The Design, Development, and Clinical Assessment of a Novel Patented Laparoscopic Instrument for Ovariectomy in Dogs
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
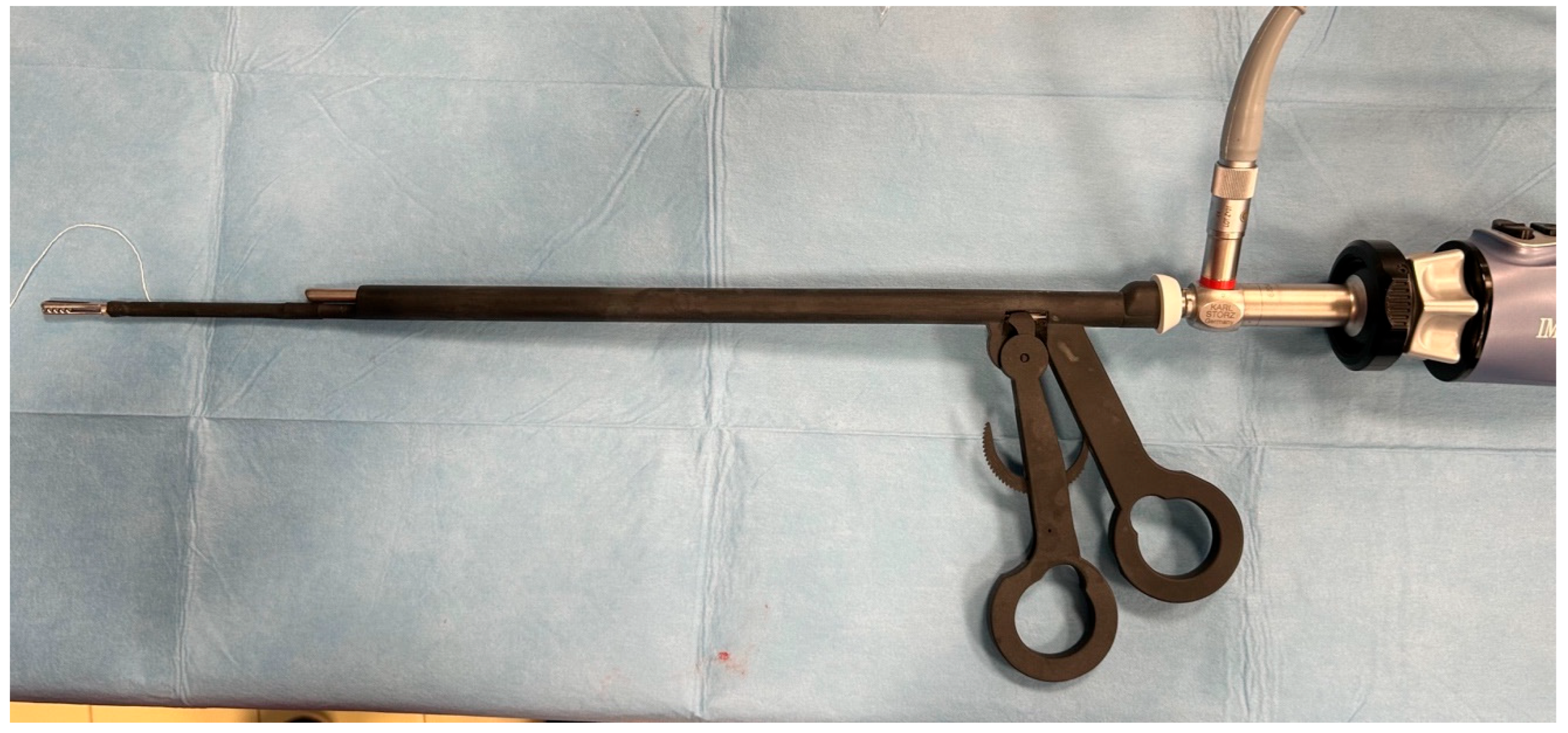
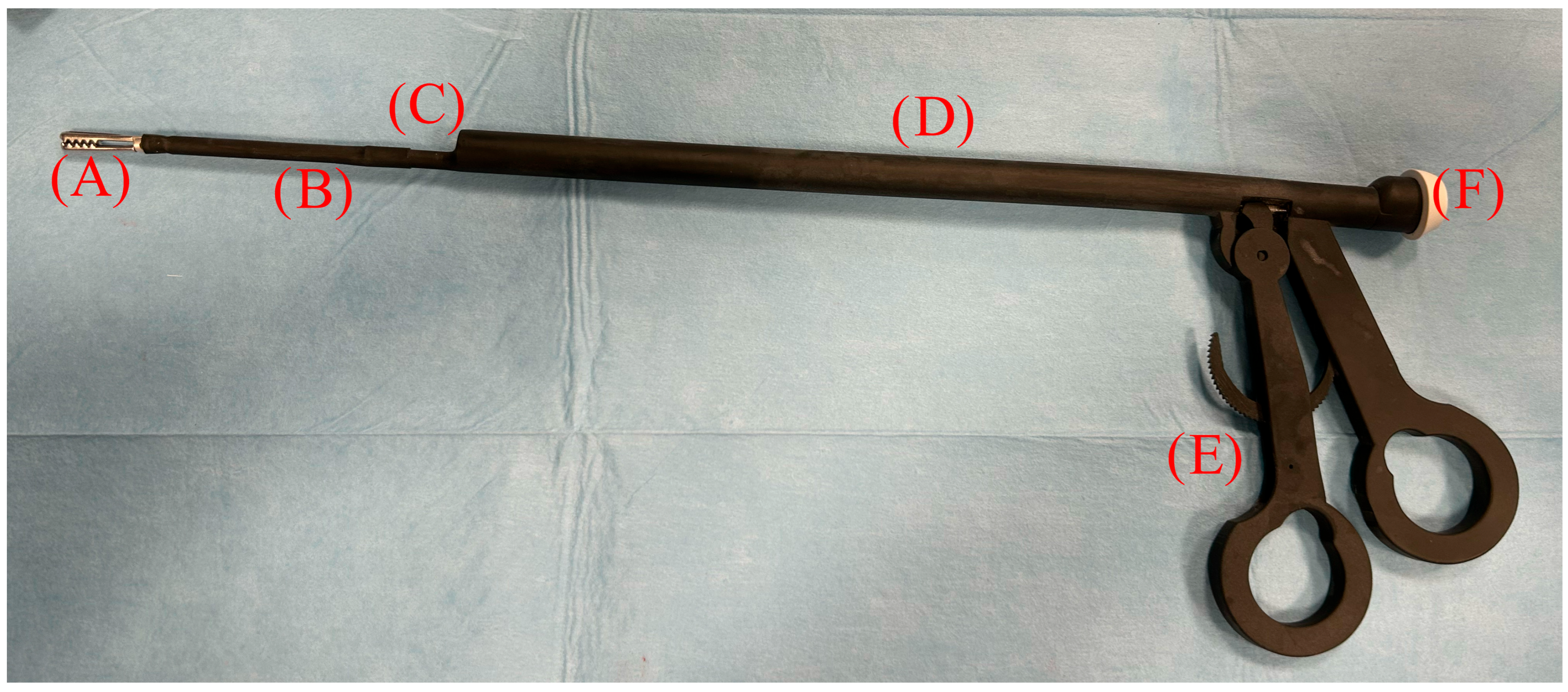
2.1. Instrumentation
2.2. Production of Highly Reliable Prototypes
2.3. Sterilization Tests
- ISO 18593:2004 for microbiological sampling of surfaces;
- Swabs with plastic shafts and cellulose tips with a transport medium and a disposable plastic delimiter (surface area: 100 cm2);
- Swabs taken from the handle, shaft, and insert of laparoscopic forceps after sanitization and EtOx sterilization;
- The total mesophilic count (TMC) at 30 °C (ISO 4833:2003—Horizontal method for the enumeration of microorganisms—Colony-count technique at 30 °C);
- The Enterobacteriaceae count (ISO 21528-2:2017, Part 2: Colony-count technique).
2.4. Ex Vivo Clinical Application
2.5. In Vivo Clinical Study
2.5.1. Patients
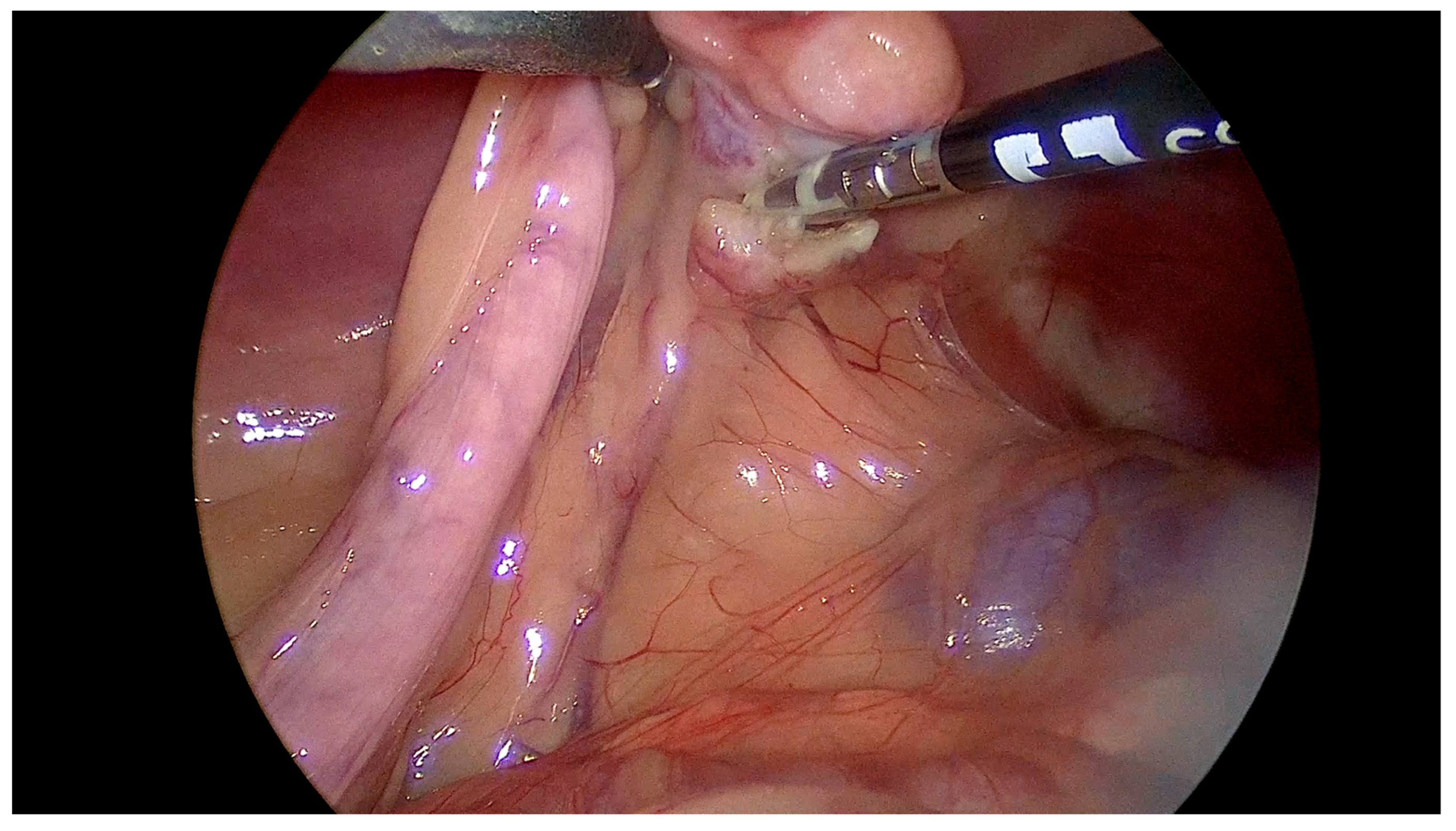
2.5.2. Surgical Technique
2.5.3. Surgical Variables
2.5.4. Statistical Analysis
3. Results
3.1. Sterilization Test
3.2. Microbiological Tests
3.3. Cadaveric Tests
3.4. Clinical Study
4. Discussion
5. Conclusions
6. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Culp, W.T.; Mayhew, P.D.; Brown, D.C. The effect of laparoscopic versus open ovariectomy on postsurgical activity in small dogs. Vet. Surg. 2009, 38, 811–817. [Google Scholar] [CrossRef]
- Manassero, M.; Viateau, V. Advances in laparoscopic spay techniques for dogs: The past, present and future. Vet. Rec. 2018, 183, 742–744. [Google Scholar] [CrossRef] [PubMed]
- Dupre, G.; Fiorbianco, V.; Skalicky, M.; Gultiken, N.; Ay, S.S.; Findik, M. Laparoscopic ovariectomy in dogs: Comparison between single portal and two-portal access. Vet. Surg. 2009, 38, 818–824. [Google Scholar] [CrossRef] [PubMed]
- Van Goethem, B.E.; Rosenveldt, K.W.; Kirpensteijn, J. Monopolar versus bipolar electrocoagulation in canine laparoscopic ovariectomy: A nonrandomized, prospective, clinical trial. Vet. Surg. 2003, 32, 464–470. [Google Scholar] [CrossRef]
- Fuertes-Recuero, M.; de Segura, I.A.G.; López, A.S.; Suárez-Redondo, M.; Arrabé, S.C.; Hidalgo, S.P.; Fontanillas-Pérez, J.C.; Ortiz-Diez, G. Postoperative pain in dogs undergoing either laparoscopic or open ovariectomy. Vet. J. 2024, 306, 106156. [Google Scholar] [CrossRef]
- Bydzovsky, N.D.; Bockstahler, B.; Dupré, G. Single-port laparoscopic-assisted ovariohysterectomy with a modified glove-port technique in dogs. Vet. Surg. 2019, 48, 715–725. [Google Scholar] [CrossRef] [PubMed]
- Gower, S.; Mayhew, P. Canine laparoscopic and laparoscopic-assisted ovariohysterectomy and ovariectomy. Compend. Contin. Educ. Vet. 2008, 30, 430–432, 434, 436, 438, 440. [Google Scholar]
- Lacitignola, L.; Guadalupi, M.; Massari, F. Single Incision Laparoscopic Surgery (SILS) in Small Animals: A Systematic Review and Meta-Analysis of Current Veterinary Literature. Vet. Sci. 2021, 8, 144. [Google Scholar] [CrossRef]
- Tapia-Araya, A.E.; Díaz-Güemes Martin-Portugués, I.; Bermejo, L.F.; Sánchez-Margallo, F.M. Laparoscopic ovariectomy in dogs: Comparison between laparoendoscopic single-site and three-portal access. J. Vet. Sci. 2015, 16, 525–530. [Google Scholar] [CrossRef]
- Becher-Deichsel, A.; Aurich, J.E.; Schrammel, N.; Dupre, G. A surgical glove port technique for laparoscopic-assisted ovariohysterectomy for pyometra in the bitch. Theriogenology 2016, 86, 619–625. [Google Scholar] [CrossRef]
- Arntz, G.H.M. Transvaginal laparoscopic ovariectomy in 60 dogs: Description of the technique and comparison with 2-portal-access laparoscopic ovariectomy. Vet. Surg. 2019, 48, 726–734. [Google Scholar] [CrossRef] [PubMed]
- Linhares, M.T.; Feranti, J.P.S.; Coradini, G.P.; Martins, L.R.; Martins, A.R.; Sarturi, V.Z.; Gavioli, F.B.; Machado Silva, M.A.; de Ataíde, M.W.; Teixeira, L.G. Canine ovariectomy by hybrid or total natural orifice transluminal endoscopic surgery: Technical feasibility study and pain assessment. Vet. Surg. 2019, 48, O74–O82. [Google Scholar] [CrossRef]
- Delaune, T.; Matres-Lorenzo, L.; Bernarde, A.; Bernard, F. Use of a T’LIFT transabdominal organ retraction device in two-portal laparoscopic ovariectomy in dogs. Vet. Surg. 2021, 50 (Suppl. S1), O40–O48. [Google Scholar] [CrossRef] [PubMed]
- Case, J.B.; Marvel, S.J.; Boscan, P.; Monnet, E.L. Surgical time and severity of postoperative pain in dogs undergoing laparoscopic ovariectomy with one, two, or three instrument cannulas. J. Am. Vet. Med. Assoc. 2011, 239, 203–208. [Google Scholar] [CrossRef]
- Maurin, M.P.; Mullins, R.A.; Singh, A.; Mayhew, P.D. A systematic review of complications related to laparoscopic and laparoscopic-assisted procedures in dogs. Vet. Surg. 2020, 49 (Suppl. S1), O5–O14. [Google Scholar] [CrossRef]
- Manassero, M.; Leperlier, D.; Vallefuoco, R.; Viateau, V. Laparoscopic ovariectomy in dogs using a single-port multiple-access device. Vet. Rec. 2012, 171, 69. [Google Scholar] [CrossRef]
- Binder, C.; Katic, N.; Aurich, J.E.; Dupre, G. Postoperative complications and owner assessment of single portal laparoscopic ovariectomy in dogs. Vet. Rec. 2018, 183, 745. [Google Scholar] [CrossRef]
- Mayhew, P.D.; Brown, D.C. Comparison of three techniques for ovarian pedicle hemostasis during laparoscopic-assisted ovariohysterectomy. Vet. Surg. 2007, 36, 541–547. [Google Scholar] [CrossRef] [PubMed]
- Öhlund, M.; Höglund, O.; Olsson, U.; Lagerstedt, A.-S. Laparoscopic ovariectomy in dogs: A comparison of the LigaSure™ and the SonoSurg™ systems. J. Small Anim. Pract. 2011, 52, 290–294. [Google Scholar] [CrossRef]
- Van Nimwegen, S.A.; Kirpensteijn, J. Comparison of Nd:YAG surgical laser and Remorgida bipolar electrosurgery forceps for canine laparoscopic ovariectomy. Vet. Surg. 2007, 36, 533–540. [Google Scholar] [CrossRef]
- Van Nimwegen, S.A.; Van Swol, C.F.; Kirpensteijn, J. Neodymium:yttrium aluminum garnet surgical laser versus bipolar electrocoagulation for laparoscopic ovariectomy in dogs. Vet. Surg. 2005, 34, 353–357. [Google Scholar] [CrossRef] [PubMed]


| Phase | Sample Point | TMC at 30 °C (CFU/cm2) | Enterobacteriaceae (CFU/cm2) |
|---|---|---|---|
| Post-sanitization | Handle | 2 | 0 |
| Post-sanitization | Shaft and insert | 6 | 0 |
| Post-sterilization | Handle | 0 | 0 |
| Post-sterilization | Shaft and insert | 0 | 0 |
| Technique | Installation Time | Ovariectomy Time | Closure Time | Total Surgery Time | |
|---|---|---|---|---|---|
| Mean | ES | 3.28 | 23.7 | 3.44 | 30.4 |
| OF | 3.33 | 7.50 | 3.44 | 14.3 | |
| Mean lower bound of 95% CI | ES | 2.78 | 20.2 | 3.16 | 27.0 |
| OF | 2.83 | 6.75 | 3.21 | 13.5 | |
| Mean upper bound of 95% CI | ES | 3.77 | 27.3 | 3.73 | 33.9 |
| OF | 3.83 | 8.25 | 3.68 | 15.1 | |
| Median | ES | 3.00 | 23.5 | 3.00 | 29.5 |
| OF | 3.00 | 7.00 | 3.00 | 15.0 | |
| Standard deviation | ES | 1.07 | 7.69 | 0.616 | 7.43 |
| OF | 1.08 | 1.62 | 0.511 | 1.74 | |
| Minimum | ES | 2 | 12 | 3 | 18 |
| OF | 2 | 6 | 3 | 11 | |
| Maximum | ES | 6 | 35 | 5 | 43 |
| OF | 6 | 12 | 4 | 17 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guadalupi, M.; Piemontese, C.; Vicenti, C.; Piergentili, R.; Staffieri, F.; Lacitignola, L. The Design, Development, and Clinical Assessment of a Novel Patented Laparoscopic Instrument for Ovariectomy in Dogs. Vet. Sci. 2025, 12, 639. https://doi.org/10.3390/vetsci12070639
Guadalupi M, Piemontese C, Vicenti C, Piergentili R, Staffieri F, Lacitignola L. The Design, Development, and Clinical Assessment of a Novel Patented Laparoscopic Instrument for Ovariectomy in Dogs. Veterinary Sciences. 2025; 12(7):639. https://doi.org/10.3390/vetsci12070639
Chicago/Turabian StyleGuadalupi, Marta, Claudia Piemontese, Caterina Vicenti, Rachele Piergentili, Francesco Staffieri, and Luca Lacitignola. 2025. "The Design, Development, and Clinical Assessment of a Novel Patented Laparoscopic Instrument for Ovariectomy in Dogs" Veterinary Sciences 12, no. 7: 639. https://doi.org/10.3390/vetsci12070639
APA StyleGuadalupi, M., Piemontese, C., Vicenti, C., Piergentili, R., Staffieri, F., & Lacitignola, L. (2025). The Design, Development, and Clinical Assessment of a Novel Patented Laparoscopic Instrument for Ovariectomy in Dogs. Veterinary Sciences, 12(7), 639. https://doi.org/10.3390/vetsci12070639







