Development of an In Vivo Model for Eustachian Tube Dysfunction
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethic Statement
2.2. Hyaluronic Acid
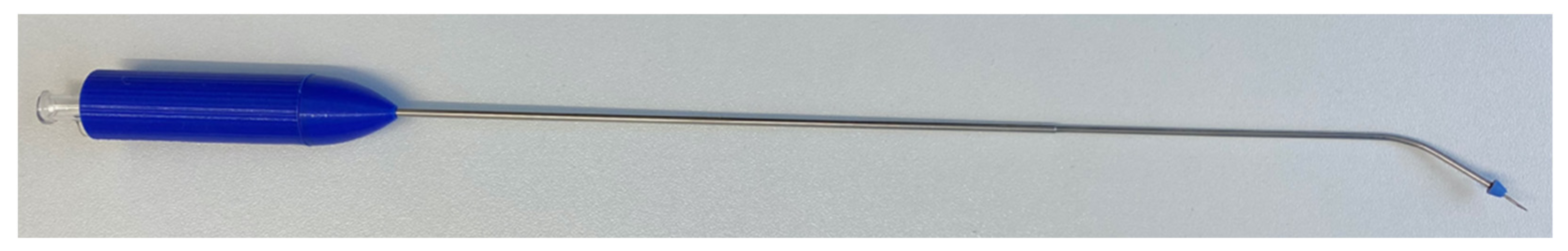
2.3. Injection Instrument
2.4. Ex Vivo Experiments
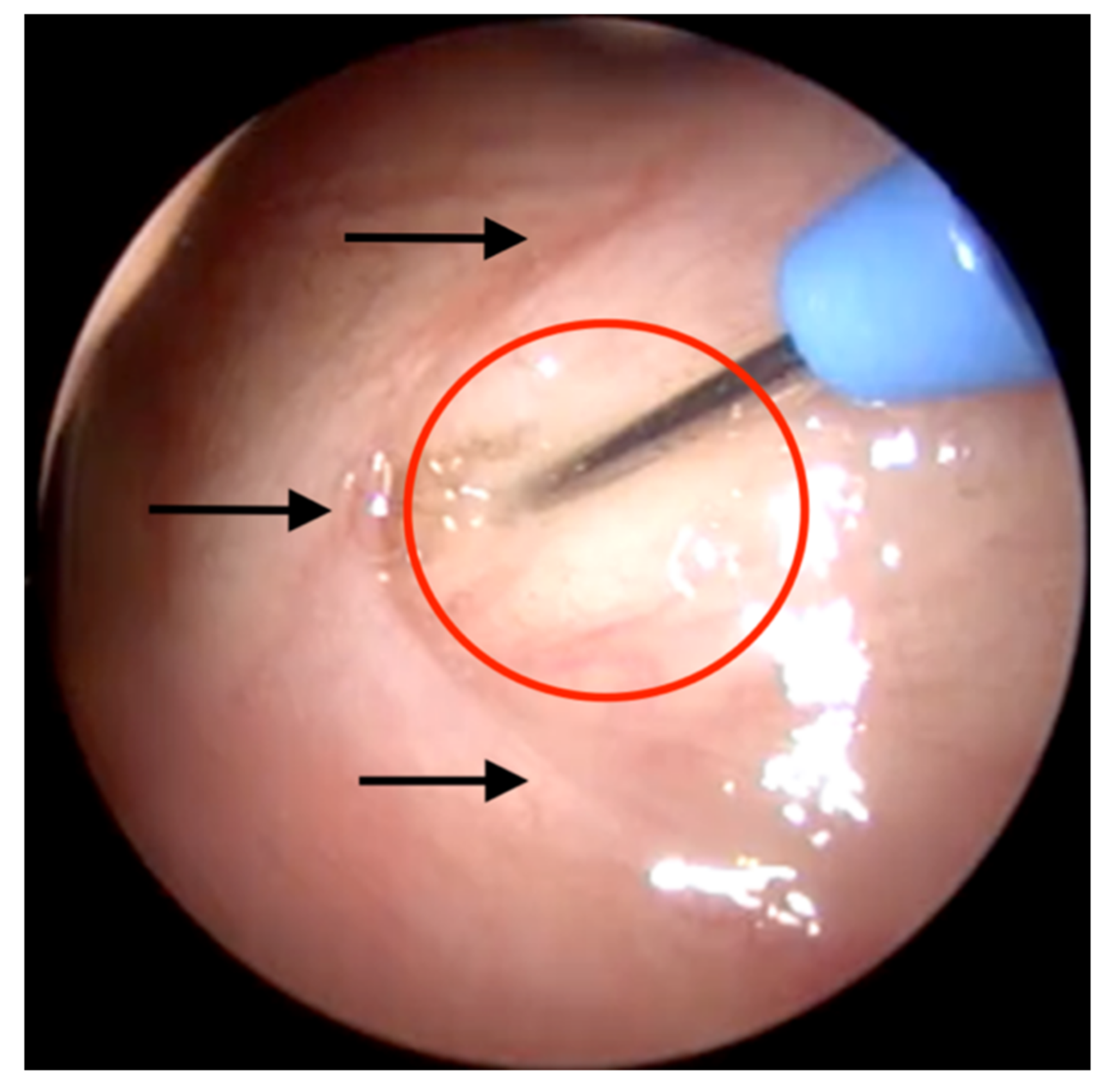
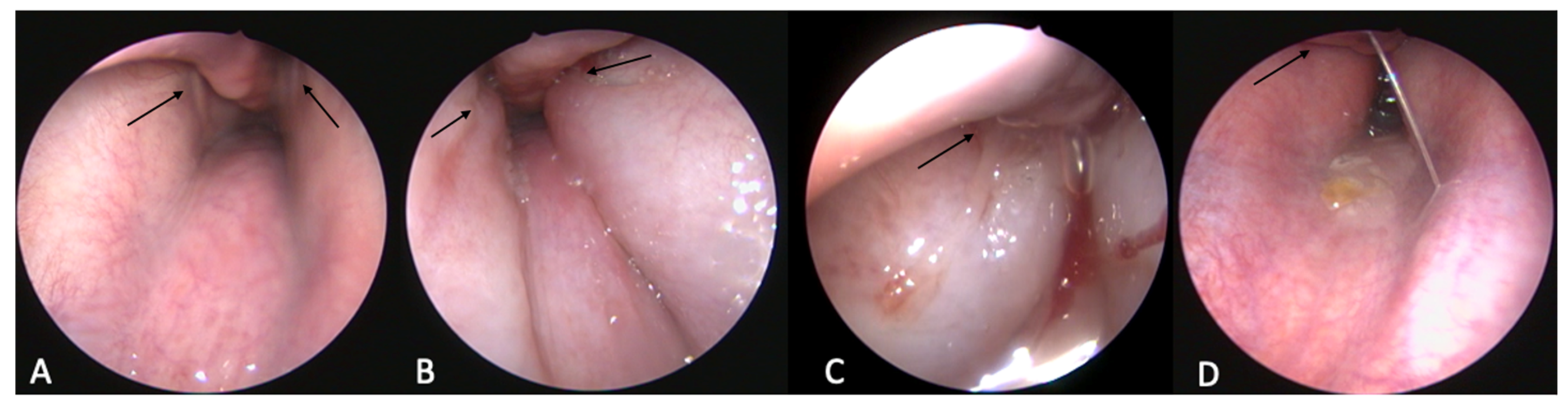
2.4.1. Endoscopic Procedure and HA Injection
| ET | HA [mL] | Insertion Angle | Insertion Side | Outflow of HA | CBCT/MRI |
|---|---|---|---|---|---|
| 1 | 0.3 | n/a | n/a | No | |
| 2 | 1 | n/a | n/a | No | |
| 3 | 0.3 | n/a | n/a | No | |
| 4 | 0.35 | 30° | Aligned | No | Good |
| 5 | 0.35 | 30° | Aligned | No | Good |
| 6 | 0.35 | 30° | Aligned | Yes | Good |
| 7 | 0.4 | 30° | Aligned | No | Good |
| 8 | 0.3 | 45° | Aligned | No | Good |
| 9 | 0.3 | 45° | Aligned | No | Good |
| 10 | 0.4 | 40° | Aligned | No | Good |
| 11 | 0.4 | 40° | Central slightly behind the entrance | No | Too nuchal |
| 12 | 0.3 | 40° | Aligned | Yes | Hardly visible |
| 13 | 0.3 | 40° | Aligned | No | Good |
| 14 | 0.3 | 40° | Aligned | No | Hardly visible |
| 15 | 0.65 | 40° | Approx. 2 mm further rostral | Yes | Good with rostral bulge |
| 16 | 0.3 | 50° | Central slightly behind the entrance | No | Good |
| 17 | 0.4 | 40° | Aligned | No | Good with rostral bulge |
| 18a | 0.3 | 40° | Aligned | No | Good |
| 18b | 0.3 + 0.75 | 40° | Aligned | No | Good with rostral bulge |
| 19a | 0.5 | 40° | Aligned | No | Good |
| 19b | 0.5 + 0.5 | 40° | Aligned | Yes | Good with rostral bulge |
| 20 | 0.2 | 40° | Approx. 4 mm further rostral | No | Just rostral of the ET |
| 21a | 0.4 | 40° | Aligned | No | Good |
| 21b | 0.4 + 0.2 | 40° | Approx. 2 mm further rostral | No | Good with a separate depot rostral |
| 22 | 1.2 (s) | 40° | Aligned | No | Good with rostral bulge (MRI) |
| 23 | 0.5 (s) | 40° | Aligned | No | Good (MRI) |
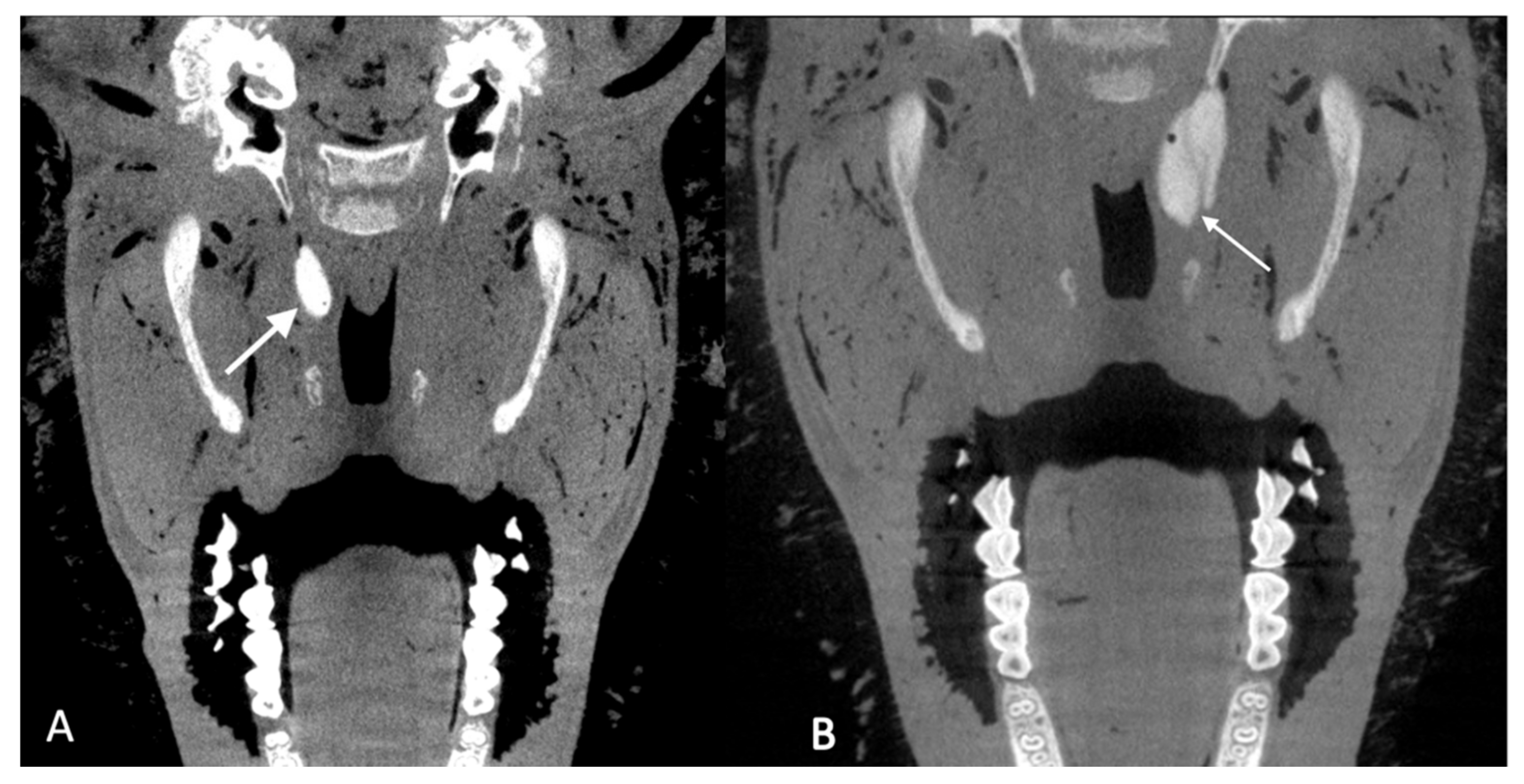
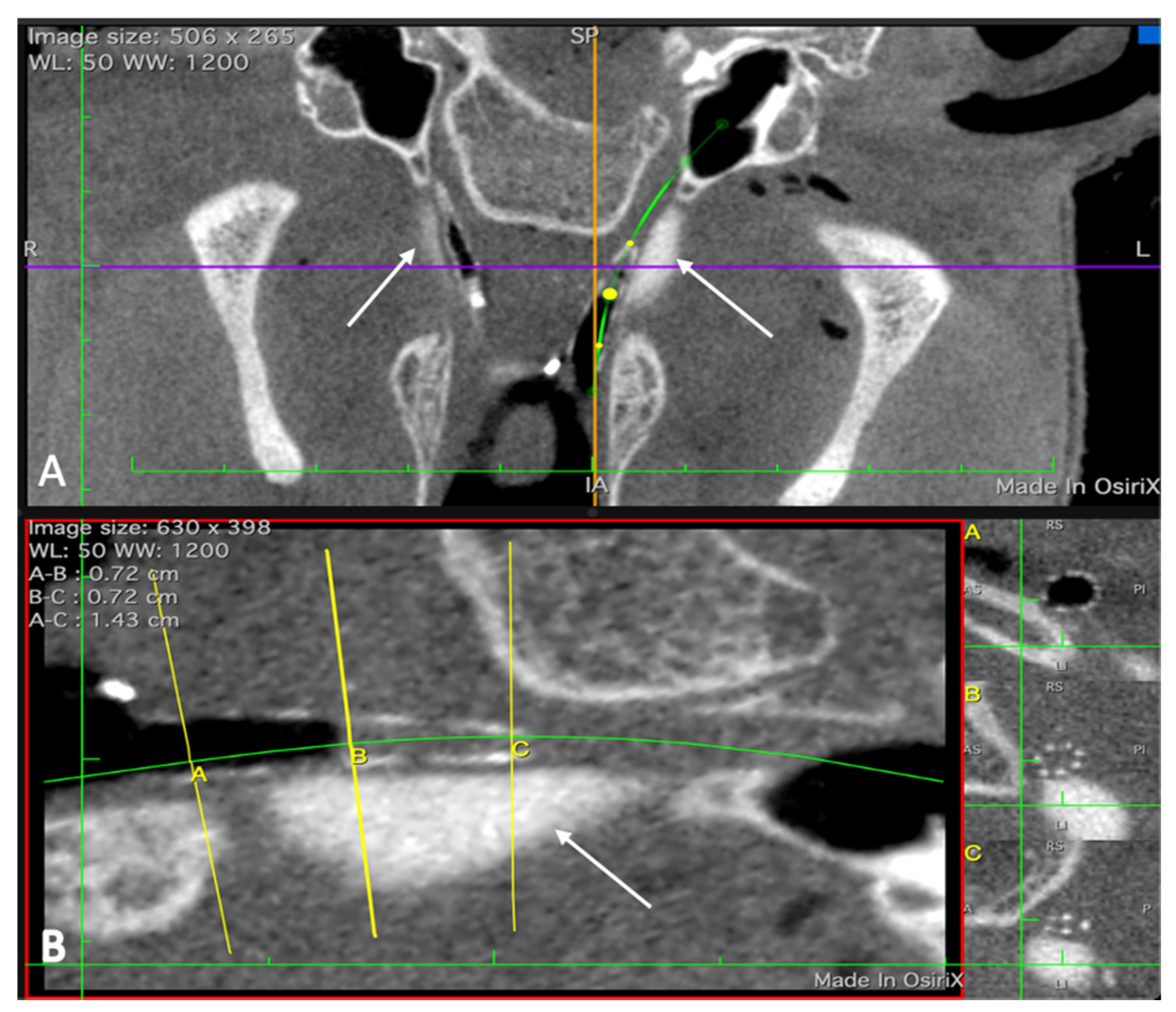
2.4.2. Imaging
2.4.3. Feasibility of Stent Insertion
2.5. In Vivo Experiments
2.5.1. Animals and Study Design
2.5.2. Cleaning the External Ear Canal
2.5.3. Tympanometry
2.5.4. Hyaluronic Acid Injection
2.5.5. Imaging
2.5.6. Health Score
3. Results
3.1. Ex Vivo Experiments
3.2. In Vivo Experiments
3.2.1. Injection of Non-Stabilized HA
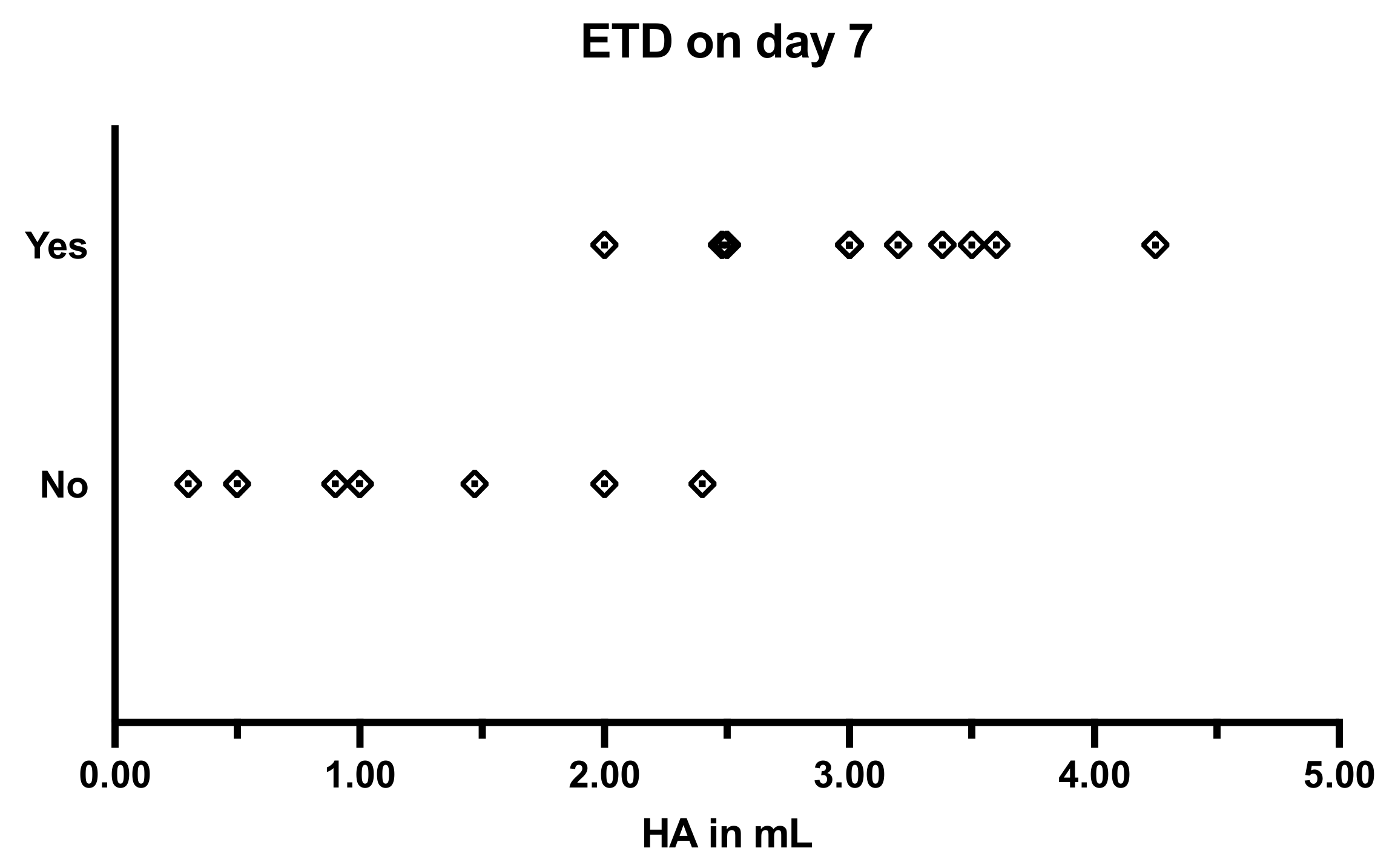
3.2.2. Injection of Stabilized HA
3.2.3. Tympanic Membrane
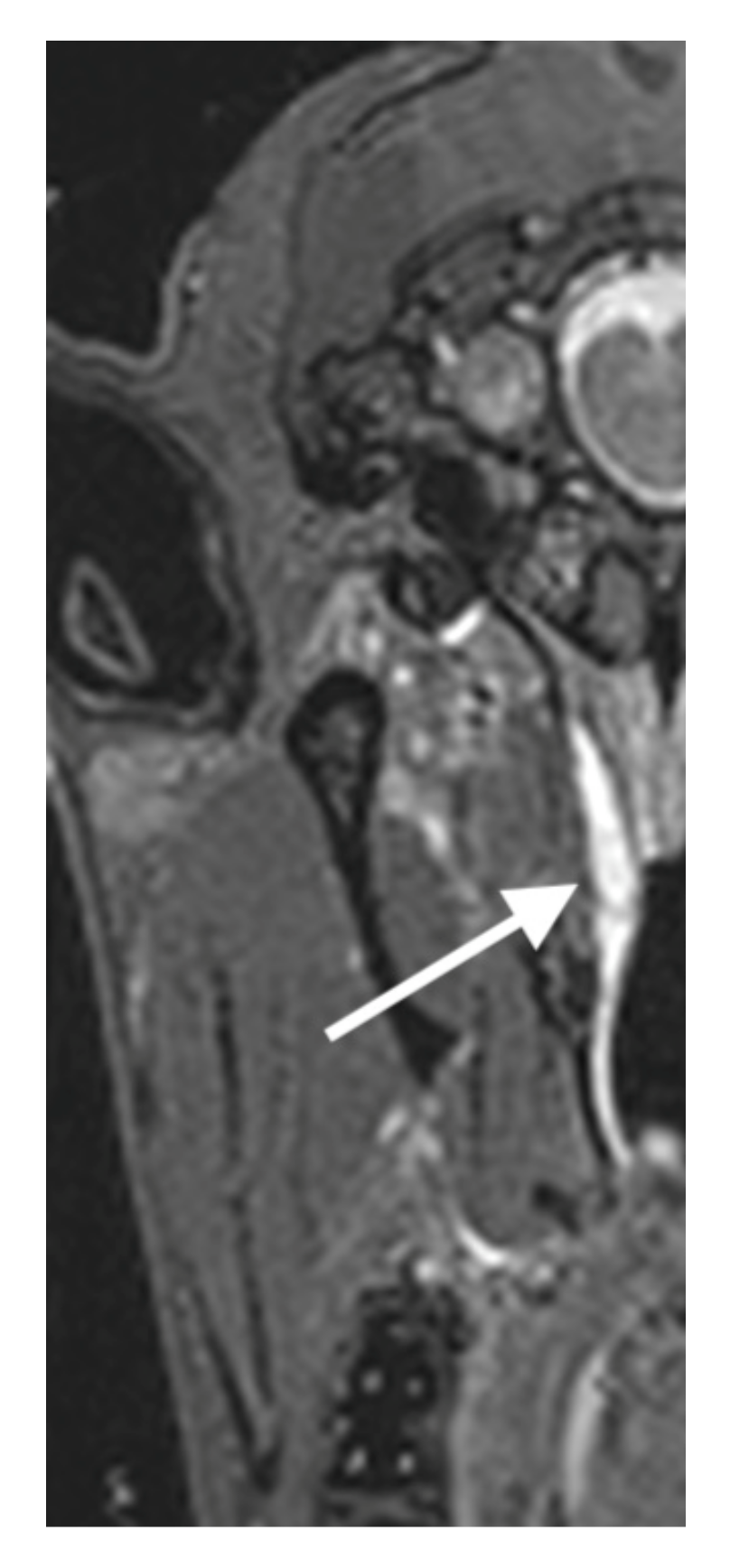
3.2.4. Imaging
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Category | Observed Behavior | Score |
|---|---|---|
| Vocalization | Occasional communication with each other | 0 |
| Occasional teeth grinding, sporadic snorting | 1 | |
| Frequent grinding of teeth, frequent snorting | 2 | |
| Moaning/sighing during expiration | 3 | |
| Activity | Sleeping, quietly standing or lying down | 0 |
| Frequent changes of position and attempts to stand up | 1 | |
| Restlessness (e.g., running around bleating) | 2 | |
| Feed/water intake | Normal, normal rumination | 0 |
| Only special food, moderate rumination | 1 | |
| No food intake, no rumination | 2 | |
| Behavior/facial expression | Interested in the environment, searches in the straw, head is carried straight | 0 |
| Depressed, dull, sporadic moderate head tilting and/or head shaking | 1 | |
| Flehming, absent staring, permanent head tilting and/or head shaking | 2 | |
| Breathing rate | Up to 25 breaths/min | 0 |
| 25–30% increase above normal | 0.5 | |
| More than 50% increase above normal | 1 | |
| Other abnormalities | None | 0 |
| Temperature increase, serous nasal discharge | 1 | |
| Fever, purulent nasal discharge, bloody nasal discharge | 2 |
References
- Lapsley, R.M. Diseases of the Middle Ear. Laryngoscope 1898, 5, 170–172. [Google Scholar] [CrossRef]
- Healy, G.B.; Rosbe, K.W. Otitis Media and Middle Ear Effusions. In Ballenger’s Otorhinolaryngology—Head and Neck Surgery, 16th ed.; Snow, J.B., Ballenger, J.J., Eds.; BC Decker Inc.: Hamilton, ON, Canada, 2003; pp. 249–260. ISBN 1550091972. [Google Scholar]
- Proctor, B. Embryology and Anatomy of the Eustachian Tube. Arch. Otolaryngol. 1967, 86, 503–514. [Google Scholar] [CrossRef] [PubMed]
- Leuwer, R.; Koch, U. Anatomie und Physiologie der Tuba Auditiva. HNO 1999, 47, 514–523. [Google Scholar] [CrossRef] [PubMed]
- Leuwer, R.; Schubert, R.; Wenzel, S.; Kucinski, T.; Koch, U.; Maier, H. Neue Aspekte zur Mechanik der Tuba Auditiva. HNO 2003, 51, 431–437. [Google Scholar] [CrossRef] [PubMed]
- Llewellyn, A.; Norman, G.; Harden, M.; Coatesworth, A.; Kimberling, D.; Schilder, A.; McDaid, C. Interventions for Adult Eustachian Tube Dysfunction: Asystematic Review. Health Technol. Assess. 2014, 18, 1–180. [Google Scholar] [CrossRef]
- Söderman, A.C.H.; Knutsson, J.; Priwin, C.; von Unge, M. A Randomized Study of Four Different Types of Tympanostomy Ventilation Tubes—One-Year Follow-Up. Int. J. Pediatric Otorhinolaryngol. 2016, 89, 159–163. [Google Scholar] [CrossRef]
- Todt, I.; Seidl, R.; Ernst, A. A New Minimally Invasive Method for the Transtubal, Microendoscopic Application of Fluids to the Middle Ear. Minim. Invasive Ther. Allied Technol. 2008, 17, 300–302. [Google Scholar] [CrossRef]
- Zöllner, F. The Principles of Plastic Surgery of the Sound-Conducting Apparatus. J. Laryngol. Otol. 1955, 69, 637–652. [Google Scholar] [CrossRef]
- Poe, D.S.; Grimmer, J.F.; Metson, R. Laser Eustachian Tuboplasty: Two-Year Results. Laryngoscope 2007, 117, 231–237. [Google Scholar] [CrossRef]
- Poe, D.S.; Hanna, B.M.N. Balloon Dilation of the Cartilaginous Portion of the Eustachian Tube: Initial Safety and Feasibility Analysis in a Cadaver Model. Am. J. Otolaryngol. 2011, 32, 115–123. [Google Scholar] [CrossRef]
- Ockermann, T.; Reineke, U.; Upile, T.; Ebmeyer, J.; Sudhoff, H.H. Balloon Dilatation Eustachian Tuboplasty: A Clinical Study. Laryngoscope 2010, 120, 1411–1416. [Google Scholar] [CrossRef] [PubMed]
- Schnabl, J.; Glueckert, R.; Feuchtner, G.; Recheis, W.; Potrusil, T.; Kuhn, V.; Wolf-Magele, A.; Riechelmann, H.; Sprinzl, G.M. Sheep as a Large Animal Model for Middle and Inner Ear Implantable Hearing Devices. Otol. Neurotol. 2012, 33, 481–489. [Google Scholar] [CrossRef] [PubMed]
- Miller, F.; Burghard, A.; Salcher, R.; Scheper, V.; Leibold, W.; Lenarz, T.; Paasche, G. Treatment of Middle Ear Ventilation Disorders: Sheep as Animal Model for Stenting the Human Eustachian Tube—A Cadaver Study. PLoS ONE 2014, 9, e113906. [Google Scholar] [CrossRef] [PubMed]
- Pohl, F.; Schuon, R.A.; Miller, F.; Kampmann, A.; Bültmann, E.; Hartmann, C.; Lenarz, T.; Paasche, G. Stenting the Eustachian Tube to Treat Chronic Otitis Media—A Feasibility Study in Sheep. Head Face Med. 2018, 14, 8. [Google Scholar] [CrossRef]
- Russell, J.D.; Giles, S.J. Persistent Otitis Media with Effusion: A New Experimental Model. Laryngoscope 1998, 108, 1181–1184. [Google Scholar] [CrossRef]
- Piltcher, O.B.; Swarts, J.D.; Magnuson, K.; Alper, C.M.; Doyle, W.J.; Hebda, P.A. A Rat Model of Otitis Media with Effusion Caused by Eustachian Tube Obstruction with and without Streptococcus pneumoniae Infection: Methods and Course. Otolaryngol. Head Neck Surg. 2002, 126, 490–498. [Google Scholar] [CrossRef]
- Doyle, W.J. Functional Eustachian Tube Obstruction and Otitis Media in a Primate Model: A Review. Acta Oto-Laryngol. 1984, 98, 52–57. [Google Scholar] [CrossRef]
- Aynali, G.; Yariktaş, M.; Yasan, H.; Karahan, N.; Başpinar, Ş.; Tüz, M.; Gümüş, S. The Effects of Methylprednisolone, Montelukast and Indomethacine in Experimental Otitis Media with Effusion. Int. J. Pediatric Otorhinolaryngol. 2011, 75, 15–19. [Google Scholar] [CrossRef]
- Kerschner, J.E.; Hong, W.; Taylor, S.R.; Kerschner, J.A.; Khampang, P.; Wrege, K.C.; North, P.E. A Novel Model of Spontaneous Otitis Media with Effusion (OME) in the Oxgr1 Knock-out Mouse. Int. J. Pediatric Otorhinolaryngol. 2013, 77, 79–84. [Google Scholar] [CrossRef][Green Version]
- Rhee, C.K.; Jung, T.T.K.; Miller, S.; Weeks, D. Experimental Otitis Media with Effusion Induced by Platelet Activating Factor. Ann. Otol. Rhinol. Laryngol. 1993, 102, 600–605. [Google Scholar] [CrossRef]
- Ganbo, T.; Hisamatsu, K.I.; Kikushima, K.; Nakajima, M.; Inoue, H.; Murakami, Y. Effects of Platelet Activating Factor on Mucociliary Clearance of the Eustachian Tube. Ann. Otol. Rhinol. Laryngol. 1996, 105, 140–145. [Google Scholar] [CrossRef] [PubMed]
- Welsh, E. Hyaluronic Acid Fillers. Synop. Aesthetic Dermatol. Cosmet. Surg. 2013, 19, 177–192. [Google Scholar] [CrossRef]
- Tezel, A.; Fredrickson, G.H. The Science of Hyaluronic Acid Dermal Fillers. J. Cosmet. Laser Ther. 2008, 10, 35–42. [Google Scholar] [CrossRef]
- Hartog, F.J. Clinical Results of the Treatment of Patulous Eustachian Tube Byaugmentation of the Epipharyngeal Tubal Ostium with Hyaluronic Acid. Ph.D. Thesis, Universitätsklinikum Hamburg-Eppendorf, Hamburg, Germany, 2018. [Google Scholar]
- Weber, G.C.; Buhren, B.A.; Schrumpf, H.; Wohlrab, J.; Gerber, P.A. Clinical Applications of Hyaluronidase. In Therapeutic Enzymes: Function and Clinical Implications; Advances in Experimental Medicine and Biology Series; Springer: Berlin/Heidelberg, Germany, 2019; Volume 1148, pp. 255–277. ISBN 9789811377082. [Google Scholar]
- Pohl, F.; Paasche, G.; Lenarz, T.; Schuon, R. Tympanometric Measurements in Conscious Sheep—A Diagnostic Tool for Pre-Clinical Middle Ear Implant Studies. Int. J. Audiol. 2017, 56, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Gelfand, S.A. Essentials of Audiology; Georg Thieme Verlag: Stuttgart, Germany, 2016; ISBN 9781604068627. [Google Scholar]
- Schröder, S.; Reineke, U.; Lehmann, M.; Ebmeyer, J.; Sudhoff, H. Chronisch Obstruktive Tubenfunktionsstörung des Erwachsenen. HNO 2013, 61, 142–151. [Google Scholar] [CrossRef]
- Schuon, R.; Schwarzensteiner, J.; Paasche, G.; Lenarz, T.; John, S. Functional Aspects of the Eustachian Tube by Means of 3D-Modeling. PLoS ONE 2021, 16, e0244909. [Google Scholar] [CrossRef]
- Trinh, L.N.; Gupta, A. Hyaluronic Acid Fillers for Midface Augmentation: A Systematic Review. Facial Plast. Surg. 2021, 37, 576–584. [Google Scholar] [CrossRef]
- Halderman, A.A.; Bryson, P.C.; Benninger, M.S.; Chota, R. Safety and Length of Benefit of Restylane for Office-Based Injection Medialization-a Retrospective Review of One Institution’s Experience. J. Voice 2014, 28, 631–635. [Google Scholar] [CrossRef]
- McDonald, M.H.; Hoffman, M.R.; Gentry, L.R.; Jiang, J.J. New Insights into Mechanism of Eustachian Tube Ventilation Based on Cine Computed Tomography Images. Eur. Arch. Oto-Rhino-Laryngol. 2012, 269, 1901–1907. [Google Scholar] [CrossRef][Green Version]
- Park, M.K.; Lee, B.D. Development of Animal Models of Otitis Media. Korean J. Audiol. 2013, 17, 9–12. [Google Scholar] [CrossRef]



| ET Case | HA [mL] | Bending Angle | Insertion Point | Insertions Needed | Outflow of HA | Protrusion |
|---|---|---|---|---|---|---|
| 1 | 0.3 | 45° | Aligned | 1 | No | 0 |
| 2 | 0.5 | 50° | Aligned | 2 | No | 1 |
| 3 | 0.5 | 50° | Centrally behind the entrance | 2 | No | 0 |
| 4 | 0.9 | 50° | Aligned | 3 | Yes | 1 |
| 5 | 1 | 45° | Aligned | 1 | No | 1 |
| Days and Respective Tympanometric Measurement Results | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case 1 (0.3 mL HA) | −7 | 0 | 1 | 5 | 12 | 19 | 26 | 36 | 40 | 47 | 54 | 61 | 68 | 77 | |||
| A | A | A | A | A | A | A | A | A | A | A | A | A | A | ||||
| Case 2 (0.5 mL HA) | −7 | −5 | 1 | 3 | 7 | 9 | 14 | 17 | 21 | 31 | 35 | 42 | 49 | 56 | 63 | 72 | 77 |
| A | A | A | A | B* | B* | A | A | A | A | A | A | A | A | A | A | A | |
| Case 3 (0.5 mL HA) | −6 | −1 | 1 | 3 | 6 | 13 | 20 | 30 | 34 | 41 | 48 | 55 | 62 | 71 | 76 | 83 | 90 |
| A | A | A | A | A | A | A | A | A | A | A | A | A | A | A | A | A | |
| −7 | −4 | 0 | 1 | 3 | 10 | 14 | 21 | 28 | 35 | 42 | 51 | 56 | 63 | 70 | 78 | ||
| Case 4 (0.9 mL HA) | A | A | A | A | A | A | A | A | A | A | A | A | A | A | A | A | |
| Case 5 (1.0 mL HA) | A | A | C | C | A | A | C | A | A | A | A | A | A | A | A | A | |
| ET Case | Observation [Weeks] | HA [mL] | Bending Angle | Insertion Point | Insertions Needed | Outflow of HA | Protrusion | Protrusion w 1 | Protrusion w 7 | Protrusion w 13 (12) | TM w 1 | TM w 7 | TM w 13 (12) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 6 | 13 | 1 | 50° | Slightly inside the ET | 1 | No | 1 | n/a | n/a | n/a | n/a | n/a | n/a |
| 7 | 12 | 3 | 35° | Distributed at the entrance | 6 | Yes | 3 | 3 (day 14) | n/a | 1 | Phys. (day 14) | n/a | Phys. |
| 8 | 13 | 1.47 | 40° | Aligned | 4 | Yes | 1 | 1 | 1 | 1 | Phys. | Phys. | Phys. |
| 9 | 1 | 2.48 | 40° | Aligned | 2 | Yes | 2 | 1 | n/a | n/a | Bulg. | n/a | n/a |
| 10 | 13 | 3.38 | 25° | Aligned | 1 | No | 3 | 3 | 1 | 1 | Rupt. | Bulg. | Bulg. |
| 11 | 1 | 4.25 | 25° | Dorsally aligned | 1 | Yes | 3 | 3 | n/a | n/a | Bulg. | n/a | n/a |
| 12 | 1 | 3.5 | 20° | Aligned | 1 | Yes | 2 | 3 | n/a | n/a | Bulg. | n/a | n/a |
| 13 | 13 | 3 | 20° | Aligned | 1 | No | 2 | 3 | 0 | 0 | Bulg. | Bulg. | Bulg. |
| 14 | 13 | 3.65 | 20° | Aligned | 3 | Yes | 2 | 3 | 1 | 1 | Phys. | Bulg. | Phys. |
| 15 | 1 | 3 | 30° | Aligned | 1 | No | 2 | 3 | n/a | n/a | Phys. | n/a | n/a |
| 16 | 1 | 2.5 | 25° | Aligned | 1 | No | 2 | 3 | n/a | n/a | Phys. | n/a | n/a |
| 17 | 13 | 2.4 | 25° | Aligned | 1 | No | 3 | 3 | 1 | 1 | Phys. | Phys. | Phys. |
| 18 | 1 | 2 | 25° | Aligned | 1 | No | 2 | 3 | n/a | n/a | Phys. | n/a | n/a |
| 19 | 13 | 2 | 30° | Aligned | 1 | No | 2 | 3 | 2 | 2 | Phys. | Phys. | Phys. |
| 20 | 1 | 3 | 30° | Aligned | 1 | Yes | 3 | 3 | n/a | n/a | Phys. | n/a | n/a |
| 21 | 13 | 3 | 40° | Aligned | 1 | Yes | 3 | 2 | 2 | 0 | Bulg. | Phys. | Phys. |
| 22 | 1 | 3.2 | 40° | Aligned | 1 | No | 3 | 2 | n/a | n/a | Phys. | n/a | n/a |
| Days and Respective Tympanometric Mesurement Results | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case 6 (1.0 mL HA) | −7 | −1 | 0 | 1 | 2 | 5 | 6 | 7 | 8 | 9 | 12 | 13 | 14 | 21 | 26 | 27 | 33 | 40 | 48 | 54 | 64 | 68 | 75 | 82 |
| A | A | A | A | C | A | C | A | A | A | A | A | A | A | C | C | A | A | A | A | A | A | A | A | |
| Case 7 (3.0 mL HA) | −7 | −3 | 0 | 1 | 2 | 3 | 4 | 5 | ←→ | 32 | 35 | 37 | 39 | 42 | 44 | 46 | 49 | 51 | 53 | 56 | 63 | 70 | 77 | |
| A | A | C | C | C | C | C | B | B | B | B | A | C | C | A | A | A | B | C | A | A | C | B | A | |
| −10 | −3 | 1 | 2 | 3 | 4 | 5 | 6 | 8 | 9 | 10 | 11 |  | 90 | |||||||||||
| Case 8 (1.47 mL HA) | A | A | A | A | A | C | C | A | A | A | A | A | A | A | A | A | A | A | A | A | A | A | A | A |
| Case 9 (2.48 mL HA) | A | A | C | C | C | A | A | B | ||||||||||||||||
| Case 10 (3.38 mL HA) | A | A | C | C | C | C | B | B | B | B | B | B | B | B | B | B | B | B | B | B | B | B | B | B |
| Case 11 (4.25 mL HA) | A | A | C | C | C | C | B | B | ||||||||||||||||
| −8 | −1 | 1 | 2 | 3 | 4 | 5 | 6 | 8 | 9 | 10 | 11 | 12 | 13 | 14 |  | 87 | ||||||||
| Case 12 (3.5 mL HA) | A | A | C | C | C | C | C | C | ||||||||||||||||
| Case 13 (3.0 mL HA) | A | A | C | C | C | C | C | C | C | C | C | C | C | B | B | B | B | B | B | B | B | B | B | B |
| −8 | −1 | 1 | 2 | 3 |  | 57 | 59 | 62 | 64 | 66 | 69 | 71 | 73 | 76 | 78 | 80 | 83 | 85 | 87 | |||||
| Case 14 (3.65 mL HA) | A | A | C | C | B | B | B | B | B | B | C | C | C | A | A | A | C | A | A | A | A | A | A | A |
| Case 15 (3.0 mL HA) | A | A | A | A | C | A | B | B | ||||||||||||||||
| −7 | −1 | 1 | 3 | 6 | 7 | 8 | 10 | 13 |  | 90 | ||||||||||||||
| Case 16 (2.5 mL HA) | A | A | C | C | B | B | ||||||||||||||||||
| Case 17 (2.4 mL HA) | A | A | C | C | A | A | A | A | A | A | A | A | A | A | A | A | A | A | A | A | A | A | A | A |
| −7 | −1 | 1 | 3 | 6 | 7 | 8 | ←→ | 34 | 36 | 37 | 41 | 43 | ←→ | 64 | 66 | 69 |  | 90 | ||||||
| Case 18 (2.0 mL HA) | A | A | C | C | B | B | ||||||||||||||||||
| Case 19 (2.0 mL HA) | A | A | C | A | A | A | A | A | A | A | C | A | C | A | A | A | A | C | A | A | A | A | A | A |
| Case 20 (3.0 mL HA) | −14 | −7 | 1 | 2 | 4 | 7 | ||||||||||||||||||
| A | A | B | B | B | B | |||||||||||||||||||
| −4 | −3 | 1 | 2 | 4 | 7 | 9 | 11 | 14 | 47 | 18 | 21 | 23 | 25 | 28 | 30 | ←→ | 74 | 77 | 79 | ←→ | 88 | |||
| Case 21 (3.0 mL HA) | A | A | C | C | B | B | B | B | B | B | B | A | A | A | B | A | A | A | A | C | A | A | A | A |
| Case 22 (3.2 mL HA) | A | A | C | B | B | B | ||||||||||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oppel, N.; Ezzat, M.; Krüger, P.; Schmitt, K.; Napp, A.; Pohl, F.; Bleich, A.; Lenarz, T.; Stein, T.; Paasche, G.; et al. Development of an In Vivo Model for Eustachian Tube Dysfunction. Bioengineering 2022, 9, 317. https://doi.org/10.3390/bioengineering9070317
Oppel N, Ezzat M, Krüger P, Schmitt K, Napp A, Pohl F, Bleich A, Lenarz T, Stein T, Paasche G, et al. Development of an In Vivo Model for Eustachian Tube Dysfunction. Bioengineering. 2022; 9(7):317. https://doi.org/10.3390/bioengineering9070317
Chicago/Turabian StyleOppel, Niels, Malena Ezzat, Philipp Krüger, Katharina Schmitt, Alexandra Napp, Friederike Pohl, Andre Bleich, Thomas Lenarz, Tobias Stein, Gerrit Paasche, and et al. 2022. "Development of an In Vivo Model for Eustachian Tube Dysfunction" Bioengineering 9, no. 7: 317. https://doi.org/10.3390/bioengineering9070317
APA StyleOppel, N., Ezzat, M., Krüger, P., Schmitt, K., Napp, A., Pohl, F., Bleich, A., Lenarz, T., Stein, T., Paasche, G., & Schuon, R. (2022). Development of an In Vivo Model for Eustachian Tube Dysfunction. Bioengineering, 9(7), 317. https://doi.org/10.3390/bioengineering9070317






