.J.; Pacey, S.; Holmes, A.H.; Enoch, D. Patient and public understanding and knowledge of antimicrobial resistance and stewardship in a UK hospital: Should public campaigns change focus? J. Antimicrob. Chemother. 2016, 72, 311–314. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, I.; Rabbi, B.; Sultana, S. Antibiotic resistance in Bangladesh: A systematic review. Int. J. Infect. Dis. 2019, 80, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Raosoft. Sample Size Calculator. Available online: https://www.calculator.net/sample-size-calculator.html?type=1&cl=85&ci=5&pp=50&ps=&x=53&y=14 (accessed on 9 May 2021).
- Kim, J.-O.; Mueller, C.W. Factor Analysis: Statistical Methods and Practical Issues; Sage: New York, NY, USA, 1978; Volume 14. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Academic press: Cambridge, MA, USA, 2013. [Google Scholar]
- Rigg, K.K.; Kurtz, S.P.; Surratt, H.L. Patterns of prescription medication diversion among drug dealers. Drugs Educ. Prev. Policy 2012, 19, 145–155. [Google Scholar] [CrossRef] [PubMed]
- Hoxha, I.; Malaj, A.; Kraja, B.; Bino, S.; Oluka, M.; Marković-Peković, V.; Godman, B. Are pharmacists’ good knowledge and awareness on antibiotics taken for granted? The situation in Albania and future implications across countries. J. Glob. Antimicrob. Resist. 2018, 13, 240–245. [Google Scholar] [CrossRef] [PubMed]
- Hedman, H.D.; Vasco, K.A.; Zhang, L. A Review of Antimicrobial Resistance in Poultry Farming within Low-Resource Settings. Animals 2020, 10, 1264. [Google Scholar] [CrossRef]
- Glasgow, L.; Forde, M.; Brow, D.; Mahoney, C.; Fletcher, S.; Rodrigo, S. Antibiotic use in poultry production in Grenada. Vet. Med. Int. 2019, 2019, 1–7. [Google Scholar] [CrossRef][Green Version]
- Hassan, M.M.; Begum, S.; Al Faruq, A.; Alam, M.; Mahmud, T.; Islam, A. Multidrug resistant Salmonella isolated from street foods in Chittagong, Bangladesh. Microbiol. Res. J. Int. 2018, 26, 1–8. [Google Scholar] [CrossRef]
- Rousham, E.K.; Islam, M.A.; Nahar, P.; Lucas, P.J.; Naher, N.; Ahmed, S.M.; Nizame, F.A.; Unicomb, L. Pathways of antibiotic use in Bangladesh: Qualitative protocol for the PAUSE study. BMJ Open 2019, 9, e028215. [Google Scholar] [CrossRef]
- Gajdács, M.; Paulik, E.; Szabó, A. Knowledge, attitude and practice of community pharmacists regarding antibiotic use and infectious diseases: A cross-sectional survey in Hungary (KAPPhA-HU). Antibiotics 2020, 9, 41. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.M.; Naher, N.; Hossain, T.; Rawal, L.B. Exploring the status of retail private drug shops in Bangladesh and action points for developing an accredited drug shop model: A facility based cross-sectional study. J. Pharm. Policy Pract. 2017, 10, 1–12. [Google Scholar] [CrossRef]
- Pham-Duc, P.; Cook, M.A.; Cong-Hong, H.; Nguyen-Thuy, H.; Padungtod, P.; Nguyen-Thi, H.; Dang-Xuan, S. Knowledge, attitudes and practices of livestock and aquaculture producers regarding antimicrobial use and resistance in Vietnam. PLoS ONE 2019, 14, e0223115. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Guo, F.; Wei, J.; Zhang, Y.; Liu, Z.; Huang, Y. Knowledge, attitudes and practices in relation to antimicrobial resistance amongst Chinese public health undergraduates. J. Glob. Antimicrob. Resist. 2020, 23, 9–15. [Google Scholar] [CrossRef]
- Waseem, H.; Ali, J.; Sarwar, F.; Khan, A.; Rehman, H.S.U.; Choudri, M.; Arif, N.; Subhan, M.; Saleem, A.R.; Jamal, A. Assessment of knowledge and attitude trends towards antimicrobial resistance (AMR) among the community members, pharmacists/pharmacy owners and physicians in district Sialkot, Pakistan. Antimicrob. Resist. Infect. Control 2019, 8, 1–7. [Google Scholar] [CrossRef]
- Nepal, A.; Hendrie, D.; Robinson, S.; Selvey, L.A. Knowledge, attitudes and practices relating to antibiotic use among community members of the Rupandehi District in Nepal. BMC Public Health 2019, 19, 1–12. [Google Scholar] [CrossRef]
- Reynolds, L.; McKee, M. Factors influencing antibiotic prescribing in China: An exploratory analysis. Health Policy 2009, 90, 32–36. [Google Scholar] [CrossRef]
- Ministry of Health and Family Welfare. National Action Plan: Antimicrobial Resistance Containment in Bangladesh 2017–2022; Directorate General of Health Services: Dhaka, Bangladesh, 2017; pp. 1–12. [Google Scholar]

| Variables | n (%) | |
|---|---|---|
| Type of respondents | Drug sellers | 110 (50.0) |
| Feed sellers | 110 (50.0) | |
| Age (Years) | Minimum–25 | 23 (10.5) |
| 26–30 | 42 (19.1) | |
| 31–35 | 63 (28.6) | |
| 36–40 | 35 (15.9) | |
| 41 or more | 57 (25.9) | |
| Years of experience (Years) | 0–4 | 25 (11.4) |
| 5–8 | 96 (43.6) | |
| 9–12 | 79 (35.9) | |
| 13 or more | 20 (9.1) | |
| Level of Education | Graduate | 95 (43.2) |
| Up to 12th grade | 125 (56.8) | |
| Training on drug | Non-trained | 113 (51.4) |
| Trained | 107 (48.6) | |
| Variables | Knowledge | Attitudes | Practices | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Incorrect: n (%) | Correct: n (%) | p | Negative: n (%) | Positive: n (%) | p | Bad: n (%) | Good: n (%) | p | ||
| Type of respondent | Drug sellers | 45 (40.9) | 65 (59.1) | 0.000 | 27 (24.6) | 83 (75.4) | 0.000 | 33 (30) | 77 (70) | 0.000 |
| Feed sellers | 72 (65.4) | 38 (34.6) | 84 (76.4) | 26 (23.6) | 84 (76.4) | 26 (23.6) | ||||
| Age (years) | Minimum–25 | 12 (52.2) | 11 (47.8) | 0.074 | 14 (60.9) | 9 (39.1) | 0.047 | 11 (47.8) | 12 (52.2) | 0.077 |
| 26–30 | 21 (50.0) | 21 (50.0) | 24 (57.1) | 18 (42.9) | 17 (40.5) | 25 (59.5) | ||||
| 31–35 | 42 (66.7) | 21 (33.3) | 28 (44.4) | 35 955.6) | 37 (58.7) | 26 (41.3) | ||||
| 36–40 | 13 (37.1) | 22 (62.9) | 11 (31.43) | 24 (68.6) | 15 (42.9) | 20 (57.1) | ||||
| 41 or more | 29 (50.9) | 28 (49.1) | 34 (59.6) | 23 (40.4) | 37 (64.9) | 20 (35.1) | ||||
| Years of experience | 0–4 | 20 (80.0) | 5 (20.0) | 0.000 | 16 (64.0) | 9 (36.0) | 0.078 | 18 (72.0) | 7 (28.0) | 0.028 |
| 5–8 | 61 (63.5) | 35 (36.5) | 53 (55.2) | 43 (44.8) | 56 (58.3) | 40 (41.7) | ||||
| 9–12 | 29 (36.7) | 50 (63.3) | 36 (45.6) | 43 (54.4) | 36 (45.6) | 43 (54.4) | ||||
| 13 or more | 7 (35.0) | 13 (65.0) | 6 (30.0) | 14 (70.0) | 7 (35.0) | 13 (65.0) | ||||
| Level of Education | Graduate | 65 (68.4) | 30 (31.6) | 0.000 | 59 (62.1) | 36 (37.9) | 0.003 | 60 (63.2) | 35 (36.8) | 0.673 |
| Up to 12th grade | 52 (41.6) | 73 (58.4) | 52 (41.6) | 73 (58.4) | 57 (45.6) | 68 (54.4) | ||||
| Training on drug | Non-trained | 76 (67.3) | 37 (32.7) | 0.000 | 57 (50.4) | 54 (50.5) | 0.997 | 60 (53.1) | 53 (46.9) | 0.979 |
| Trained | 41 (38.3) | 66 (61.7) | 56 (49.5) | 53 (49.5) | 57 (53.3) | 50 (46.7) | ||||
| Variables | Knowledge | Attitudes | Practices | |
|---|---|---|---|---|
| OR, 95%CI, p | OR, 95%CI, p | OR, 95%CI, p | ||
| Type of respondents | Feed sellers | Ref | Ref | Ref |
| Drug sellers | 5.20, 2.5–11.0, 0.000 | 26.71, 10.5–68.0, 0.000 | 14.16, 6.33–31.66, 0.000 | |
| Age (Years) | 41 or more | Ref | Ref | Ref |
| 18–25 | 1.33, 0.42–4.22, 0.633 | 1.20, 0.30–4.71, 0.797 | 4.73, 1.33–16.85, 0.017 | |
| 26–30 | 1.24, 0.48–3.23, 0.658 | 1.52, 0.53–4.3, 0.435 | 5.85, 2.03–16.87, 0.001 | |
| 31–35 | 0.63, 0.25–1.56, 0.318 | 3.72, 1.42–9.72, 0.007 | 2.12, 0.84–5.36, 0.298 | |
| 36–40 | 1.26, 0.43–3.72, 0.672 | 4.59, 1.31–16.08, 0.017 | 2.58, 0.84–7.97, 0.098 | |
| Experience(Years) | 0–4 | Ref | Ref | Ref |
| 5–8 | 1.79, 0.54–5.93, 0.339 | 0.74, 0.24–2.31, 0.608 | 1.38, 0.45–4.21, 0.571 | |
| 9–12 | 3.78, 1.07–13.32, 0.039 | 0.64, 0.18–2.29, 0.493 | 1.80, 0.536.13, 0.348 | |
| 13 or more | 3.23, 0.68–15.46, 0.142 | 1.60, 0.30–8.55, 0.578 | 2.89, 0.58–14.38, 0.196 | |
| Level of Education | Graduate | Ref | Ref | Ref |
| Up to 12th grade | 4.88, 2.42–9.85, 0.000 | 7.80, 3.25–18.68, 0.000 | 3.68, 1.76–7.68, 0.001 | |
| Training on drug | Not trained | Ref | Ref | Ref |
| Trained | 5.22, 2.52–10.81, 0.000 | 1.93, 0.90–4.15, 0.093 | 1.47, 0.72–2.98, 0.291 | |
| Variables | Correlation Coefficient | p-Value |
|---|---|---|
| Knowledge–Attitudes | 0.4731 | 0.000 |
| Knowledge–Practice | 0.3610 | 0.000 |
| Attitudes–Practices | 0.3456 | 0.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kalam, M.A.; Alim, M.A.; Shano, S.; Nayem, M.R.K.; Badsha, M.R.; Mamun, M.A.A.; Hoque, A.; Tanzin, A.Z.; Khan, S.A.; Islam, A.; et al. Knowledge, Attitude, and Practices on Antimicrobial Use and Antimicrobial Resistance among Poultry Drug and Feed Sellers in Bangladesh. Vet. Sci. 2021, 8, 111. https://doi.org/10.3390/vetsci8060111
Kalam MA, Alim MA, Shano S, Nayem MRK, Badsha MR, Mamun MAA, Hoque A, Tanzin AZ, Khan SA, Islam A, et al. Knowledge, Attitude, and Practices on Antimicrobial Use and Antimicrobial Resistance among Poultry Drug and Feed Sellers in Bangladesh. Veterinary Sciences. 2021; 8(6):111. https://doi.org/10.3390/vetsci8060111
Chicago/Turabian StyleKalam, Md. Abul, Md. Abdul Alim, Shahanaj Shano, Md. Raihan Khan Nayem, Md. Rahim Badsha, Md. Abdullah Al Mamun, Ashraful Hoque, Abu Zubayer Tanzin, Shahneaz Ali Khan, Ariful Islam, and et al. 2021. "Knowledge, Attitude, and Practices on Antimicrobial Use and Antimicrobial Resistance among Poultry Drug and Feed Sellers in Bangladesh" Veterinary Sciences 8, no. 6: 111. https://doi.org/10.3390/vetsci8060111
APA StyleKalam, M. A., Alim, M. A., Shano, S., Nayem, M. R. K., Badsha, M. R., Mamun, M. A. A., Hoque, A., Tanzin, A. Z., Khan, S. A., Islam, A., Islam, M. M., & Hassan, M. M. (2021). Knowledge, Attitude, and Practices on Antimicrobial Use and Antimicrobial Resistance among Poultry Drug and Feed Sellers in Bangladesh. Veterinary Sciences, 8(6), 111. https://doi.org/10.3390/vetsci8060111











