Plate Augmentation in Aseptic Femoral Shaft Nonunion after Intramedullary Nailing: A Literature Review
Abstract
1. Introduction
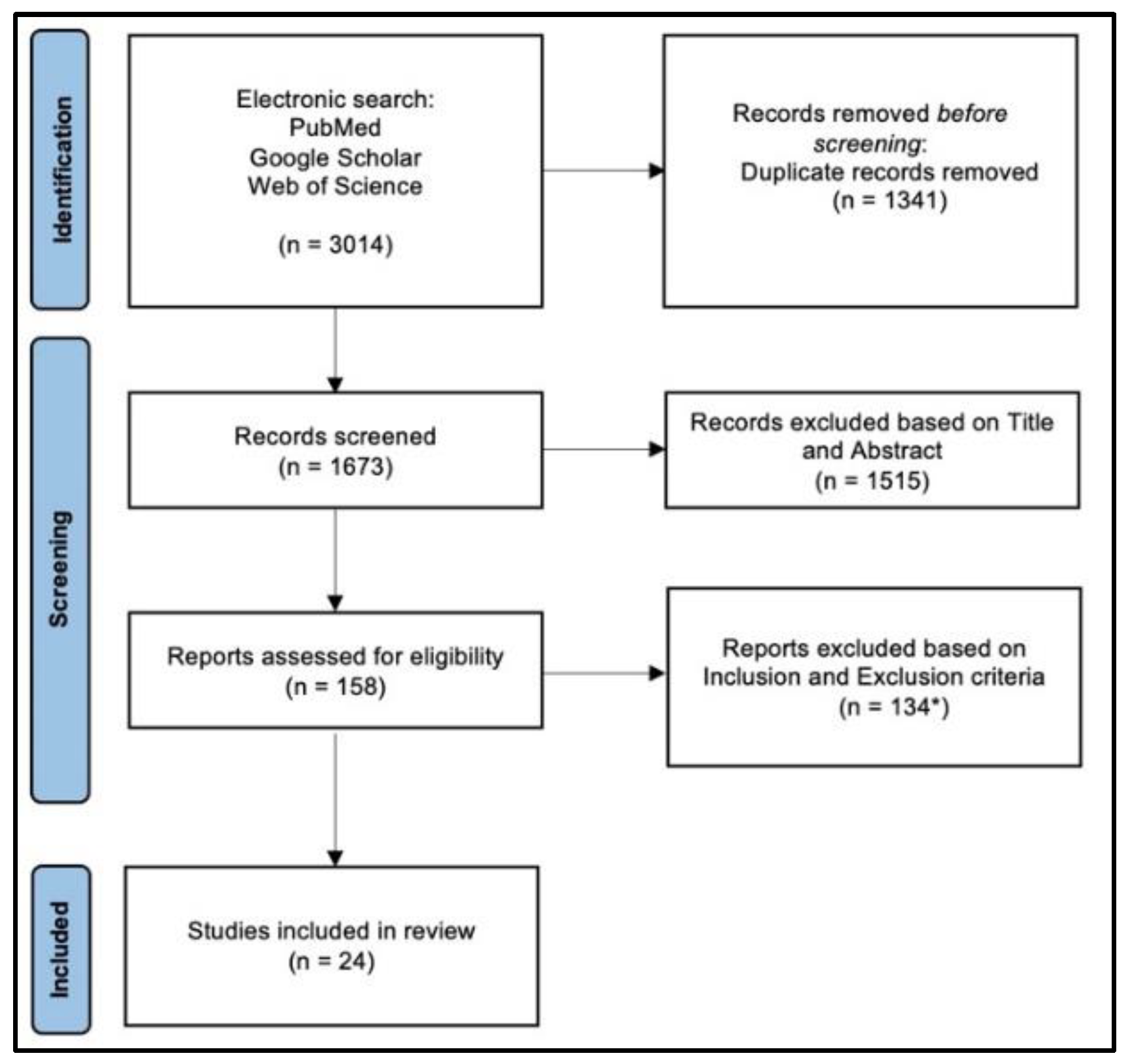
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction
3. Results
3.1. Demographics
3.2. Surgical Information about PA
3.3. Outcomes
4. Discussion
4.1. Exchange Nail
4.2. Nail Dynamization
4.3. Ilizarov External Fixation
4.4. Plate Augmentation
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Neumann, M.V.; Südkamp, N.P.; Strohm, P.C. Management of Femoral Shaft Fractures. Acta Chir. Orthop. Traumatol. Cech. 2015, 82, 22–32. [Google Scholar] [PubMed]
- Vaishya, R.; Agarwal, A.K.; Gupta, N.; Vijay, V. Plate Augmentation with Retention of Intramedullary Nail Is Effective for Resistant Femoral Shaft Non-Union. J. Orthop. 2016, 13, 242–245. [Google Scholar] [CrossRef] [PubMed]
- Smith, W.R.; Morgan, S.J. Failure of Internal Fixation of the Femoral Shaft. Tech. Orthop. 2002, 17, 448–457. [Google Scholar] [CrossRef]
- Bell, A.; Templeman, D.; Weinlein, J.C. Nonunion of the Femur and Tibia: An Update. Orthop. Clin. N. Am. 2016, 47, 365–375. [Google Scholar] [CrossRef] [PubMed]
- Greco, T.; Cianni, L.; Polichetti, C.; Inverso, M.; Maccauro, G.; Perisano, C. Uncoated vs. Antibiotic-Coated Tibia Nail in Open Diaphyseal Tibial Fracture (42 According to AO Classification): A Single Center Experience. BioMed Res. Int. 2021, 2021, 7421582. [Google Scholar] [CrossRef]
- Perisano, C.; Greco, T.; Polichetti, C.; Inverso, M.; Maccauro, G. Antibiotic-Coated Nail in Open Tibial Fracture: A Retrospective Case Series. J. Funct. Morphol. Kinesiol. 2021, 6, 97. [Google Scholar] [CrossRef]
- Greco, T.; Vitiello, R.; Cazzato, G.; Cianni, L.; Malerba, G.; Maccauro, G.; Perisano, C. Intramedullary Antibiotic Coated Nail in Tibial Fracture: A Systematic Review. J. Biol. Regul. Homeost. Agents 2020, 34, 63–69. [Google Scholar]
- Lai, P.-J.; Hsu, Y.-H.; Chou, Y.-C.; Yeh, W.-L.; Ueng, S.W.N.; Yu, Y.-H. Augmentative Antirotational Plating Provided a Significantly Higher Union Rate than Exchanging Reamed Nailing in Treatment for Femoral Shaft Aseptic Atrophic Nonunion—Retrospective Cohort Study. BMC Musculoskelet. Disord. 2019, 20, 127. [Google Scholar] [CrossRef]
- Pihlajamäki, H.K.; Salminen, S.T.; Böstman, O.M. The Treatment of Nonunions Following Intramedullary Nailing of Femoral Shaft Fractures. J. Orthop. Trauma 2002, 16, 394–402. [Google Scholar] [CrossRef]
- Tsang, S.T.J.; Mills, L.A.; Baren, J.; Frantzias, J.; Keating, J.F.; Simpson, A.H.R.W. Exchange Nailing for Femoral Diaphyseal Fracture Non-Unions: Risk Factors for Failure. Injury 2015, 46, 2404–2409. [Google Scholar] [CrossRef]
- Said, G.Z.; Said, H.G.; El-Sharkawi, M.M. Failed Intramedullary Nailing of Femur: Open Reduction and Plate Augmentation with the Nail in Situ. Int. Orthop. 2011, 35, 1089–1092. [Google Scholar] [CrossRef][Green Version]
- Uliana, C.S.; Bidolegui, F.; Kojima, K.; Giordano, V. Augmentation Plating Leaving the Nail in Situ Is an Excellent Option for Treating Femoral Shaft Nonunion after IM Nailing: A Multicentre Study. Eur. J. Trauma Emerg. Surg. 2021, 47, 1895–1901. [Google Scholar] [CrossRef] [PubMed]
- Gardner, M.J.; Toro-Arbelaez, J.B.; Harrison, M.; Hierholzer, C.; Lorich, D.G.; Helfet, D.L. Open Reduction and Internal Fixation of Distal Femoral Nonunions: Long-Term Functional Outcomes Following a Treatment Protocol. J. Trauma 2008, 64, 434–438. [Google Scholar] [CrossRef] [PubMed]
- Hak, D.J.; Lee, S.S.; Goulet, J.A. Success of Exchange Reamed Intramedullary Nailing for Femoral Shaft Nonunion or Delayed Union. J. Orthop. Trauma 2000, 14, 178–182. [Google Scholar] [CrossRef] [PubMed]
- Litrenta, J.; Tornetta, P.; Vallier, H.; Firoozabadi, R.; Leighton, R.; Egol, K.; Kruppa, C.; Jones, C.B.; Collinge, C.; Bhandari, M.; et al. Dynamizations and Exchanges: Success Rates and Indications. J. Orthop. Trauma 2015, 29, 569–573. [Google Scholar] [CrossRef]
- Menon, D.K.; Dougall, T.W.; Pool, R.D.; Simonis, R.B. Augmentative Ilizarov External Fixation after Failure of Diaphyseal Union with Intramedullary Nailing. J. Orthop. Trauma 2002, 16, 491–497. [Google Scholar] [CrossRef]
- Chiang, J.C.; Johnson, J.E.; Tarkin, I.S.; Siska, P.A.; Farrell, D.J.; Mormino, M.A. Plate Augmentation for Femoral Nonunion: More than Just a Salvage Tool? Arch. Orthop. Trauma Surg. 2016, 136, 149–156. [Google Scholar] [CrossRef]
- Jhunjhunwala, H.R.; Dhawale, A.A. Is Augmentation Plating an Effective Treatment for Non-Union of Femoral Shaft Fractures with Nail in Situ? Eur. J. Trauma Emerg. Surg. 2016, 42, 339–343. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, 264–269. [Google Scholar] [CrossRef]
- Choi, Y.S.; Kim, K.S. Plate Augmentation Leaving the Nail in Situ and Bone Grafting for Non-Union of Femoral Shaft Fractures. Int. Orthop. 2005, 29, 287–290. [Google Scholar] [CrossRef]
- Nadkarni, B.; Srivastav, S.; Mittal, V.; Agarwal, S. Use of Locking Compression Plates for Long Bone Nonunions without Removing Existing Intramedullary Nail: Review of Literature and Our Experience. J. Trauma Inj. Infect. Crit. Care 2008, 65, 482–486. [Google Scholar] [CrossRef] [PubMed]
- Birjandinejad, A.; Ebrahimzadeh, M.H.; Ahmadzadeh-Chabock, H. Augmentation Plate Fixation for the Treatment of Femoral and Tibial Nonunion after Intramedullary Nailing. Orthopedics 2009, 32, 409. [Google Scholar] [CrossRef]
- Gao, K.; Huang, J.; Tao, J.; Li, F.; Gao, W.; Li, H.; Wang, Q. Management of Femoral Diaphyseal Nonunion after Nailing with Augmentative Locked Plating and Bone Graft. Orthop. Surg. 2011, 3, 83–87. [Google Scholar] [CrossRef]
- Ye, J.; Zheng, Q. Augmentative Locking Compression Plate Fixation for the Management of Long Bone Nonunion after Intramedullary Nailing. Arch. Orthop. Trauma Surg. 2012, 132, 937–940. [Google Scholar] [CrossRef] [PubMed]
- Hakeos, W.M.; Richards, J.E.; Obremskey, W.T. Plate Fixation of Femoral Nonunions Over an Intramedullary Nail with Autogenous Bone Grafting. J. Orthop. Trauma 2011, 25, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.-J.; Chiang, C.-C.; Wu, P.-K.; Chen, C.-F.; Huang, C.-K.; Su, A.W.; Chen, W.-M.; Liu, C.-L.; Chen, T.-H. Effectiveness of Plate Augmentation for Femoral Shaft Nonunion after Nailing. J. Chin. Med. Assoc. 2012, 75, 396–401. [Google Scholar] [CrossRef][Green Version]
- KhAnFOuR, A.A.; ZAKZOuK, S.A. Distal Femur Non-Union after Interlocked Intramedullary Nailing. Successful Augmentation with Wave Plate and Strut Graft. Orthopædica Belg. 2012, 78, 8. [Google Scholar]
- Park, J.; Yang, K.H. Indications and Outcomes of Augmentation Plating with Decortication and Autogenous Bone Grafting for Femoral Shaft Nonunions. Injury 2013, 44, 1820–1825. [Google Scholar] [CrossRef]
- Wang, Z.; Liu, C.; Liu, C.; Zhou, Q.; Liu, J. Effectiveness of Exchange Nailing and Augmentation Plating for Femoral Shaft Nonunion after Nailing. Int. Orthop. 2014, 38, 2343–2347. [Google Scholar] [CrossRef]
- Jiang, L.; Pan, Z.; Zheng, Q. Augmentation Plating in Hypertrophic Non-Union after Nail Fixation of Femoral Shaft Fracture Compared with Exchange Plating. Chin. Med. J. 2014, 127, 2900–2905. [Google Scholar]
- Sancheti, K.H.; Pradhan, C.; Patil, A.; Puram, C.; Bharti, P.; Sancheti, P.; Shyam, A. Effectiveness of Exchange K-Nail and Augmented Plating in Aseptic Femoral Diaphyseal Non-Union. Injury 2017, 48, S61–S65. [Google Scholar] [CrossRef]
- Park, K.-C.; Oh, C.-W.; Kim, J.-W.; Park, K.-H.; Oh, J.-K.; Park, I.-H.; Kyung, H.-S.; Heo, J. Minimally Invasive Plate Augmentation in the Treatment of Long-Bone Non-Unions. Arch. Orthop. Trauma Surg. 2017, 137, 1523–1528. [Google Scholar] [CrossRef] [PubMed]
- Verma, R.; Sharma, P.; Gaur, S. Augmentation Plating in Management of Failed Femoral Nailing. Injury 2017, 48, S23–S26. [Google Scholar] [CrossRef]
- El Zahlawy, H.; Abdeldayem, S.M.; Metwaly, R.G. Plate Augmentation Combined with Bone Grafting for Aseptic Non-Union of Femoral Shaft Fractures Following Interlocking Nails. Acta Orthop. Belg. 2019, 85, 205–209. [Google Scholar]
- Mittal, K.K.; Gupta, H.; Kaushik, N. Reunion of Post Nail Aseptic Non-Union of Diaphyseal Femoral Fractures by Augmentation Plating, Decortication and Bone Grafting—Replacement for Exchange Nailing. Injury 2021, 52, 1529–1533. [Google Scholar] [CrossRef]
- Ebrahimpour, A.; Chehrassan, M.; Biglari, F.; Minator Sajjadi, M.; Jalalpour, P.; Sadighi, M. Augmented Plating and Bone Grafting in Treatment of Tibial and Femoral Shaft Nonunion. Trauma Mon. 2021, 26, 187–193. [Google Scholar] [CrossRef]
- Mohamed, M.A.; Noaman, H.H.; Soroor, Y.O.; Elsayed, M. Plate Augmentation and Bone Grafting in Treatment of Femoral Shaft Nonunion Initially Fixed by Intramedullary Nail. SICOT-J 2022, 8, 19. [Google Scholar] [CrossRef]
- Luo, H.; Su, Y.; Ding, L.; Xiao, H.; Wu, M.; Xue, F. Exchange Nailing versus Augmentative Plating in the Treatment of Femoral Shaft Nonunion after Intramedullary Nailing: A Meta-Analysis. EFORT Open Rev. 2019, 4, 513–518. [Google Scholar] [CrossRef]
- Basilico, M.; Vitiello, R.; Oliva, M.S.; Covino, M.; Greco, T.; Cianni, L.; Dughiero, G.; Ziranu, A.; Perisano, C.; Maccauro, G. Predictable Risk Factors for Infections in Proximal Femur Fractures. J. Biol. Regul. Homeost. Agents 2020, 34, 77–81. [Google Scholar]
- Park, K.; Kim, K.; Choi, Y.S. Comparison of Mechanical Rigidity between Plate Augmentation Leaving the Nail in Situ and Interlocking Nail Using Cadaveric Fracture Model of the Femur. Int. Orthop. 2011, 35, 581–585. [Google Scholar] [CrossRef][Green Version]
- Yoshino, O.; Brady, J.; Young, K.; Hardy, B.; Matthys, R.; Buxton, T.; Appleyard, R.; Tomka, J.; Dabirrahmani, D.; Woodford, P.; et al. Reamed Locked Intramedullary Nailing for Studying Femur Fracture and Its Complications. Eur. Cell. Mater. 2017, 34, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Weresh, M.J.; Hakanson, R.; Stover, M.D.; Sims, S.H.; Kellam, J.F.; Bosse, M.J. Failure of Exchange Reamed Intramedullary Nails for Ununited Femoral Shaft Fractures. J. Orthop. Trauma 2000, 14, 335–338. [Google Scholar] [CrossRef] [PubMed]
- Medlock, G.; Stevenson, I.M.; Johnstone, A.J. Uniting the Un-United: Should Established Non-Unions of Femoral Shaft Fractures Initially Treated with IM Nails Be Treated by Plate Augmentation Instead of Exchange IM Nailing? A Systematic Review. Strateg. Trauma Limb Reconstr. 2018, 13, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Shroeder, J.E.; Mosheiff, R.; Khoury, A.; Liebergall, M.; Weil, Y.A. The Outcome of Closed, Intramedullary Exchange Nailing with Reamed Insertion in the Treatment of Femoral Shaft Nonunions. J. Orthop. Trauma 2009, 23, 653–657. [Google Scholar] [CrossRef] [PubMed]
- Vaughn, J.E.; Shah, R.V.; Samman, T.; Stirton, J.; Liu, J.; Ebraheim, N.A. Systematic Review of Dynamization vs. Exchange Nailing for Delayed/Non-Union Femoral Fractures. World J. Orthop. 2018, 9, 92–99. [Google Scholar] [CrossRef]
- Papakostidis, C.; Bhandari, M.; Giannoudis, P.V. Distraction Osteogenesis in the Treatment of Long Bone Defects of the Lower Limbs: Effectiveness, Complications and Clinical Results; A Systematic Review and Meta-Analysis. Bone Jt. J. 2013, 95, 1673–1680. [Google Scholar] [CrossRef]
- Velazquez, R.J.; Bell, D.F.; Armstrong, P.F.; Babyn, P.; Tibshirani, R. Complications of Use of the Ilizarov Technique in the Correction of Limb Deformities in Children. J. Bone Jt. Surg. Am. 1993, 75, 1148–1156. [Google Scholar] [CrossRef]
- Gelalis, I.D.; Politis, A.N.; Arnaoutoglou, C.M.; Korompilias, A.V.; Pakos, E.E.; Vekris, M.D.; Karageorgos, A.; Xenakis, T.A. Diagnostic and Treatment Modalities in Nonunions of the Femoral Shaft: A Review. Injury 2012, 43, 980–988. [Google Scholar] [CrossRef]
| Author and Year | Type of Study | Cases | Sex (M-F) | Age (Mean) | Localization (P-Mi-D) | Type of NU (A-H) | Bone Graft | Union Rate (%) | Time of Union (m) | Type of Plate | EN | Follow-Up (m) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Choi and Kim, 2005 [20] | Re | 15 | 12-3 | 36.8 | 0-10-5 | 14-1 | 15 | 100 | 7.2 | DCP | NS | 42.3 |
| Nadkarni et al., 2008 [21] | Re | 7 | 2-5 | 48.7 | 3-0-4 | NS | 7 | 100 | 6.8 | LCP | NS | 14.7 |
| Birjandinejad et al., 2009 [22] | Re | 25 | NS | 31.4 | NS | NS | 25 | 100 | 4.8 | DCP | NS | 12 |
| Gao et al., 2011 [23] | Re | 13 | 12-1 | 38.9 | NS | NS | 13 | 100 | 7.5 | 11 LCP, 2 PHLP | NS | 14.4 |
| Hakeos et al., 2011 [25] | Re | 7 | 6-1 | 42.5 | NS | 4-3 | 7 | 100 | 5 | LC–DCP | NS | 17.9 |
| Said et al., 2011 [11] | Re | 14 | 14-0 | 42 | NS | NS | 9 | 100 | 4.3 | DCP | NS | 26 |
| Ye and Zheng, 2012 [24] | Re | 4 | 3-1 | 48.5 | 2-1-1 | 2-2 | 4 | 100 | 5 | LCP | NS | 14.5 |
| Lin et al., 2012 [26] | Re | 22 | 13-9 | 34.3 | 5-12-5 | 13-22 | 22 | 100 | 5.5 | DCP | NS | 17.2 |
| Khanfour and Zakzouk, 2012 [27] | Re | 11 | 10-1 | 40 | 0-0-11 | NS | 11 | 100 | 7.5 | DCP | NS | 24.2 |
| Park and Yang, 2013 [28] | Re | 39 | 34-5 | 41.9 | 8-16-15 | 30-9 | 39 | 97.4 | 6.1 | DCP or LC–DCP | NS | 24.8 |
| Wang et al., 2014 [29] | Re | 21 | 9-12 | 40 | NS | NS | 21 | 100 | 6 | LCP | 21 | 12 |
| Jiang et al., 2014 [30] | Re | 12 | 9-3 | 42 | NS | 0-12 | None | 100 | 4.17 | LC–DCP | NS | 18.37 |
| Jhunjhunwala et al., 2016 [18] | Re | 40 | 31-9 | 35 | 3-32-5 | 26-14 | 26 | 97.5 | 4 | DCP | 9 | 12 |
| Chiang et al., 2016 [17] | Re | 30 | 18-12 | 50.5 | 6-13-11 | 25-5 | 17 * | 96.6 | 4.3 | LC–DCP | NS | NS |
| Vaishya et al., 2016 [2] | Re | 16 | 11-5 | 36 | NS | 4-12 | 4 | 100 | 6.25 | LC–DCP | NS | 9.6 |
| Sancheti et al., 2017 [31] | Re | 70 | 60-10 | 40.7 | 9-48-13 | 24-46 | 70 | 100 | 4 | DCP | 70 | 31.37 |
| Park et al., 2017 [32] | Re | 5 | 5-0 | NS | NS | NS | None | 100 | 5.3 | LCP | NS | 29.5 |
| Verma et al., 2017 [33] | Pr | 15 | 9-6 | 43.7 | NS | NS | 15 | 100 | 5.2 | LCP | 15 | 12.6 |
| Lai et al., 2019 [8] | Re | 26 | 18-8 | 31.77 | NS | 26-0 | 26 | 88.46 | 7.5 | DCP | NS | 11.9 |
| El Zahlawy et al., 2019 [34] | Pr | 34 | 25-9 | 36.6 | 7-17-10 | NS | 34 | 100 | 6.3 | DCP | NS | 12 |
| Uliana et al., 2021 [12] | Re | 22 | 18-4 | 32.3 | 1-12-9 | 12-10 | 18 | 86.3 | 11.7 | 10 DCP, 12 LCP | NS | 23.5 |
| Mittal et al., 2021 [35] | Pr | 21 | 15-6 | 40 | NS | NS | 21 | 100 | 6 | LCP | NS | 14.1 |
| Ebrahimpour et al., 2021 [36] | Re | 13 | NS | 42.8 | NS | NS | 13 | 92.3 | 4.75 | LCP | NS | 12 |
| Mohamed et al., 2022 [37] | Re | 20 | 13-7 | 32.4 | 3-7-10 | 20-0 | 20 | 100 | 4.9 | DCP | NS | 13 |
| Numbers of Patients | 502 | |
| Age (average on 512 patients) | 39.5 ± 5.4 years old | |
| Sex | Male | 347 (74.8%) |
| Female | 117 (25.2%) | |
| NS | 38/502 (7.6%) | |
| NU localization | Proximal | 47 (15.0%) |
| Middle | 168 (53.5%) | |
| Distal | 99 (31.5%) | |
| NS | 188/502 (37.4%) | |
| NU type | Atrophic | 200 (61.9%) |
| Hypertrophic | 123 (38.1%) | |
| NS | 179/502 (35.6%) | |
| First IMN | Anterograde | 151 (85.8%) |
| Retrograde | 25 (14.2%) | |
| NS | 326/502 (65.0%) | |
| Type of plate | DCP | 287 (57.1%) |
| LCP | 109 (21.7%) | |
| LC–DCP | 65 (13.0%) | |
| PHLP | 2 (0.4%) | |
| DCP or LC–DCP | 39 (7.8%) |
| Numbers of Patients | 502 | |
| EN before PA | 115 (22.9%) | |
| Bone graft | Autologous iliac crest bone graft | 437 (87.1%) |
| Bone union | 492 (98.0%) | |
| Time of union (m) | 5.8 ± 2.12 | |
| Complications | Shortening of the limb | 25 (5.0%) |
| Wound infections | 10 (2.0%) | |
| Graft site donor pain | 3 (0.6%) | |
| Broken screws | 2 (0.4%) | |
| DVT | 2 (0.4%) | |
| Deep infection | 2 (0.4%) | |
| Infected hematoma | 1 (0.2%) | |
| Total | 45 (9.0%) | |
| Follow-up (m) | 18.2 (range 9.4–42.3) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perisano, C.; Cianni, L.; Polichetti, C.; Cannella, A.; Mosca, M.; Caravelli, S.; Maccauro, G.; Greco, T. Plate Augmentation in Aseptic Femoral Shaft Nonunion after Intramedullary Nailing: A Literature Review. Bioengineering 2022, 9, 560. https://doi.org/10.3390/bioengineering9100560
Perisano C, Cianni L, Polichetti C, Cannella A, Mosca M, Caravelli S, Maccauro G, Greco T. Plate Augmentation in Aseptic Femoral Shaft Nonunion after Intramedullary Nailing: A Literature Review. Bioengineering. 2022; 9(10):560. https://doi.org/10.3390/bioengineering9100560
Chicago/Turabian StylePerisano, Carlo, Luigi Cianni, Chiara Polichetti, Adriano Cannella, Massimiliano Mosca, Silvio Caravelli, Giulio Maccauro, and Tommaso Greco. 2022. "Plate Augmentation in Aseptic Femoral Shaft Nonunion after Intramedullary Nailing: A Literature Review" Bioengineering 9, no. 10: 560. https://doi.org/10.3390/bioengineering9100560
APA StylePerisano, C., Cianni, L., Polichetti, C., Cannella, A., Mosca, M., Caravelli, S., Maccauro, G., & Greco, T. (2022). Plate Augmentation in Aseptic Femoral Shaft Nonunion after Intramedullary Nailing: A Literature Review. Bioengineering, 9(10), 560. https://doi.org/10.3390/bioengineering9100560











