Evaluation of Blood Lactate, Heart Rate, Blood Pressure, and Shock Index, and Their Association with Prognosis in Calves
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
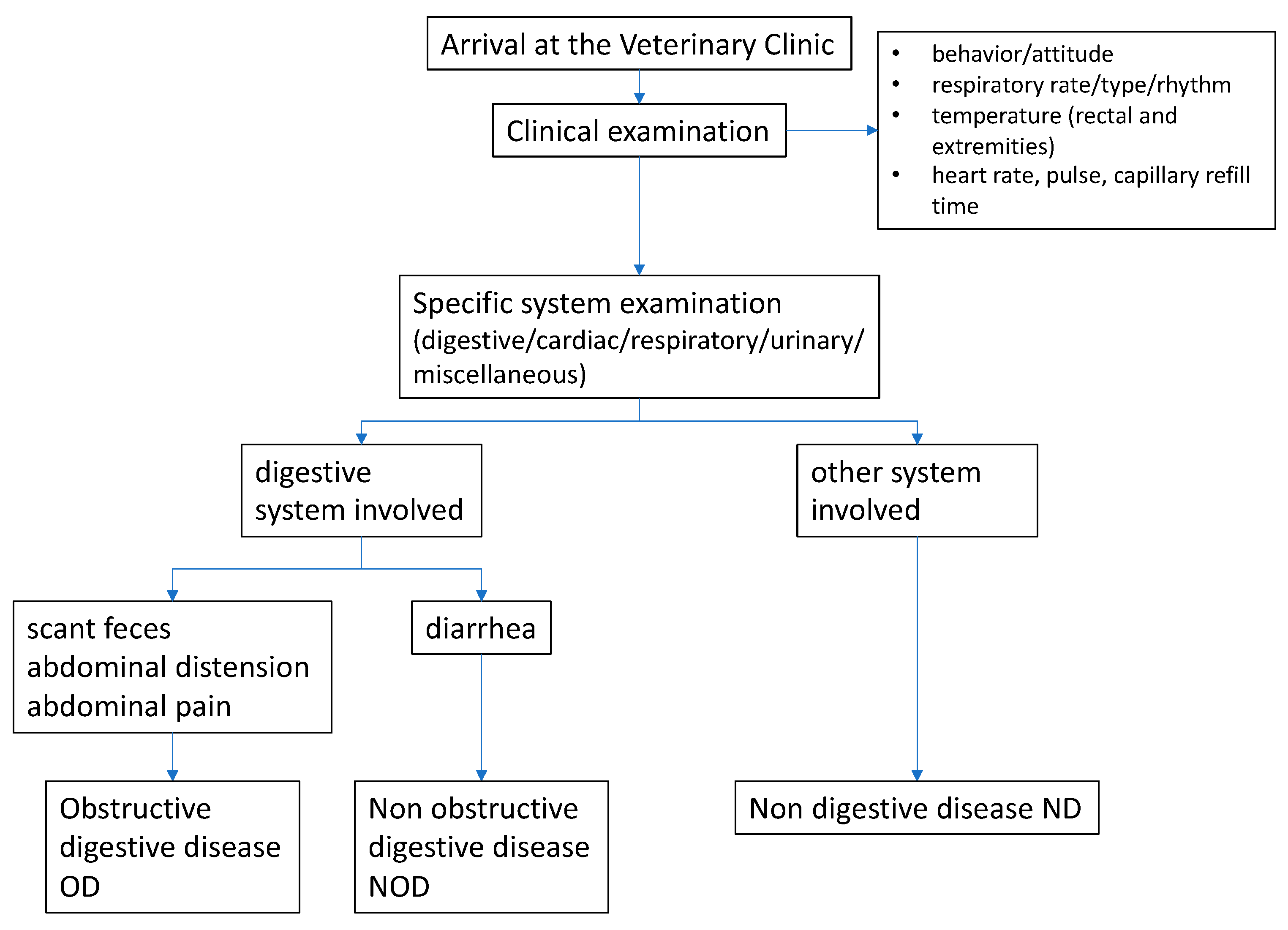
2.1. Animal and Clinical Evaluation
2.2. Ancillary Tests
2.3. Clinical Shock Evaluation
2.4. Therapy and Outcome
2.5. Statistical Analysis
3. Results
3.1. Demographic Data
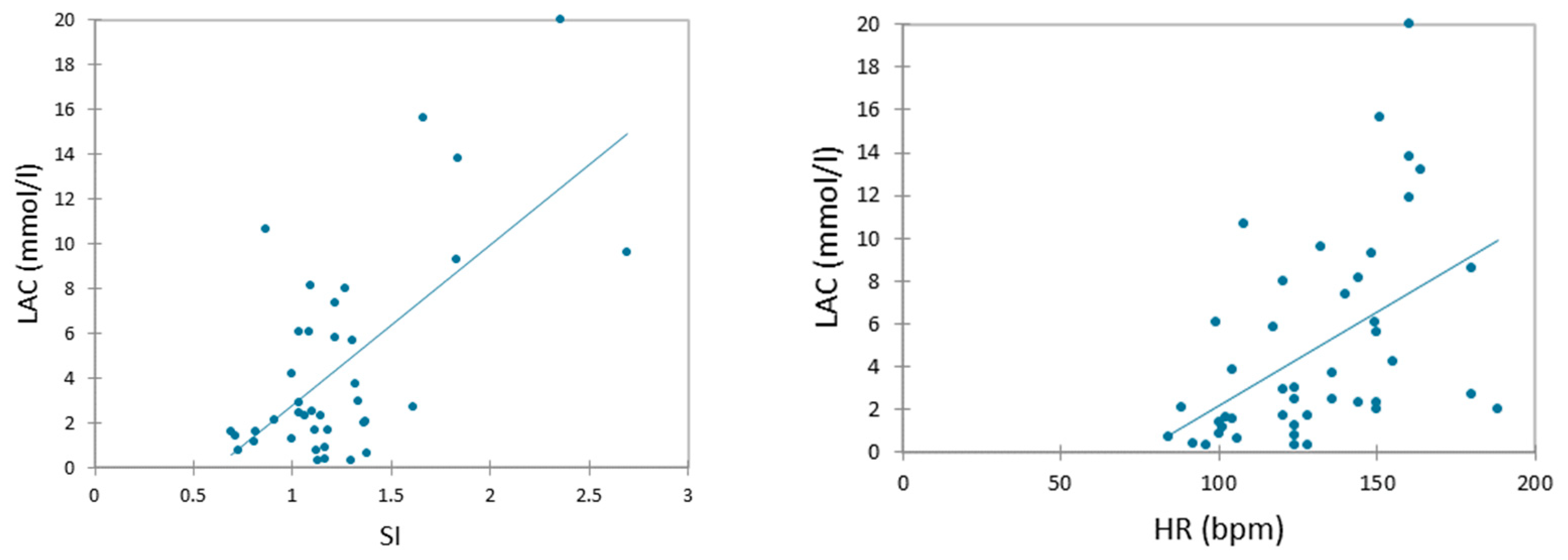
3.2. Shock Evaluation
3.3. Outcome
4. Discussion
5. Limitations of the Study
6. Perspectives
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Porter, A.E.; Rozanski, E.A.; Sharp, C.R.; Dixon, K.L.; Price, L.L.; Shaw, S.P. Evaluation of the Shock Index in Dogs Presenting as Emergencies. J. Vet. Emerg. Crit. Care 2013, 23, 538–544. [Google Scholar] [CrossRef] [PubMed]
- Cecconi, M.; De Backer, D.; Antonelli, M.; Beale, R.; Bakker, J.; Hofer, C.; Jaeschke, R.; Mebazaa, A.; Pinsky, M.R.; Teboul, J.L.; et al. Consensus on Circulatory Shock and Hemodynamic Monitoring. Task Force of the European Society of Intensive Care Medicine. Intensive Care Med. 2014, 40, 1795–1815. [Google Scholar] [CrossRef] [PubMed]
- De Laforcade, A.; Silverstein, D.C. Shock. In Small Animal Critical Care Medicine, 2nd ed.; Elsevier Inc.: Amsterdam, The Netherlands, 2014; pp. 26–30. ISBN 9781455703067. [Google Scholar]
- Kashani, K.; Omer, T.; Shaw, A.D. The Intensivist’s Perspective of Shock, Volume Management, and Hemodynamic Monitoring. Clin. J. Am. Soc. Nephrol. 2022, 17, 706–716. [Google Scholar] [CrossRef] [PubMed]
- Constable, P.D.; Hinchcliff, K.W.; Done, S.H.; Grünberg, W. General Systemic States. In Veterinary Medicine; Elsevier: Amsterdam, The Netherlands, 2017; pp. 43–112. [Google Scholar]
- Londoño, J.; Niño, C.; Díaz, J.; Morales, C.; León, J.; Bernal, E.; Vargas, C.; Mejía, L.; Hincapié, C.; Ascuntar, J.; et al. Association of Clinical Hypoperfusion Variables with Lactate Clearance and Hospital Mortality. Shock 2018, 50, 286–292. [Google Scholar] [CrossRef] [PubMed]
- Burgunder, L.; Heyrend, C.; Olson, J.; Stidham, C.; Lane, R.D.; Workman, J.K.; Larsen, G.Y. Medication and Fluid Management of Pediatric Sepsis and Septic Shock. Pediatr. Drugs 2022, 24, 193–205. [Google Scholar] [CrossRef] [PubMed]
- Hilarius, K.W.E.; Skippen, P.W.; Kissoon, N. Early Recognition and Emergency Treatment of Sepsis and Septic Shock in Children. Pediatr. Emerg. Care 2020, 36, 101–106. [Google Scholar] [CrossRef]
- Fielding, C.L.; Magdesian, K.G. Sepsis and Septic Shock in the Equine Neonate. Vet. Clin. N. Am.—Equine Pract. 2015, 31, 483–496. [Google Scholar] [CrossRef]
- Aldrich, J. Global Assessment of the Emergency Patient. Vet. Clin. N. Am.—Small Anim. Pract. 2005, 35, 281–305. [Google Scholar] [CrossRef]
- Boag, A.K.; Hughes, D. Assessment and Treatment of Perfusion Abnormalities in the Emergency Patient. Vet. Clin. N. Am.—Small Anim. Pract. 2005, 35, 319–342. [Google Scholar] [CrossRef]
- Cummings, C.O.; Krucik, D.D.R.; Price, E. Clinical Predictive Models in Equine Medicine: A Systematic Review. Equine Vet. J. 2022, 55, 573–583. [Google Scholar] [CrossRef]
- Shea, E.K.; Dombrowki, S.C.; Silvertein, D.C. Survival Analysis of Hypotensive Cats Admitted to an Intensive Care Unit with or without Hyperlactatemia: 39 Cases (2005–2011). JAVMA 2017, 250, 887–893. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, G.; Bruhn, A.; Castro, R.; Pedreros, C.; Rovegno, M.; Kattan, E.; Veas, E.; Fuentealba, A.; Regueira, T.; Ruiz, C.; et al. Persistent Sepsis-Induced Hypotension without Hyperlactatemia: A Distinct Clinical and Physiological Profile within the Spectrum of Septic Shock. Crit. Care Res. Pract. 2012, 2012, 536852. [Google Scholar] [CrossRef] [PubMed]
- Troia, R.; Buzzurra, F.; Ciuffoli, E.; Mascalzoni, G.; Foglia, A.; Magagnoli, I.; Dondi, F.; Giunti, M. Classification of Septic Shock Phenotypes Based on the Presence of Hypotension and Hyperlactatemia in Cats. Front. Vet. Sci. 2021, 8, 692528. [Google Scholar] [CrossRef] [PubMed]
- Messina, A.; Calabrò, L.; Pugliese, L.; Lulja, A.; Sopuch, A.; Rosalba, D.; Morenghi, E.; Hernandez, G.; Monnet, X.; Cecconi, M. Fluid Challenge in Critically Ill Patients Receiving Haemodynamic Monitoring: A Systematic Review and Comparison of Two Decades. Crit. Care 2022, 26, 186. [Google Scholar] [CrossRef] [PubMed]
- Tennent-Brown, B.S.; Wilkins, P.A.; Lindborg, S.; Russell, G.; Boston, R.C. Sequential Plasma Lactate Concentrations as Prognostic Indicators in Adult Equine Emergencies. J. Vet. Intern. Med. 2010, 24, 198–205. [Google Scholar] [CrossRef] [PubMed]
- Wardi, G.; Brice, J.; Correia, M.; Liu, D.; Self, M.; Tainter, C. Demystifying Lactate in the Emergency Department. Ann. Emerg. Med. 2020, 75, 287–298. [Google Scholar] [CrossRef] [PubMed]
- Pang, D.S.; Boysen, S. Lactate in Veterinary Critical Care: Pathophysiology and Management. J. Am. Anim. Hosp. Assoc. 2007, 43, 270–279. [Google Scholar] [CrossRef]
- Verhaeghe, M.; Hachimi-Idrissi, S. Blood Lactate and Lactate Kinetics as Treatment and Prognosis Markers for Tissue Hypoperfusion. Acta Clin. Belg. Int. J. Clin. Lab. Med. 2020, 75, 1–8. [Google Scholar] [CrossRef]
- Blutinger, A.L.; Zollo, A.M.; Weltman, J.; Prittie, J. Prospective Evaluation of Plasma Lactate Parameters for Prognosticating Dogs with Shock. J. Vet. Emerg. Crit. Care 2021, 31, 351–359. [Google Scholar] [CrossRef]
- Zollo, A.M.; Ayoob, A.L.; Prittie, J.E.; Jepson, R.D.; Lamb, K.E.; Fox, P.R. Utility of Admission Lactate Concentration, Lactate Variables, and Shock Index in Outcome Assessment in Dogs Diagnosed with Shock. J. Vet. Emerg. Crit. Care 2019, 29, 505–513. [Google Scholar] [CrossRef]
- Lausch, C.K.; Lorch, A.; Knubben-Schweizer, G.; Rieger, A.; Trefz, F.M. Prognostic Value of Preoperative Plasma L-Lactate Concentrations in Calves with Acute Abdominal Emergencies. J. Dairy Sci. 2019, 102, 10202–10212. [Google Scholar] [CrossRef] [PubMed]
- Lausch, C.K.; Lorch, A.; Giertzuch, S.; Rieger, A.; Knubben-Schweizer, G.; Trefz, F.M. Prognostic Relevance of Pre- and Postoperative Plasma L-Lactate Measurements in Calves with Acute Abdominal Emergencies. J. Dairy Sci. 2020, 103, 1856–1865. [Google Scholar] [CrossRef] [PubMed]
- Giertzuch, S.; Lorch, A.; Lausch, C.K.; Knubben-Schweizer, G.; Trefz, F.M. Prognostic Utility of Pre- and Postoperative Plasma L-Lactate Measurements in Hospitalized Cows with Acute Abdominal Emergencies. J. Dairy Sci. 2020, 103, 11769–11781. [Google Scholar] [CrossRef] [PubMed]
- Kraenzlin, M.N.; Cortes, Y.; Fettig, P.K.; Bailey, D.B. Shock Index Is Associated with Mortality in Canine Vehicular Trauma Patients. J. Vet. Emerg. Crit. Care 2020, 30, 706–711. [Google Scholar] [CrossRef] [PubMed]
- Yasaka, Y.; Khemani, R.G.; Markovitz, B.P. Is Shock Index Associated with Outcome in Children with Sepsis/Septic Shock? Pediatr. Crit. Care Med. 2013, 14, e372–e379. [Google Scholar] [CrossRef] [PubMed]
- Birkhahn, R.H.; Gaeta, T.J.; Terry, D.; Bove, J.J.; Tloczkowski, J. Shock Index in Diagnosing Early Acute Hypovolemia. Am. J. Emerg. Med. 2005, 23, 323–326. [Google Scholar] [CrossRef] [PubMed]
- Peterson, K.L.; Hardy, B.T.; Hall, K. Assessment of Shock Index in Healthy Dogs and Dogs in Hemorrhagic Shock. J. Vet. Emerg. Crit. Care 2013, 23, 545–550. [Google Scholar] [CrossRef] [PubMed]
- McGowan, E.E.; Marryott, K.; Drobatz, K.J.; Reineke, E.L. Evaluation of the Use of Shock Index in Identifying Acute Blood Loss in Healthy Blood Donor Dogs. J. Vet. Emerg. Crit. Care 2017, 27, 524–531. [Google Scholar] [CrossRef]
- Homerosky, E.R.; Caulkett, N.A.; Timsit, E.; Pajor, E.A.; Kastelic, J.P.; Windeyer, M.C. Clinical Indicators of Blood Gas Disturbances, Elevated L-Lactate Concentration and Other Abnormal Blood Parameters in Newborn Beef Calves. Vet. J. 2017, 219, 49–57. [Google Scholar] [CrossRef]
- Yildiz, R.; Aydogdu, U.; Guzelbektes, H.; Coskun, A.; Sen, I. Venous Lactate, PH and Partial Pressure of Carbon Dioxide Levels as Prognostic Indicators in 110 Premature Calves with Respiratory Distress Syndrome. Vet. Rec. 2017, 180, 611. [Google Scholar] [CrossRef]
- Buczinski, S.; Rademacher, R.D.; Tripp, H.M.; Edmonds, M.; Johnson, E.G.; Dufour, S. Assessment of L-Lactatemia as a Predictor of Respiratory Disease Recognition and Severity in Feedlot Steers. Prev. Vet. Med. 2015, 118, 306–318. [Google Scholar] [CrossRef] [PubMed]
- Bleul, U. Respiratory Distress Syndrome in Calves. Vet. Clin. N. Am. Food Anim. Pract. 2009, 25, 179–193. [Google Scholar] [CrossRef] [PubMed]
- Danlois, F.; Zaltash, S.; Johansson, J.; Robertson, B.; Haagsman, H.P.; Rollin, F.; Ruysschaert, J.M.; Vandenbussche, G. Pulmonary Surfactant from Healthy Belgian White and Blue and Holstein Friesian Calves: Biochemical and Biophysical Comparison. Vet. J. 2003, 165, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Danlois, F.; Zaltash, S.; Johansson, J.; Robertson, B.; Haagsman, H.P.; van Eijk, M.; Beers, M.F.; Rollin, F.; Ruysschaert, J.M.; Vandenbussche, G. Very Low Surfactant Protein C Contents in Newborn Belgian White and Blue Calves with Respiratory Distress Syndrome. Biochem. J. 2000, 351 Pt 3, 779–787. [Google Scholar] [CrossRef] [PubMed]
- Karapinar, T.; Dabak, M. Treatment of Premature Calves with Clinically Diagnosed Respiratory Distress Syndrome. J. Vet. Intern. Med. 2008, 22, 462–466. [Google Scholar] [CrossRef] [PubMed]
- Christmann, U.; Buechner-Maxwell, V.A.; Witonsky, S.G.; Hite, R.D. Role of Lung Surfactant in Respiratory Disease: Current Knowledge in Large Animal Medicine. J. Vet. Intern. Med. 2009, 23, 227–242. [Google Scholar] [CrossRef] [PubMed]
- Ateca, L.B.; Dombrowski, S.C.; Silverstein, D.C. Survival Analysis of Critically Ill Dogs with Hypotension with or without Hyperlactatemia: 67 Cases (2006–2011). JAVMA 2015, 246, 100–104. [Google Scholar] [CrossRef]
- Mair, T.S.; Smith, L.J.; Sherlock, C.E. Evidence-Based Gastrointestinal Surgery in Horses. Vet. Clin. N. Am.—Equine Pract. 2007, 23, 267–292. [Google Scholar] [CrossRef]
- Mair, T.S.; Smith, L.J. Survival and Complication Rates in 300 Horses Undergoing Surgical Treatment of Colic. Part 2: Short-Term Complications. Equine Vet. J. 2005, 37, 303–309. [Google Scholar] [CrossRef]
- Spadari, A.; Gialletti, R.; Gandini, M.; Valle, E.; Cerullo, A.; Cavallini, D.; Bertoletti, A.; Rinnovati, R.; Forni, G.; Scilimati, N.; et al. Short-Term Survival and Postoperative Complications Rates in Horses Undergoing Colic Surgery: A Multicentre Study. Animals 2023, 13, 1107. [Google Scholar] [CrossRef]
- Van der Linden, M.A.; Laffont, C.M.; Sloet van Oldruitenborgh-Oosterbaan, M.M. Prognosis in Equine Medical and Surgical Colic. J. Vet. Intern. Med. 2003, 17, 343–348. [Google Scholar] [CrossRef] [PubMed]
- Saint-Pierre, L.M.; Hopper, K.; Epstein, S.E. Retrospective Evaluation of the Prognostic Utility of Plasma Lactate Concentration and Serial Lactate Measurements in Dogs and Cats Presented to the Emergency Room (January 2012–December 2016): 4863 Cases. J. Vet. Emerg. Crit. Care 2022, 32, 42–49. [Google Scholar] [CrossRef]
- Rosenstein, P.G.; Tennent-Brown, B.S.; Hughes, D. Clinical Use of Plasma Lactate Concentration. Part 2: Prognostic and Diagnostic Utility and the Clinical Management of Hyperlactatemia. J. Vet. Emerg. Crit. Care 2018, 28, 106–121. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, E.K.; Hobbs, K.J.; McKinney-Aguirre, C.A.; Gonzalez, L.M. Biomarkers of Intestinal Injury in Colic. Animals 2023, 13, 227. [Google Scholar] [CrossRef]
- Boulay, G.; Francoz, D.; Doré, E.; Dufour, S.; Veillette, M.; Badillo, M.; Bélanger, A.-M.; Buczinski, S. Preoperative Cow-Side Lactatemia Measurement Predicts Negative Outcome in Holstein Dairy Cattle with Right Abomasal Disorders. J. Dairy Sci. 2014, 97, 212–221. [Google Scholar] [CrossRef] [PubMed]
- Buczinski, S.; Boulay, G.; Francoz, D. Preoperative and Postoperative L-Lactatemia Assessment for the Prognosis of Right Abomasal Disorders in Dairy Cattle. J. Vet. Intern. Med. 2015, 29, 375–380. [Google Scholar] [CrossRef] [PubMed]
- Castagnetti, C.; Pirrone, A.; Mariella, J.; Mari, G. Venous Blood Lactate Evaluation in Equine Neonatal Intensive Care. Theriogenology 2010, 73, 343–357. [Google Scholar] [CrossRef] [PubMed]
- Straticò, P.; Varasano, V.; Palozzo, A.; Guerri, G.; Celani, G.; Revelant, O.; Petrizzi, L. Retrospective Study on Risk Factors and Short-Term Outcome of Horses Referred for Colic from 2016 to 2022. Vet. Sci. 2022, 9, 545. [Google Scholar] [CrossRef]
- Proudman, C.J.; Dugdale, A.H.A.; Senior, J.M.; Edwards, G.B.; Smith, J.E.; Leuwer, M.L.; French, N.P. Pre-Operative and Anaesthesia-Related Risk Factors for Mortality in Equine Colic Cases. Vet. J. 2006, 171, 89–97. [Google Scholar] [CrossRef]
- Grulke, S.; Olle, E.; Detilleux, J.; Gangl, M.; Caudron, I.; Serteyn, D. Determination of a Gravity and Shock Score for Prognosis in Equine Surgical Colic. J. Vet. Med. Ser. A 2001, 48, 465–473. [Google Scholar] [CrossRef]
- Redavid, L.A.; Sharp, C.R.; Mitchell, M.A.; Beckel, N.F. Hyperlactatemia and Serial Lactate Measurements in Sick Cats. J. Vet. Emerg. Crit. Care 2016, 26, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Mulon, P.Y.; Desrochers, A. Surgical Abdomen of the Calf. Vet. Clin. N. Am.—Food Anim. Pract. 2005, 21, 101–132. [Google Scholar] [CrossRef] [PubMed]
- Bjorklund, A.; Resch, J.; Slusher, T. Pediatric Shock Review. Pediatr. Rev. 2023, 44, 551–565. [Google Scholar] [CrossRef] [PubMed]
| n | HR (bpm) | CRT (s) | SBP (mmHg) | DBP (mmHg) | MBP (mmHg) | LAC (mmol/L) | SI | ||
|---|---|---|---|---|---|---|---|---|---|
| CLINICAL SHOCK | CSS | 28 | NA | NA | 111 ± 23 | 63 ± 16 | 79 ± 17 | 3.73 (1.85–8.94) a | 1.20 (1.02–1.37) |
| WOCSS | 17 | NA | NA | 107 ± 25 | 59 ± 21 | 75 ± 22 | 2.10 (0.88–3.88) b | 1.12 (1.05–1.19) | |
| DISEASE | OD | 22 | 141 ± 22 c | 3 (2–3) | 111 ± 20 | 61 ± 15 | 77 ± 16 | 4.20 (2.46–10.65) c | 1.15 (1.10–1.53) |
| NOD | 11 | 121 ± 30 d | 3 (3–4) | 105 ± 24 | 60 ± 16 | 75 ± 18 | 2.05 (0.69–6.08) d | 1.16 (1.09–1.32) | |
| ND | 12 | 119 ± 22 d | 3 (2–4) | 112 ± 29 | 64 ± 25 | 80 ± 25 | 2.05 (1.38–2.45) d | 1.05 (0.88–1.24) | |
| Total | 45 | 130 ± 26 | 3 (2–4) | 110 ± 23 | 61 ± 18 | 77 ± 19 | 2.60 (1.54–7.53) | 1.14 (1.03–1.32) | |
| N | HR (bpm) | CRT (s) | SBP (mmHg) | DBP (mmHg) | MBP (mmHg) | LAC (mmol/L) | SI | ||
|---|---|---|---|---|---|---|---|---|---|
| OUTCOME | P | 21 | 124 ± 27 | 3 (2–4) | 112 ± 24 | 63 ± 15 | 79 ± 17 | 2.0 (0.7–6.1) a | 1.1 (1.0–1.2) |
| N | 24 | 136 ± 25 | 3 (3–4) | 108 ± 23 | 61 ± 21 | 76 ± 21 | 3.0 (2.1–9.5) b | 1.2 (1.1–1.5) | |
| Total | 45 | 130 ± 26 | 3 (2–4) | 110 ± 23 | 61 ± 18 | 77 ± 19 | 2.6 (1.5–7.3) | 1.1 (1.0–1.3) | |
| SBP ≤ 90 | SBP > 90 | LAC > 2 | LAC ≤ 2 | LAC > 2; SBP ≤ 90 | LAC ≤ 2; SBP > 90 | ||
|---|---|---|---|---|---|---|---|
| n | 8 | 32 | 28 | 16 | 4 | 35 | |
| OUTCOME | P | 4 | 13 | 10 a | 11 | 0 | 17 |
| N | 4 | 19 | 18 b | 5 | 4 | 18 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Casalta, H.; Bayrou, C.; Djebala, S.; Eppe, J.; Gille, L.; Gommeren, K.; Marduel, E.; Sartelet, A.; Seys, C.; Versyp, J.; et al. Evaluation of Blood Lactate, Heart Rate, Blood Pressure, and Shock Index, and Their Association with Prognosis in Calves. Vet. Sci. 2024, 11, 45. https://doi.org/10.3390/vetsci11010045
Casalta H, Bayrou C, Djebala S, Eppe J, Gille L, Gommeren K, Marduel E, Sartelet A, Seys C, Versyp J, et al. Evaluation of Blood Lactate, Heart Rate, Blood Pressure, and Shock Index, and Their Association with Prognosis in Calves. Veterinary Sciences. 2024; 11(1):45. https://doi.org/10.3390/vetsci11010045
Chicago/Turabian StyleCasalta, Hélène, Calixte Bayrou, Salem Djebala, Justine Eppe, Linde Gille, Kris Gommeren, Eva Marduel, Arnaud Sartelet, Celine Seys, Jérôme Versyp, and et al. 2024. "Evaluation of Blood Lactate, Heart Rate, Blood Pressure, and Shock Index, and Their Association with Prognosis in Calves" Veterinary Sciences 11, no. 1: 45. https://doi.org/10.3390/vetsci11010045
APA StyleCasalta, H., Bayrou, C., Djebala, S., Eppe, J., Gille, L., Gommeren, K., Marduel, E., Sartelet, A., Seys, C., Versyp, J., & Grulke, S. (2024). Evaluation of Blood Lactate, Heart Rate, Blood Pressure, and Shock Index, and Their Association with Prognosis in Calves. Veterinary Sciences, 11(1), 45. https://doi.org/10.3390/vetsci11010045







