Development of Semi-Automated Image-Based Analysis Tool for CBCT Evaluation of Alveolar Ridge Changes After Tooth Extraction
Abstract
1. Introduction
2. Materials and Methods
2.1. Software and Data Format
2.2. Clinical Trial Study Design
2.2.1. Study Design
2.2.2. Inclusion and Exclusion Criteria
2.3. Sample Size Calculation
2.4. Surgical Procedures
2.4.1. Tooth Extraction and Socket Preservation
2.4.2. Follow-Up and Radiological Evaluation
2.5. Statistical Analysis
3. Results
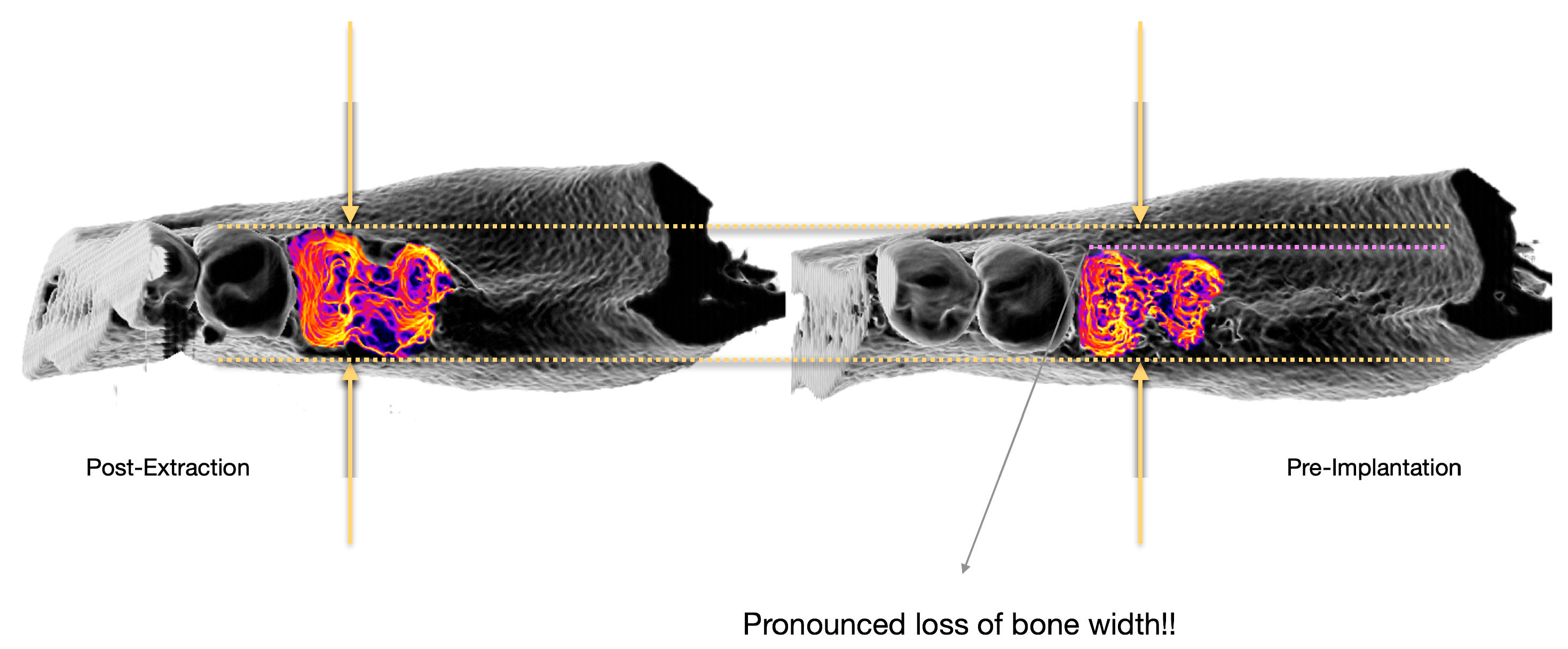
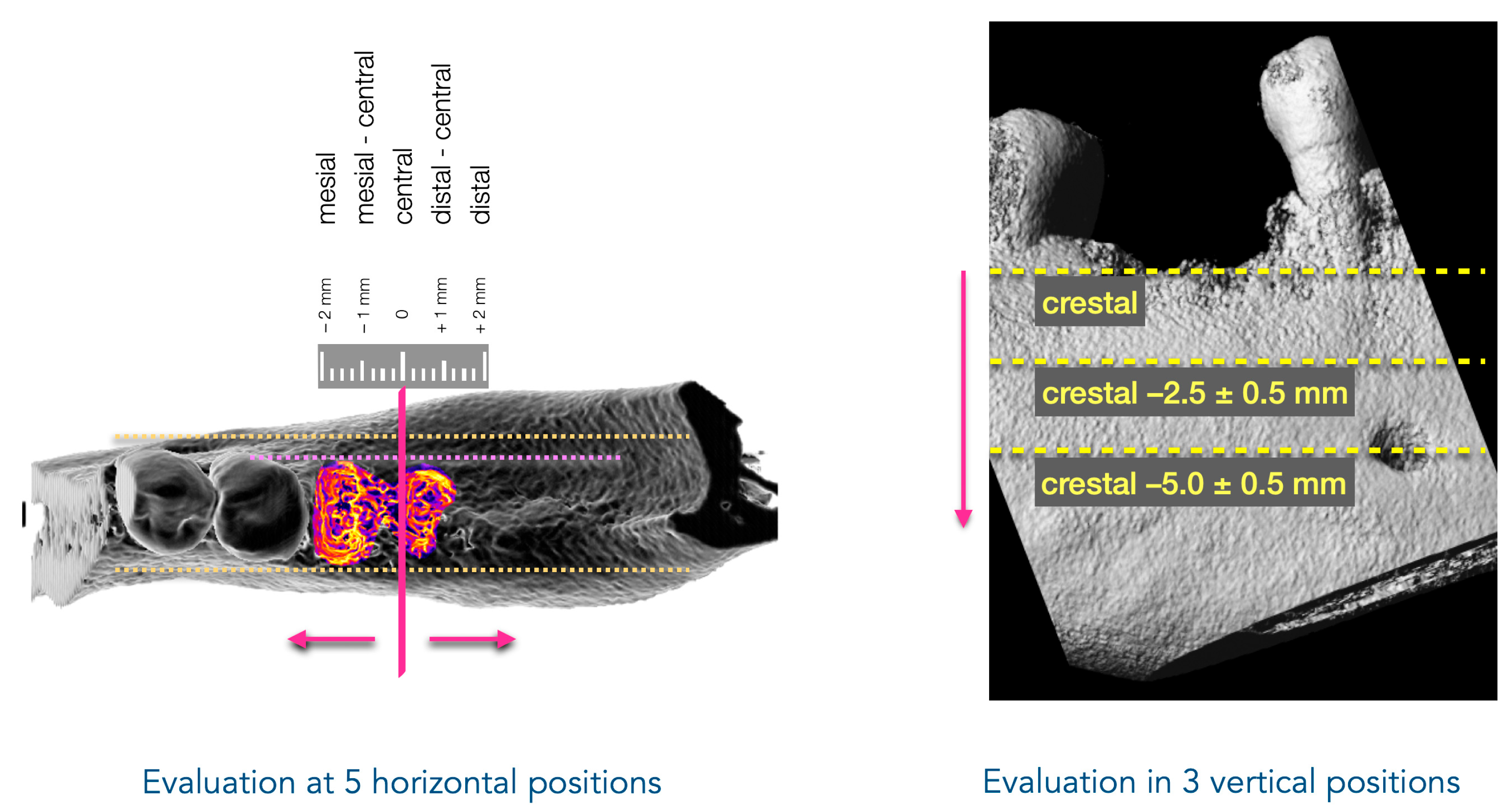
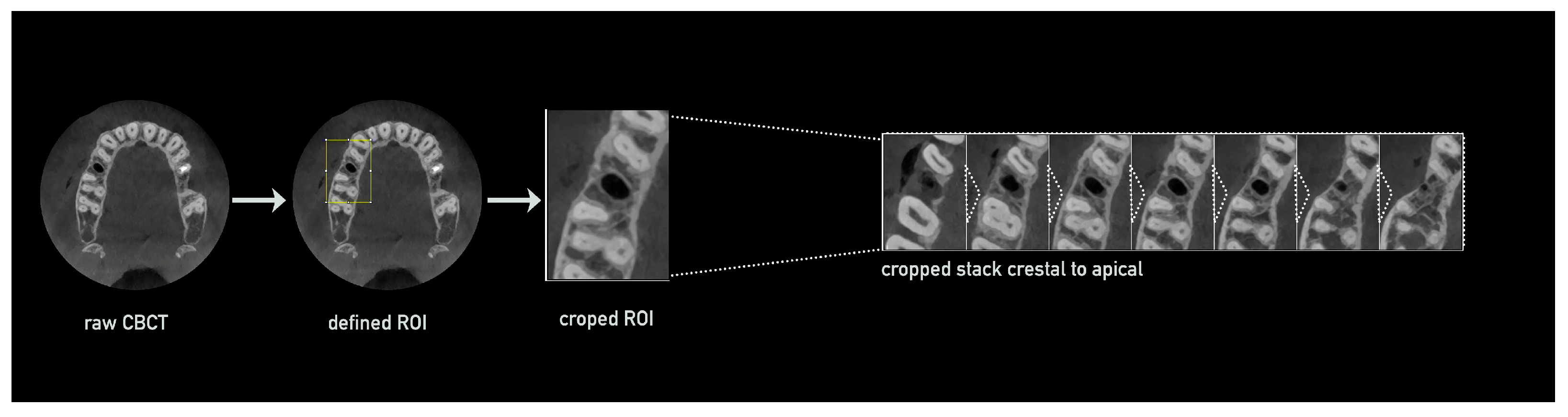
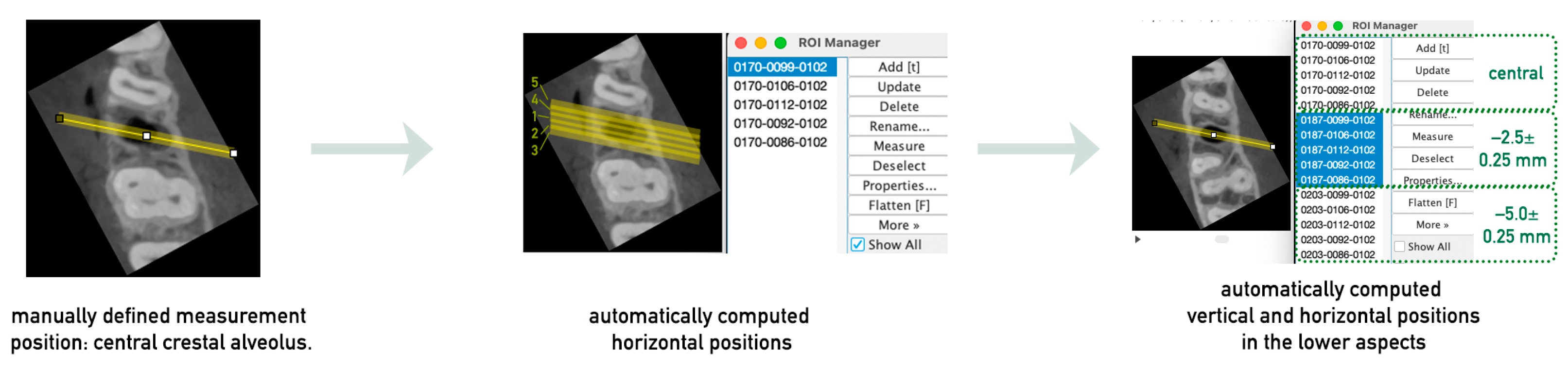
3.1. Method Development
3.1.1. CBCT Preparation and Processing for Measurement Analysis
3.1.2. Definition of the Measurement Positions
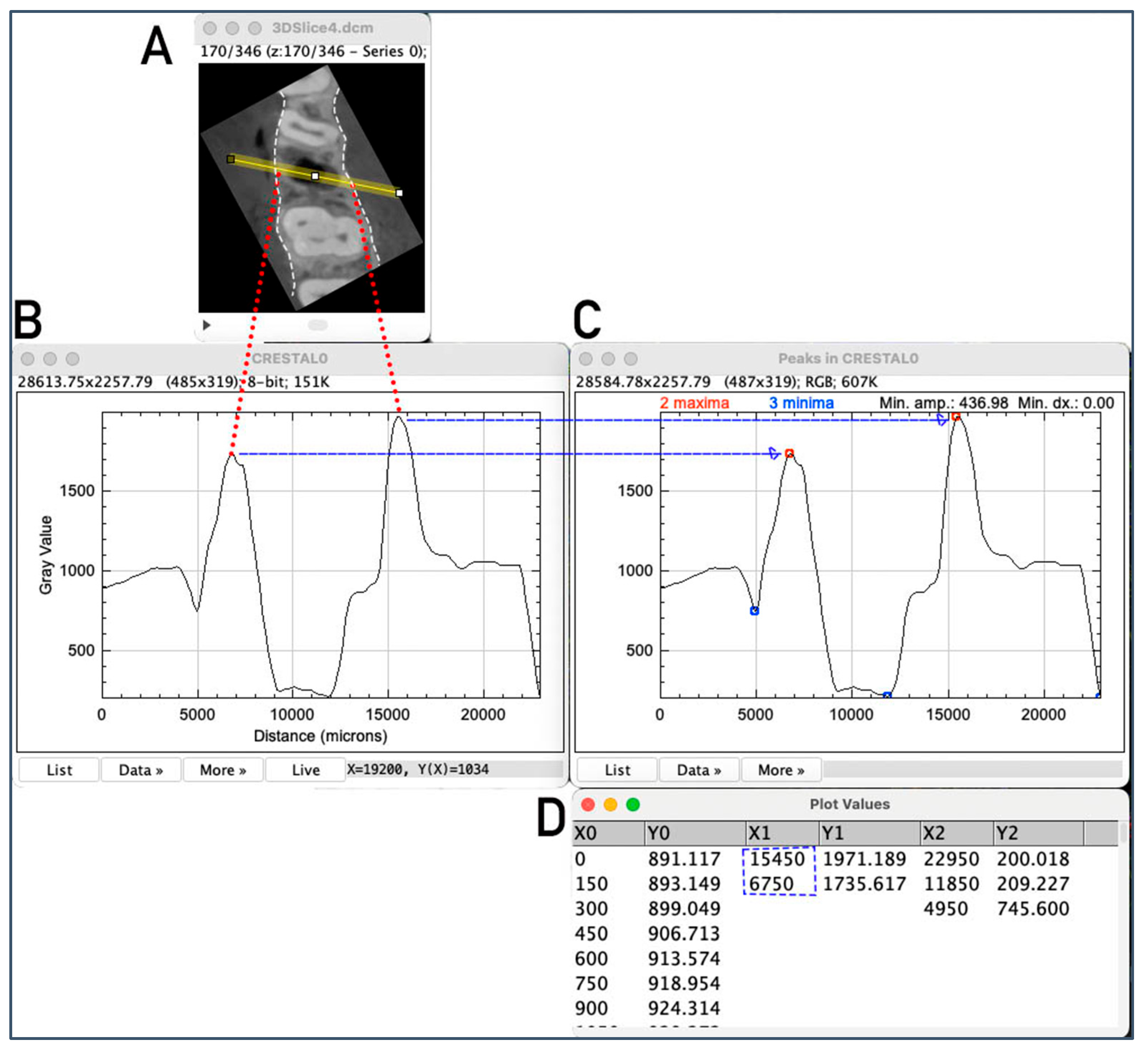
3.1.3. Evaluation of Alveolar Crest Width at the Measurement Positions
3.2. Reproducibility Analysis
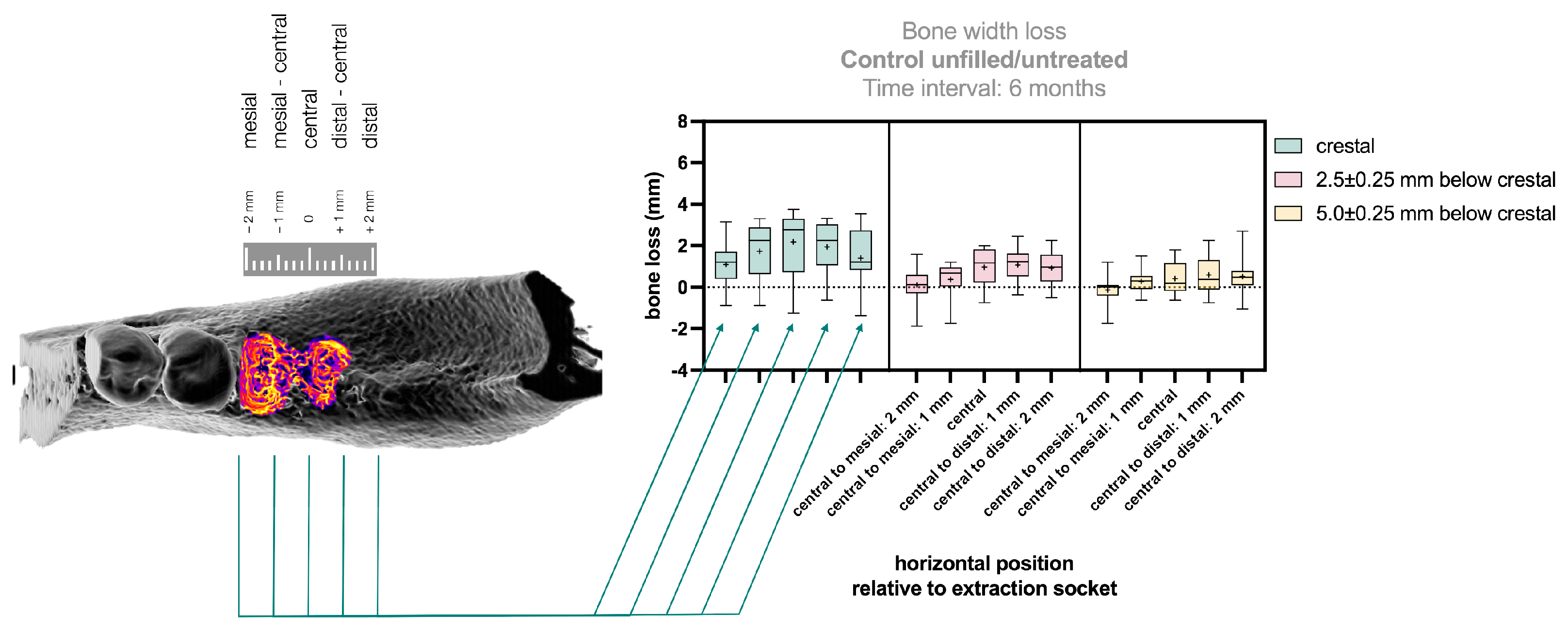
3.3. Application of the Method to Clinical Data
4. Discussion
4.1. Development of a Novel Evaluation Method and Application to Clinical Data
4.2. Strengths and Limitations of Radiological Evaluation
4.3. Clinical Relevance
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PRF | Platelet-Rich Fibrin |
| CBCT | Cone Beam Computer Tomography |
References
- Pagni, G.; Pellegrini, G.; Giannobile, W.V.; Rasperini, G. Postextraction alveolar ridge preservation: Biological basis and treatments. Int. J. Dent. 2012, 2012, 151030. [Google Scholar] [CrossRef]
- Araujo, M.G.; Silva, C.O.; Misawa, M.; Sukekava, F. Alveolar socket healing: What can we learn? Periodontology 2000 2015, 68, 122–134. [Google Scholar] [CrossRef] [PubMed]
- Amler, M.H. The time sequence of tissue regeneration in human extraction wounds. Oral Surg. Oral Med. Oral Pathol. 1969, 27, 309–318. [Google Scholar] [CrossRef] [PubMed]
- Udeabor, S.E.; Heselich, A.; Al-Maawi, S.; Alqahtani, A.F.; Sader, R.; Ghanaati, S. Current Knowledge on the Healing of the Extraction Socket: A Narrative Review. Bioengineering 2023, 10, 1145. [Google Scholar] [CrossRef]
- Trombelli, L.; Farina, R.; Marzola, A.; Bozzi, L.; Liljenberg, B.; Lindhe, J. Modeling and remodeling of human extraction sockets. J. Clin. Periodontol. 2008, 35, 630–639. [Google Scholar] [CrossRef]
- Ghanaati, S.; Smieszek-Wilczewska, J.; Al-Maawi, S.; Heselich, A.; Sader, R. After Extraction, Upper Premolars Undergo Programmed Socket Collapse with Development of Cavitations Rather than Complete Socket Healing: A Radiological Study. Bioengineering 2025, 12, 128. [Google Scholar] [CrossRef]
- Araujo, M.G.; Lindhe, J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J. Clin. Periodontol. 2005, 32, 212–218. [Google Scholar] [CrossRef]
- Cardaropoli, G.; Araujo, M.; Lindhe, J. Dynamics of bone tissue formation in tooth extraction sites. An experimental study in dogs. J. Clin. Periodontol. 2003, 30, 809–818. [Google Scholar] [CrossRef]
- Fickl, S.; Zuhr, O.; Wachtel, H.; Stappert, C.F.; Stein, J.M.; Hurzeler, M.B. Dimensional changes of the alveolar ridge contour after different socket preservation techniques. J. Clin. Periodontol. 2008, 35, 906–913. [Google Scholar] [CrossRef]
- Schropp, L.; Wenzel, A.; Kostopoulos, L.; Karring, T. Bone healing and soft tissue contour changes following single-tooth extraction: A clinical and radiographic 12-month prospective study. Int. J. Periodontics Restor. Dent. 2003, 23, 313–323. [Google Scholar]
- Cawood, J.I.; Howell, R.A. A classification of the edentulous jaws. Int. J. Oral Maxillofac. Surg. 1988, 17, 232–236. [Google Scholar] [CrossRef]
- Chappuis, V.; Engel, O.; Reyes, M.; Shahim, K.; Nolte, L.P.; Buser, D. Ridge alterations post-extraction in the esthetic zone: A 3D analysis with CBCT. J. Dent. Res. 2013, 92 (Suppl. S12), 195S–201S. [Google Scholar] [CrossRef]
- Araujo, M.G.; da Silva, J.C.C.; de Mendonca, A.F.; Lindhe, J. Ridge alterations following grafting of fresh extraction sockets in man. A randomized clinical trial. Clin. Oral Implants Res. 2015, 26, 407–412. [Google Scholar] [CrossRef]
- Pietrokovski, J.; Massler, M. Alveolar ridge resorption following tooth extraction. J. Prosthet. Dent. 1967, 17, 21–27. [Google Scholar] [CrossRef]
- Van der Weijden, F.; Dell’Acqua, F.; Slot, D.E. Alveolar bone dimensional changes of post-extraction sockets in humans: A systematic review. J. Clin. Periodontol. 2009, 36, 1048–1058. [Google Scholar] [CrossRef]
- Kao, S.T.; Scott, D.D. A review of bone substitutes. Oral Maxillofac. Surg. Clin. N. Am. 2007, 19, 513–521. [Google Scholar] [CrossRef]
- Hammerle, C.H.; Araujo, M.G.; Simion, M.; Osteology Consensus, G. Evidence-based knowledge on the biology and treatment of extraction sockets. Clin. Oral Implants Res. 2012, 23 (Suppl. S5), 80–82. [Google Scholar] [CrossRef]
- Avila-Ortiz, G.; Elangovan, S.; Kramer, K.W.; Blanchette, D.; Dawson, D.V. Effect of alveolar ridge preservation after tooth extraction: A systematic review and meta-analysis. J. Dent. Res. 2014, 93, 950–958. [Google Scholar] [CrossRef]
- Darby, I.; Chen, S.T.; Buser, D. Ridge preservation techniques for implant therapy. Int. J. Oral Maxillofac. Implants 2009, 24 (Suppl.), 260–271. [Google Scholar]
- Ten Heggeler, J.M.; Slot, D.E.; Van der Weijden, G.A. Effect of socket preservation therapies following tooth extraction in non-molar regions in humans: A systematic review. Clin. Oral Implants Res. 2011, 22, 779–788. [Google Scholar] [CrossRef]
- Al-Maawi, S.; Becker, K.; Schwarz, F.; Sader, R.; Ghanaati, S. Efficacy of platelet-rich fibrin in promoting the healing of extraction sockets: A systematic review. Int. J. Implant Dent. 2021, 7, 117. [Google Scholar] [CrossRef] [PubMed]
- Alzahrani, A.A.; Murriky, A.; Shafik, S. Influence of platelet rich fibrin on post-extraction socket healing: A clinical and radiographic study. Saudi Dent. J. 2017, 29, 149–155. [Google Scholar] [CrossRef]
- Canellas, J.; da Costa, R.C.; Breves, R.C.; de Oliveira, G.P.; Figueredo, C.; Fischer, R.G.; Thole, A.A.; Medeiros, P.J.D.; Ritto, F.G. Tomographic and histomorphometric evaluation of socket healing after tooth extraction using leukocyte- and platelet-rich fibrin: A randomized, single-blind, controlled clinical trial. J. Craniomaxillofac. Surg. 2020, 48, 24–32. [Google Scholar] [CrossRef]
- Castro, A.B.; Van Dessel, J.; Temmerman, A.; Jacobs, R.; Quirynen, M. Effect of different platelet-rich fibrin matrices for ridge preservation in multiple tooth extractions: A split-mouth randomized controlled clinical trial. J. Clin. Periodontol. 2021, 48, 984–995. [Google Scholar] [CrossRef]
- Girish Kumar, N.; Chaudhary, R.; Kumar, I.; Arora, S.S.; Kumar, N.; Singh, H. To assess the efficacy of socket plug technique using platelet rich fibrin with or without the use of bone substitute in alveolar ridge preservation: A prospective randomised controlled study. Oral Maxillofac. Surg. 2018, 22, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Hauser, F.; Gaydarov, N.; Badoud, I.; Vazquez, L.; Bernard, J.P.; Ammann, P. Clinical and histological evaluation of postextraction platelet-rich fibrin socket filling: A prospective randomized controlled study. Implant Dent. 2013, 22, 295–303. [Google Scholar] [CrossRef]
- Suttapreyasri, S.; Leepong, N. Influence of platelet-rich fibrin on alveolar ridge preservation. J. Craniofac. Surg. 2013, 24, 1088–1094. [Google Scholar] [CrossRef]
- Yewale, M.; Bhat, S.; Kamath, A.; Tamrakar, A.; Patil, V.; Algal, A.S. Advanced platelet-rich fibrin plus and osseous bone graft for socket preservation and ridge augmentation—A randomized control clinical trial. J. Oral Biol. Craniofac. Res. 2021, 11, 225–233. [Google Scholar] [CrossRef]
- Zhang, Y.; Ruan, Z.; Shen, M.; Tan, L.; Huang, W.; Wang, L.; Huang, Y. Clinical effect of platelet-rich fibrin on the preservation of the alveolar ridge following tooth extraction. Exp. Ther. Med. 2018, 15, 2277–2286. [Google Scholar] [CrossRef]
- Tonetti, M.S.; Jung, R.E.; Avila-Ortiz, G.; Blanco, J.; Cosyn, J.; Fickl, S.; Figuero, E.; Goldstein, M.; Graziani, F.; Madianos, P.; et al. Management of the extraction socket and timing of implant placement: Consensus report and clinical recommendations of group 3 of the XV European Workshop in Periodontology. J. Clin. Periodontol. 2019, 46 (Suppl. S21), 183–194. [Google Scholar] [CrossRef]
- Landsberg, C.J. Implementing socket seal surgery as a socket preservation technique for pontic site development: Surgical steps revisited--a report of two cases. J. Periodontol. 2008, 79, 945–954. [Google Scholar] [CrossRef]
- Avila-Ortiz, G.; Chambrone, L.; Vignoletti, F. Effect of alveolar ridge preservation interventions following tooth extraction: A systematic review and meta-analysis. J. Clin. Periodontol. 2019, 46 (Suppl. S21), 195–223. [Google Scholar] [CrossRef] [PubMed]
- Clark, D.; Rajendran, Y.; Paydar, S.; Ho, S.; Cox, D.; Ryder, M.; Dollard, J.; Kao, R.T. Advanced platelet-rich fibrin and freeze-dried bone allograft for ridge preservation: A randomized controlled clinical trial. J. Periodontol. 2018, 89, 379–387. [Google Scholar] [CrossRef] [PubMed]
- Srinivas, B.; Das, P.; Rana, M.M.; Qureshi, A.Q.; Vaidya, K.C.; Ahmed Raziuddin, S.J. Wound Healing and Bone Regeneration in Postextraction Sockets with and without Platelet-rich Fibrin. Ann. Maxillofac. Surg. 2018, 8, 28–34. [Google Scholar]
- Temmerman, A.; Vandessel, J.; Castro, A.; Jacobs, R.; Teughels, W.; Pinto, N.; Quirynen, M. The use of leucocyte and platelet-rich fibrin in socket management and ridge preservation: A split-mouth, randomized, controlled clinical trial. J. Clin. Periodontol. 2016, 43, 990–999. [Google Scholar] [CrossRef]
- Thakkar, D.J.; Deshpande, N.C.; Dave, D.H.; Narayankar, S.D. A comparative evaluation of extraction socket preservation with demineralized freeze-dried bone allograft alone and along with platelet-rich fibrin: A clinical and radiographic study. Contemp. Clin. Dent. 2016, 7, 371–376. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Ingole, S.; Deshpande, M.; Ranadive, P.; Sharma, S.; Kazi, N.; Rajurkar, S. Influence of platelet-rich fibrin on wound healing and bone regeneration after tooth extraction: A clinical and radiographic study. J. Oral Biol. Craniofac. Res. 2020, 10, 385–390. [Google Scholar] [CrossRef]
- Abellan, D.; Barallat, L.; Vilarrasa, J.; Cabezas, M.; Pascual La Rocca, A.; Valles, C.; Nart, J. Ridge preservation in molar sites comparing xenograft versus mineralized freeze-dried bone allograft: A randomized clinical trial. Clin. Oral Implants Res. 2022, 33, 511–523. [Google Scholar] [CrossRef]
- Schindelin, J.; Arganda-Carreras, I.; Frise, E.; Kaynig, V.; Longair, M.; Pietzsch, T.; Preibisch, S.; Rueden, C.; Saalfeld, S.; Schmid, B.; et al. Fiji: An open-source platform for biological-image analysis. Nat. Methods 2012, 9, 676–682. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Monje, A.; Gonzalez-Martin, O.; Avila-Ortiz, G. Impact of peri-implant soft tissue characteristics on health and esthetics. J. Esthet. Restor. Dent. 2023, 35, 183–196. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.C.; Huang, Y.C.; Ding, S.J. Primary stability of implant placement and loading related to dental implant materials and designs: A literature review. J. Dent. Sci. 2023, 18, 1467–1476. [Google Scholar] [CrossRef] [PubMed]
- Heselich, A.; Neff, P.; Śmieszek-Wilczewska, J.; Sader, R.; Ghanaati, S. Introduction of a Semi-Quantitative Image-Based Analysis Tool for CBCT-Based Evaluation of Bone Regeneration in Tooth Extraction Sockets. Bioengineering 2025, 12, 301. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heselich, A.; Śmieszek-Wilczewska, J.; Boyo, L.; Sader, R.; Ghanaati, S. Development of Semi-Automated Image-Based Analysis Tool for CBCT Evaluation of Alveolar Ridge Changes After Tooth Extraction. Bioengineering 2025, 12, 307. https://doi.org/10.3390/bioengineering12030307
Heselich A, Śmieszek-Wilczewska J, Boyo L, Sader R, Ghanaati S. Development of Semi-Automated Image-Based Analysis Tool for CBCT Evaluation of Alveolar Ridge Changes After Tooth Extraction. Bioengineering. 2025; 12(3):307. https://doi.org/10.3390/bioengineering12030307
Chicago/Turabian StyleHeselich, Anja, Joanna Śmieszek-Wilczewska, Louisa Boyo, Robert Sader, and Shahram Ghanaati. 2025. "Development of Semi-Automated Image-Based Analysis Tool for CBCT Evaluation of Alveolar Ridge Changes After Tooth Extraction" Bioengineering 12, no. 3: 307. https://doi.org/10.3390/bioengineering12030307
APA StyleHeselich, A., Śmieszek-Wilczewska, J., Boyo, L., Sader, R., & Ghanaati, S. (2025). Development of Semi-Automated Image-Based Analysis Tool for CBCT Evaluation of Alveolar Ridge Changes After Tooth Extraction. Bioengineering, 12(3), 307. https://doi.org/10.3390/bioengineering12030307





