Use of Wearable Inertial Sensors to Assess Trunk and Cervical Postures Among Surgeons: Effect of Surgical Specialties and Roles
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Data Collection and Processing
2.3. Statistical Analysis
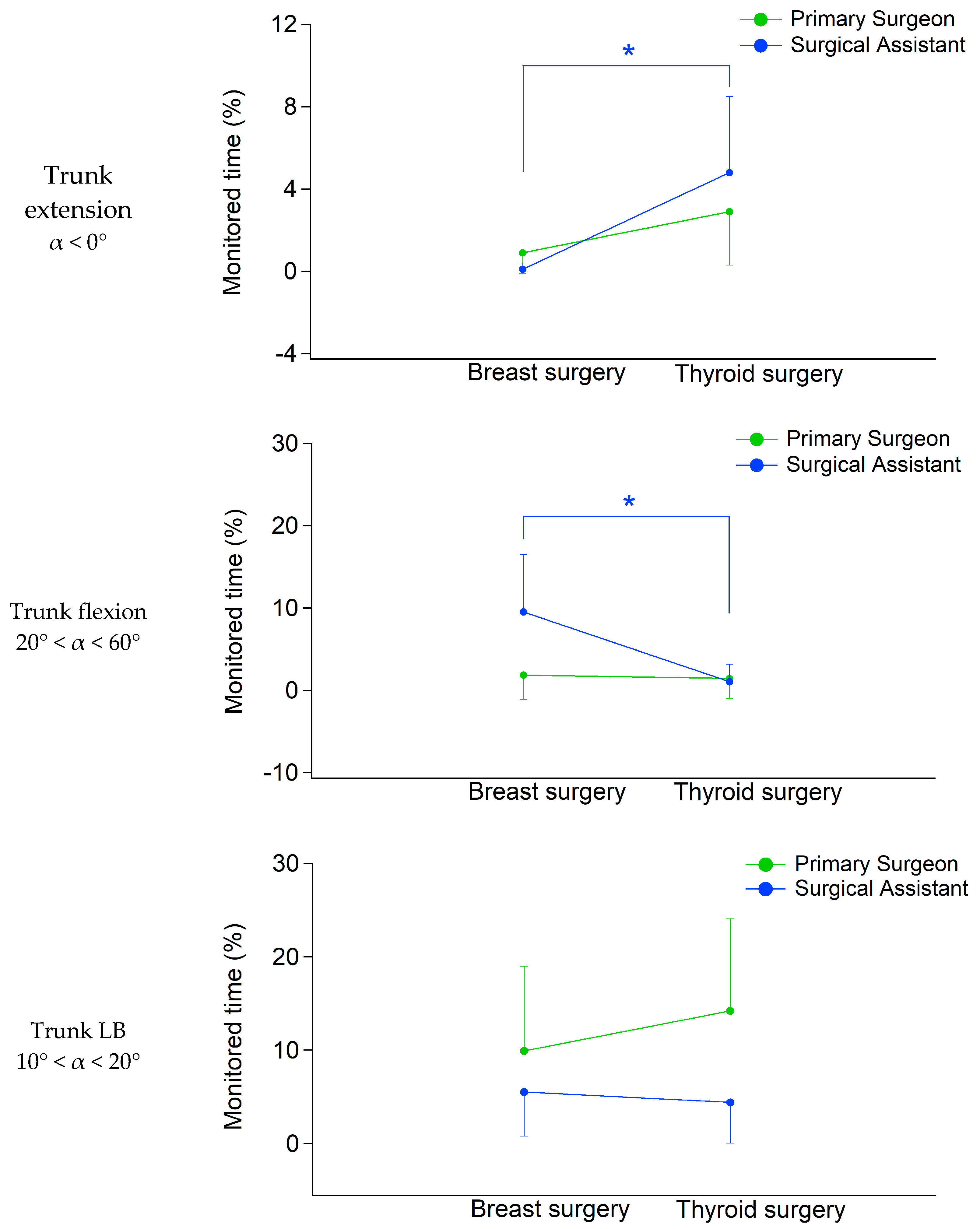
- Two-way MANOVA carried out by setting the surgery (i.e., breast vs. thyroid) and the role (i.e., primary surgeon vs. surgical assistant) as independent variables and trunk posture parameters (i.e., percentage of time spent in different classes of trunk FE and LB) as dependent variables;
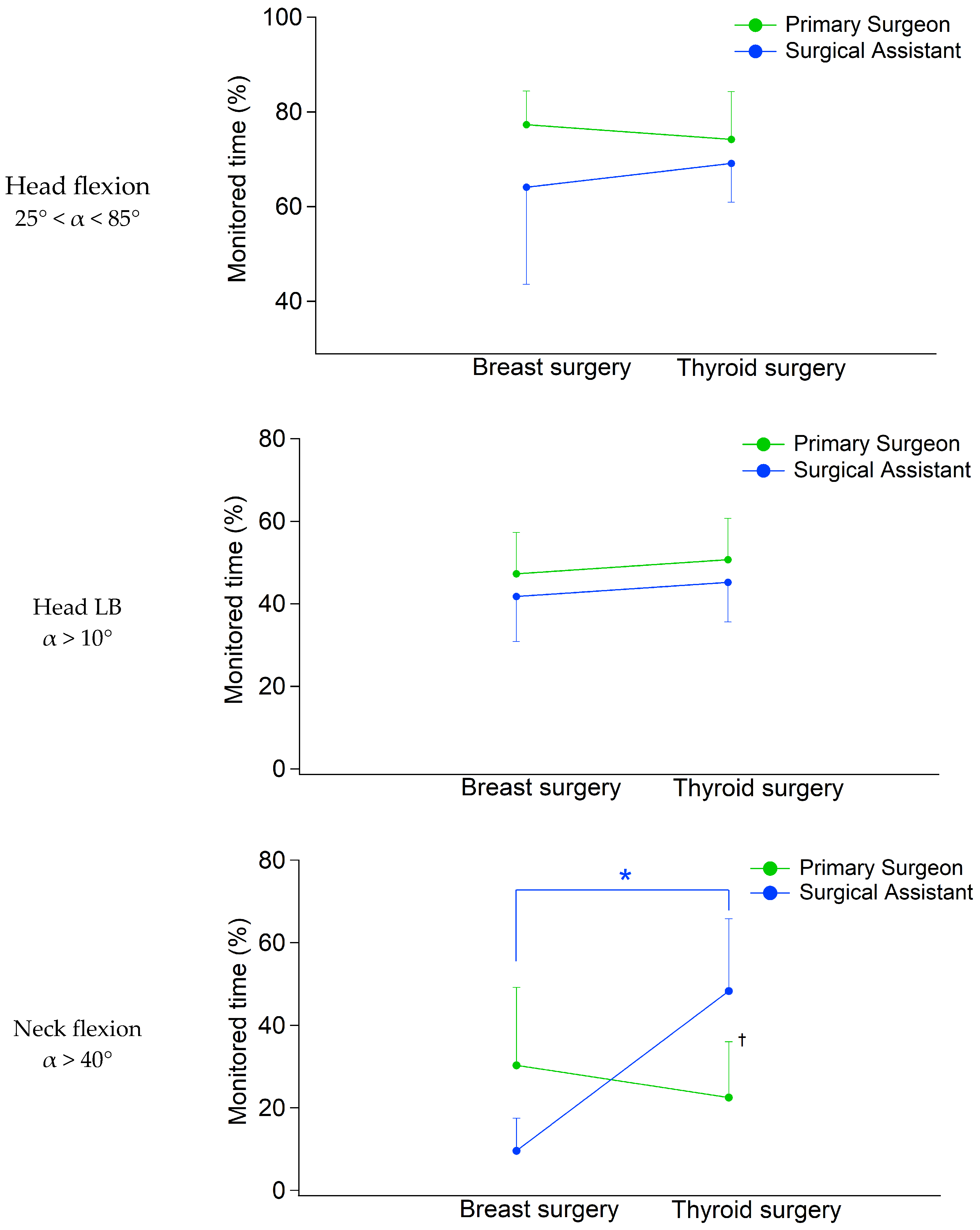
- Two-way MANOVA carried out by setting the surgery (i.e., breast vs. thyroid) and the role (i.e., primary surgeon vs. surgical assistant) as independent variables and head/neck posture parameters (i.e., percentage of time spent in different classes of head FE, head LB, and neck FE) as dependent variables.
3. Results
3.1. Trunk
3.2. Head and Neck
4. Discussion
4.1. Effect of the Surgical Specialty on Trunk, Head and Neck Postures
4.2. Effect of the Surgical Role on Trunk, Head and Neck Posture
4.3. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| WMSDs | Work-related Musculoskeletal Disorders; |
| MIS | Minimally Invasive Surgeries; |
| IMUs | Inertial Measurement Units; |
| FE | Flexion–Extension; |
| LB | Lateral Bending |
References
- Szeto, G.P.; Ho, P.; Ting, A.C.; Poon, J.T.; Cheng, S.W.; Tsang, R.C. Work-related musculoskeletal symptoms in surgeons. J. Occup. Rehabil. 2009, 19, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Howarth, A.L.; Hallbeck, S.; Mahabir, R.C.; Lemaine, V.; Evans, G.R.; Noland, S.S. Work-related musculoskeletal discomfort and injury in microsurgeons. J. Reconstr. Microsurg. 2019, 35, 322–328. [Google Scholar] [CrossRef]
- Jacquier-Bret, J.; Gorce, P. Prevalence of body area work-related musculoskeletal disorders among healthcare professionals: A systematic review. Int. J. Environ. Res. Public Health 2023, 20, 841. [Google Scholar] [CrossRef] [PubMed]
- Berguer, R.; Rab, G.T.; Abu-Ghaida, H.; Alarcon, A.; Chung, J. A comparison of surgeons’ posture during laparoscopic and open surgical procedures. Surg. Endosc. 1997, 11, 139–142. [Google Scholar] [CrossRef] [PubMed]
- Aaron, K.A.; Vaughan, J.; Gupta, R.; Ali, N.E.S.; Beth, A.H.; Moore, J.M.; Vaisbuch, Y. The risk of ergonomic injury across surgical specialties. PLoS ONE 2021, 16, e0244868. [Google Scholar] [CrossRef]
- Merbah, J.; Caré, B.R.; Gorce, P.; Gadea, F.; Prince, F. A new approach to quantifying muscular fatigue using wearable EMG sensors during surgery: An ergonomic case study. Sensors 2023, 23, 1686. [Google Scholar] [CrossRef]
- Catanzarite, T.; Tan-Kim, J.; Whitcomb, E.L.; Menefee, S. Ergonomics in surgery: A review. Urogynecology 2018, 24, 1–12. [Google Scholar] [CrossRef]
- Stucky, C.C.H.; Cromwell, K.D.; Voss, R.K.; Chiang, Y.J.; Woodman, K.; Lee, J.E.; Cormier, J.N. Surgeon symptoms, strain, and selections: Systematic review and meta-analysis of surgical ergonomics. Ann. Med. Surg. 2018, 27, 1–8. [Google Scholar] [CrossRef]
- Gorce, P.; Jacquier-Bret, J. Work-related musculoskeletal disorders among surgeons: A bibliometric analysis from 1982 to 2024. Explor. Musculoskelet. Dis. 2024, 2, 317–335. [Google Scholar] [CrossRef]
- Jensen, M.J.; Pagedar, N.A.; Sugg, S.L.; Lal, G. Endocrine surgeons have high rates of work-related musculoskeletal (MSK) injury and symptoms. Am. J. Surg. 2022, 224, 315–318. [Google Scholar] [CrossRef]
- Ho, T.V.T.; Hamill, C.S.; Sykes, K.J.; Kraft, S.M. Work-related musculoskeletal symptoms among otolaryngologists by subspecialty: A national survey. Laryngoscope 2018, 128, 632–640. [Google Scholar] [CrossRef] [PubMed]
- Davidson, B.J.; Guardiani, E.; Wang, A. Adopting the operating microscope in thyroid surgery: Safety, efficiency, and ergonomics. Head Neck J. Sci. Spec. Head Neck 2010, 32, 154–159. [Google Scholar] [CrossRef]
- Dwyer, A.; Huckleby, J.; Kabbani, M.; Delano, A.; De Sutter, M.; Crawford, D. Ergonomic assessment of robotic general surgeons: A pilot study. J. Robot. Surg. 2020, 14, 387–392. [Google Scholar] [CrossRef]
- Zihni, A.M.; Cavallo, J.A.; Ray, S.; Ohu, I.; Cho, S.; Awad, M.M. Ergonomic analysis of primary and assistant surgical roles. J. Surg. Res. 2016, 203, 301–305. [Google Scholar] [CrossRef]
- Yurteri-Kaplan, L.A.; Zhu, X.; Iglesia, C.B.; Gutman, R.E.; Sokol, A.I.; Paquet, V.; Park, A.J. Differences in postural loading between primary and assistant surgeons during vaginal surgery. Int. J. Ind. Ergon. 2018, 65, 60–67. [Google Scholar] [CrossRef]
- Lee, G.; Lee, T.; Dexter, D.; Godinez, C.; Meenaghan, N.; Catania, R.; Park, A. Ergonomic risk associated with assisting in minimally invasive surgery. Surg. Endosc. 2009, 23, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Epstein, S.; Sparer, E.H.; Tran, B.N.; Ruan, Q.Z.; Dennerlein, J.T.; Singhal, D.; Lee, B.T. Prevalence of work-related musculoskeletal disorders among surgeons and interventionalists: A systematic review and meta-analysis. JAMA Surg. 2018, 153, e174947. [Google Scholar] [CrossRef] [PubMed]
- ISO 11226; Ergonomics Evaluation of Static Working Postures. International Organization for Standardization: Geneva, Switzerland, 2000.
- Porta, M.; Orrù, P.F.; Pau, M. Use of wearable sensors to assess patterns of trunk flexion in young and old workers in the Metalworking Industry. Ergonomics 2021, 64, 1543–1554. [Google Scholar] [CrossRef]
- Porta, M.; Porceddu, S.; Mura, G.M.; Campagna, M.; Pau, M. Continuous assessment of trunk posture in healthcare workers assigned to wards with different MAPO index. Ergonomics 2023, 66, 875–885. [Google Scholar] [CrossRef]
- Faber, G.S.; Kingma, I.; Bruijn, S.M.; van Dieën, J.H. Optimal inertial sensor location for ambulatory measurement of trunk inclination. J. Biomech. 2009, 42, 2406–2409. [Google Scholar] [CrossRef]
- Ionut-Cristian, S.; Dan-Marius, D. Using inertial sensors to determine head motion—A review. J. Imaging 2021, 7, 265. [Google Scholar] [CrossRef]
- Hoogendoorn, W.E.; Bongers, P.M.; De Vet, H.C.; Douwes, M.; Koes, B.W.; Miedema, M.C.; Bouter, L.M. Flexion and rotation of the trunk and lifting at work are risk factors for low back pain: Results of a prospective cohort study. Spine 2000, 25, 3087–3092. [Google Scholar] [CrossRef] [PubMed]
- Nimbarte, A.D.; Sivak-Callcott, J.A.; Zreiqat, M.; Chapman, M. Neck postures and cervical spine loading among microsurgeons operating with loupes and headlamp. IIE Trans. Occup. Ergon. Hum. Factors 2013, 1, 215–223. [Google Scholar] [CrossRef]
- Hansraj, K.K. Assessment of stresses in the cervical spine caused by posture and position of the head. Surg. Technol. Int. 2014, 25, 277–279. [Google Scholar] [PubMed]
- Zhang, C.; Roossien, C.C.; Verkerke, G.J.; Houdijk, H.; Hijmans, J.M.; Greve, C. Biomechanical Load of Neck and Lumbar Joints in Open-Surgery Training. Sensors 2023, 23, 6974. [Google Scholar] [CrossRef]
- Rodman, C.; Kelly, N.; Niermeyer, W.; Banks, L.; Onwuka, A.; Mason, E.; Chiang, T. Quantitative assessment of surgical ergonomics in otolaryngology. Otolaryngol. Head Neck Surg. 2020, 163, 1186–1193. [Google Scholar] [CrossRef]
- Kant, I.J.; de Jong, L.C.G.M.; van Rijssen-Moll, M.; Borm, P.J.A. A survey of static and dynamic work postures of operating room staff. Int. Arch. Occup. Environ. Health 1992, 63, 423–428. [Google Scholar] [CrossRef]
- Szeto, G.P.; Cheng, S.W.; Poon, J.T.; Ting, A.C.; Tsang, R.C.; Ho, P. Surgeons’ static posture and movement repetitions in open and laparoscopic surgery. J. Surg. Res. 2012, 172, e19–e31. [Google Scholar] [CrossRef]
- Yang, L.; Wang, T.; Weidner, T.K.; Madura, J.A.; Morrow, M.M.; Hallbeck, M.S. Intraoperative musculoskeletal discomfort and risk for surgeons during open and laparoscopic surgery. Surg. Endosc. 2021, 35, 6335–6343. [Google Scholar] [CrossRef]
- Norasi, H.; Tetteh, E.; Money, S.R.; Davila, V.J.; Meltzer, A.J.; Morrow, M.M.; Hallbeck, M.S. Intraoperative posture and workload assessment in vascular surgery. Appl. Ergon. 2021, 92, 103344. [Google Scholar] [CrossRef]
- Zhu, X.; Yurteri-kaplan, L.A.; Gutman, R.E.; Sokol, A.; Iglesias, C.B.; Park, A.; Paquet, V. Postural stress experienced by vaginal surgeons. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2014, 58, 763–767. [Google Scholar] [CrossRef]
- Leung, K.L.; Segal, R.M.; Bernstein, J.D.; Orosco, R.K.; Reid, C.M. Surgical ergonomics: Assessment of surgeon posture and impact of training device during otolaryngology procedures. Laryngoscope Investig. Otolaryngol. 2022, 7, 1351–1359. [Google Scholar] [CrossRef] [PubMed]
- Tetteh, E.; Wang, T.; Kim, J.Y.; Smith, T.; Norasi, H.; Van Straaten, M.G.; Hallbeck, M.S. Optimizing ergonomics during open, laparoscopic, and robotic-assisted surgery: A review of surgical ergonomics literature and development of educational illustrations. Am. J. Surg. 2024, 235, 115551. [Google Scholar] [CrossRef] [PubMed]
- Ronstrom, C.; Hallbeck, S.; Lowndes, B.; Chrouser, K.L. Surgical ergonomics. Surgeons as Educators: A Guide for Academic Development and Teaching Excellence; Springer: Cham, Switzerland, 2018; pp. 387–417. [Google Scholar] [CrossRef]
- Bhat, S.; Chia, B.; Babidge, W.; Maddern, G.J. Assessing performance in ageing surgeons: Systematic review. Br. J. Surg. 2023, 110, 1425–1427. [Google Scholar] [CrossRef]


| Thyroid Surgery | Breast Surgery | |||
|---|---|---|---|---|
| Primary Surgeons | Surgical Assistants | Primary Surgeons | Surgical Assistants | |
| Participants | 7M | 7M | 7M | 7 (6M, 1F) |
| Age (years) | 55.7 (3.4) | 40.4 (9.0) † | 50.8 (9.2) | 56.1 (6.4) * |
| Height (cm) | 175.7 (0.4) | 172.4 (4.1) | 173.4 (2.3) | 167.6 (4.6) *,† |
| Body mass (kg) | 78.4 (7.8) | 71.9 (10.9) | 79.0 (10.4) | 64.3 (14.2) † |
| Seniority at work (years) | 30.9 (5.4) | 10.4 (7.9) † | 18.7 (13.1) * | 18.7 (9.3) |
| Body Segment | Movement | ISO 11226 Class | Description |
|---|---|---|---|
| Trunk | Extension | α < 0° | Not recommended |
| Flexion | 0° < α < 20° | Always acceptable | |
| 20° < α < 60° | Conditionally acceptable | ||
| α > 60° | Not recommended | ||
| Lateral Bending (+ → right;− → left) | 0° < α < 10° | Always acceptable | |
| 10° < α < 20° | Not recommended | ||
| α > 20° | Not recommended | ||
| Head | Extension | α < 0° | Not recommended |
| Flexion | 0° < α < 25° | Always acceptable | |
| 25° < α < 85° | Conditionally acceptable | ||
| α > 85° | Not recommended | ||
| Lateral Bending a (+ → right;− → left) | 0° < α < 10° | Always acceptable | |
| α > 10° | Not recommended | ||
| Neck | Extension | α < 0° | Not recommended |
| Flexion | α < 40° | Always acceptable | |
| α > 40° | Not recommended |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Casu, G.; Porta, M.; Lecca, L.I.; Murru, A.; Medas, F.; Pau, M.; Campagna, M. Use of Wearable Inertial Sensors to Assess Trunk and Cervical Postures Among Surgeons: Effect of Surgical Specialties and Roles. Bioengineering 2025, 12, 299. https://doi.org/10.3390/bioengineering12030299
Casu G, Porta M, Lecca LI, Murru A, Medas F, Pau M, Campagna M. Use of Wearable Inertial Sensors to Assess Trunk and Cervical Postures Among Surgeons: Effect of Surgical Specialties and Roles. Bioengineering. 2025; 12(3):299. https://doi.org/10.3390/bioengineering12030299
Chicago/Turabian StyleCasu, Giulia, Micaela Porta, Luigi Isaia Lecca, Alessandro Murru, Fabio Medas, Massimiliano Pau, and Marcello Campagna. 2025. "Use of Wearable Inertial Sensors to Assess Trunk and Cervical Postures Among Surgeons: Effect of Surgical Specialties and Roles" Bioengineering 12, no. 3: 299. https://doi.org/10.3390/bioengineering12030299
APA StyleCasu, G., Porta, M., Lecca, L. I., Murru, A., Medas, F., Pau, M., & Campagna, M. (2025). Use of Wearable Inertial Sensors to Assess Trunk and Cervical Postures Among Surgeons: Effect of Surgical Specialties and Roles. Bioengineering, 12(3), 299. https://doi.org/10.3390/bioengineering12030299










