Expandable Interbody Cages in 1–3 Level Circumferential Lumbar Arthrodesis with 2-Year Follow up: A Retrospective Study
Abstract
1. Introduction
2. Methods
2.1. Patient Population
2.2. Surgical Procedures
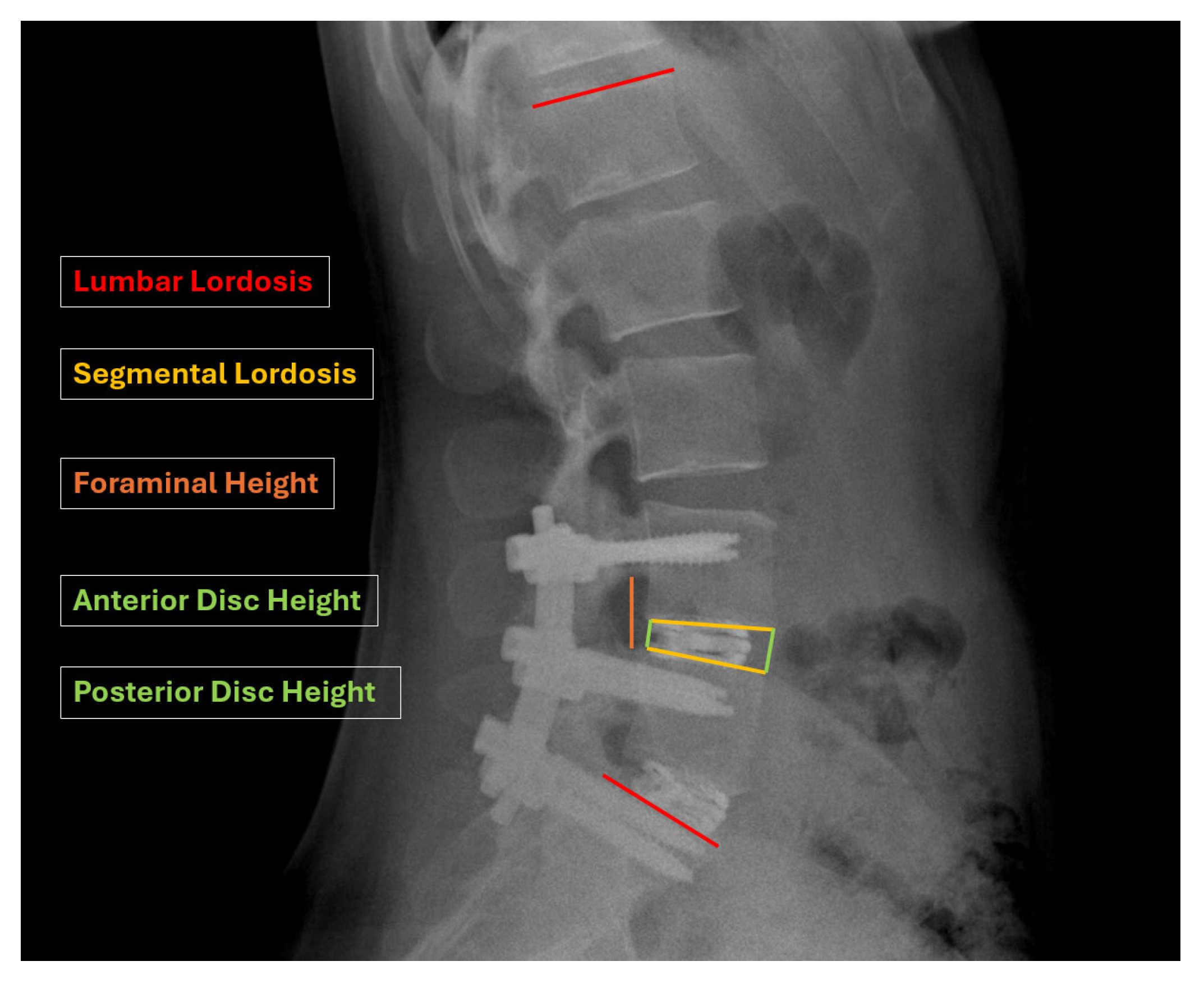
2.3. Radiographic Measures
2.4. Statistical Analysis
3. Results
3.1. Demographics
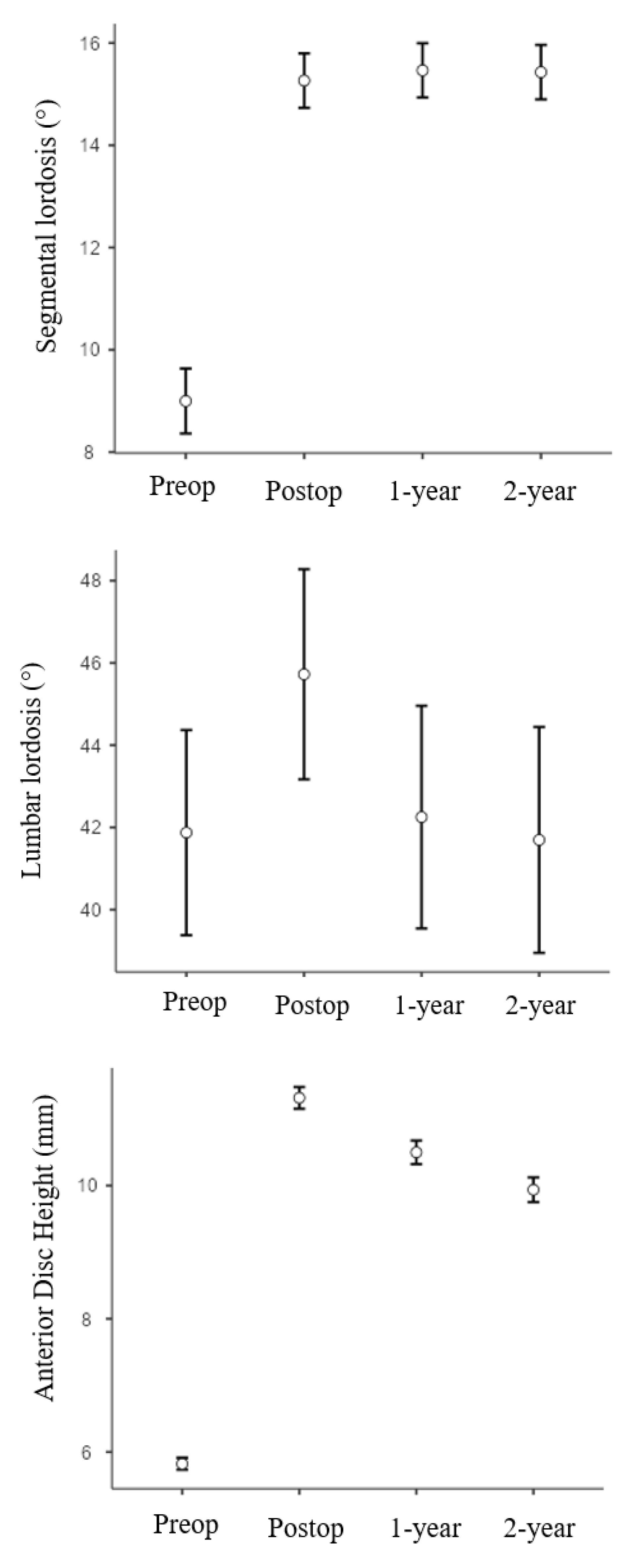
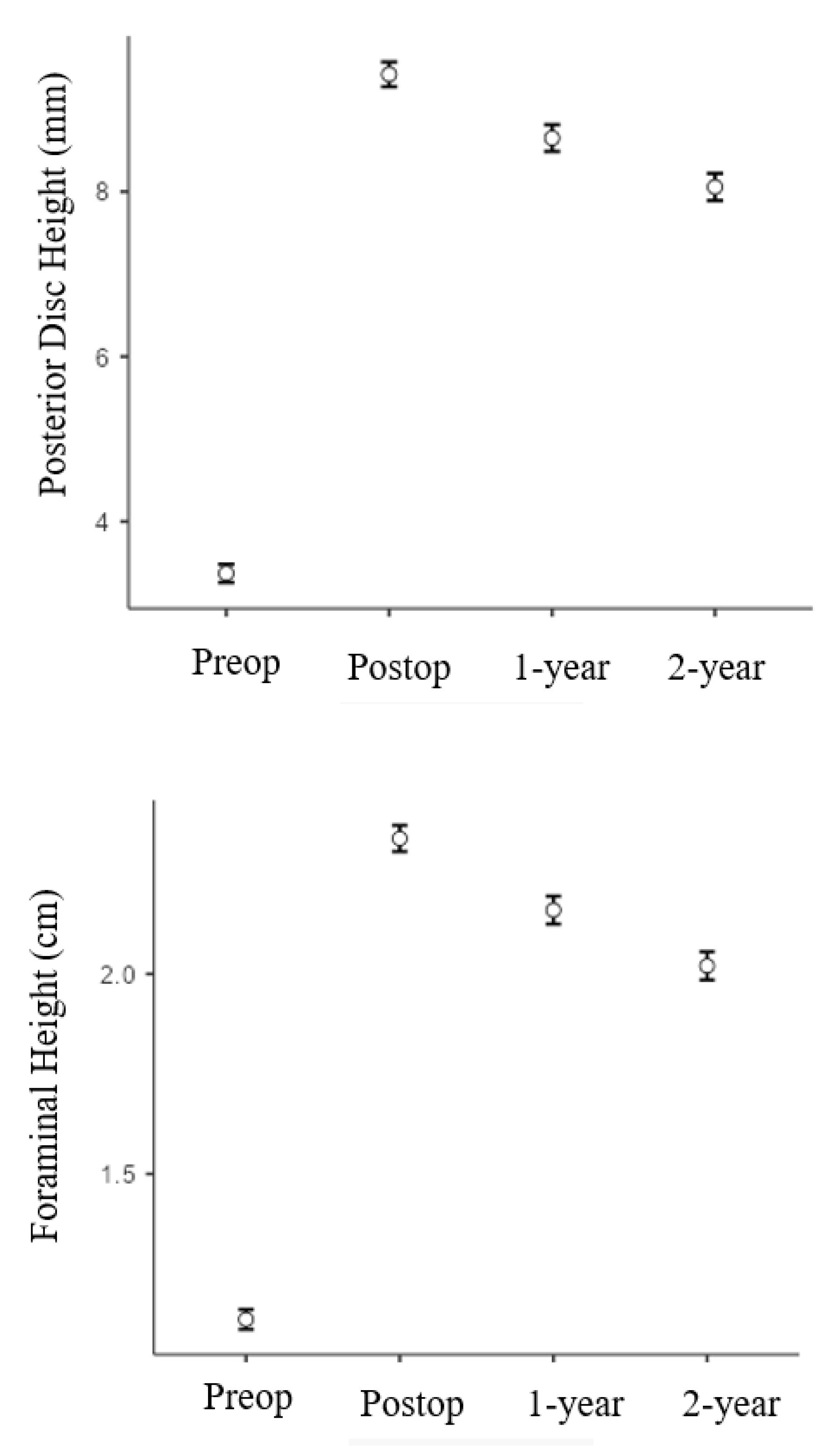
3.2. Radiographic Results
3.3. Complications
4. Discussion
Strengths and Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mobbs, R.J.; Phan, K.; Malham, G.; Seex, K.; Rao, P.J. Lumbar interbody fusion: Techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J. Spine Surg. 2015, 1, 2–18. [Google Scholar] [PubMed]
- Chen, D.; Fay, L.A.; Lok, J.; Yuan, P.; Edwards, W.T.; Yuan, H.A. Increasing neuroforaminal volume by anterior interbody distraction in degenerative lumbar spine. Spine 1995, 20, 74–79. [Google Scholar] [CrossRef] [PubMed]
- Calvachi-Prieto, P.; McAvoy, M.B.; Cerecedo-Lopez, C.D.; Lu, Y.; Chi, J.H.; Aglio, L.S.; Smith, T.R.; Gormley, W.B.; Groff, M.W.; Mekary, R.A.; et al. Expandable versus static cages in minimally invasive lumbar interbody fusion: A systematic review and meta-analysis. World Neurosurg. 2021, 151, e607–e614. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.M.; Frisch, R.F.; Huang, Z.; Towner, J.; Li, Y.I.; Greeley, S.L.; Ledonio, C. Comparative effectiveness of expandable versus static interbody spacers via MIS LLIF: A 2-year radiographic and clinical outcomes study. Glob. Spine J. 2020, 10, 998–1005. [Google Scholar] [CrossRef]
- Elgafy, H.; Behrens, K. Comparing expandable and static interbody cages in lumbar interbody fusion. J. Spine Surg. 2023, 9, 1–5. [Google Scholar] [CrossRef]
- Kucharzyk, D.W.; Budimir, D.; Waldorff, E.I.; Shum, L.C.; Vannabouathong, C. The effect of expandable versus static lordotic interbody implants in minimally invasive spine surgery: Patient reported outcomes, sagittal alignment, and restoration of disc height and foraminal height. J. Spine Surg. 2023, 9, 39–53. [Google Scholar] [CrossRef]
- Zdeblick, T.A.; Phillips, F.M. Interbody cage devices. Spine 2003, 28 (Suppl. S15), S2–S7. [Google Scholar] [CrossRef]
- Marchi, L.; Abdala, N.; Oliveira, L.; Amaral, R.; Coutinho, E.; Pimenta, L. Radiographic and clinical evaluation of cage subsidence after stand-alone lateral interbody fusion. J. Neurosurg. Spine 2013, 19, 110–118. [Google Scholar] [CrossRef]
- Schwab, F.J.; Blondel, B.; Bess, S.; Hostin, R.; Shaffrey, C.I.; Smith, J.S.; Boachie-Adjei, O.; Burton, D.C.; Akbarnia, B.A.; Mundis, G.M.; et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: A prospective multicenter analysis. Spine 2013, 38, E803–E812. [Google Scholar] [CrossRef]
- Macki, M.; Hamilton, T.; Haddad, Y.W.; Chang, V. Expandable cage technology-transforaminal, anterior, and lateral lumbar interbody fusion. Oper. Neurosurg. 2021, 21 (Suppl. S1), S69–S80. [Google Scholar] [CrossRef]
- Kumar, M.N.; Baklanov, A.; Chopin, D. Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur. Spine J. 2001, 10, 314–319. [Google Scholar] [CrossRef]
- Barrey, C.; Darnis, A. Current strategies for the restoration of adequate lordosis during lumbar fusion. World J. Orthop. 2015, 6, 117–126. [Google Scholar] [CrossRef] [PubMed]
- Vaishnav, A.S.; Saville, P.; McAnany, S.; Kirnaz, S.; Wipplinger, C.; Navarro-Ramirez, R.; Hartl, R.; Yang, J.; Gang, C.H.; Qureshi, S.A. Retrospective review of immediate restoration of lordosis in single-level minimally invasive transforaminal lumbar interbody fusion: A comparison of static and expandable interbody cages. Oper. Neurosurg. 2020, 18, 518–523. [Google Scholar] [CrossRef] [PubMed]
- Cheng, B.C.; Swink, I.; Yusufbekov, R.; Birgelen, M.; Ferrara, L.; Coric, D. Current concepts of contemporary expandable lumbar interbody fusion cage designs, part 2: Feasibility assessment of an endplate conforming bidirectional expandable interbody cage. Int. J. Spine Surg. 2020, 14 (Suppl. S3), S68–S74. [Google Scholar] [CrossRef] [PubMed]
- Torretti, J.; Harris, J.A.; Bucklen, B.S.; Moldavsky, M.; Khalil, S.E.D. In vitro biomechanical and fluoroscopic study of a continuously expandable interbody spacer concerning its role in insertion force and segmental kinematics. Asian Spine J. 2018, 12, 601–610. [Google Scholar] [CrossRef]
- Weinstein, M.A.; Ayala, G.A.; Roura, R.; Christmas, K.N.; Warren, D.H.; Simon, P. Transforaminal lumbar interbody fusion with an expandable inter-body device: Two-year clinical and radiographic outcomes. N. Am. Spine Soc. J. 2023, 16, 100286. [Google Scholar]
- Boktor, J.G.; Pockett, R.D.; Verghese, N. The expandable transforaminal lumbar interbody fusion—Two years follow-up. J. Craniovertebr. Junction Spine 2018, 9, 50–55. [Google Scholar] [CrossRef]
- Alimi, M.; Shin, B.; Macielak, M.; Hofstetter, C.P.; Njoku, I., Jr.; Tsiouris, A.J.; Elowitz, E.; Härtl, R. Expandable polyaryl-ether-ether-ketone spacers for interbody distraction in the lumbar spine. Glob. Spine J. 2015, 5, 169–178. [Google Scholar] [CrossRef]
- Mulvaney, G.; Monk, S.; Clemente, J.D.; Pfortmiller, D.; Coric, D. Expandable interbody spacers: A two-year study evaluating radiologic and clinical outcomes with patient-reported outcomes. Int. J. Spine Surg. 2020, 14 (Suppl. S3), S31–S38. [Google Scholar] [CrossRef]
- Jitpakdee, K.; Sommer, F.; Gouveia, E.; Mykolajtchuk, C.; Boadi, B.; Berger, J.; Hussain, I.; Härtl, R. Expandable cages that expand both height and lordosis provide improved immediate effect on sagittal alignment and short-term clinical outcomes following minimally invasive transforaminal lumbar interbody fusion (MIS TLIF). J. Spine Surg. 2024, 10, 55–67. [Google Scholar] [CrossRef]
- Kim, C.W.; Doerr, T.M.; Luna, I.Y.; Joshua, G.; Shen, S.R.; Fu, X.; Wu, A.M. Minimally invasive transforaminal lumbar interbody fusion using expandable technology: A clinical and radiographic analysis of 50 patients. World Neurosurg. 2016, 90, 228–235. [Google Scholar] [CrossRef]
- Woodward, J.; Koro, L.; Richards, D.; Keegan, C.; Fessler, R.D.; Fessler, R.G. Expandable versus static transforaminal lumbar interbody fusion cages: 1-year radiographic parameters and patient-reported outcomes. World Neurosurg. 2022, 159, e1–e7. [Google Scholar] [CrossRef]
- Jagannathan, J.; Sansur, C.A.; Oskouian, R.J., Jr.; Fu, K.M.; Shaffrey, C.I. Radiographic restoration of lumbar alignment after transforaminal lumbar interbody fusion. Neurosurgery 2009, 64, 955–963. [Google Scholar] [CrossRef]
- Alvi, M.A.; Kurian, S.J.; Wahood, W.; Goyal, A.; Elder, B.D.; Bydon, M. Assessing the difference in clinical and radiologic outcomes between expandable cage and nonexpandable cage among patients undergoing minimally invasive transforaminal interbody fusion: A systematic review and meta-analysis. World Neurosurg. 2019, 127, 596–606.e1. [Google Scholar] [CrossRef]
- Lin, G.X.; Kim, J.S.; Kotheeranurak, V.; Chen, C.M.; Hu, B.S.; Rui, G. Does the application of expandable cages in TLIF provide improved clinical and radiological results compared to static cages? A meta-analysis. Front. Surg. 2022, 9, 949938. [Google Scholar] [CrossRef]
- Crawford, A.M.; Striano, B.M.; Bryan, M.R.; Amakiri, I.C.; Williams, D.L.; Nguyen, A.T.; Hatton, M.O.; Simpson, A.K.; Schoenfeld, A.J. Expandable versus Static Transforaminal Lumbar Interbody Fusion (TLIF) Cages: Comparing Radiographic Outcomes and Complication Profiles. Spine J. 2025, 25, 237–243. [Google Scholar] [CrossRef]


| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Degenerative disease from 1 to 3 continuous level(s) between L1 and S1; Age ≥ 18 years; 1–3 levels circumferential lumbar arthrodesis with expandable interbody cages; Minimum radiographic follow-up of 2 years; Failed conservative treatment (minimum 6 months) | Age < 18 years Prior fusion or surgery Trauma Tumor Surgical operation using cages different from expandable cages |
| Number of Patients | 71 |
|---|---|
| Age at the time of surgery (y) | 56 (13) |
| BMI (Kg/m2) | 25.5 (4.0) |
| Patients underwent 1-level circumferential arthrodesis | 29 |
| L2-L3 | 1 |
| L3-L4 | 2 |
| L4-L5 | 8 |
| L5-S1 | 18 |
| Patients underwent 2-level circumferential arthrodesis | 26 |
| L3-L5 | 5 |
| L4-S1 | 21 |
| Patients underwent 3-level circumferential arthrodesis | 16 |
| L2-L5 | 4 |
| L3-S1 | 12 |
| Preoperative | Postoperative | p-Value (Preoperative vs. Immediate Postop) | p-Value (Immediate Postop vs. 1 Year FU vs. 2 Years FU) | |||
|---|---|---|---|---|---|---|
| Immediate Postoperative | 1 Year FU | 2 Years FU | ||||
| Segmental lordosis (°) | 9.0 ± 3.6 | 15.3 ± 3.0 | 15.5 ± 3.0 | 15.4 ± 3.0 | p < 0.001 | p = 0.355 |
| Lumbar lordosis (°) | 41.9 ± 10.5 | 45.7 ± 10.8 | 42.3 ± 11.4 | 41.7 ± 11.6 | p = 0.01 | p = 0.041 |
| Anterior Disc Height (mm) | 5.8 ± 0.5 | 11.3 ± 0.9 | 10.5 ± 1.0 | 9.9 ± 1.0 | p < 0.001 | p < 0.001 |
| Posterior Disc Height (mm) | 3.4 ± 0.6 | 9.3 ± 0.9 | 8.6 ± 0.9 | 8.0 ± 0.9 | p < 0.001 | p < 0.001 |
| Foraminal Height (cm) | 1.0 ± 0.1 | 2.3 ± 0.2 | 2.1 ± 0.2 | 2.0 ± 0.2 | p < 0.001 | p < 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marco, F.; Francesco, V.; Angelo, T.; Giovanni, C.; Antonio, P.; Elena, M.; Giuliana, N.; Bruna, M.; Alessandro, G. Expandable Interbody Cages in 1–3 Level Circumferential Lumbar Arthrodesis with 2-Year Follow up: A Retrospective Study. Bioengineering 2025, 12, 1169. https://doi.org/10.3390/bioengineering12111169
Marco F, Francesco V, Angelo T, Giovanni C, Antonio P, Elena M, Giuliana N, Bruna M, Alessandro G. Expandable Interbody Cages in 1–3 Level Circumferential Lumbar Arthrodesis with 2-Year Follow up: A Retrospective Study. Bioengineering. 2025; 12(11):1169. https://doi.org/10.3390/bioengineering12111169
Chicago/Turabian StyleMarco, Fava, Vommaro Francesco, Toscano Angelo, Ciani Giovanni, Parciante Antonio, Mendola Elena, Nervuti Giuliana, Maccaferri Bruna, and Gasbarrini Alessandro. 2025. "Expandable Interbody Cages in 1–3 Level Circumferential Lumbar Arthrodesis with 2-Year Follow up: A Retrospective Study" Bioengineering 12, no. 11: 1169. https://doi.org/10.3390/bioengineering12111169
APA StyleMarco, F., Francesco, V., Angelo, T., Giovanni, C., Antonio, P., Elena, M., Giuliana, N., Bruna, M., & Alessandro, G. (2025). Expandable Interbody Cages in 1–3 Level Circumferential Lumbar Arthrodesis with 2-Year Follow up: A Retrospective Study. Bioengineering, 12(11), 1169. https://doi.org/10.3390/bioengineering12111169








