Telehealth and Burn Care: From Faxes to Augmented Reality
Abstract
1. Introduction
2. Background
2.1. Cameras and Facsimiles
2.2. Hand-Held Phone and Application-Based Technology
2.3. Shared Electronic Medical Record and Cloud-Based Services
2.4. Video-Based Burn Tele-Medicine
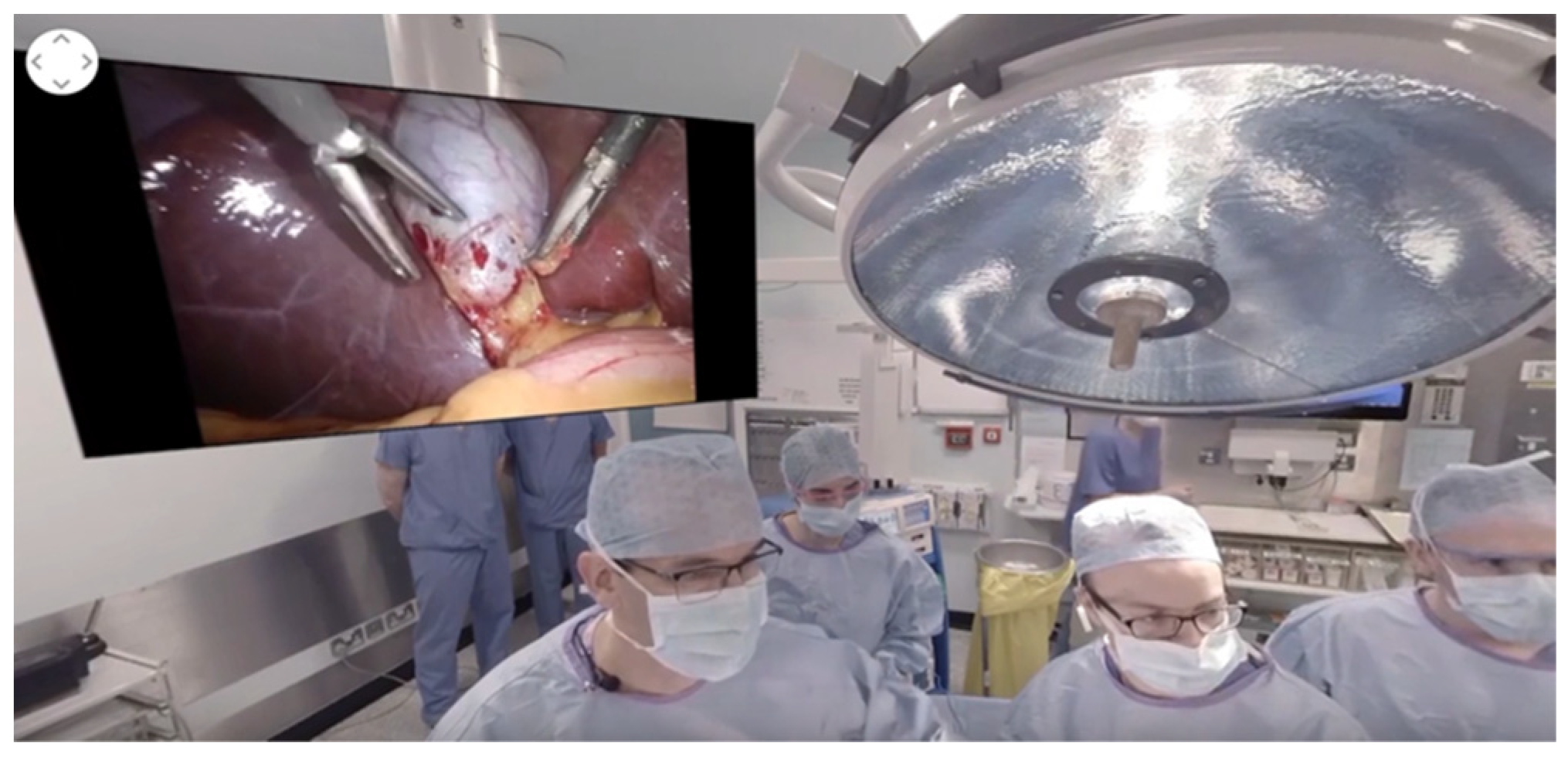
2.5. Augmented Reality and Hands-Free Telemedicine
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Boissin, C.; Laflammet, L.; Wallis, L.; Fleming, J.; Hasselberg, M. Photograph-based diagnosis of burns in patients with dark-skin types: The importance of case and assessor characteristics. Burns 2015, 41, 1253–1260. [Google Scholar] [CrossRef] [PubMed]
- Hop, M.J.; Moues, C.; Bogomolova, K.; Nietuwenhuis, M.; Oen, I.; Middelkoop, E.; Breederveld, R.; valn Baar, M. Photographic assessment of burn size and depth: Reliability and validity. J. Wound Care 2014, 23, 144–152. [Google Scholar] [CrossRef] [PubMed]
- Parvizi, D.; Giretzlehner, M.; Dirnberger, J.; Owen, R.; Haller, H.L.; Schintler, M.V.; Wurzer, P.; Lumenta, D.B.; Kamolz, L.P. The use of telemedicine in burn care: Development of a mobile system for TBSA documentation and remote assessment. Ann. Burns Fire Disasters 2014, 27, 94–100. [Google Scholar] [PubMed]
- Holt, B.; Faraklas, I.; Theurer, L.; Cochran, A.; Saffle, J.R. Telemedicine use among burn centers in the United States: A survey. J. Burn Care Res. 2012, 33, 157–162. [Google Scholar] [CrossRef]
- Jones, S.M.; Banwell, P.E.; Shakespeare, P.G. Telemedicine in wound healing. Int. Wound J. 2004, 1, 225–230. [Google Scholar] [CrossRef]
- Saffle, J.R.; Edelman, L.; Theurer, L.; Morris, S.E.; Cochran, A. Telemedicine evaluation of acute burns is accurate and cost-effective. J. Trauma 2009, 67, 358–365. [Google Scholar] [CrossRef]
- Garber, R.N.; Garcia, E.; Goodwin, C.W.; A Deeter, L. Pictures Do Influence the Decision to Transfer: Outcomes of a Telemedicine Program Serving an Eight-State Rural Population. J. Burn Care Res. 2020, 41, 690–694. [Google Scholar] [CrossRef]
- Crowther, J.B.; Poropatich, R. Telemedicine in the U.S. Army: Case reports from Somalia and Croatia. Telemed. J. 1995, 1, 73–80. [Google Scholar] [CrossRef]
- Carmichael, H.; Dyamenahalli, K.; Duffy, P.S.; Lambert Wagner, A.; Wiktor, A.J. Triage and Transfer to a Regional Burn Center-Impact of a Mobile Phone App. J. Burn Care Res. 2020, 41, 971–975. [Google Scholar] [CrossRef]
- den Hollander, D.; Mars, M. Smart phones make smart referrals: The use of mobile phone technology in burn care—A retrospective case series. Burns 2017, 43, 190–194. [Google Scholar] [CrossRef]
- Martinez, R.; Rogers, A.; Numanoglu, A.; Rode, H. The value of WhatsApp communication in paediatric burn care. Burns 2018, 44, 947–955. [Google Scholar] [CrossRef] [PubMed]
- Basaran, A.; Ozlu, O.; Das, K. Telemedicine in burn patients: Reliability and patient preference. Burns 2021, 47, 1873–1877. [Google Scholar] [CrossRef] [PubMed]
- Mars, M.; Scott, R.E. Being Spontaneous: The Future of Telehealth Implementation? Telemed. J. E Health 2017, 23, 766–772. [Google Scholar] [CrossRef] [PubMed]
- Jones, S.M.; Milroy, C.; Pickford, M.A. Telemedicine in acute plastic surgical trauma and burns. Ann. R. Coll. Surg. Engl. 2004, 86, 239–242. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wang, J.; Huang, J.; Cheung, C.S.K.; Wong, W.N.; Cheung, N.T.; Wong, M.C. Adoption of an Electronic Patient Record Sharing Pilot Project: Cross-Sectional Survey. J. Med. Internet Res. 2020, 22, e13761. [Google Scholar] [CrossRef] [PubMed]
- Wright, S.; Spaulding, R.; Henley, W. A Multipronged Digital Response to Increased Demand for Telehealth Support and Training During the COVID-19 Pandemic. J. Technol. Behav. Sci. 2021, 7, 73–80. [Google Scholar] [CrossRef]
- Wibbenmeyer, L.; Kluesner, K.; Wu, H.; Eid, A.; Heard, J.; Mann, B.; Pauley, A.; Peek-Asa, C. Video-Enhanced Telemedicine Improves the Care of Acutely Injured Burn Patients in a Rural State. J. Burn Care Res. 2016, 37, e531–e538. [Google Scholar] [CrossRef]
- Hickey, S.; Gomez, J.; Meller, B.; Schneider, J.C.; Cheney, M.; Nejad, S.; Schulz, J.; Goverman, J. Interactive home telehealth and burns: A pilot study. Burns 2017, 43, 1318–1321. [Google Scholar] [CrossRef]
- Peters, T.M. (Ed.) Mixed and Augmented Reality in Medicine; CRC Press: Raton, NM, USA, 2019. [Google Scholar]
- Ye, J.; Zuo, Y.; Xie, T.; Wu, M.; Ni, P.; Kang, Y.; Yu, X.; Sun, X.; Huang, Y.; Lu, S. A telemedicine wound care model using 4G with smart phones or smart glasses: A pilot study. Medicine 2016, 95, e4198. [Google Scholar] [CrossRef]
- Ahmed, N.; Devitt, K.S.; Keshet, I.; Spicer, J.; Imrie, K.; Feldman, L.; Cools-Lartigue, J.; Kayssi, A.; Lipsman, N.; Elmi, M.; et al. A systematic review of the effects of resident duty hour restrictions in surgery: Impact on resident wellness, training, and patient outcomes. Ann. Surg. 2014, 259, 1041–1053. [Google Scholar] [CrossRef]
- Park, C.; Grant, J.; Dumas, R.P.; Dultz, L.; Shoultz, T.H.; Scott, D.J.; Luk, S.; Abdelfattah, K.R.; Cripps, M. Does simulation work? Monthly trauma simulation and procedural training are associated with decreased time to intervention. J. Trauma Acute Care Surg. 2020, 88, 242–248. [Google Scholar] [CrossRef] [PubMed]
- Botden, S.M.; Buzink, S.N.; Schijven, M.P.; Jakimowicz, J.J. Augmented versus virtual reality laparoscopic simulation: What is the difference? A comparison of the ProMIS augmented reality laparoscopic simulator versus LapSim virtual reality laparoscopic simulator. World J. Surg. 2007, 31, 764–772. [Google Scholar] [CrossRef] [PubMed]
- Samosky, J.T.; Baillargeon, E.; Bregman, R.; Brown, A.; Chaya, A.; Enders, L.; A Nelson, D.; Robinson, E.; Sukits, A.L.; A Weaver, R. Real-time “x-ray vision” for healthcare simulation: An interactive projective overlay system to enhance intubation training and other procedural training. Stud. Health Technol. Inf. 2011, 163, 549–551. [Google Scholar]
- Andersen, D.; Popescu, V.; Cabrera, M.E.; Shanghavi, A.; Mullis, B.; Marley, S.; Gomez, G.; Wachs, J.P. An Augmented Reality-Based Approach for Surgical Telementoring in Austere Environments. Mil. Med. 2017, 182, 310–315. [Google Scholar] [CrossRef][Green Version]
- McWilliams, T.; Hendricks, J.; Twigg, D.; Wood, F.; Giles, M. Telehealth for paediatric burn patients in rural areas: A retrospective audit of activity and cost savings. Burns 2016, 42, 1487–1493. [Google Scholar] [CrossRef]
- Massman, N.J.; Dodge, J.D.; Fortman, K.K.; Schwartz, K.J.; Solem, L.D. Burns follow-up: An innovative application of telemedicine. J. Telemed. Telecare 1999, 5 (Suppl. S1), S52–S54. [Google Scholar] [CrossRef]
- Huang, E.Y.; Knight, S.; Guetter, C.R.; Davis, C.; Moller, M.; Slama, E.; Crandall, M. Telemedicine and telementoring in the surgical specialties: A narrative review. Am. J. Surg. 2019, 218, 760–766. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, C.; Cho, Y.; Harvey, J.; Arnoldo, B.; Levi, B. Telehealth and Burn Care: From Faxes to Augmented Reality. Bioengineering 2022, 9, 211. https://doi.org/10.3390/bioengineering9050211
Park C, Cho Y, Harvey J, Arnoldo B, Levi B. Telehealth and Burn Care: From Faxes to Augmented Reality. Bioengineering. 2022; 9(5):211. https://doi.org/10.3390/bioengineering9050211
Chicago/Turabian StylePark, Caroline, Youngwoo Cho, Jalen Harvey, Brett Arnoldo, and Benjamin Levi. 2022. "Telehealth and Burn Care: From Faxes to Augmented Reality" Bioengineering 9, no. 5: 211. https://doi.org/10.3390/bioengineering9050211
APA StylePark, C., Cho, Y., Harvey, J., Arnoldo, B., & Levi, B. (2022). Telehealth and Burn Care: From Faxes to Augmented Reality. Bioengineering, 9(5), 211. https://doi.org/10.3390/bioengineering9050211





