Evaluation of the Blood Neutrophil-to-Lymphocyte Ratio (NLR) as a Diagnostic and Prognostic Biomarker in Dogs with Portosystemic Shunt
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
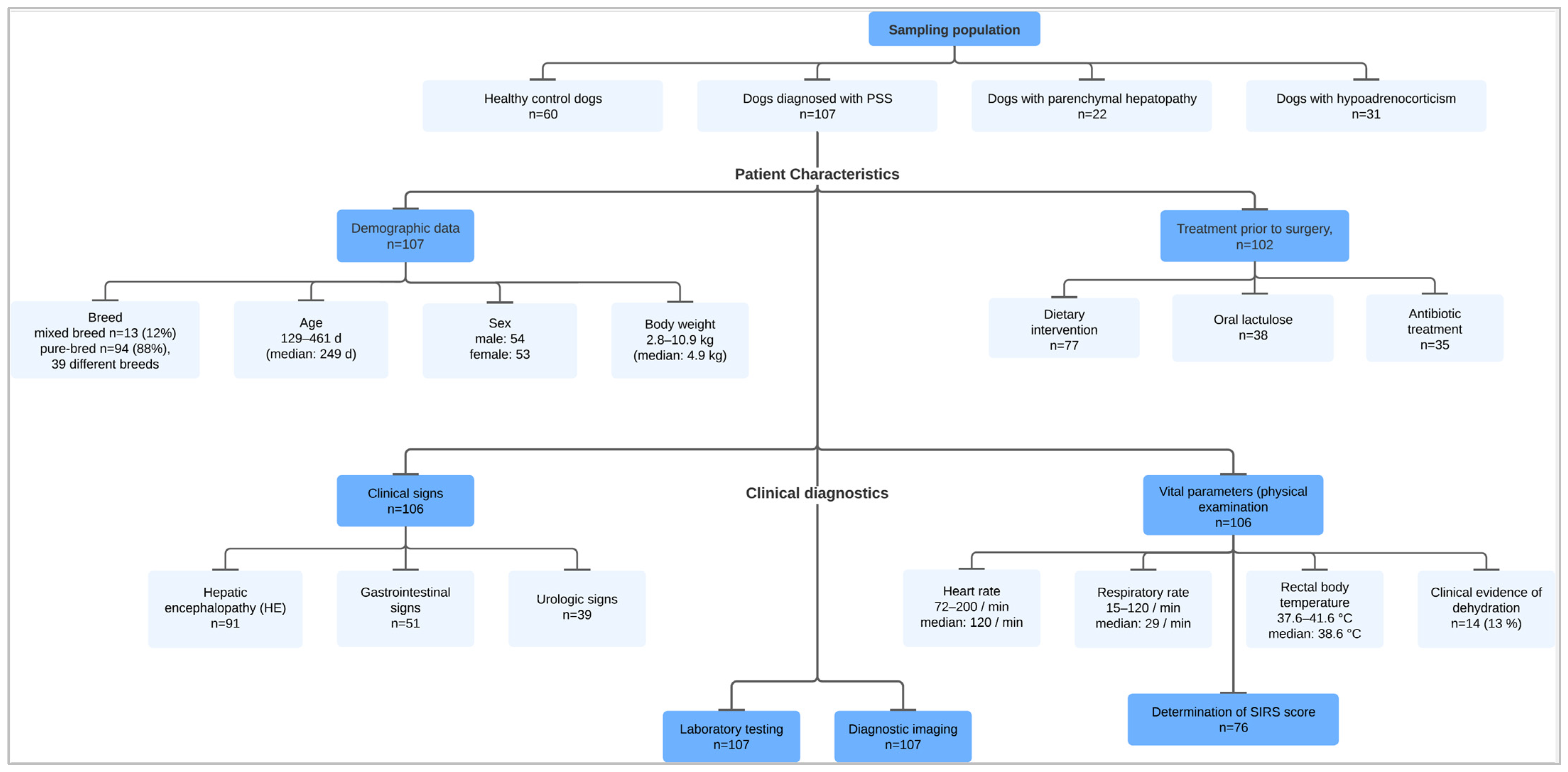
2.1. Sampling Population
2.2. Diagnostic Investigation
2.3. Statistical Analysis
3. Results
3.1. Patient Clinical Data
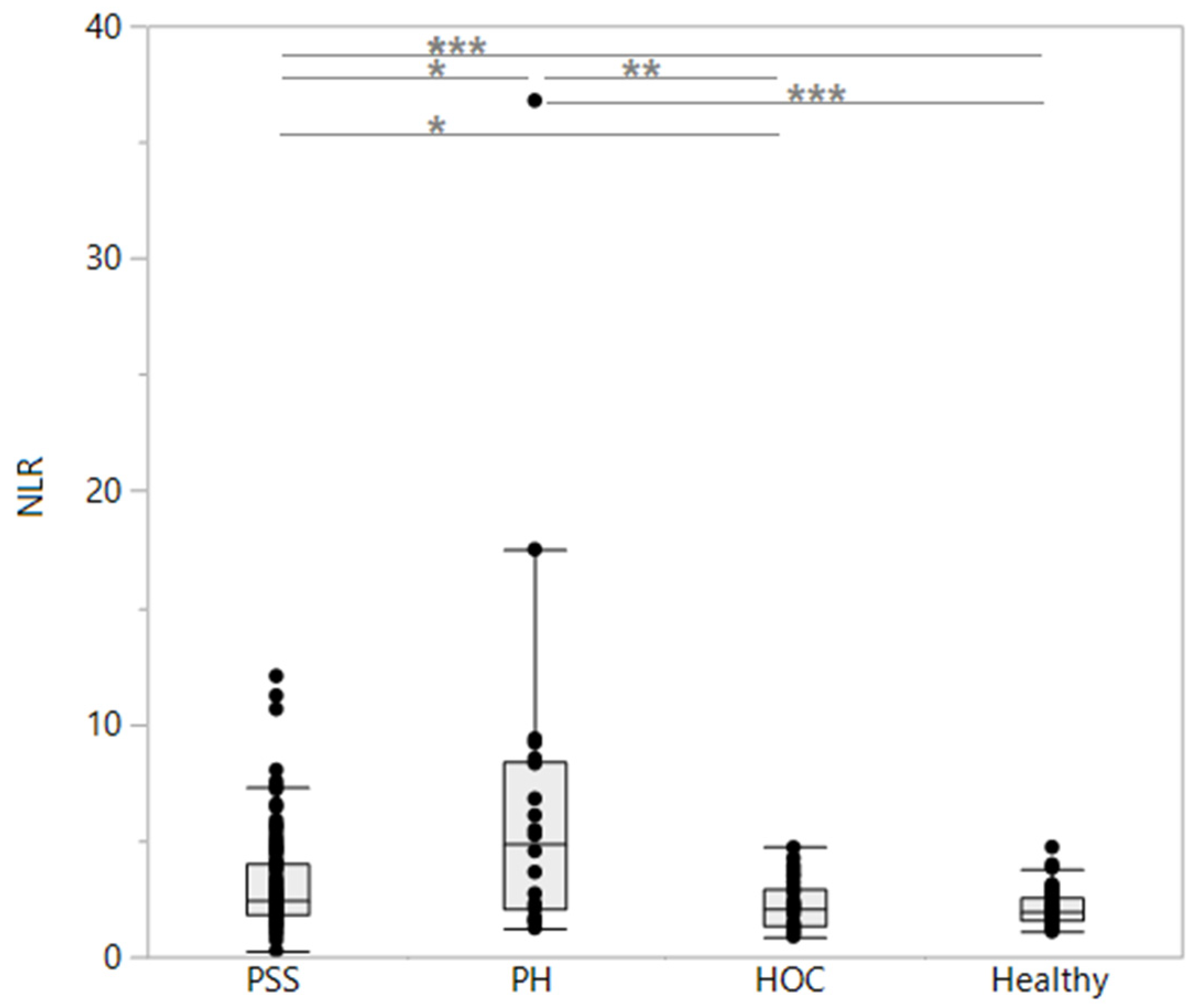
3.2. Comparison of Clinicopathologic Parameters between Groups
3.3. Association of Leukocyte Ratios with Patient and Clinicopathologic Parameters in PSS Dogs
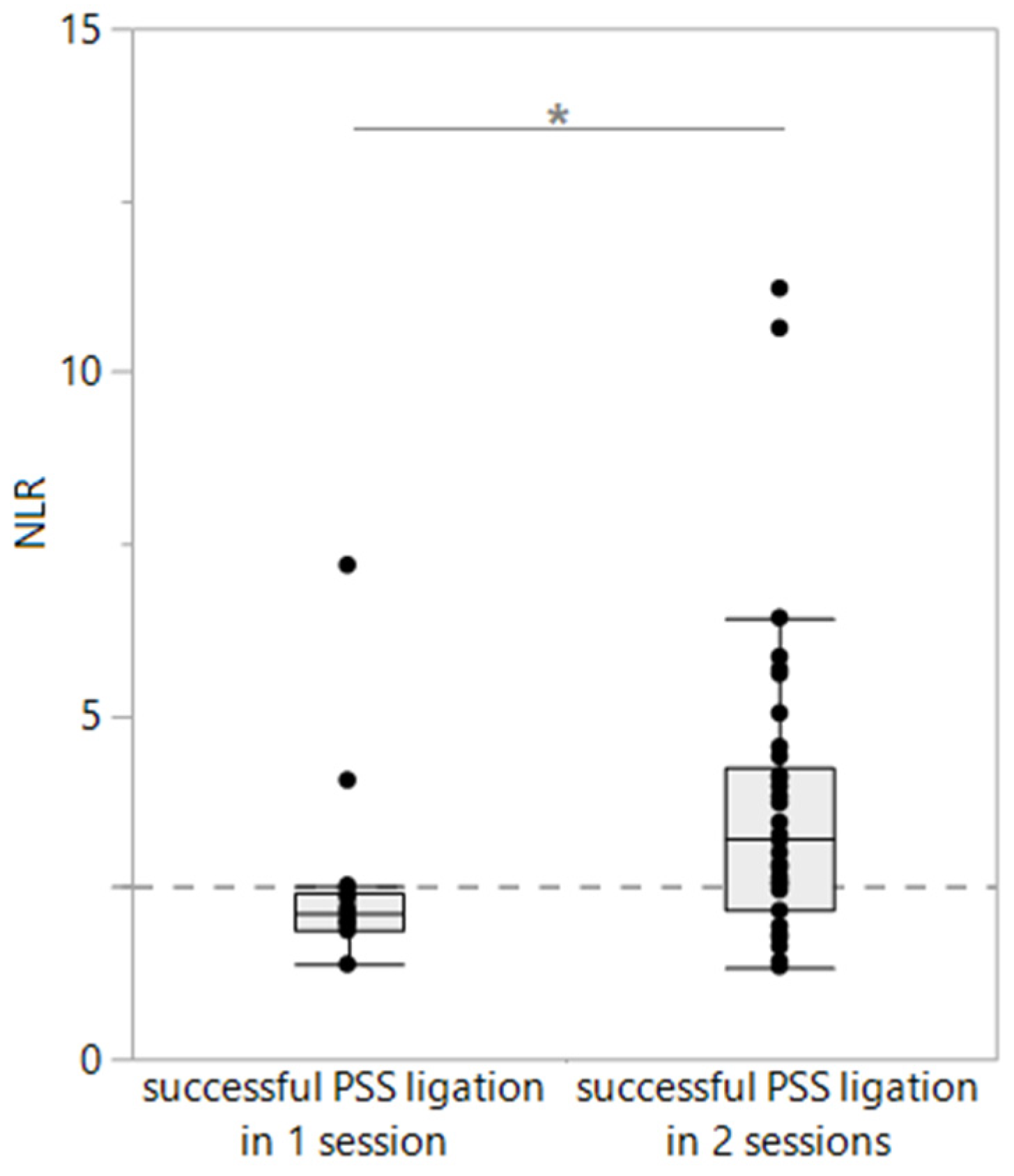
3.4. Association of Leukocyte Ratios with Histopathology, Treatment, and Surgical Outcomes in PSS Dogs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kiefer, I.; Bosch, B.; Köhler, C. Klinisches Bild und Diagnostik des angeborenen portosystemischen Shunts beim Hund. Kleintier. Konkret 2014, 16, 29–37. [Google Scholar] [CrossRef][Green Version]
- Van den Bossche, L.; van Steenbeek, F.G. Canine congenital portosystemic shunts: Disconnections dissected. Vet. J. 2016, 211, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Berent, A.C.; Tobias, K.M. Hepatic vascular anomalies. In Veterinary Surgery: Small Animal, 1st ed.; Johnston, S.A., Tobias, K.M., Eds.; Elsevier: St. Louis, MO, USA, 2018; pp. 1624–1658. [Google Scholar]
- Konstantinidis, A.O.; Patsikas, M.N.; Papazoglou, L.G.; Adamama-Moraitou, K.K. Congenital portosystemic shunts in dogs and cats: Classification, pathophysiology, clinical presentation and diagnosis. Vet. Sci. 2023, 10, 160. [Google Scholar] [CrossRef] [PubMed]
- Greenhalgh, S.N.; Reeve, J.A.; Johnstone, T.; Goodfellow, M.R.; Dunning, M.D.; O’Neill, E.J.; Hall, E.J.; Watson, P.J.; Jeffery, N.D. Long-term survival and quality of life in dogs with clinical signs associated with a congenital portosystemic shunt after surgical or medical treatment. J. Am. Vet. Med. Assoc. 2014, 245, 527–533. [Google Scholar] [CrossRef] [PubMed]
- Weisse, C.; Berent, A.C.; Todd, K.; Solomon, J.A.; Cope, C. Endovascular evaluation and treatment of intrahepatic portosystemic shunts in dogs: 100 cases (2001–2011). J. Am. Vet. Med. Assoc. 2014, 244, 78–94. [Google Scholar] [CrossRef]
- Parker, J.S.; Monnet, E.; Powers, B.E.; Twedt, D.C. Histologic examination of hepatic biopsy samples as a prognostic indicator in dogs undergoing surgical correction of congenital portosystemic shunts: 64 cases (1997–2005). J. Am. Vet. Assoc. 2008, 232, 1511–1514. [Google Scholar] [CrossRef] [PubMed]
- Toulza, O.; Center, S.A.; Brooks, M.B.; Erb, H.N.; Warner, K.L.; Deal, W. Evaluation of plasma protein C activity for detection of hepatobiliary disease and portosystemic shunting in dogs. J. Am. Vet. Med. Assoc. 2006, 229, 1761–1771. [Google Scholar] [CrossRef]
- Tivers, M.S.; Handel, I.; Gow, A.G.; Lipscomb, V.J.; Jalan, R.; Mellanby, R.J. Hyperammonemia and systemic inflammatory response syndrome predicts presence of hepatic encephalopathy in dogs with congenital portosystemic shunts. PLoS ONE 2014, 9, e82303. [Google Scholar] [CrossRef]
- Peng, Y.; Li, Y.; He, Y.; Wie, Q.; Xie, Q.; Zhang, L.; Xia, Y.; Zhou, X.; Zhang, L.; Feng, X.; et al. The role of neutrophil to lymphocyte ratio for the assessment of liver fibrosis and cirrhosis: A systematic review. Expert Rev. Gastroenterol. Hepatol. 2018, 12, 503–513. [Google Scholar] [CrossRef]
- Devriendt, N.; Serrano, G.; Paepe, D.; de Rooster, H. Liver function tests in dogs with congenital portosystemic shunts and their potential to determine persistent shunting after surgical attenuation. Vet. J. 2020, 261, 105478. [Google Scholar] [CrossRef]
- Huang, Z.; Fu, Z.; Huang, W.; Huang, K. Prognostic value of neutrophil-to-lymphocyte ratio in sepsis: A meta-analysis. Am. J. Emerg. Med. 2020, 38, 641–647. [Google Scholar] [CrossRef]
- Poordad, F.F. Review article: The burden of hepatic encephalopathy. Aliment. Pharmacol. Ther. 2007, 25 (Suppl. S1), 3–9. [Google Scholar] [CrossRef] [PubMed]
- Gow, A.G. Hepatic encephalopathy. Vet. Clin. N. Am. Small Anim. Pract. 2017, 47, 585–599. [Google Scholar] [CrossRef] [PubMed]
- Ong, J.P.; Aggarwal, A.; Krieger, D.; Easley, K.A.; Karafa, M.T.; Van Lente, F.; Arroliga, A.C.; Mullen, K.D. Correlation between ammonia levels and the severity of hepatic encephalopathy. Am. J. Med. 2003, 114, 188–193. [Google Scholar] [CrossRef] [PubMed]
- Serrano, G.; Devriendt, N.; De Rooster, H.; Paepe, D. Comparison of diet, lactulose, and metronidazole combination in the control of pre-surgical clinical signs in dogs with congenital extrahepatic portosystemic shunts. J. Vet. Intern. Med. 2022, 36, 1258–1266. [Google Scholar] [CrossRef] [PubMed]
- Ahn, J.O.; Li, Q.; Lee, Y.H.; Han, S.M.; Hwang, C.Y.; Youn, H.Y.; Chung, J.Y. Hyperammonemic hepatic encephalopathy management through L-ornithin-L-aspartate administration in dogs. J. Vet. Sci. 2016, 17, 431–433. [Google Scholar] [CrossRef] [PubMed]
- Singer, M.; Deutschmann, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef]
- Dupont, N.; Jessen, L.R.; Moberg, F.; Zyskind, N.; Lorentzen, C.; Reinhard Bjørnvad, C. A retrospective study of 237 dogs hospitalized with suspected acute hemorrhagic diarrhea syndrome: Disease severity, treatment, and outcome. J. Vet. Intern. Med. 2021, 35, 867–877. [Google Scholar] [CrossRef]
- Cavanaugh, M. AAHA/AAFP Fluid Therapy Guidelines for Dogs and Cats. Implementation Toolkit. 2013. Available online: https://www.aaha.org/globalassets/02-guidelines/fluid-therapy/fluidtherapy_guidlines_toolkit.pdf (accessed on 13 December 2023).
- Klein, S.C.; Peterson, M.E. Canine hypoadrenocorticism: Part I. Can. Vet. J 2010, 51, 63–69. [Google Scholar]
- Klein, S.C.; Peterson, M.E. Canine hypoadrenocorticism: Part II. Can. Vet. J 2010, 51, 179–184. [Google Scholar]
- Serrano, G.; Charalambous, M.; Devriendt, N.; De Rooster, H.; Mortier, F.; Paepe, D. Treatment of congenital extrahepatic portosystemic shunts in dogs: A systematic review and meta-analysis. J. Vet. Intern. Med. 2019, 33, 1865–1879. [Google Scholar] [CrossRef] [PubMed]
- Lidbury, J.A.; Rodrigues Hoffmann, A.; Ivanek, R.; Cullen, J.M.; Porter, B.F.; Oliveira, F.; Van Winkle, T.J.; Grinwis, G.C.; Sucholdolski, J.S.; Steiner, J.M. Interobserver agreement using histological scoring of the canine liver. J. Vet. Intern. Med. 2017, 31, 778–783. [Google Scholar] [CrossRef] [PubMed]
- Meyer, H.P.; Rothuizen, J. Increased free cortisol in plasma of dogs with portosystemic encephalopathy (PSE). Domest. Anim. Endocrinol. 1994, 11, 317–322. [Google Scholar] [CrossRef]
- Sterczer, A.; Meyer, H.P.; Van Sluijs, F.J.; Rothuizen, J. Fast resolution of hypercortisolism in dogs with portosystemic encephalopathy after surgical shunt closure. Res. Vet. Sci. 1999, 66, 63–67. [Google Scholar] [CrossRef]
- Baumstark, M.E.; Nussberger, J.; Boretti, F.S.; Baumstark, M.W.; Riond, B.; Reusch, C.E.; Sieber-Ruckstuhl, N.S. Use of plasma renin activity to monitor mineralocorticoid treatment in dogs with primary hypoadrenocorticism: Desoxycorticosterone versus fludrocortisone. J. Vet. Intern. Med. 2014, 28, 1471–1478. [Google Scholar] [CrossRef]
- Martin, L.G. Critical illness–related corticosteroid insufficiency in small animals. Vet. Clin. North Am. Small Anim. Pract. 2011, 41, 767–782. [Google Scholar] [CrossRef]
- Baade, S.; Aupperle, H.; Grevel, V.; Schoon, H.A. Histopathological and immunohistochemical investigations of hepatic lesions associated with congenital portosystemic shunt in dogs. J. Comp. Pathol. 2006, 134, 80–90. [Google Scholar] [CrossRef]
- Anglin, E.A.; Lux, C.N.; Sun, X.; Folk, C.A.; Fazio, C. Clinical characteristics of, prognostic factors for, and long-term outcome of dogs with multiple acquired portosystemic shunts: 72 cases (2000–2018). J. Am. Vet. Med. Assoc. 2021, 260 (Suppl. S1), S30–S39. [Google Scholar] [CrossRef] [PubMed]
- Mehl, M.L.; Kyles, A.E.; Hardie, E.M.; Kass, P.H.; Adin, C.A.; Flynn, A.K.; De Cock, H.E.; Gregory, C.R. Evaluation of ameroid ring constrictors for treatment for single extrahepatic portosystemic shunts in dogs: 168 cases (1995–2001). J. Am. Vet. Med. Assoc. 2005, 226, 2020–2030. [Google Scholar] [CrossRef]
- Falls, E.L.; Milovancev, M.; Hunt, G.B.; Daniel, L.; Mehl, M.L.; Schmiedt, C.W. Long-term outcome after surgical ameroid ring constrictor placement for treatment of single extrahepatic portosystemic shunts in dogs. Vet. Surg. 2013, 42, 951–957. [Google Scholar] [CrossRef]
- Zhu, H.; Bodenheimer, H.C.; Clain, D.J.; Min, A.D.M.; Theise, N.D. Hepatic lipogranulomas in patients with chronic liver disease: Association with hepatitis C and fatty liver disease. World J. Gastroenterol. 2010, 16, 5065–5069. [Google Scholar] [CrossRef] [PubMed]
- Van Blokland-Post, K.; Weber, M.F.; van Wolferen, M.E.; Penning, L.C.; Van Sluijs, F.J.; Kummeling, A. Prediction of outcome after ligation or thin film banding of extrahepatic shunts, based on plasma albumin concentration and hematologic expression of 8 target genes in 85 dogs. J. Vet. Intern. Med. 2023, 37, 537–549. [Google Scholar] [CrossRef] [PubMed]
- Sobczak-Filipiak, M.; Szarek, J.; Badurek, I.; Padmanabhan, J.; Trębacz, P.; Januchta-Kurmin, M.; Galanty, M. Retrospective liver histomorphological analysis in dogs in instances of clinical suspicion of congenital portosystemic shunt. J. Vet. Res. 2019, 63, 243–249. [Google Scholar] [CrossRef] [PubMed]
- De Graaf, E.D. Long-Term Outcome and Prognostic Indicators of Symptomatic Treatment in Dogs and Cats with CPSS: A Retrospective Study. Master’s Thesis, University of Utrecht, Utrecht, The Netherlands, 2015. [Google Scholar]
- Laflamme, D.P.; Mahaffey, E.A.; Allen, S.W.; Twedt, D.C.; Prasse, K.W.; Huber, T.L. Microcytosis and iron status in dogs with surgically induced portosystemic shunts. J. Vet. Intern. Med. 1994, 8, 212–216. [Google Scholar] [CrossRef] [PubMed]
- Bunch, S.E.; Jordan, H.L.; Sellon, R.K.; Cullen, J.M.; Smith, J.E. Characterization of iron status in young dogs with portosystemic shunt. Am. J. Vet. Res. 1995, 56, 853–858. [Google Scholar] [CrossRef] [PubMed]
- Aedh, A.I.; Khalil, M.S.; Abd-Elkader, A.S.; El-Khawanky, M.M.; Alshehri, H.M.; Hussein, A.; Lafi Alghamdi, A.A.; Hasan, A. Reticulocyte hemoglobin as a screening test for iron deficiency anemia: A new cut-off. Hematol. Rep. 2023, 15, 201–211. [Google Scholar] [CrossRef]
- Frowde, P.E.; Gow, A.G.; Burton, C.A.; Powell, R.; Lipscomb, V.J.; House, A.K.; Mellanby, R.J.; Tivers, M.S. Hepatic hepcidin gene expression in dogs with a congenital portosystemic shunt. J. Vet. Intern. Med. 2014, 28, 1203–1205. [Google Scholar] [CrossRef]
- Frymus, J.; Trębacz, P.; Galanty, M. Gastrointestinal ulceration in dogs with portosystemic shunt. Med. Wet. 2023, 79, 275–278. [Google Scholar] [CrossRef]
- Fuchs, J.; Moritz, A.; Grußendorf, E.; Lechner, J.; Neuerer, F.; Nickel, R.; Rieker, T.; Schwedes, C.; DeNicola, D.B.; Russell, J.; et al. Evaluation of reticulocyte hemoglobin content (RET-He) in the diagnosis of iron-deficient erythropoiesis in dogs. Vet. Clin. Pathol. 2017, 46, 558–568. [Google Scholar] [CrossRef]
- Weese, J.S.; Blondeau, J.M.; Boothe, D.; Breitschwerdt, E.B.; Guardabassi, L.; Hillier, A.; Lloyd, D.H.; Papich, M.G.; Rankin, S.C.; Turnidge, J.D.; et al. Antimicrobial use guidelines for treatment of urinary tract disease in dogs and cats: Antimicrobial guidelines working group of the international society for companion animal infectious diseases. Vet. Med. Int. 2011, 2011, 263768. [Google Scholar] [CrossRef]
- Caporali, E.H.G.; Phillips, H.; Underwood, L.; Selmic, L.E. Risk factors for urolithiasis in dogs with congenital extrahepatic portosystemic shunts: 95 cases (1999–2013). J. Am. Vet. Med. Assoc. 2015, 256, 530–536. [Google Scholar] [CrossRef] [PubMed]
- Burger, N.C.; Devriendt, N.; Serrano, G.; Stock, E.; de Rooster, H.; Paepe, D. Dogs with congenital extrahepatic portosystemic shunts that have persistent shunting after surgery have a higher prevalence of urolithiasis. J. Am. Vet. Med. Assoc. 2023, 261, 1337–1344. [Google Scholar] [CrossRef] [PubMed]
- McLauchlan, G.; McLaughlin, A.; Sewell, A.C.; Bell, R. Methylmalonic aciduria secondary to selective cobalamin malabsorption in a Yorkshire terrier. J. Am. Anim. Hosp. Assoc. 2015, 51, 285–288. [Google Scholar] [CrossRef] [PubMed]
- Kather, S.; Grützner, N.; Kook, P.H.; Dengler, F.; Heilmann, R.M. Review of cobalamin status and disorders of cobalamin metabolism in dogs. J. Vet. Intern. Med. 2020, 34, 13–28. [Google Scholar] [CrossRef]
- Rørtveit, R.; Sævik, B.K.; Eggertsdóttir, A.A.; Skancke, E.; Lingaas, F.; Thoresen, S.I.; Jansen, J.H. Age-related changes in hematologic and serum biochemical variables in dogs aged 16–60 days. Vet. Clin. Pathol. 2015, 44, 47–57. [Google Scholar] [CrossRef]
- Reagan, K.L.; Pires, J.; Quach, N.; Gilor, C. Evaluation of a machine learning tool to screen for hypoadrenocorticism in dogs presenting to a teaching hospital. J. Vet. Intern. Med. 2022, 36, 1942–1946. [Google Scholar] [CrossRef]
| Grade of HE | Clinical Signs |
|---|---|
| 0 | none (no clinical signs, unremarkable physical examination) |
| I | mildly decreased activity, lethargy, or both |
| II | severe lethargy, mild ataxia, or both |
| III | hypersalivation, severe ataxia, head pressing, blindness, circling, or a combination of these |
| IV | seizures and stupor or coma |
| SIRS Score (Out of 4) | Leukocyte Count | Suspected Band Neutrophils | Heart Rate | Respiratory Rate |
|---|---|---|---|---|
| 0 | 5.0–19.5 × 109/L | no | <140/min | <40/min |
| 1 | Fulfilling 1 of 4 criteria: tachycardia (>140/min), tachypnea (>40/min), hypothermia (<37.2 °C) or hyperthermia (>39.2 °C), leukocytosis (>19.5 × 109/L), or leukopenia (<5.0 × 109/L) | |||
| 2 | Fulfilling 2 of the 4 criteria | SIRS was defined to be present if at least 2 out of the 4 following criteria were fulfilled | ||
| 3 | Fulfilling 3 of the 4 criteria | |||
| 4 | Fulfilling all 4 criteria data | |||
| Patient Characteristic | PSS | PH | HOC | Controls | p |
|---|---|---|---|---|---|
| n | 107 | 22 | 31 | 60 | – |
| Patient characteristics | |||||
| Age in days | 249 (129–461) A | 2249 (978–4213) B | 1677 (1013–2433) B | 1551 (897–2449) B | <0.0001 |
| Age in years | 0.7 (0.4–1.3) A | 6.2 (2.7–11.5) B | 4.6 (2.8–6.7) B | 6.5 (4.2–6.7) B | |
| Male/female sex | 54 (50%)/53 (50%) | 8 (36%)/14 (64%) | 18 (58%)/13 (42%) | 34 (57%)/26 (43%) | 0.3539 |
| Body weight in kg | 4.9 (2.8–10.9) A | 12.2 (8.0–18.2) B | 20.3 (8.5–25.5) B | 29.8 (26.5–34.0) C | <0.0001 |
| Breed | 0.0003 | ||||
| - Purebred | 94 (88%) A | 13 (59%) B | 22 (71%) B | 37 (62%) B | |
| - Mixed breed | 13 (12%) | 9 (41%) | 9 (29%) | 23 (38%) | |
| Clinicopathologic parameters | |||||
| Leukogram | |||||
| Leukocyte count in ×109/L | 14.38 (10.97–19.16) A,* | 16.55 (9.36–24.23) A | 14.05 (10.97–17.71) A | 8.87 (7.26–10.48) B | <0.0001 |
| Neutrophil count in ×109/L | 8.50 (6.43–11.51) A | 11.94 (5.58–18.50) A | 8.03 (6.01–10.54) A | 4.78 (4.06–6.54) B | <0.0001 |
| Lymphocyte count in ×109/L | 3.28 (2.59–4.19) A | 2.24 (1.58–3.29) B | 3.74 (2.87–5.78) A | 2.53 (1.95–3.31) B | <0.0001 |
| Monocyte count in ×109/L | 1.37 (1.02–1.96) A | 1.10 (0.51–2.52) A | 0.67 (0.49–1.01) B | 0.51 (0.41–0.69) C | <0.0001 |
| Eosinophil count in ×109/L | 0.52 (0.34–0.93) A | 0.24 (0.09–0.47) B | 0.69 (0.41–1.10) A | 0.61 (0.44–0.84) A | <0.0001 |
| NLR | 2.45 (1.86–4.05) A | 4.88 (2.06–8.35) B | 2.10 (1.31–2.95) C | 1.99 (1.60–2.52) C | <0.0001 |
| NLR < 2.3 | 47 (44%) | 8 (36%) | 20 (65%) | 39 (65%) | 0.0113 |
| ELR × 102 | 17.26 (9.58–24.86) A | 11.61 (3.66–18.47) B | 19.42 (11.48–29.31) A | 24.01 (17.05–37.11) C | <0.0001 |
| ENR × 102 | 6.28 (3.45–10.69) A | 2.26 (0.64–7.24) B | 9.81 (6.13–12.43) C | 11.99 (9.37–15.49) D | <0.0001 |
| EMR × 102 | 45.59 (21.02–67.88)A | 18.62 (7.04–58.46) B | 97.62 (72.41–132.7) C | 116.59 (85.62–153.6) C | <0.0001 |
| Erythrogram | |||||
| Hematocrit in % | 36.6 (31.9–41.8) A,* | 43.2 (31.0–48.8) A,B | 43.8 (37.6–52.6) B,C | 47.2 (43.5–50.9) C | <0.0001 |
| MCV in fL | 56.5 (53.7–60.3) A | 64.3 (61.6–69.7) B | 62.1 (59.8–63.2) C | 65.5 (63.8–67.2) B,D | <0.0001 |
| MCH in pg | 19.8 (18.9–21.0) A | 22.3 (21.9–23.5) B | 23.0 (22.0–23.8) B,C | 23.3 (22.9–23.9) C | <0.0001 |
| MCHC in g/dL | 35.4 (34.2–36.4) A,* | 35.6 (34.2–36.3) A,B | 37.3 (36.0–38.3) C | 35.8 (35.2–36.3) B | <0.0001 |
| Retic-HgB in pg | 22.0 (21.0–24.8) A,$ | 23.6 (22.2–26.2) A,B,† | 25.4 (22.8–27.4) B,‡ | 27.2 (25.1–27.8) C,# | <0.0001 |
| PSS Group (n = 106) | PH Group (n = 21) | p | |||||
|---|---|---|---|---|---|---|---|
| Parameter | Meas | Median or n (%) | Range | Meas | Median or n (%) | Range | |
| Cardiac rate (/min) | 99 | 120 | 72–200 | 21 | 120 | 78–168 | 0.8350 |
| Respiratory rate (/min) | 79 | 29 | 15–120 | 15 | 32 | 18–52 | 0.4338 |
| Clinical evidence of dehydration | 105 | 14 (13%) | – | 20 | 6 (30%) | – | 0.3136 |
| Rectal body temperature (°C) | 85 | 38.6 | 37.6–41.6 | 15 | 38.5 | 38.1–40.0 | 0.5706 |
| Increased body temperature | 85 | 3 (4%) | – | 15 | 2 (13%) | – | 0.1609 |
| Suspected band neutrophils | 103 | 10 (10%) | – | 15 | 5 (33%) | – | 0.0232 |
| SIRS score | |||||||
| including hypoglycemia | 76 | 0 | 0–3 | 13 | 0 | 0–4 | 0.8475 |
| not including hypoglycemia | 76 | 0 | 0–4 | 13 | 0 | 0–4 | 0.5356 |
| Pre-prandial serum bile acid concentration (µmol/L) | 87 | 73.2 | 0.2–527.1 | 6 | 71.1 | 4.2–167.1 | 0.4206 |
| Post-prandial serum bile acid concentration (µmol/L) | 70 | 134.1 | 20.8–580.0 | 3 | 80.5 | 8.0–120.4 | 0.0469 |
| Difference in post- vs. pre-prandial serum bile acids | 69 | 46.5 | −159–352.8 | 3 | 5.0 | 3.4–53.7 | 0.3979 |
| PSS Group (n = 106) | PH Group (n = 21) | HOC Group (n = 31) | p | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Serum Parameter | n | Median | Range | n | Median | Range | n | Median | Range | |
| BUN (mmol/L) | 102 | 2.7 | 0.8–21.2 | 18 | 5.7 | 1.8–21.0 | 31 | 21.5 | 6.2–72.8 | <0.0001 |
| Albumin (g/L) | 107 | 26 | 10– 36 | 22 | 31 | 16–45 | 30 | 32.5 | 22–48 | <0.0001 |
| Total protein (g/L) | 104 | 52 | 30–69 | 21 | 62 | 41–96 | 31 | 66 | 34–84 | <0.0001 |
| Cholesterol (mmol/L) | 48 | 3.53 | 1.12–9.93 | 14 | 7.36 | 0.98–12.0 | 14 | 4.44 | 1.97–10.53 | 0.0057 |
| Glucose (mmol/L) | 106 | 5.6 | 2.8–9.2 | 18 | 5.5 | 3.7–56.0 | 31 | 5.3 | 0.9–44.8 | 0.4256 |
| Bilirubin (µmol/L) | 54 | 3 | 0.1–27 | 17 | 6.7 | 0.2–588.4 | 14 | 5.0 | 0.1–94.0 | 0.0193 |
| Ammonia (µmol/L) | 104 | 165 | 15–677 | 12 | 58 | 11–134 | 10 | 38 | 10–70 | <0.0001 |
| ALT activity (U/L) | 101 | 161 | 16–2091 | 101 | 258 | 68–1808 | 30 | 59 | 24–286 | <0.0001 |
| ALP activity (U/L) | 103 | 242 | 1–7955 | 21 | 278 | 36–2270 | 30 | 34 | 7–107 | <0.0001 |
| γGT activity (U/L) | 39 | 6 | 2–21 | 8 | 18 | 0–115 | 13 | 5 | 1–99 | 0.0471 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Becher, A.; Acke, E.; Serrano, G.; Kiefer, I.; Alef, M.; von Bomhard, W.; Heilmann, R.M. Evaluation of the Blood Neutrophil-to-Lymphocyte Ratio (NLR) as a Diagnostic and Prognostic Biomarker in Dogs with Portosystemic Shunt. Vet. Sci. 2024, 11, 80. https://doi.org/10.3390/vetsci11020080
Becher A, Acke E, Serrano G, Kiefer I, Alef M, von Bomhard W, Heilmann RM. Evaluation of the Blood Neutrophil-to-Lymphocyte Ratio (NLR) as a Diagnostic and Prognostic Biomarker in Dogs with Portosystemic Shunt. Veterinary Sciences. 2024; 11(2):80. https://doi.org/10.3390/vetsci11020080
Chicago/Turabian StyleBecher, Anja, Els Acke, Gonçalo Serrano, Ingmar Kiefer, Michaele Alef, Wolf von Bomhard, and Romy M. Heilmann. 2024. "Evaluation of the Blood Neutrophil-to-Lymphocyte Ratio (NLR) as a Diagnostic and Prognostic Biomarker in Dogs with Portosystemic Shunt" Veterinary Sciences 11, no. 2: 80. https://doi.org/10.3390/vetsci11020080
APA StyleBecher, A., Acke, E., Serrano, G., Kiefer, I., Alef, M., von Bomhard, W., & Heilmann, R. M. (2024). Evaluation of the Blood Neutrophil-to-Lymphocyte Ratio (NLR) as a Diagnostic and Prognostic Biomarker in Dogs with Portosystemic Shunt. Veterinary Sciences, 11(2), 80. https://doi.org/10.3390/vetsci11020080








