Refinements in Clinical and Behavioral Management for Macaques on Infectious Disease Protocols
Abstract
Simple Summary
Abstract
1. Introduction
2. Social Housing
2.1. Pair Housing Macaques with SIV
2.2. Socialization of Infants
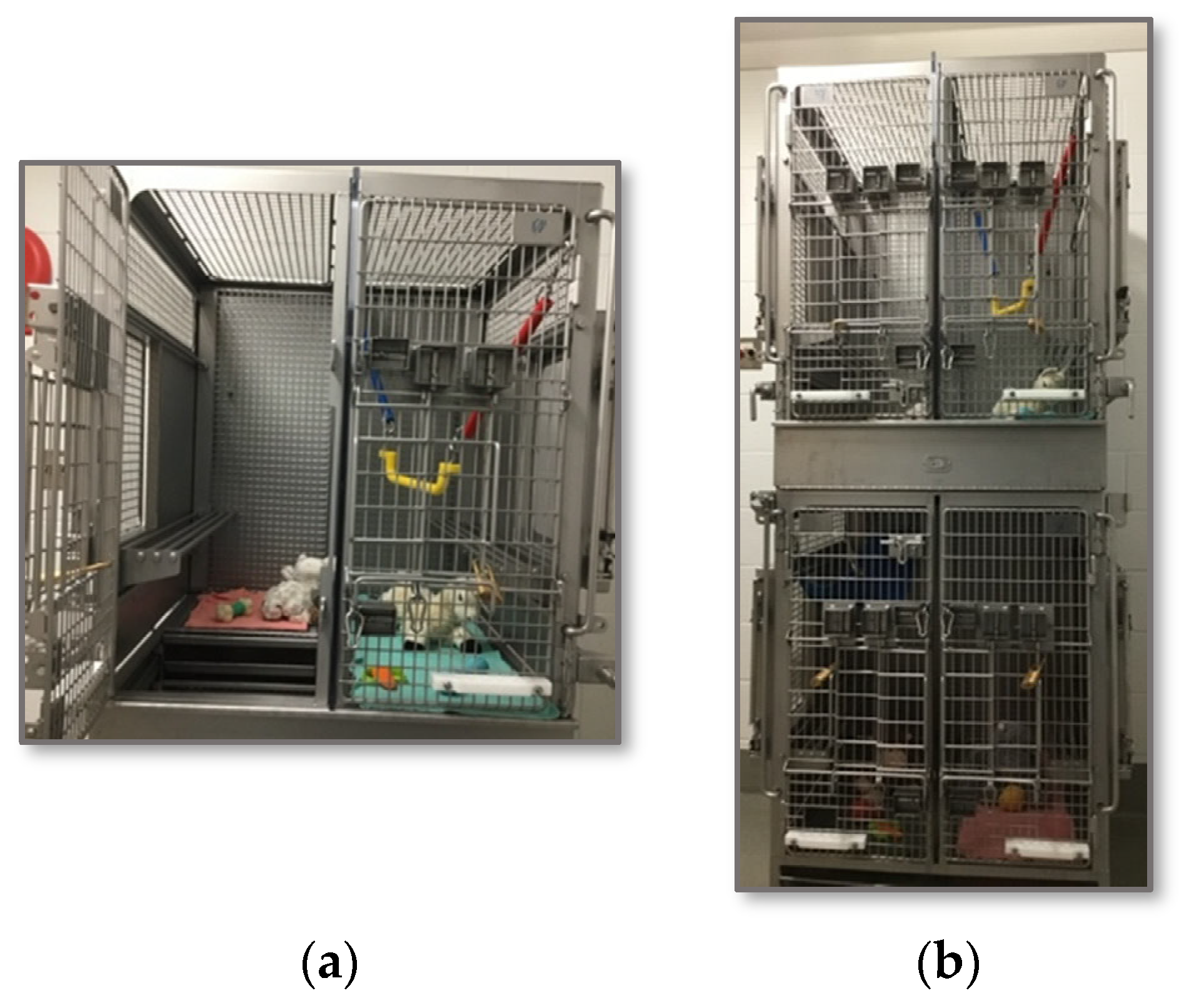
2.3. Instrumented Animals
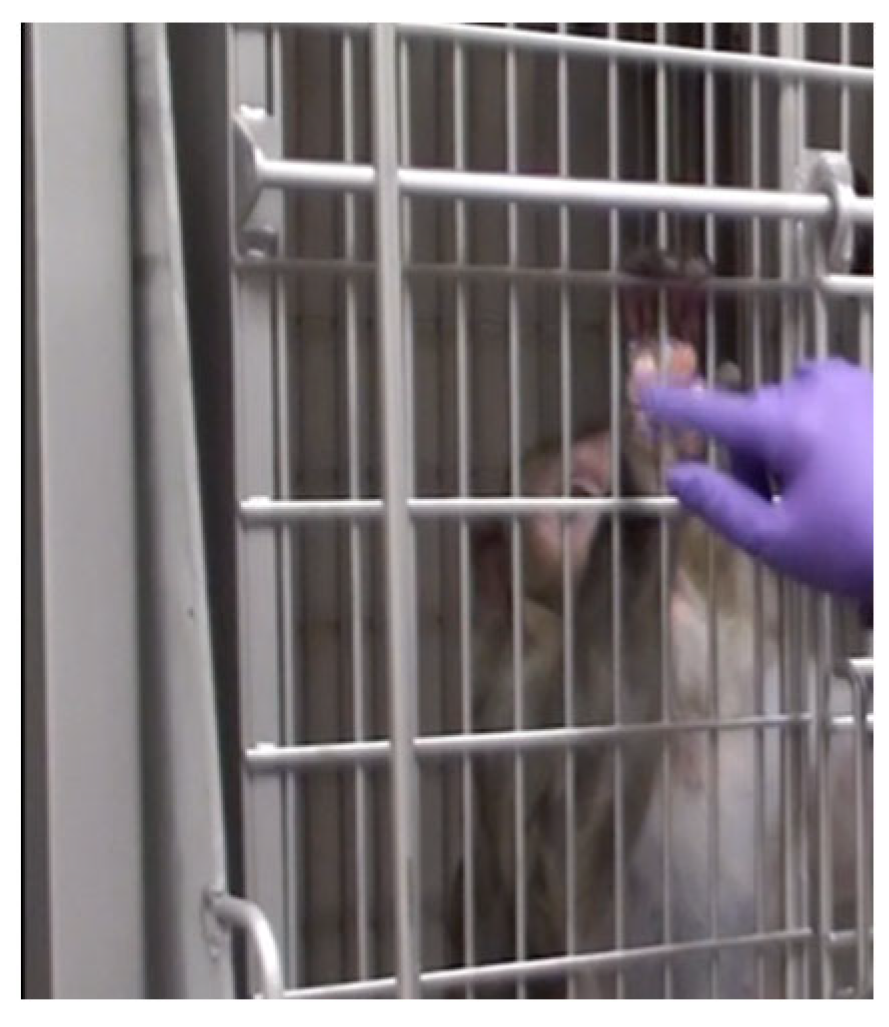
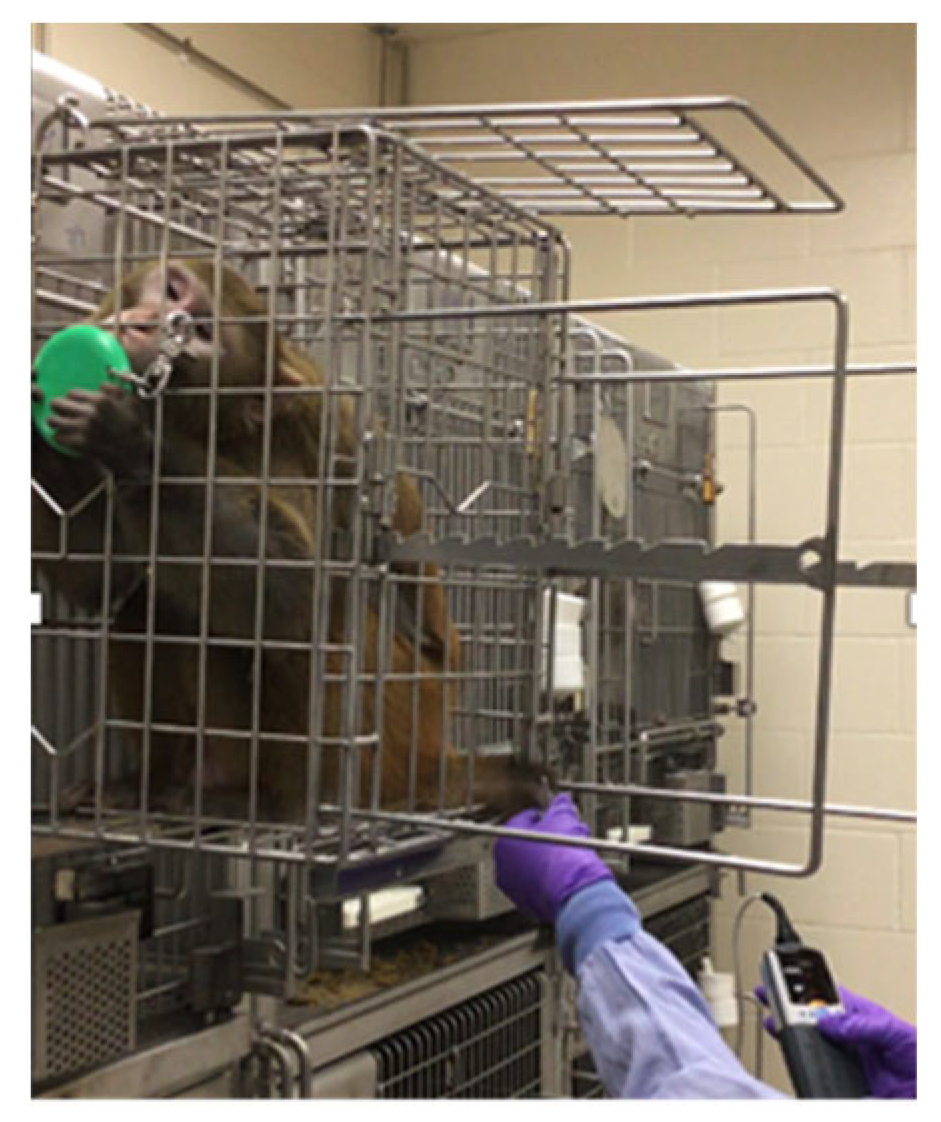
3. Positive Reinforcement Training
4. Animal Assessments
5. Discussion
6. Conclusions
7. Future Directions
7.1. Increased Socialization
7.2. Awake Blood Draws
7.3. Long-Lasting ART
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Estes, J.D.; Wong, S.W.; Brenchley, J.M. Nonhuman primate models of human viral infections. Nat. Rev. Immunol. 2018, 18, 390–404. [Google Scholar] [CrossRef] [PubMed]
- Van Rompay, K. Tackling HIV and AIDS: Contributions by non-human primate models. Lab. Anim. 2017, 46, 259–270. [Google Scholar] [CrossRef] [PubMed]
- Friedman, H.; Ator, N.; Haigwood, N.; Newsome, W.; Allan, J.S.; Golos, T.G.; Kordower, J.H.; Shade, R.E.; Goldberg, M.E.; Bailey, M.R.; et al. The critical role of nonhuman primates in medical research. Pathog. Immun. 2017, 2, 352–365. [Google Scholar] [CrossRef] [PubMed]
- Andrade, M.C.R.; Lemos, B.R.P.; Silva, L.M.; Pecotte, J.K. Eliminating potential effects of other infections during selection of nonhuman primates for COVID-19 research. Comp. Med. 2023, 73, 45–57. [Google Scholar] [CrossRef] [PubMed]
- Kaushal, D.; Mehra, S.; Didier, P.J.; Lackner, A.A. The non-human primate model of tuberculosis. J. Med. Primatol. 2012, 41, 191–201. [Google Scholar] [CrossRef]
- Mohr, E.L. Modeling zika virus-associated birth defects in nonhuman primates. J. Pediatric Infect. Dis. Soc. 2018, 7 (Suppl. S2), S60–S66. [Google Scholar] [CrossRef]
- Wei, Z.K.; Zhao, Y.C.; Wang, Z.D.; Sui, L.Y.; Zhao, Y.H.; Liu, Q. Animal models of mpox virus infection and disease. Infect. Med. 2023, 2, 153–166. [Google Scholar] [CrossRef]
- Hannibal, D.L.; Bliss-Moreau, E.; Vandeleest, J.; McCowan, B.; Capitanio, J. Laboratory rhesus macaque social housing and social changes: Implications for research. Am. J. Primatol. 2017, 79, e22528. [Google Scholar] [CrossRef]
- Rogers, C.J.; Brissette-Storkus, C.S.; Chambers, W.H.; Cameron, J.L. Acute stress impairs NK cell adhesion and cytotoxicity through CD2, but not LFA-1. J. Neuroimmunol. 1999, 99, 230–241. [Google Scholar] [CrossRef]
- Bethea, C.L.; Centeno, M.L.; Cameron, J.L. Neurobiology of stress-induced reproductive dysfunction in female macaques. Mol. Neurobiol. 2008, 38, 199–230. [Google Scholar] [CrossRef]
- Meaney, M.J.; Viau, V.; Bhatnagar, S.; Betito, K.; Iny, L.J.; O’Donnell, D.; Mitchell, J.B. Cellular mechanisms underlying the development and expression of individual differences in the hypothalamic-pituitary-adrenal stress response. J. Steroid Biochem. Mol. Biol. 1991, 39, 265–274. [Google Scholar] [CrossRef] [PubMed]
- De Kloet, E.R. Hormones and the stressed brain. Ann. N. Y. Acad. Sci. 2004, 1018, 1–15. [Google Scholar] [CrossRef]
- Bartolomucci, A.; Palanza, P.; Sacerdote, P.; Panerai, A.E.; Sgoifo, A.; Dantzer, R.; Parmigiani, S. Social factors and individual vulnerability to chronic stress exposure. Neurosci. Biobehav. Rev. 2005, 29, 67–81. [Google Scholar] [CrossRef] [PubMed]
- Weed, J.L.; Raber, J.M. Balancing animal research with animal well-being: Establishment of goals and harmonization of approaches. ILAR J. 2005, 46, 118–128. [Google Scholar] [CrossRef]
- Schapiro, S.J.; Hau, J. Research benefits of improving welfare in captive primates. In Nonhuman Primate Welfare; Robinson, L.W., Weiss, A., Eds.; Springer: Cham, Switzerland, 2023; pp. 445–462. [Google Scholar]
- Russell, W.M.S.; Burch, R.L. The Principles of Humane Experimental Technique; Methuen: London, UK, 1959. [Google Scholar]
- DiVincenti, L., Jr.; Wyatt, J.D. Pair housing of macaques in research facilities: A science-based review of benefits and risks. J. Am. Assoc. Lab. Anim. Sci. 2011, 50, 856–863. [Google Scholar]
- Truelove, M.A.; Martin, A.L.; Perlman, J.E.; Wood, J.S.; Bloomsmith, M.A. Pair housing of macaques: A review of partner selection, introduction techniques, monitoring for compatibility, and methods for long-term maintenance of pairs. Am. J. Primatol. 2017, 79, e22485. [Google Scholar] [CrossRef]
- Gottlieb, D.H.; Capitanio, J.P.; McCowan, B. Risk factors for stereotypic behavior and self-biting in rhesus macaques (Macaca mulatta): Animal’s history, current environment, and personality. Am. J. Primatol. 2013, 75, 995–1008. [Google Scholar] [CrossRef] [PubMed]
- Gottlieb, D.H.; Maier, A.; Coleman, K. Evaluation of environmental and intrinsic factors that contribute to stereotypic behavior in captive rhesus macaques (Macaca mulatta). Appl. Anim. Behav. Sci. 2015, 171, 184–191. [Google Scholar] [CrossRef]
- Bellanca, R.U.; Crockett, C.M. Factors predicting increased incidence of abnormal behavior in male pigtailed macaques. Am. J. Primatol. 2002, 58, 57–69. [Google Scholar] [CrossRef]
- Eaton, G.G.; Kelley Stephen, T.; Axthelm Michael, K.; Iliff-Sizemore Susan, A.; Shigi Stanley, M. Psychological well-being in paired adult female rhesus (Macaca mulatta). Am. J. Primatol. 1994, 33, 89–99. [Google Scholar] [CrossRef]
- Reinhardt, V. Pair-housing overcomes self-biting behavior in macaques. Lab. Prim. Newsl. 1999, 38, 4–5. [Google Scholar]
- Reinhardt, V.; Cowley, D.; Eisele, S. Serum cortisol concentrations of single-housed and isosexually pair-housed adult rhesus macaques. J. Experl Anim. Sci. 1991, 34, 73–76. [Google Scholar]
- Schapiro, S.J.; Nehete, P.N.; Perlman, J.E.; Sastry, K.J. A comparison of cell-mediated immune responses in rhesus macaques housed singly, in pairs, or in groups. Appl. Anim. Behav. Sci. 2000, 68, 67–84. [Google Scholar] [CrossRef]
- Gilbert, M.H.; Baker, K.C. Social buffering in adult male rhesus macaques (Macaca mulatta): Effects of stressful events in single vs. pair housing. J. Med. Primatol. 2011, 40, 71–78. [Google Scholar] [CrossRef]
- Coleman, K.; Stull, C. Pair housing mitigates against effects of construction noise in caged rhesus macaques (Macaca mulatta) in the laboratory environment. Am. J. Primatol. 2020, 82 (Suppl. S1), 69. [Google Scholar]
- Guerrero-Martin, S.M.; Rubin, L.H.; McGee, K.M.; Shirk, E.N.; Queen, S.E.; Li, M.; Bullock, B.; Carlson, B.W.; Adams, R.J.; Gama, L.; et al. Psychosocial stress alters the immune response and results in higher viral load during acute simian immunodeficiency virus infection in a pigtailed macaque model of human immunodeficiency virus. J. Infect. Dis. 2021, 224, 2113–2121. [Google Scholar] [CrossRef]
- Castell, N.; Guerrero-Martin, S.M.; Rubin, L.H.; Shirk, E.N.; Brockhurst, J.K.; Lyons, C.E.; Najarro, K.M.; Queen, S.E.; Carlson, B.W.; Adams, R.J.; et al. Effect of single housing on innate immune activation in immunodeficiency virus-infected pigtail macaques (Macaca nemestrina) as a model of psychosocial stress in acute hiv infection. Psychosom. Med. 2022, 84, 966–975. [Google Scholar] [CrossRef] [PubMed]
- Pahar, B.; Baker, K.C.; Jay, A.N.; Russell-Lodrigue, K.E.; Srivastav, S.K.; Aye, P.P.; Blanchard, J.L.; Bohm, R.P. Effects of social housing changes on immunity and vaccine-specific immune responses in adolescent male rhesus macaques. Front. Immunol. 2020, 11, 565746. [Google Scholar] [CrossRef]
- MacAllister, R.P.; Heagerty, A.; Coleman, K. Behavioral predictors of pairing success in rhesus macaques (Macaca mulatta). Am. J. Primatol. 2020, 82, e23081. [Google Scholar] [CrossRef]
- Rommeck, I.; Gottlieb, D.H.; Strand, S.C.; McCowan, B. The effects of four nursery rearing strategies on infant behavioral development in rhesus macaques (Macaca mulatta). J. Am. Assoc. Lab. Anim. Sci. 2009, 48, 395–401. [Google Scholar]
- Roberts, S.J.; Platt, M.L. Effects of isosexual pair-housing on biomedical implants and study participation in male macaques. Contemp. Top. Lab. Anim. Sci. 2005, 44, 13–18. [Google Scholar] [PubMed]
- Oppler, S.H.; Palmer, S.D.; Phu, S.N.; Graham, M.L. The role of behavioral management in enhancing clinical care and efficiency, minimizing social disruption, and promoting welfare in captive primates. Vet. Sci. 2024, in press.
- Graham, M.L.; Rieke, E.F.; Mutch, L.A.; Zolondek, E.K.; Faig, A.W.; Dufour, T.A.; Munson, J.W.; Kittredge, J.A.; Schuurman, H.J. Successful implementation of cooperative handling eliminates the need for restraint in a complex non-human primate disease model. J. Med. Primatol. 2012, 41, 89–106. [Google Scholar] [CrossRef] [PubMed]
- Burwitz, B.J.; Wu, H.L.; Abdulhaqq, S.; Shriver-Munsch, C.; Swanson, T.; Legasse, A.W.; Hammond, K.B.; Junell, S.L.; Reed, J.S.; Bimber, B.N.; et al. Allogeneic stem cell transplantation in fully MHC-matched Mauritian cynomolgus macaques recapitulates diverse human clinical outcomes. Nat. Commun. 2017, 8, 1418. [Google Scholar] [CrossRef]
- Hütter, G. Stem cell transplantation in strategies for curing HIV/AIDS. AIDS Res. Ther. 2016, 13, 31. [Google Scholar] [CrossRef]
- Shelton, J.; Stanton, J.; Price, H.M.; Wu, H.L.; Sacha, J.B.; Coleman, K. Pair-housing macaques with chronic catheters. In Proceedings of the AALAS, Denver, CO, USA, 13–17 October 2019. [Google Scholar]
- Skinner, B.F. The Behavior of Organisms; Appleton-Century-Crofts: New York, NY, USA, 1938. [Google Scholar]
- Pryor, K. Don’t Shoot the Dog: The New Art of Teaching and Training; Simon & Schuster: New York, NY, USA, 1999; p. 202. [Google Scholar]
- Laule, G.E.; Bloomsmith, M.A.; Schapiro, S.J. The use of positive reinforcement training techniques to enhance the care, management, and welfare of primates in the laboratory. J. Appl. Anim. Welf. Sci. 2003, 6, 163–173. [Google Scholar] [CrossRef]
- Schapiro, S.J.; Bloomsmith, M.A.; Laule, G.E. Positive reinforcement training as a technique to alter nonhuman primate behavior: Quantitative assessments of effectiveness. J. Appl. Anim. Welf. Sci. 2003, 6, 175–187. [Google Scholar] [CrossRef] [PubMed]
- Schapiro, S.J.; Perlman, J.E.; Thiele, E.; Lambeth, S. Training nonhuman primates to perform behaviors useful in biomedical research. Lab. Anim. 2005, 34, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Prescott, M.J.; Bowell, V.A.; Buchanan-Smith, H.M. Training of laboratory-housed non-human primates, part 2: Resources for developing and implementing training programmes. Anim. Tech. Welf. 2005, 4, 133–148. [Google Scholar]
- McKinley, J.; Buchanan-Smith, H.M.; Bassett, L.; Morris, K. Training common marmosets (Callithrix jacchus) to cooperate during routine laboratory procedures: Ease of training and time investment. J. Appl. Anim. Welf. Sci. 2003, 6, 209–220. [Google Scholar] [CrossRef]
- Coleman, K.; Pranger, L.; Maier, A.; Lambeth, S.P.; Perlman, J.E.; Thiele, E.; Schapiro, S.J. Training rhesus macaques for venipuncture using positive reinforcement techniques: A comparison with chimpanzees. J. Am. Assoc. Lab. Anim. Sci. 2008, 47, 37–41. [Google Scholar]
- Veeder, C.L.; Bloomsmith, M.A.; McMillan, J.L.; Perlman, J.E.; Martin, A.L. Positive reinforcement training to enhance the voluntary movement of group-housed sooty mangabeys (Cercocebus atys atys). J. Am. Assoc. Lab. Anim. Sci. 2009, 48, 192–195. [Google Scholar] [PubMed]
- Priest, G.M. Training a diabetic drill (Mandrillus leucophaeus) to accept insulin injections and venipuncture. Lab. Prim. Newsl. 1991, 30, 1–4. [Google Scholar]
- Klaiber-Schuh, A.; Welker, C. Crab-eating monkeys can be trained to cooperate in non-invasive oral medication without stress. Primate Rep. 1997, 47, 11–30. [Google Scholar]
- Laule, G.E.; Thurston, R.H.; Alford, P.L.; Bloomsmith, M.A. Training to reliably obtain blood and urine samples from a young, diabetic chimpanzee (Pan troglodytes). Zoo. Biol. 1996, 15, 587–591. [Google Scholar] [CrossRef]
- Bassett, L.; Buchanan-Smith, H.M.; McKinley, J.; Smith, T.E. Effects of training on stress-related behavior of the common marmoset (Callithrix jacchus) in relation to coping with routine husbandry procedures. J. Appl. Anim. Welf. Sci. 2003, 6, 221–233. [Google Scholar] [CrossRef]
- Coleman, K.; Maier, A. The use of positive reinforcement training to reduce stereotypic behavior in rhesus macaques. Appl. Anim. Behav. Sci. 2010, 124, 142–148. [Google Scholar] [CrossRef]
- Adams, K.M.; Navarro, A.M.; Hutchinson, E.K.; Weed, J.L. A canine socialization and training program at the National Institutes of Health. Lab. Anim. 2004, 33, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Guerrero-Martin, S.M.; Shirk, E.N.; Queen, S.E.; Li, M.; Carlson, B.W.; Brill, S.; Graham, M.L.; Hopper, L.M.; Bullock, B.; Adams, R.J.; et al. Positive reinforcement training may influence the acute immune response to SIV-infection in socially housed, laboratory pigtailed macaques (Macaca nemestrina) and rhesus macaques (Macaca mulatta). Am. J. Primatol. 2023, 85, 20. [Google Scholar]
- Reinhardt, V. Refining the traditional housing and handling of laboratory rhesus macaques improves scientific methodology. Primate Rep. 1997, 49, 93–112. [Google Scholar]
- Manciocco, A.; Chiarotti, F.; Vitale, A. Effects of positive interaction with caretakers on the behaviour of socially housed common marmosets (Callithrix jacchus). Appl. Anim. Behav. Sci. 2009, 120, 100–107. [Google Scholar] [CrossRef]
- Waitt, C.; Buchanan-Smith, H.M.; Morris, K. The effects of caretaker-primate relationships on primates in the laboratory. J. Appl. Anim. Welf. Sci. 2002, 5, 309–319. [Google Scholar] [CrossRef]
- Baker, K. Benefits of positive human interaction for socially housed chimpanzees. Anim. Welf. 2004, 13, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Rennie, A.; Buchanan-Smith, H. Refinement of the use of non-human primates in scientific research. Part 1: The influence of humans. Anim. Welf. 2006, 15, 203–213. [Google Scholar] [CrossRef]
- Coleman, K.; Heagerty, A. Human-animal interactions in the research environment. In Anthrozoology: Human-Animal Interactions in Domesticated and Wild Animals; Hosey, G., Melfi, V., Eds.; Oxford University Press: Oxford, UK, 2019; pp. 59–80. [Google Scholar]
- Coleman, K. Individual differences in temperament and behavioral management. In Handbook of Primate Behavioral Management; Schapiro, S.J., Ed.; Springer: Boca Raton, FL, USA, 2017; pp. 95–114. [Google Scholar]
- Capitanio, J.P. Variation in biobehavioral organization. In Handbook of Primate Behavioral Management; Schapiro, S.J., Ed.; CRC Press: Boca Raton, FL, USA, 2017; pp. 55–74. [Google Scholar]
- Coleman, K.; Tully, L.A.; McMillan, J.L. Temperament correlates with training success in adult rhesus macaques. Am. J. Primatol. 2005, 65, 63–71. [Google Scholar] [CrossRef]
- National Resource Council. The Psychological Well-Being of Nonhuman Primates; National Academy Press: Washington, DC, USA, 1998; p. 168. [Google Scholar]
- Witham, C.L. Automated face recognition of rhesus macaques. J. Neurosci. Methods 2018, 300, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Crockett, C.M.; Shimoji, M.; Bowden, D.M. Behavior, appetite, and urinary cortisol responses by adult female pigtailed macaques to cage size, cage level, room change, and ketamine sedation. Am. J. Primatol. 2000, 52, 63–80. [Google Scholar] [CrossRef] [PubMed]
- Hotchkiss, C.E.; Young, M.A. Comparative Risk of Human Injury/Exposure While Collecting Blood from Sedated and Unsedated Nonhuman Primates. J. Am. Assoc. Lab. Anim. Sci. 2020, 59, 371–376. [Google Scholar] [CrossRef] [PubMed]
- Masters, M.C.; Krueger, K.M.; Williams, J.L.; Morrison, L.; Cohn, S.E. Beyond one pill, once daily: Current challenges of antiretroviral therapy management in the United States. Expert. Rev. Clin. Pharmacol. 2019, 12, 1129–1143. [Google Scholar] [CrossRef]
- Daly, M.B.; Clayton, A.M.; Ruone, S.; Mitchell, J.; Dinh, C.; Holder, A.; Jolly, J.; Garcia-Lerma, J.G.; Weed, J.L. Training rhesus macaques to take daily oral antiretroviral therapy for preclinical evaluation of HIV prevention and treatment strategies. PLoS ONE 2019, 14, e0225146. [Google Scholar] [CrossRef]
- Venkatesan, P. Long-acting injectable ART for HIV: A (cautious) step forward. Lancet Microbe 2022, 3, e94. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martin, L.D.; Shelton, J.; Houser, L.A.; MacAllister, R.; Coleman, K. Refinements in Clinical and Behavioral Management for Macaques on Infectious Disease Protocols. Vet. Sci. 2024, 11, 460. https://doi.org/10.3390/vetsci11100460
Martin LD, Shelton J, Houser LA, MacAllister R, Coleman K. Refinements in Clinical and Behavioral Management for Macaques on Infectious Disease Protocols. Veterinary Sciences. 2024; 11(10):460. https://doi.org/10.3390/vetsci11100460
Chicago/Turabian StyleMartin, Lauren Drew, Jaclyn Shelton, Lisa A. Houser, Rhonda MacAllister, and Kristine Coleman. 2024. "Refinements in Clinical and Behavioral Management for Macaques on Infectious Disease Protocols" Veterinary Sciences 11, no. 10: 460. https://doi.org/10.3390/vetsci11100460
APA StyleMartin, L. D., Shelton, J., Houser, L. A., MacAllister, R., & Coleman, K. (2024). Refinements in Clinical and Behavioral Management for Macaques on Infectious Disease Protocols. Veterinary Sciences, 11(10), 460. https://doi.org/10.3390/vetsci11100460





