Measurement of Ghrelin as a Marker of Appetite Dysregulation in Cats with and without Chronic Kidney Disease
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
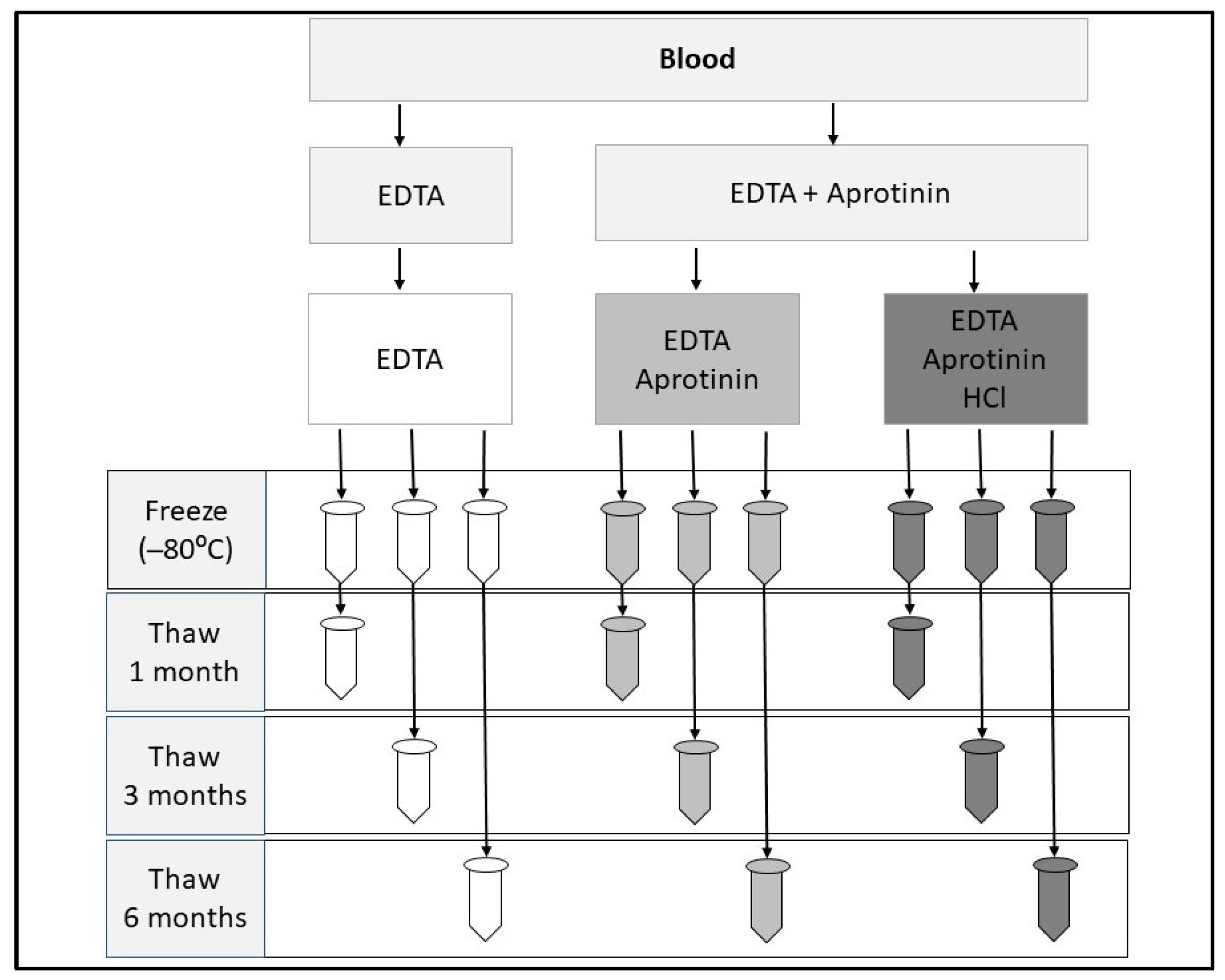
2.1. Sample Storage Optimization
2.1.1. Cats
2.1.2. Sample Collection
2.1.3. Sample Measurement
2.1.4. Statistical Analysis
2.2. Ghrelin in Cats with and without CKD
2.2.1. Cats
2.2.2. Appetite Questionnaire
2.2.3. Sample Collection and Preparation
2.2.4. Sample Analysis
2.2.5. Statistical Analysis
3. Results
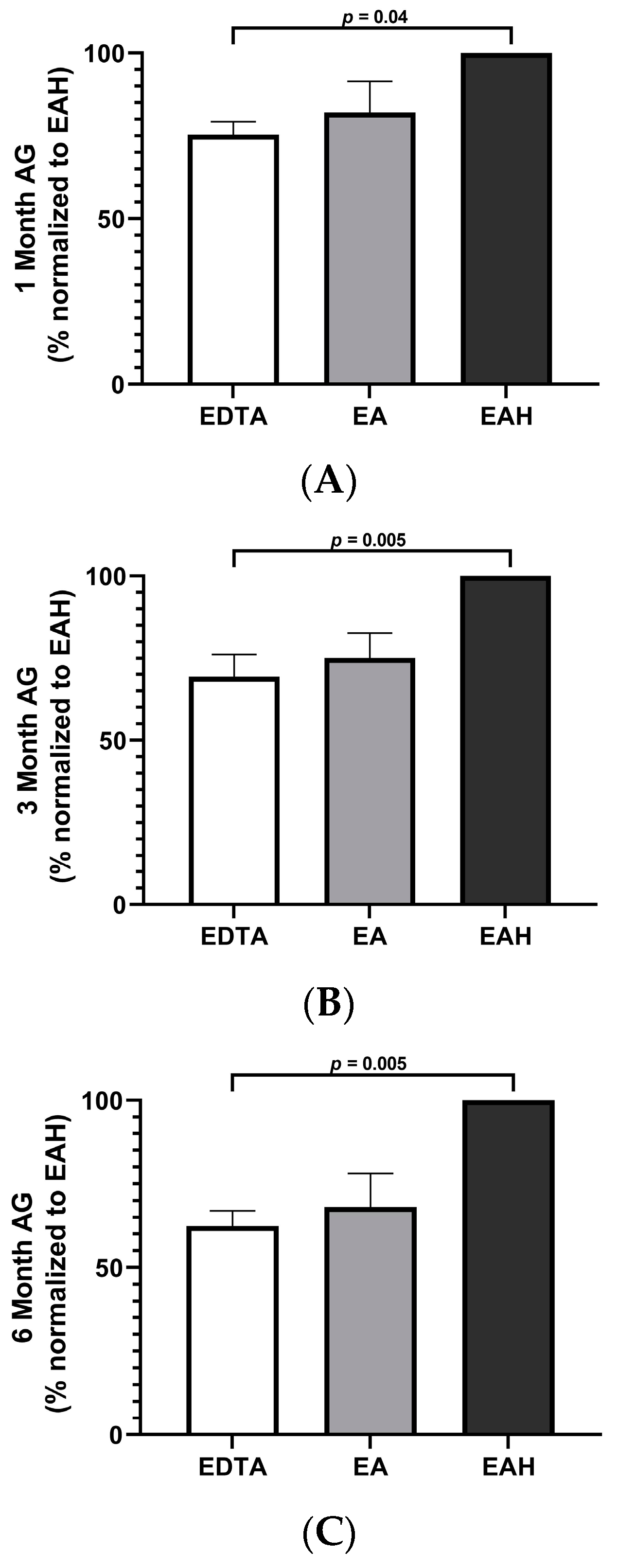
3.1. Sample Storage Optimization
3.1.1. Cats
3.1.2. Radioimmunoassay Results
3.2. Ghrelin in Cats with and without CKD
3.2.1. Cats
3.2.2. Appetite Questionnaire
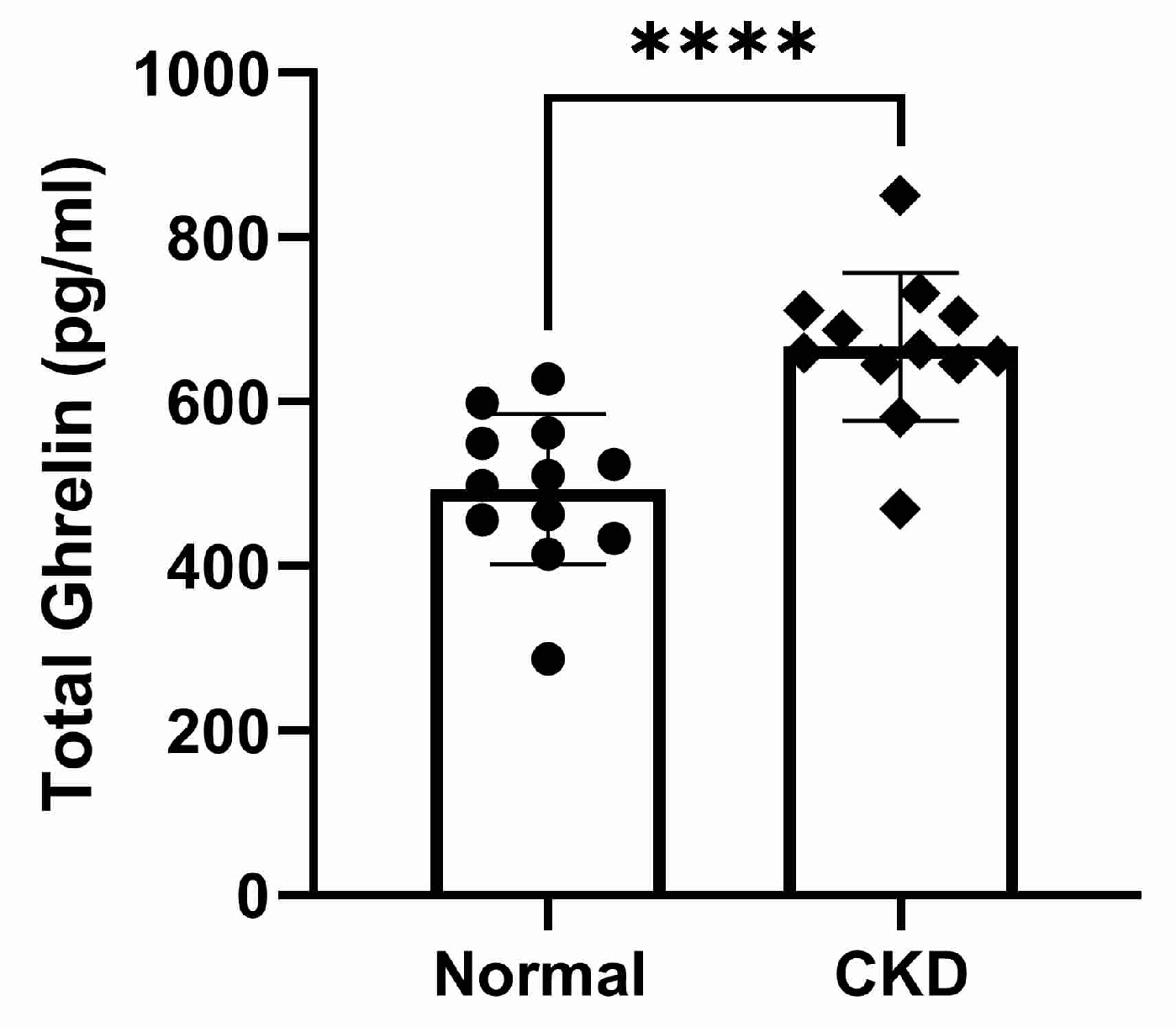
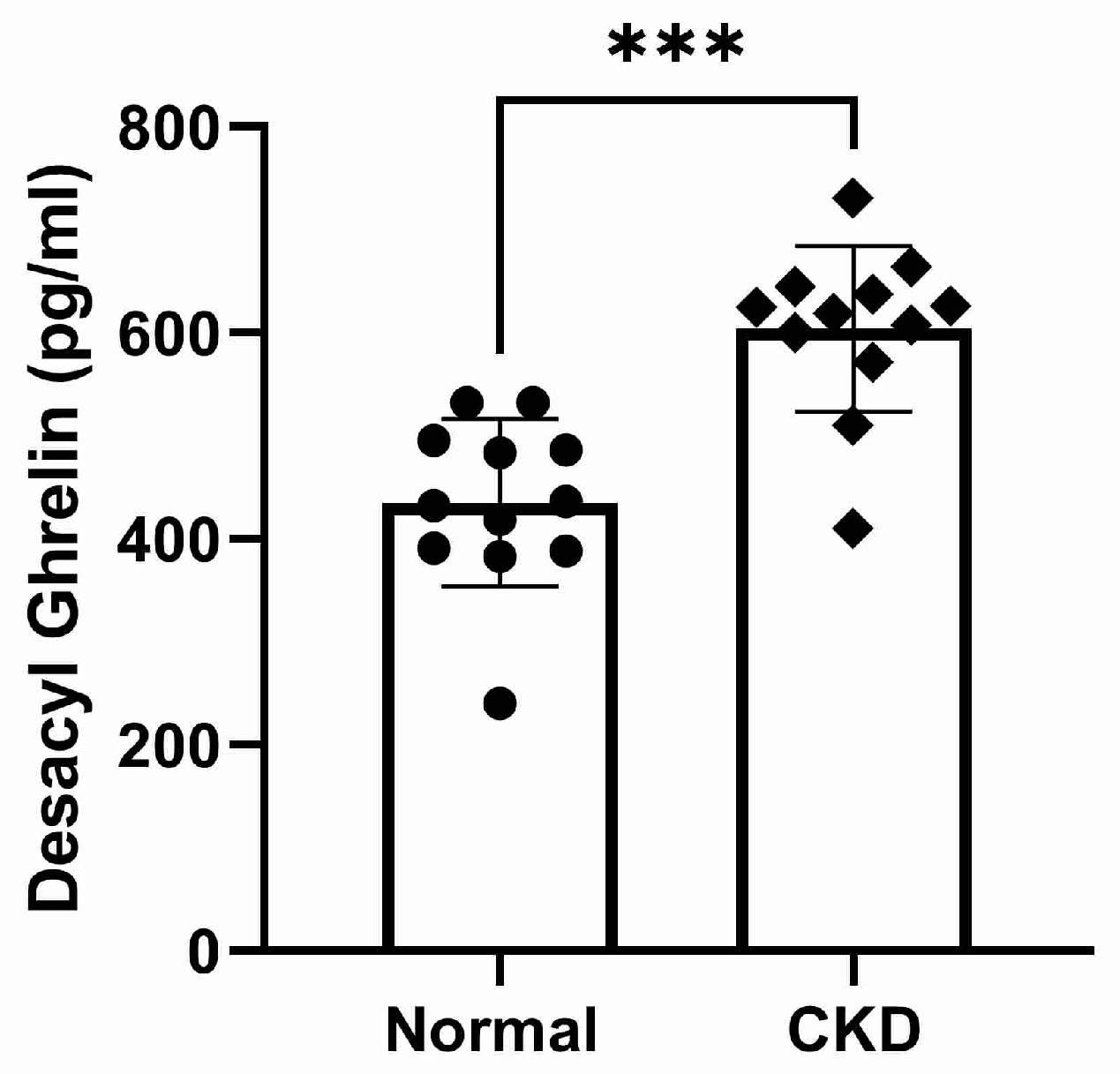
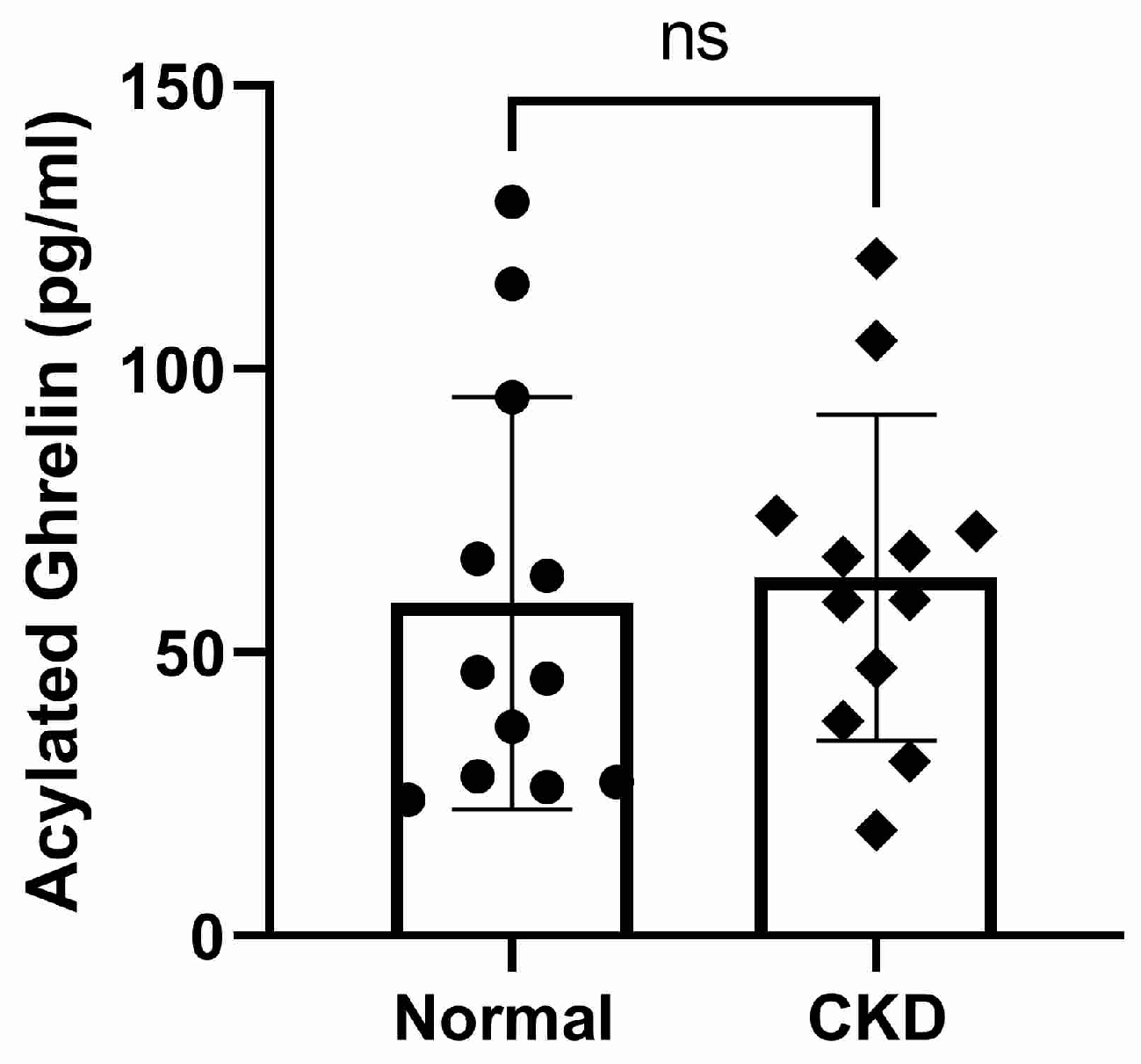
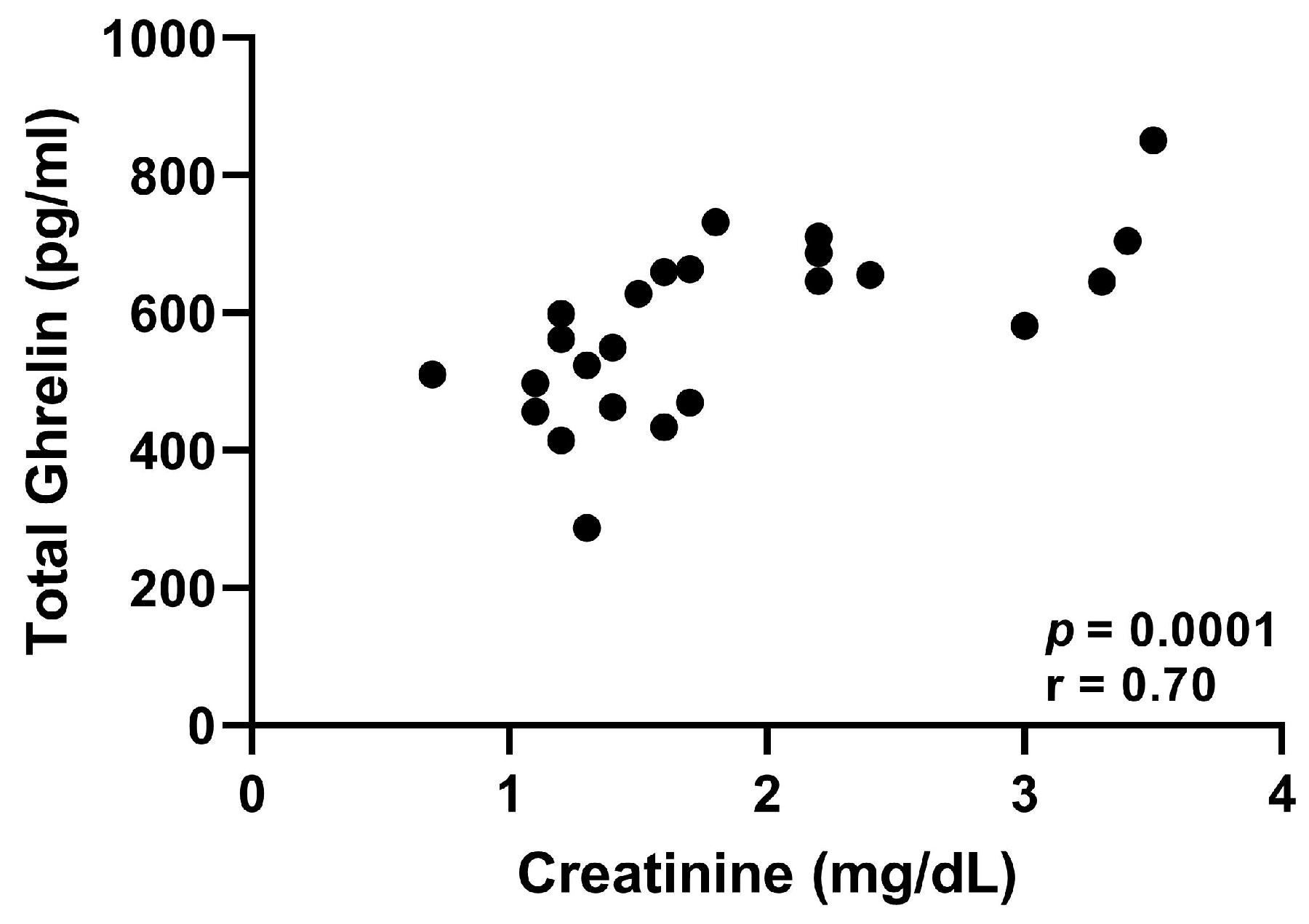
3.2.3. Radioimmunoassay Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- King, J.N.; Tasker, S.; Gunn-Moore, D.A.; Strehlau, G. Prognostic factors in cats with chronic kidney disease. J. Vet. Intern. Med. 2007, 21, 906–916. [Google Scholar] [CrossRef] [PubMed]
- Markovich, J.E.; Freeman, L.M.; Labato, M.A.; Heinze, C.R. Survey of dietary and medication practices of owners of cats with chronic kidney disease. J. Feline Med. Surg. 2015, 17, 979–983. [Google Scholar] [CrossRef] [PubMed]
- Freeman, L.M.; Lachaud, M.P.; Matthews, S.; Rhodes, L.; Zollers, B. Evaluation of weight loss over time in cats with chronic kidney disease. J. Vet. Intern. Med. 2016, 30, 1661–1666. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, C.A.; Oyama, M.A.; Rush, J.E.; Rozanski, E.A.; Singletary, G.E.; Brown, D.C.; Cunningham, S.M.; Fox, P.R.; Bond, B.; Adin, D.B.; et al. Perceptions of quality of life and priorities of owners of cats with heart disease. J. Vet. Intern. Med. 2010, 24, 1421–1426. [Google Scholar] [CrossRef]
- Kovesdy, C.P.; Kopple, J.D.; Kalantar-Zadeh, K. Management of protein-energy wasting in non-dialysis-dependent chronic kidney disease: Reconciling low protein intake with nutritional therapy. Am. J. Clin. Nutr. 2013, 97, 1163–1177. [Google Scholar] [CrossRef]
- Asakawa, A.; Inui, A.; Fujimiya, M.; Sakamaki, R.; Shinfuku, N.; Ueta, Y.; Meguid, M.M.; Kasuga, M. Stomach regulates energy balance via acylated ghrelin and desacyl ghrelin. Gut 2005, 54, 18–24. [Google Scholar] [CrossRef]
- Wren, A.M.; Small, C.J.; Ward, H.L.; Murphy, K.G.; Dakin, C.L.; Taheri, S.; Kennedy, A.R.; Roberts, G.H.; Morgan, D.G.; Ghatei, M.A.; et al. The novel hypothalamic peptide ghrelin stimulates food intake and growth hormone secretion. Endocrinology 2000, 141, 4325–4328. [Google Scholar] [CrossRef]
- Kojima, M.; Hosoda, H.; Date, Y.; Nakazato, M.; Matsuo, H.; Kangawa, K. Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature 1999, 402, 656–660. [Google Scholar] [CrossRef]
- Howard, A.D.; Feighner, S.D.; Cully, D.F.; Arena, J.P.; Liberator, P.A.; Rosenblum, C.I.; Hamelin, M.; Hreniuk, D.L.; Palyha, O.C.; Anderson, J.; et al. A receptor in pituitary and hypothalamus that functions in growth hormone release. Science 1996, 273, 974–977. [Google Scholar] [CrossRef]
- Hosoda, H.; Kangawa, K. Standard sample collections for blood ghrelin measurements. Methods Enzymol. 2012, 514, 113–126. [Google Scholar] [CrossRef]
- Buscher, A.K.; Buscher, R.; Hauffa, B.P.; Hoyer, P.F. Alterations in appetite-regulating hormones influence protein-energy wasting in pediatric patients with chronic kidney disease. Pediatr. Nephrol. 2010, 25, 2295–2301. [Google Scholar] [CrossRef] [PubMed]
- Monzani, A.; Perrone, M.; Prodam, F.; Moia, S.; Genoni, G.; Testa, S.; Paglialonga, F.; Rapa, A.; Bona, G.; Montini, G.; et al. Unacylated ghrelin and obestatin: Promising biomarkers of protein energy wasting in children with chronic kidney disease. Pediatr. Nephrol. 2018, 33, 661–672. [Google Scholar] [CrossRef] [PubMed]
- Hosoda, H.; Doi, K.; Nagaya, N.; Okumura, H.; Nakagawa, E.; Enomoto, M.; Ono, F.; Kangawa, K. Optimum collection and storage conditions for ghrelin measurements: Octanoyl modification of ghrelin is rapidly hydrolyzed to desacyl ghrelin in blood samples. Clin. Chem. 2004, 50, 1077–1080. [Google Scholar] [CrossRef]
- Marsilio, S.; Glanemann, B.; Martin, L.; Szladovits, B.; Neiger, R. Leptin and ghrelin concentration in hyperthyroid cats before and after radioactive iodine therapy compared to euthyroid control cats. Tierärztliche Prax. Ausg. K Kleintiere Heimtiere 2017, 45, 95–101. [Google Scholar] [CrossRef]
- Ida, T.; Miyazato, M.; Naganobu, K.; Nakahara, K.; Sato, M.; Lin, X.Z.; Kaiya, H.; Doi, K.; Noda, S.; Kubo, A.; et al. Purification and characterization of feline ghrelin and its possible role. Domest. Anim. Endocrinol. 2007, 32, 93–105. [Google Scholar] [CrossRef]
- Sakao, Y.; Sugimoto, M.; Ichikawa, H.; Sahara, S.; Tsuji, T.; Ohashi, N.; Kato, A.; Fujigaki, Y.; Sugimoto, K.; Furuta, T.; et al. Severity of Gastric Mucosal Atrophy Is the Major Determinant of Plasma Ghrelin Level in Hemodialysis Patients. Am. J. Nephrol. 2016, 44, 224–233. [Google Scholar] [CrossRef]
- Yoshimoto, A.; Mori, K.; Sugawara, A.; Mukoyama, M.; Yahata, K.; Suganami, T.; Takaya, K.; Hosoda, H.; Kojima, M.; Kangawa, K.; et al. Plasma ghrelin and desacyl ghrelin concentrations in renal failure. J. Am. Soc. Nephrol. 2002, 13, 2748–2752. [Google Scholar] [CrossRef] [PubMed]
- Eftekhari, M.H.; Ranjbar-Zahedani, M.; Basiratnia, M.; Rezaianzadeh, A.; Faghih, S. Comparison of Appetite-regulating Hormones and Body Composition in Pediatric Patients in Predialysis Stage of Chronic Kidney Disease and Healthy Control Group. Iran. J. Med. Sci. 2015, 40, 27–33. [Google Scholar]
- Gupta, R.K.; Kuppusamy, T.; Patrie, J.T.; Gaylinn, B.; Liu, J.; Thorner, M.O.; Bolton, W.K. Association of plasma des-acyl ghrelin levels with CKD. Clin. J. Am. Soc. Nephrol. 2013, 8, 1098–1105. [Google Scholar] [CrossRef]
- Arbeiter, A.K.; Buscher, R.; Petersenn, S.; Hauffa, B.P.; Mann, K.; Hoyer, P.F. Ghrelin and other appetite-regulating hormones in paediatric patients with chronic renal failure during dialysis and following kidney transplantation. Nephrol. Dial. Transplant. 2009, 24, 643–646. [Google Scholar] [CrossRef]
- Naufel, M.F.; Bordon, M.; de Aquino, T.M.; Ribeiro, E.B.; de Abreu Carvalhaes, J.T. Plasma levels of acylated and total ghrelin in pediatric patients with chronic kidney disease. Pediatr. Nephrol. 2010, 25, 2477–2482. [Google Scholar] [CrossRef] [PubMed]
- Tong, J.; Dave, N.; Mugundu, G.M.; Davis, H.W.; Gaylinn, B.D.; Thorner, M.O.; Tschop, M.H.; D’Alessio, D.; Desai, P.B. The pharmacokinetics of acyl, des-acyl, and total ghrelin in healthy human subjects. Eur. J. Endocrinol. 2013, 168, 821–828. [Google Scholar] [CrossRef] [PubMed]
- Carrero, J.J. Mechanisms of altered regulation of food intake in chronic kidney disease. J. Ren. Nutr. 2011, 21, 7–11. [Google Scholar] [CrossRef]
- Muscaritoli, M.; Molfino, A.; Chiappini, M.G.; Laviano, A.; Ammann, T.; Spinsanti, P.; Melchiorri, D.; Inui, A.; Alegiani, F.; Rossi Fanelli, F. Anorexia in hemodialysis patients: The possible role of des-acyl ghrelin. Am. J. Nephrol. 2007, 27, 360–365. [Google Scholar] [CrossRef]
- Akamizu, T.; Kangawa, K. Therapeutic applications of ghrelin to cachexia utilizing its appetite-stimulating effect. Peptides 2011, 32, 2295–2300. [Google Scholar] [CrossRef]
- Ashby, D.R.; Ford, H.E.; Wynne, K.J.; Wren, A.M.; Murphy, K.G.; Busbridge, M.; Brown, E.A.; Taube, D.H.; Ghatei, M.A.; Tam, F.W.; et al. Sustained appetite improvement in malnourished dialysis patients by daily ghrelin treatment. Kidney Int. 2009, 76, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Wynne, K.; Giannitsopoulou, K.; Small, C.J.; Patterson, M.; Frost, G.; Ghatei, M.A.; Brown, E.A.; Bloom, S.R.; Choi, P. Subcutaneous ghrelin enhances acute food intake in malnourished patients who receive maintenance peritoneal dialysis: A randomized, placebo-controlled trial. J. Am. Soc. Nephrol. 2005, 16, 2111–2118. [Google Scholar] [CrossRef] [PubMed]
- Wofford, J.A.; Zollers, B.; Rhodes, L.; Bell, M.; Heinen, E. Evaluation of the safety of daily administration of capromorelin in cats. J. Vet. Pharmacol. Ther. 2018, 41, 324–333. [Google Scholar] [CrossRef]
- Serra-Prat, M.; Palomera, E.; Clave, P.; Puig-Domingo, M. Effect of age and frailty on ghrelin and cholecystokinin responses to a meal test. Am. J. Clin. Nutr. 2009, 89, 1410–1417. [Google Scholar] [CrossRef]
- Blatnik, M.; Soderstrom, C.I. A practical guide for the stabilization of acylghrelin in human blood collections. Clin. Endocrinol. 2011, 74, 325–331. [Google Scholar] [CrossRef]
- Tvarijonaviciute, A.; Martinez-Subiela, S.; Ceron, J.J. Influence of different storage conditions and anticoagulants on the measurement of total and acylated ghrelin in dogs: A preliminary study. Vet. Rec. 2013, 172, 289. [Google Scholar] [CrossRef] [PubMed]
- De Vriese, C.; Gregoire, F.; Lema-Kisoka, R.; Waelbroeck, M.; Robberecht, P.; Delporte, C. Ghrelin degradation by serum and tissue homogenates: Identification of the cleavage sites. Endocrinology 2004, 145, 4997–5005. [Google Scholar] [CrossRef] [PubMed]
- Lass, J.; Nielsen, M.L.; Bjornvad, C.R.; Vitger, A.D.; Cremer, S.E. Analytical performance of canine acylated and unacylated ghrelin enzyme-linked immunosorbent assays. Vet. Clin. Pathol. 2019, 48, 748–753. [Google Scholar] [CrossRef] [PubMed]
- Martin, L.J.; Siliart, B.; Lutz, T.A.; Biourge, V.; Nguyen, P.; Dumon, H.J. Postprandial response of plasma insulin, amylin and acylated ghrelin to various test meals in lean and obese cats. Br. J. Nutr. 2010, 103, 1610–1619. [Google Scholar] [CrossRef] [PubMed]

| Storage Time | EDTA Only | EA | EAH |
|---|---|---|---|
| 1 Month (n = 4) | 65.6 * (51.6–90.4) | 72.3 (52.9–100.2) | 87.7 * (69.5–114.6) |
| 3 Months (n = 5) | 44.4 * (23.7–56.5) | 44.8 (27.2–63.2) | 61.3 * (36.1–85.3) |
| 6 Months (n = 5) | 60.1 * (37.0–83.3) | 65.4 (44.8– 86.1) | 94.5 * (52.4–136.6) |
| Storage Time | EDTA Only (%) | EA (%) | EAH (%) |
|---|---|---|---|
| 1 Month (n = 4) | 76.2 * (70.4–78.9) | 86.4 (68.0–87.5) | 100 * |
| 3 Months (n = 5) | 66.3 * (62.7–80.3) | 75.3 (63.0–82.3) | 100 * |
| 6 Months (n = 5) | 65.7 * (61.0–70.5) | 74.2 (63.0–85.4) | 100 * |
| Normal (n = 12) | CKD (n = 12) | |
|---|---|---|
| Age (years) * | 5.5 (3.3–14.3) | 12.3 (10.0–19.0) |
| Weight (kilograms) * | 5.0 (3.3–6.3) | 3.8 (2.5–5.5) |
| Serum Creatinine (mg/dL) * | 1.3 (0.7–1.6) | 2.4 (1.6–3.4) |
| Total Ghrelin (pg/mL) * | 493.76 (414.68–627.66) | 667.26 (469.23–851.0) |
| Acylated Ghrelin (pg/mL) | 58.72 (24.02–129.62) | 62.21 (18.7–119.68) |
| Desacyl Ghrelin (pg/mL) * | 435.11 (410.29–731.31) | 604.05 (240.40–532.57) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brusach, K.; Lorbach, S.; Quimby, J.; Nijveldt, E.; Paschall, R.; Kinsella, H.; Parker, V.; Toribio, R. Measurement of Ghrelin as a Marker of Appetite Dysregulation in Cats with and without Chronic Kidney Disease. Vet. Sci. 2023, 10, 464. https://doi.org/10.3390/vetsci10070464
Brusach K, Lorbach S, Quimby J, Nijveldt E, Paschall R, Kinsella H, Parker V, Toribio R. Measurement of Ghrelin as a Marker of Appetite Dysregulation in Cats with and without Chronic Kidney Disease. Veterinary Sciences. 2023; 10(7):464. https://doi.org/10.3390/vetsci10070464
Chicago/Turabian StyleBrusach, Katelyn, Sarah Lorbach, Jessica Quimby, Eline Nijveldt, Rene Paschall, Hannah Kinsella, Valerie Parker, and Ramiro Toribio. 2023. "Measurement of Ghrelin as a Marker of Appetite Dysregulation in Cats with and without Chronic Kidney Disease" Veterinary Sciences 10, no. 7: 464. https://doi.org/10.3390/vetsci10070464
APA StyleBrusach, K., Lorbach, S., Quimby, J., Nijveldt, E., Paschall, R., Kinsella, H., Parker, V., & Toribio, R. (2023). Measurement of Ghrelin as a Marker of Appetite Dysregulation in Cats with and without Chronic Kidney Disease. Veterinary Sciences, 10(7), 464. https://doi.org/10.3390/vetsci10070464






