Therapeutic Potential of Local Application of Fibroblast Growth Factor-2 to Periodontal Defects in a Preclinical Osteoporosis Model
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Ovariectomy (OVX)
2.3. Confirmation of Osteoporotic Conditions
2.4. Preparation of Fibroblast Growth Factor-2 (FGF-2)
2.5. In Vivo Model and Surgical Interventions
2.6. Microcomputed Tomography of Surgical Periodontal Defect
2.7. Histological Analysis
2.8. In Vitro Cell Culture
2.9. Assessment of Cell Morphology
2.10. Assessment of Cell Viability/Proliferation
2.11. Quantitative Reverse Transcription-PCR (qRT-PCR)
2.12. Alkaline Phosphatase (ALP) Staining
2.13. Statistical Analysis
3. Results
3.1. Establishment of Osteoporotic Model
3.2. Micro-CT Analysis of Periodontal Defects and Their Healing
3.3. Histological Findings
3.4. In Vitro Cell Morphology
3.5. Cell Viability/Proliferation
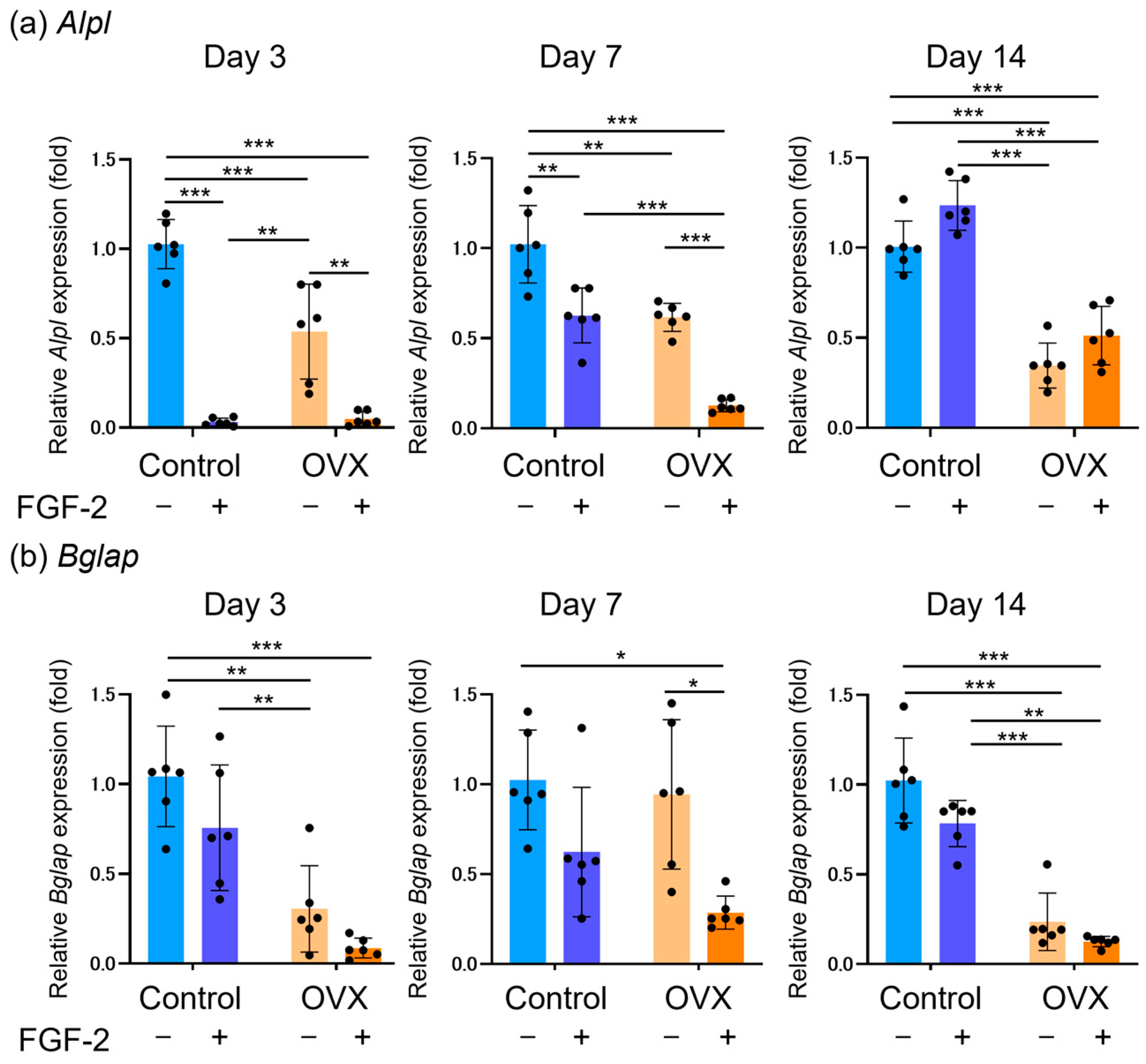
3.6. Expression of Osteoblastic Differentiation Markers
3.7. Assessment of ALP Staining
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| FGF-2 | Fibroblast growth factor-2 |
| OVX | Ovariectomy |
| PDL | Periodontal ligament |
| HPC | Hydroxypropylcellulose |
| ALP | Alkaline phosphatase |
| BMSCs | Bone marrow mesenchymal stromal cells |
| CLSM | Confocal laser scanning microscopy |
References
- Salari, N.; Ghasemi, H.; Mohammadi, L.; Behzadi, M.H.; Rabieenia, E.; Shohaimi, S.; Mohammadi, M. The global prevalence of osteoporosis in the world: A comprehensive systematic review and meta-analysis. J. Orthop. Surg. Res. 2021, 16, 609. [Google Scholar] [PubMed]
- Yoshimura, N.; Iidaka, T.; Horii, C.; Muraki, S.; Oka, H.; Kawaguchi, H.; Nakamura, K.; Akune, T.; Tanaka, S. Trends in osteoporosis prevalence over a 10-year period in Japan: The ROAD study 2005–2015. J. Bone Miner. Metab. 2022, 40, 829–838. [Google Scholar]
- Kanis, J.A.; Cooper, C.; Rizzoli, R.; Reginster, J.-Y.; on behalf of the Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis (ESCEO) and the Committees of Scientific Advisors and National Societies of the International Osteoporosis Foundation (IOF). European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos. Int. 2019, 30, 3–44. [Google Scholar]
- Rodan, G.A.; Martin, T.J. Therapeutic approaches to bone diseases. Science 2000, 289, 1508–1514. [Google Scholar] [PubMed]
- Bartold, P.M. Lifestyle and periodontitis: The emergence of personalized periodontics. Periodontology 2000 2018, 78, 7–11. [Google Scholar]
- Peng, J.; Chen, J.; Liu, Y.; Lyu, J.; Zhang, B. Association between periodontitis and osteoporosis in United States adults from the national health and nutrition examination survey: A cross-sectional analysis. BMC Oral Health 2023, 23, 254. [Google Scholar]
- Penoni, D.C.; Fidalgo, T.K.S.; Torres, S.R.; Varela, V.M.; Masterson, D.; Leão, A.T.T.; Maia, L.C. Bone density and clinical periodontal attachment in postmenopausal women: A systematic review and meta-analysis. J. Dent. Res. 2017, 96, 261–269. [Google Scholar]
- Kribbs, P.J. Comparison of mandibular bone in normal and osteoporotic women. J. Prosthet. Dent. 1990, 63, 218–222. [Google Scholar]
- Cheung, W.H.; Miclau, T.; Chow, S.K.H.; Yang, F.F.; Alt, V. Fracture healing in osteoporotic bone. Injury 2016, 47, S21–S26. [Google Scholar]
- Só, B.B.; Silveira, F.M.; Llantada, G.S.; Jardim, L.C.; Calcagnotto, T.; Martins, M.A.T.; Martins, M.D. Effects of osteoporosis on alveolar bone repair after tooth extraction: A systematic review of preclinical studies. Arch. Oral Biol. 2021, 125, 105054. [Google Scholar]
- Namkung-Matthai, H.; Appleyard, R.; Jansen, J.; Lin, J.H.; Maastricht, S.; Swain, M.; Mason, R.S.; Murrell, G.A.C.; Diwan, A.D.; Diamond, T. Osteoporosis influences the early period of fracture healing in rat osteoporotic model. Bone 2001, 28, 80–86. [Google Scholar]
- Gomes-Filho, I.S.; Oliveira, T.J.S.; Passos, J.S.; de M.M. Cerqueira, E.; da Cruz, S.S.; Barreto, M.L.; Coelho, J.M.F.; Trindade, S.C.; Santos, C.A.S.T.; Sarmento, V.A. Effect of osteoporosis on periodontal therapy among post-menopausal women. Gerodontology 2013, 30, 40–48. [Google Scholar] [PubMed]
- Sculean, A.; Nikolidakis, D.; Nikou, G.; Ivanovic, A.; Chapple, I.L.C.; Stavropoulos, A. Biomaterials for promoting periodontal regeneration in human intrabony defects: A systematic review. Periodontology 2000 2015, 68, 182–216. [Google Scholar]
- Bartold, P.M.; Gronthos, S.; Ivanovski, S.; Fisher, A.; Hutmacher, D.W. Tissue engineered periodontal products. J. Periodontal Res. 2016, 51, 1–15. [Google Scholar] [PubMed]
- Murakami, S. Periodontal tissue regeneration by signaling molecule(s): What role does basic fibroblast growth factor (FGF-2) have in periodontal therapy? Periodontology 2000 2011, 56, 188–208. [Google Scholar]
- Aoki, H.; Bizenjima, T.; Seshima, F.; Sato, M.; Irokawa, D.; Yoshikawa, K.; Yoshida, W.; Imamura, K.; Matsugami, D.; Kitamura, Y.; et al. Periodontal surgery using rhFGF-2 with deproteinized bovine bone mineral or rhFGF-2 alone: 2-year follow-up of a randomized Controlled trial. J. Clin. Periodontol. 2021, 48, 92–100. [Google Scholar]
- Seshima, F.; Bizenjima, T.; Aoki, H.; Imamura, K.; Kita, D.; Irokawa, D.; Matsugami, D.; Kitamura, Y.; Yamashita, K.; Sugito, H.; et al. Periodontal regenerative therapy using rhFGF-2 and deproteinized bovine bone mineral versus rhFGF-2 alone: 4-year extended follow-up of a randomized controlled trial. Biomolecules 2022, 12, 1682. [Google Scholar]
- Yu, B.; Wang, C.Y. Osteoporosis and periodontal diseases—An update on their association and mechanistic links. Periodontology 2000 2022, 89, 99–113. [Google Scholar]
- Corrêa, M.G.; Gomes Campos, M.L.; Marques, M.R.; Casati, M.Z.; Nociti, F.H., Jr.; Sallum, E.A. Histometric analysis of the effect of enamel matrix derivative on the healing of periodontal defects in rats with diabetes. J. Periodontol. 2013, 84, 1309–1318. [Google Scholar]
- Bizenjima, T.; Seshima, F.; Ishizuka, Y.; Takeuchi, T.; Kinumatsu, T.; Saito, A. Fibroblast growth factor-2 promotes healing of surgically created periodontal defects in rats with early, streptozotocin-induced diabetes via increasing cell proliferation and regulating angiogenesis. J. Clin. Periodontol. 2015, 42, 62–71. [Google Scholar]
- Miron, R.J.; Wei, L.; Yang, S.; Caluseru, O.M.; Sculean, A.; Zhang, Y. Effect of enamel matrix derivative on periodontal wound healing and regeneration in an osteoporotic model. J. Periodontol. 2014, 85, 1603–1611. [Google Scholar] [PubMed]
- Nakamura, K.; Kawaguchi, H.; Aoyama, I.; Hanada, K.; Hiyama, Y.; Awa, T.; Tamura, M.; Kurokawa, T. Stimulation of bone formation by intraosseous application of recombinant basic fibroblast growth factor in normal and ovariectomized rabbits. J. Orthop. Res. 1997, 15, 307–313. [Google Scholar]
- Zhang, Y.; Cheng, N.; Miron, R.; Shi, B.; Cheng, X. Delivery of PDGF-B and BMP-7 by mesoporous bioglass/silk fibrin scaffolds for the repair of osteoporotic defects. Biomaterials 2012, 33, 6698–6708. [Google Scholar] [PubMed]
- Ju, Y.-I.; Choi, H.-J.; Sone, T. Effects of Korean red ginseng on three-dimensional trabecular bone microarchitecture and strength in growing rats: Comparison with changes due to jump exercise. PLoS ONE 2022, 17, e0267466. [Google Scholar]
- Yoshida, W.; Matsugami, D.; Murakami, T.; Bizenjima, T.; Imamura, K.; Seshima, F.; Saito, A. Combined effects of systemic parathyroid hormone (1–34) and locally delivered neutral self-assembling peptide hydrogel in the treatment of periodontal defects: An experimental in vivo investigation. J. Clin. Periodontol. 2019, 46, 1030–1040. [Google Scholar]
- Arima, Y.; Uemura, N.; Hashimoto, Y.; Baba, S.; Matsumoto, N. Evaluation of bone regeneration by porous alpha-tricalcium phosphate/atelocollagen sponge composite in rat calvarial defects. Orthod. Waves 2013, 72, 23–29. [Google Scholar]
- Zhou, Q.; Zhou, L.; Li, J. MiR-218-5p-dependent SOCS3 downregulation increases osteoblast differentiation in postmenopausal osteoporosis. J. Orthop. Surg. Res. 2023, 18, 109. [Google Scholar] [PubMed]
- Sangeetha, P.; Maiti, S.K.; Divya, M.; Shivaraju, S.; Raguvaran, R.; Malik, A.R.; Bindhuja, B.V.; Naveen, K.; Raguvanshi, P.D.S. Mesenchymal stem cells derived from rat bone marrow: Techniques for isolation, expansion and differentiation. J. Stem Cell Res. Ther. 2017, 3, 272–277. [Google Scholar]
- Boyd, S.K.; Davison, P.; Müller, R.; Gasser, J.A. Monitoring individual morphological changes over time in ovariectomized rats by in vivo micro-computed tomography. Bone 2006, 39, 854–862. [Google Scholar]
- Otomo-Corgel, J. Osteoporosis and osteopenia: Implications for periodontal and implant therapy. Periodontology 2000 2012, 59, 111–139. [Google Scholar]
- Raisz, L.G. Pathogenesis of osteoporosis: Concepts, conflicts, and prospects. J. Clin. Investig. 2005, 115, 3318–3325. [Google Scholar] [PubMed]
- Wang, C.J.; McCauley, L.K. Osteoporosis and periodontitis. Curr. Osteoporos. Rep. 2016, 14, 284–291. [Google Scholar] [PubMed]
- Chen, W.J.; Jingushi, S.; Aoyama, I.; Anzai, J.; Hirata, G.; Tamura, M.; Iwamoto, Y. Effects of FGF-2 on metaphyseal fracture repair in rabbit tibiae. J. Bone Miner. Metab. 2004, 22, 303–309. [Google Scholar]
- Murakami, S.; Takayama, S.; Kitamura, M.; Shimabukuro, Y.; Yanagi, K.; Ikezawa, K.; Saho, T.; Nozaki, T.; Okada, H. Recombinant human basic fibroblast growth factor (bFGF) stimulates periodontal regeneration in class II furcation defects created in beagle dogs. J. Periodontal Res. 2003, 38, 97–103. [Google Scholar]
- Yanagita, M.; Kojima, Y.; Kubota, M.; Mori, K.; Yamashita, M.; Yamada, S.; Kitamura, M.; Murakami, S. Cooperative effects of FGF-2 and VEGF-A in periodontal ligament cells. J. Dent. Res. 2014, 93, 89–95. [Google Scholar]
- Saran, U.; Gemini Piperni, S.; Chatterjee, S. Role of angiogenesis in bone repair. Arch. Biochem. Biophys. 2014, 561, 109–117. [Google Scholar]
- Meng, J.; Yu, Q. Primary osteoporosis in postmenopausal women. Chronic Dis. Transl. Med. 2015, 1, 9–13. [Google Scholar]
- Yang, Y.; Sun, Y.; Mao, W.; Zhang, H.; Ni, B.; Jiang, L. Oxidative stress induces downregulation of TP53INP2 and suppresses osteogenic differentiation of BMSCs during osteoporosis through the autophagy degradation pathway. Free Radic. Biol. Med. 2021, 166, 226–237. [Google Scholar] [PubMed]
- Pino, A.M.; Rosen, C.J.; Rodríguez, J.P. In osteoporosis, differentiation of mesenchymal stem cells (MSCs) improves bone marrow adipogenesis. Biol. Res. 2012, 45, 279–287. [Google Scholar]
- Liu, Q.; Zhang, X.; Jiao, Y.; Liu, X.; Wang, Y.; Li, S.L.; Wei, Z.; Chen, F.-M.; Ding, Y.; Jiang, C.; et al. In vitro cell behaviors of bone mesenchymal stem cells derived from normal and postmenopausal osteoporotic rats. Int. J. Mol. Med. 2018, 41, 669–678. [Google Scholar]
- Bidwell, J.P.; Alvarez, M.B.; Hood, M.; Childress, P. Functional impairment of bone formation in the pathogenesis of osteoporosis: The bone marrow regenerative competence. Curr. Osteoporos. Rep. 2013, 11, 117–125. [Google Scholar] [PubMed]
- Ma, Q.; Miri, Z.; Haugen, H.J.; Moghanian, A.; Loca, D. Significance of mechanical loading in bone fracture healing, bone regeneration, and vascularization. J. Tissue Eng. 2023, 14, 20417314231172573. [Google Scholar] [PubMed]
- Deepak, V.; Kayastha, P.; McNamara, L.M. Estrogen deficiency attenuates fluid flow-induced [Ca2+]i oscillations and mechanoresponsiveness of MLO-Y4 osteocytes. FASEB J. 2017, 31, 3027–3039. [Google Scholar] [PubMed]
- Shimabukuro, Y.; Terashima, H.; Takedachi, M.; Maeda, K.; Nakamura, T.; Sawada, K.; Kobashi, M.; Awata, T.; Oohara, H.; Kawahara, T.; et al. Fibroblast growth factor-2 stimulates directed migration of periodontal ligament cells via PI3K/AKT signaling and CD44/hyaluronan interaction. J. Cell. Physiol. 2011, 226, 809–821. [Google Scholar]
- Nagayasu-Tanaka, T.; Anzai, J.; Takaki, S.; Shiraishi, N.; Terashima, A.; Asano, T.; Nozaki, T.; Kitamura, T.; Murakami, S. Action mechanism of fibroblast growth factor-2 (FGF-2) in the promotion of periodontal regeneration in beagle dogs. PLoS ONE 2015, 10, e0131870. [Google Scholar]
- Kalu, D.N. The ovariectomized rat model of postmenopausal bone loss. Bone Miner. 1991, 15, 175–191. [Google Scholar]
- Khajuria, D.K.; Razdan, R.; Mahapatra, D.R. Description of a new method of ovariectomy in female rats. Rev. Bras. Reumatol. 2012, 52, 466–470. [Google Scholar]





Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mori, S.; Mano, S.; Miyata, N.; Murakami, T.; Yoshida, W.; Imamura, K.; Saito, A. Therapeutic Potential of Local Application of Fibroblast Growth Factor-2 to Periodontal Defects in a Preclinical Osteoporosis Model. Bioengineering 2025, 12, 748. https://doi.org/10.3390/bioengineering12070748
Mori S, Mano S, Miyata N, Murakami T, Yoshida W, Imamura K, Saito A. Therapeutic Potential of Local Application of Fibroblast Growth Factor-2 to Periodontal Defects in a Preclinical Osteoporosis Model. Bioengineering. 2025; 12(7):748. https://doi.org/10.3390/bioengineering12070748
Chicago/Turabian StyleMori, Shinta, Sho Mano, Naoki Miyata, Tasuku Murakami, Wataru Yoshida, Kentaro Imamura, and Atsushi Saito. 2025. "Therapeutic Potential of Local Application of Fibroblast Growth Factor-2 to Periodontal Defects in a Preclinical Osteoporosis Model" Bioengineering 12, no. 7: 748. https://doi.org/10.3390/bioengineering12070748
APA StyleMori, S., Mano, S., Miyata, N., Murakami, T., Yoshida, W., Imamura, K., & Saito, A. (2025). Therapeutic Potential of Local Application of Fibroblast Growth Factor-2 to Periodontal Defects in a Preclinical Osteoporosis Model. Bioengineering, 12(7), 748. https://doi.org/10.3390/bioengineering12070748







