A Biomechanical Comparison Study of Plate–Nail and Dual-Plate Fixation in AO/OTA 41-C2 Tibial Plateau Fractures
Abstract
1. Introduction
2. Methods
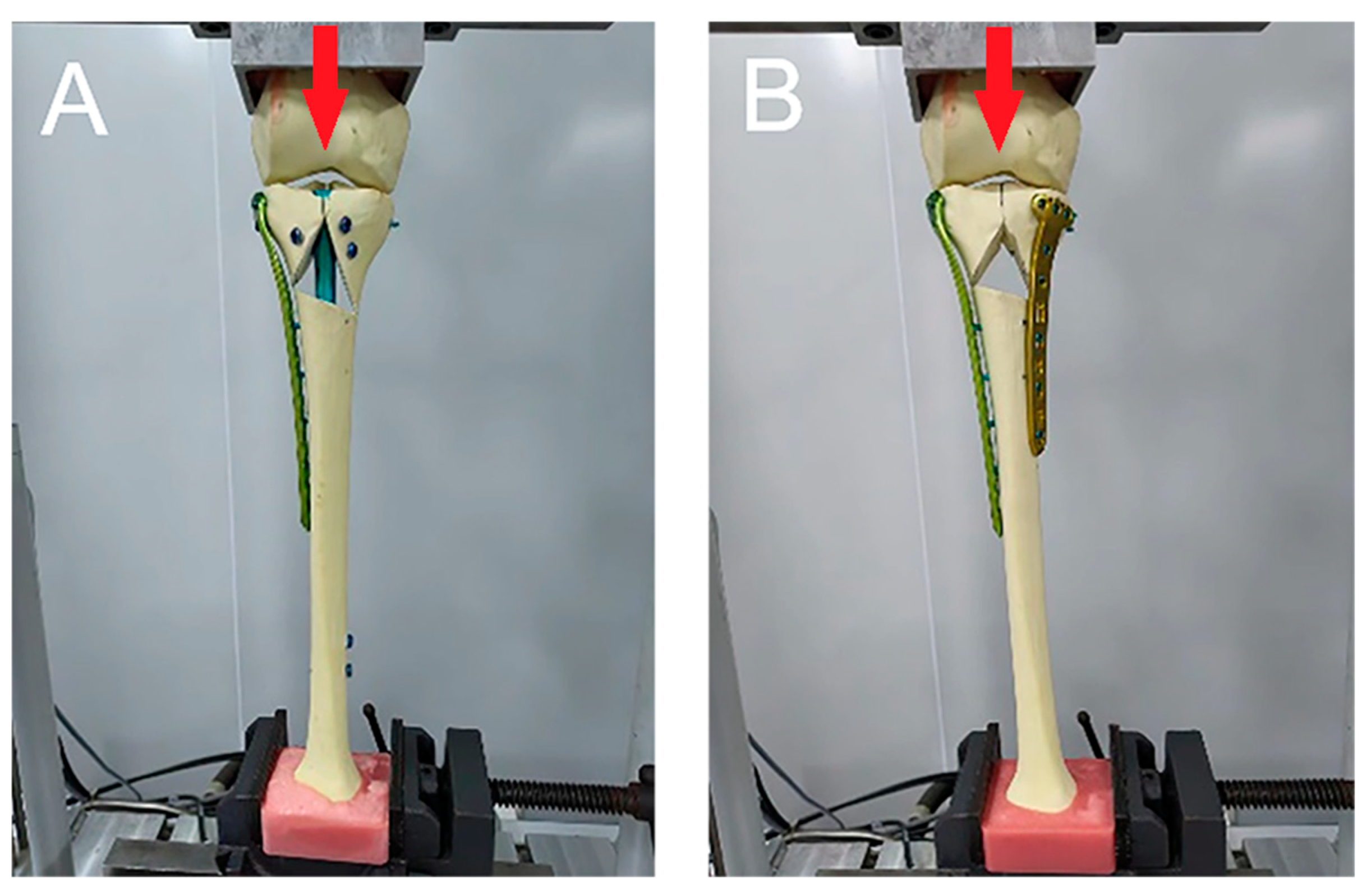
2.1. Materials and Methods
2.2. Biomechanical Testing
2.3. Statistical Analysis
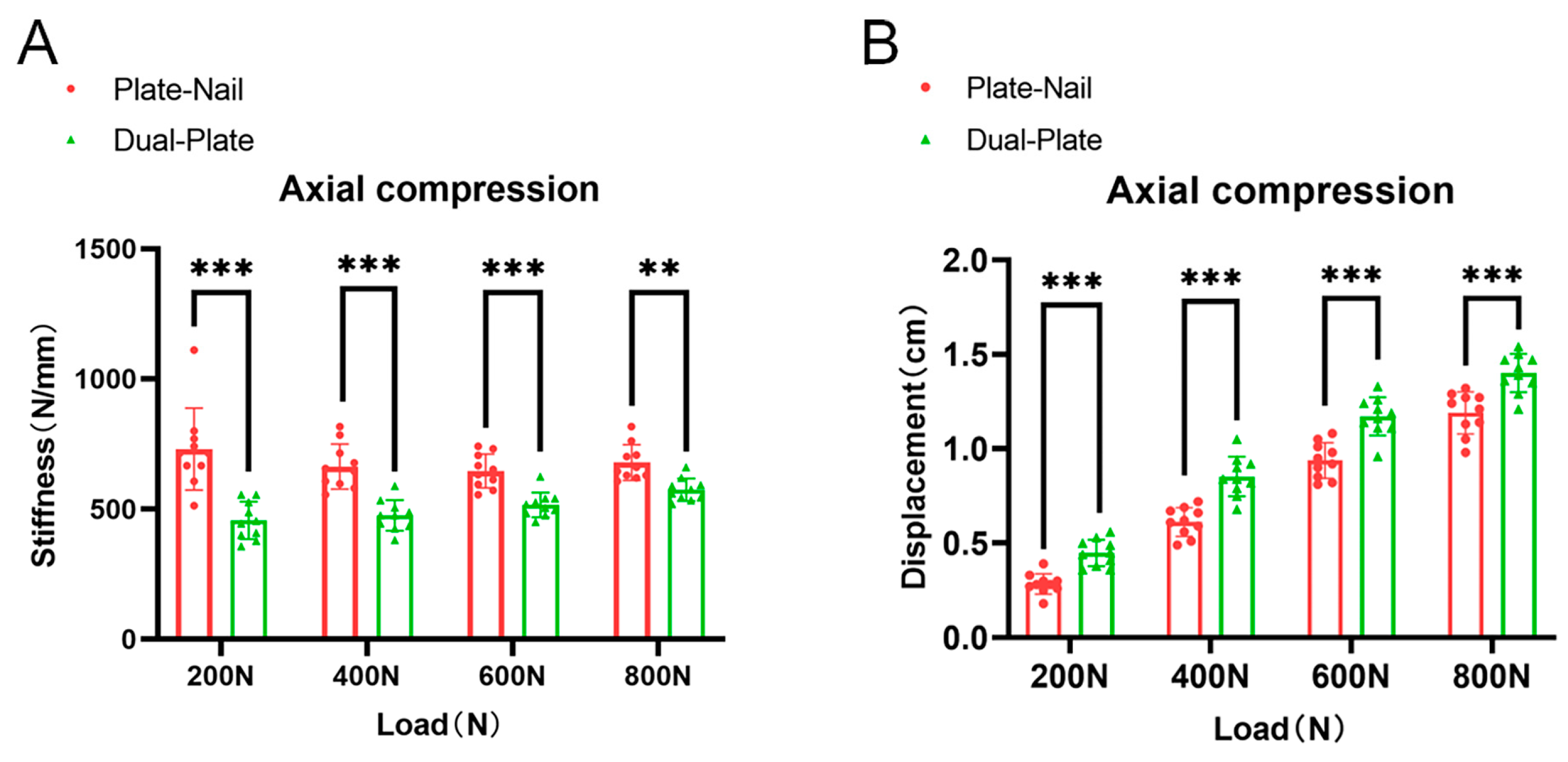
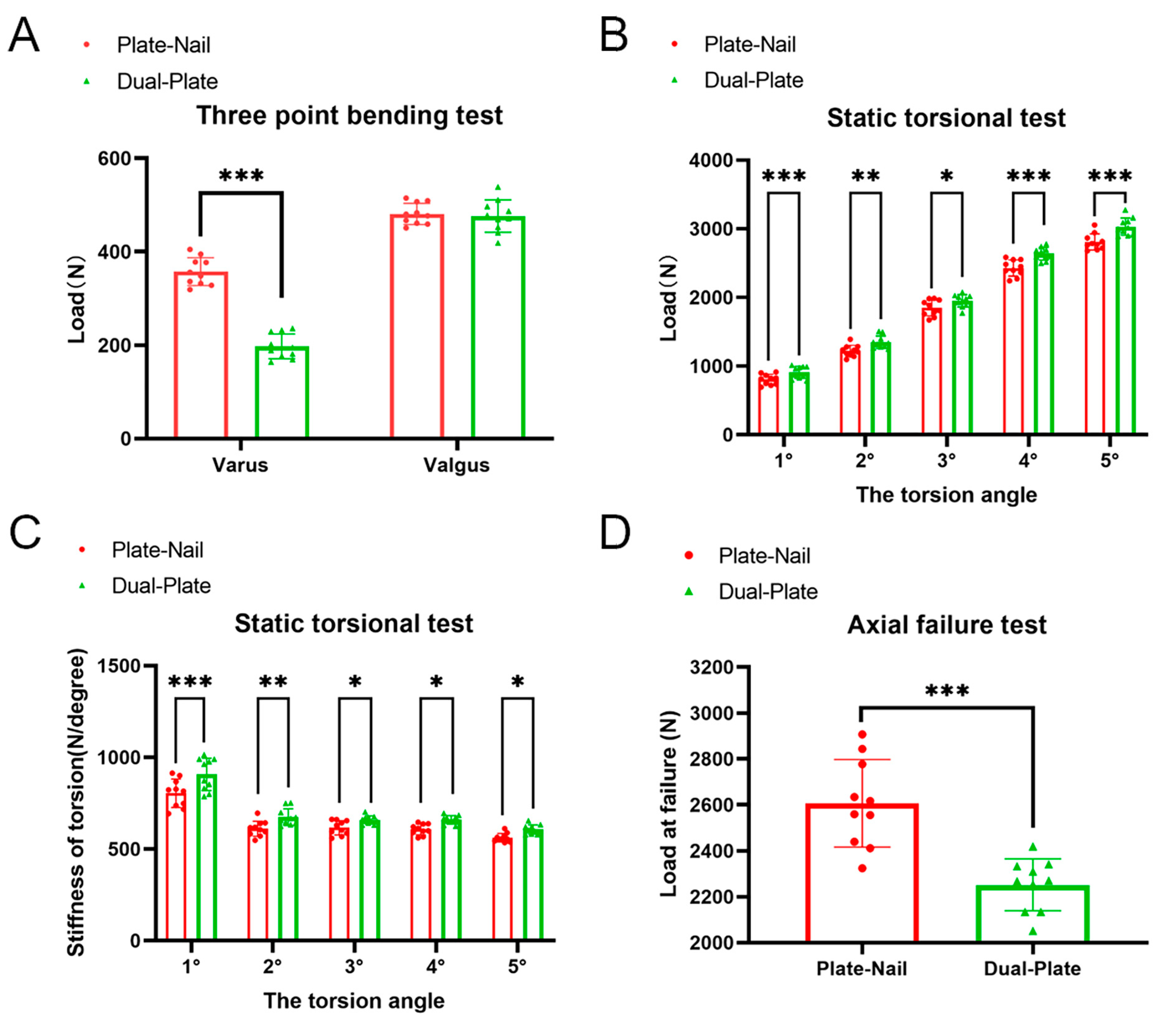
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tuncez, M.; Akan, I.; Seyfettinoğlu, F.; Çetin Tunçez, H.; Dirim Mete, B.; Kazımoğlu, C. Is It Necessary to Add Soft Tissue Injury to the Classification in Tibial Plateau Fracture Management? Cureus 2022, 14, e22236. [Google Scholar] [CrossRef]
- Reátiga Aguilar, J.; Gonzalez Edery, E.; Guzmán Badrán, J.; Molina Gandara, J.; Arzuza Ortega, L.; Ríos Garrido, X.; Medina Monje, C. Open tibial plateau fractures: Infection rate and functional outcomes. Injury 2023, 54 (Suppl. S6), 110720. [Google Scholar] [CrossRef]
- Wang, H.; Liu, Y.; Shi, Z.; Wang, D.; Zhang, H.; Diao, S.; Xu, X.; Waheed, M.Z.; Lu, T.; Zhou, J. Intrawound application of vancomycin reduces the proportion of fracture-related infections in high-risk tibial plateau fractures. Injury 2023, 54, 1088–1094. [Google Scholar] [CrossRef]
- Schneiderman, B.A.; O’Toole, R.V. Compartment Syndrome in High-Energy Tibial Plateau Fractures. Orthop. Clin. 2022, 53, 43–50. [Google Scholar] [CrossRef]
- Grisdela, P., Jr.; Olson, J.; Guild, T.; Dekhne, M.; Hresko, A.; Singh, U.M.; Weaver, M.J.; von Keudell, A.; Stenquist, D. Complications and timing of soft tissue coverage after complete articular, open tibial plateau fractures. Injury 2023, 54, 722–727. [Google Scholar] [CrossRef]
- Adams, J.D.J., Jr.; Loeffler, M.F. Soft Tissue Injury Considerations in the Treatment of Tibial Plateau Fractures. Orthop. Clin. North Am. 2020, 51, 471–479. [Google Scholar] [CrossRef]
- Ozkaya, U.; Parmaksizoglu, A.S. Dual locked plating of unstable bicondylar tibial plateau fractures. Injury 2015, 46 (Suppl. S2), S9–S13. [Google Scholar] [CrossRef]
- Weaver, M.J.; Harris, M.B.; Strom, A.C.; Smith, R.M.; Lhowe, D.; Zurakowski, D.; Vrahas, M.S. Fracture pattern and fixation type related to loss of reduction in bicondylar tibial plateau fractures. Injury 2012, 43, 864–869. [Google Scholar] [CrossRef]
- Barei, D.P.; Nork, S.E.; Mills, W.J.; Coles, C.P.; Henley, M.B.; Benirschke, S.K. Functional outcomes of severe bicondylar tibial plateau fractures treated with dual incisions and medial and lateral plates. J. Bone Joint Surg. Am. 2006, 88, 1713–1721. [Google Scholar] [CrossRef]
- Olszewski, N.; Manzano, G.; Wilson, E.; Joseph, N.; Vallier, H.; Pawlak, A.; Kottmeier, S.; Miller, A.; Gary, J.; Namm, J.; et al. Bicondylar Tibial Plateau Fractures: What Predicts Infection? J. Am. Acad. Orthop. Surg. 2022, 30, e1311–e1318. [Google Scholar] [CrossRef]
- Morris, B.J.; Unger, R.Z.; Archer, K.R.; Mathis, S.L.; Perdue, A.M.; Obremskey, W.T. Risk factors of infection after ORIF of bicondylar tibial plateau fractures. J. Orthop. Trauma 2013, 27, e196–e200. [Google Scholar] [CrossRef]
- Lasanianos, N.G.; Garnavos, C.; Magnisalis, E.; Kourkoulis, S.; Babis, G.C. A comparative biomechanical study for complex tibial plateau fractures: Nailing and compression bolts versus modern and traditional plating. Injury 2013, 44, 1333–1339. [Google Scholar] [CrossRef]
- Lee, T.C.; Huang, H.T.; Lin, Y.C.; Chen, C.H.; Cheng, Y.M.; Chen, J.C. Bicondylar tibial plateau fracture treated by open reduction and fixation with unilateral locked plating. Kaohsiung J. Med. Sci. 2013, 29, 568–577. [Google Scholar] [CrossRef]
- Thamyongkit, S.; Abbasi, P.; Parks, B.G.; Shafiq, B.; Hasenboehler, E.A. Weightbearing after combined medial and lateral plate fixation of AO/OTA 41-C2 bicondylar tibial plateau fractures: A biomechanical study. BMC Musculoskelet Disord. 2022, 23, 86. [Google Scholar] [CrossRef]
- Wright, D.J.; Etiz, B.; Scolaro, J.A. Combined plate and nail fixation of bicondylar tibial plateau fractures. Injury 2021, 52, 3104–3110. [Google Scholar] [CrossRef] [PubMed]
- Högel, F.; Hoffmann, S.; Panzer, S.; Wimber, J.; Bühren, V.; Augat, P. Biomechanical comparison of intramedullar versus extramedullar stabilization of intra-articular tibial plateau fractures. Arch. Orthop. Trauma Surg. 2013, 133, 59–64. [Google Scholar] [CrossRef]
- Chapman, J.P.; Patrick, M.R.; Reb, C.W.; Hao, K.A.; Vincent, H.K.; Hagen, J.E. Comparable outcomes with intramedullary nail and plate constructs for Schatzker VI tibial plateau fractures. Eur. J. Orthop. Surg. Traumatol. 2023, 33, 1653–1661. [Google Scholar] [CrossRef]
- Gao, W.; Zhao, K.; Guo, Y.; Xie, M.; Feng, X.; Liu, P.; Xie, X.; Fu, D. Biomechanical comparison of intramedullary nail and plate osteosynthesis for extra-articular proximal tibial fractures with segmental bone defect. Front. Bioeng. Biotechnol. 2023, 11, 1099241. [Google Scholar] [CrossRef]
- Momaya, A.M.; Hlavacek, J.; Etier, B.; Johannesmeyer, D.; Oladeji, L.O.; Niemeier, T.E.; Herrera, N.; Lowe, J.A. Risk factors for infection after operative fixation of Tibial plateau fractures. Injury 2016, 47, 1501–1505. [Google Scholar] [CrossRef]
- DeKeyser, G.; Bunzel, E.; O’Neill, D.; Nork, S.; Haller, J.; Barei, D. Single-Incision Fasciotomy Decreases Infection Risk Compared with Dual-Incision Fasciotomy in Treatment of Tibial Plateau Fractures With Acute Compartment Syndrome. J. Orthop. Trauma 2023, 37, 519–524. [Google Scholar] [CrossRef]
- Molenaars, R.J.; Mellema, J.J.; Doornberg, J.N.; Kloen, P. Tibial Plateau Fracture Characteristics: Computed Tomography Mapping of Lateral, Medial, and Bicondylar Fractures. J. Bone Joint Surg. Am. 2015, 97, 1512–1520. [Google Scholar] [CrossRef]
- Xie, X.; Zhan, Y.; Wang, Y.; Lucas, J.F.; Zhang, Y.; Luo, C. Comparative Analysis of Mechanism-Associated 3-Dimensional Tibial Plateau Fracture Patterns. J. Bone Joint Surg. Am. 2020, 102, 410–418. [Google Scholar] [CrossRef]
- Weigel, D.P.; Marsh, J.L. High-energy fractures of the tibial plateau. Knee function after longer follow-up. J. Bone Joint Surg. Am. 2002, 84, 1541–1551. [Google Scholar] [CrossRef]
- Kim, Y.J.; Scott, T.; Richard, R.D.; Parry, J.A. An Acute Fixation Protocol for High-Energy Tibial Plateau Fractures Decreases Time to Fixation and Lowers Operative Costs Without Affecting Wound Complications and Reoperations. J. Orthop. Trauma 2023, 37, 287–293. [Google Scholar] [CrossRef]
- Guo, J.; Gao, Z.; Wang, L.; Feng, C.; Hou, Z.; Zhang, Y. The blister occurring in severe tibial plateau fractures (Schatzker V–VI) decreases the risk of acute compartment syndrome. Int. Orthop. 2021, 45, 743–749. [Google Scholar] [CrossRef]
- Zhao, X.-W.; Ma, J.-X.; Ma, X.-L.; Jiang, X.; Wang, Y.; Li, F.; Lu, B. A meta-analysis of external fixation versus open reduction and internal fixation for complex tibial plateau fractures. Int. J. Surg. 2017, 39, 65–73. [Google Scholar] [CrossRef]
- Zhao, W.-Q.; Li, X.-S.; Hua, J.; Huang, J.-F. Reverse traction with Kirschner wires and bilateral external fixation device combined with minimally invasive plate oseoynthesis technique for tibial plateau fractures of type Schatzker V and VI. Int. Orthop. 2023, 47, 2327–2336. [Google Scholar] [CrossRef]
- Gupta, S.; Yapp, L.Z.; Sadczuk, D.; MacDonald, D.J.; Clement, N.D.; White, T.O.; Keating, J.F.; Scott, C.E.H. Tibial plateau fractures in older adults are associated with a clinically significant deterioration in health-related quality of life. Bone Jt. Open 2023, 4, 273–282. [Google Scholar] [CrossRef]
- Egol, K.A.; Tejwani, N.C.; Capla, E.L.; Wolinsky, P.L.; Koval, K.J. Staged management of high-energy proximal tibia fractures (OTA types 41): The results of a prospective, standardized protocol. J. Orthop. Trauma 2005, 19, 448–456. [Google Scholar] [CrossRef]
- Shao, J.; Chang, H.; Zhu, Y.; Chen, W.; Zheng, Z.; Zhang, H.; Zhang, Y. Incidence and risk factors for surgical site infection after open reduction and internal fixation of tibial plateau fracture: A systematic review and meta-analysis. Int. J. Surg. 2017, 41, 176–182. [Google Scholar] [CrossRef]
- Kumar, V.; Singhroha, M.; Arora, K.; Sahu, A.; Beniwal, R.; Kundu, A. A clinico-radiological study of bicondylar tibial plateau fractures managed with dual locking plates. J. Clin. Orthop. Trauma 2021, 21, 101563. [Google Scholar] [CrossRef]
- Yao, Y.; Lv, H.; Zan, J.; Li, J.; Zhu, N.; Jing, J. Functional outcomes of bicondylar tibial plateau fractures treated with dual buttress plates and risk factors: A case series. Injury 2014, 45, 1980–1984. [Google Scholar] [CrossRef]
- Jia, P.; Lu, F.C.; Ullah, K.; Zhang, M.; Dong, Y.S.; Xiong, C.; Zhao, Z.H.; Wang, J.F.; Chen, J.W.; Wang, Y.Q. Angle Stable Interlocking Intramedullary Nails for Tibial Plateau Fractures. Orthop. Surg. 2018, 10, 115–120. [Google Scholar] [CrossRef]
- Yoon, R.S.; Bible, J.; Marcus, M.S.; Donegan, D.J.; Bergmann, K.A.; Siebler, J.C.; Mir, H.R.; Liporace, F.A. Outcomes following combined intramedullary nail and plate fixation for complex tibia fractures: A multi-centre study. Injury 2015, 46, 1097–1101. [Google Scholar] [CrossRef]
- Yocum, D.S.; Valenzuela, K.A.; Standifird, T.W.; Cates, H.E.; Zhang, S. Altered biomechanics in bilateral total knee replacement patients during stair negotiation. Knee 2022, 34, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Warmerdam, E.; Orth, M.; Pohlemann, T.; Ganse, B. Gait Analysis to Monitor Fracture Healing of the Lower Leg. Bioengineering 2023, 10, 255. [Google Scholar] [CrossRef]
- Saul, D.; Menger, M.M.; Ehnert, S.; Nüssler, A.K.; Histing, T.; Laschke, M.W. Bone Healing Gone Wrong: Pathological Fracture Healing and Non-Unions-Overview of Basic and Clinical Aspects and Systematic Review of Risk Factors. Bioengineering 2023, 10, 85. [Google Scholar] [CrossRef]
- Tian, Y.; Zhang, L.; Zhang, C.; Bao, B.; Li, Q.; Wang, L.; Song, Z.; Li, D. Deep-learning enabled smart insole system aiming for multifunctional foot-healthcare applications. Exploration 2024, 4, 20230109. [Google Scholar] [CrossRef]
- McDevitt, S.; Hernandez, H.; Hicks, J.; Lowell, R.; Bentahaikt, H.; Burch, R.; Ball, J.; Chander, H.; Freeman, C.; Taylor, C.; et al. Wearables for Biomechanical Performance Optimization and Risk Assessment in Industrial and Sports Applications. Bioengineering 2022, 9, 33. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xie, W.; Luo, D.; Xie, L.; Zhu, L.; Zhou, L.; Lian, K.; Lin, D.; Liu, H. A Biomechanical Comparison Study of Plate–Nail and Dual-Plate Fixation in AO/OTA 41-C2 Tibial Plateau Fractures. Bioengineering 2024, 11, 839. https://doi.org/10.3390/bioengineering11080839
Xie W, Luo D, Xie L, Zhu L, Zhou L, Lian K, Lin D, Liu H. A Biomechanical Comparison Study of Plate–Nail and Dual-Plate Fixation in AO/OTA 41-C2 Tibial Plateau Fractures. Bioengineering. 2024; 11(8):839. https://doi.org/10.3390/bioengineering11080839
Chicago/Turabian StyleXie, Wei, Deqing Luo, Li Xie, Lingqi Zhu, Liang Zhou, Kejian Lian, Dasheng Lin, and Hui Liu. 2024. "A Biomechanical Comparison Study of Plate–Nail and Dual-Plate Fixation in AO/OTA 41-C2 Tibial Plateau Fractures" Bioengineering 11, no. 8: 839. https://doi.org/10.3390/bioengineering11080839
APA StyleXie, W., Luo, D., Xie, L., Zhu, L., Zhou, L., Lian, K., Lin, D., & Liu, H. (2024). A Biomechanical Comparison Study of Plate–Nail and Dual-Plate Fixation in AO/OTA 41-C2 Tibial Plateau Fractures. Bioengineering, 11(8), 839. https://doi.org/10.3390/bioengineering11080839







