Primary Stability of Kyphoplasty in Incomplete Vertebral Body Burst Fractures in Osteoporosis: A Biomechanical Investigation
Abstract
1. Introduction
2. Materials and Methods
2.1. Specimens
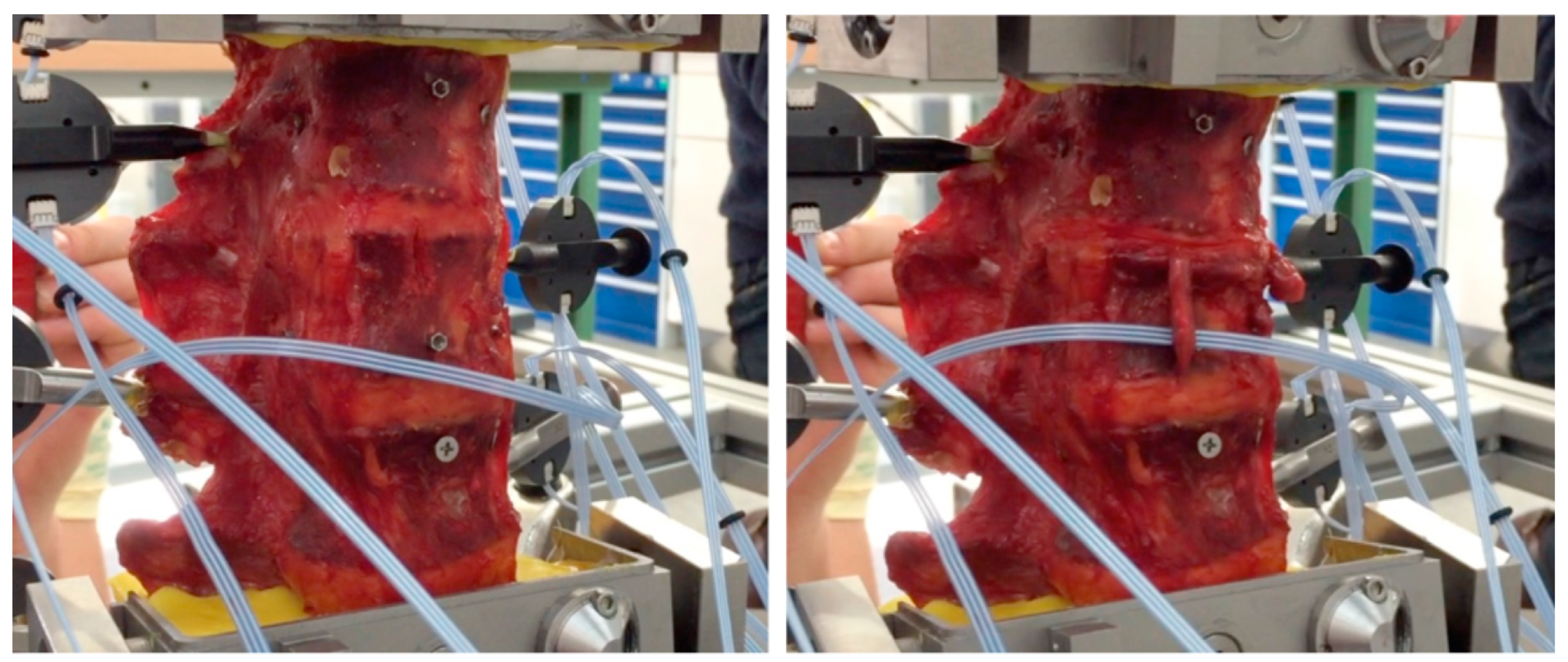
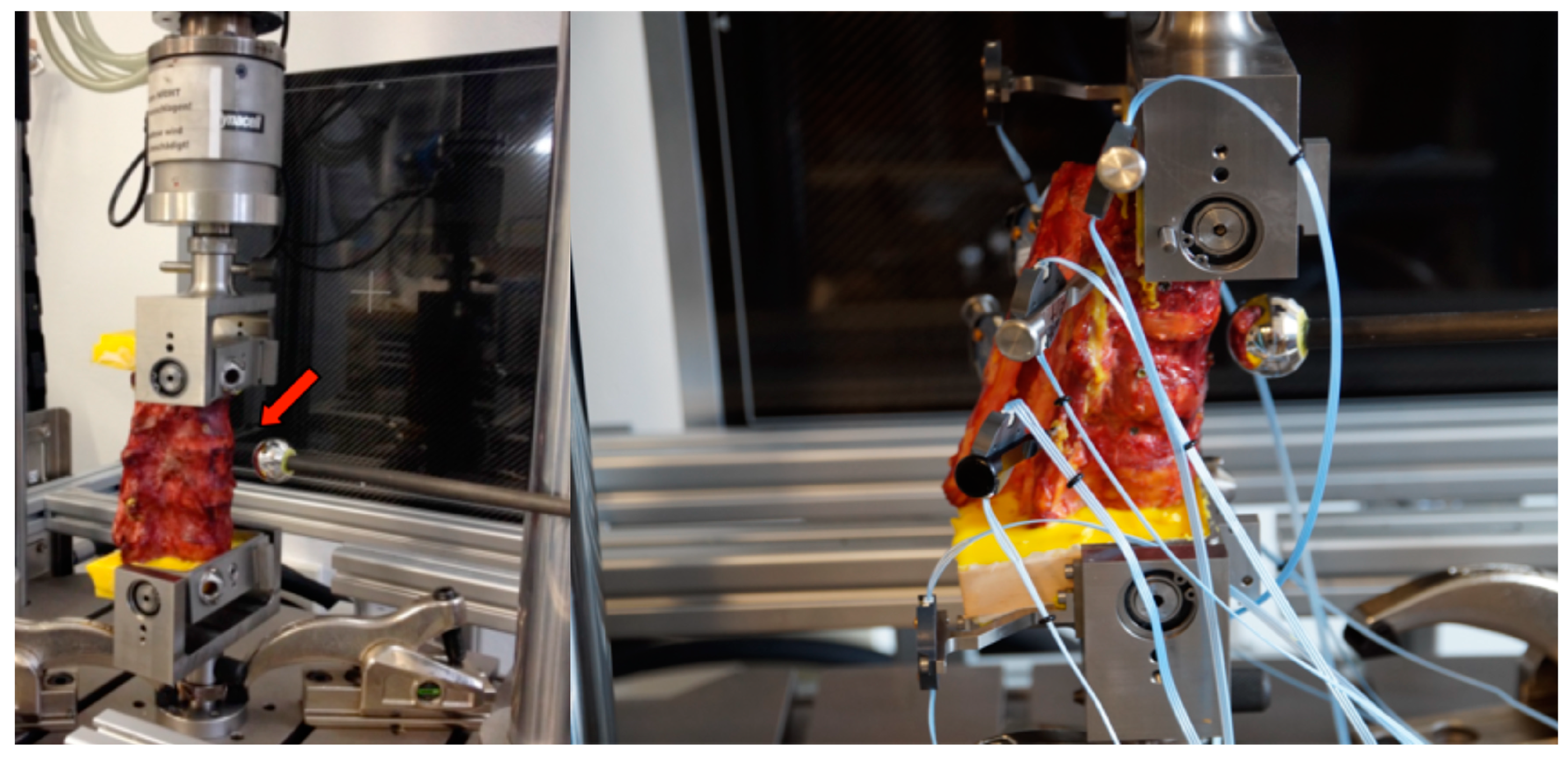
2.2. Fracture Creation
2.3. Kyphoplasty
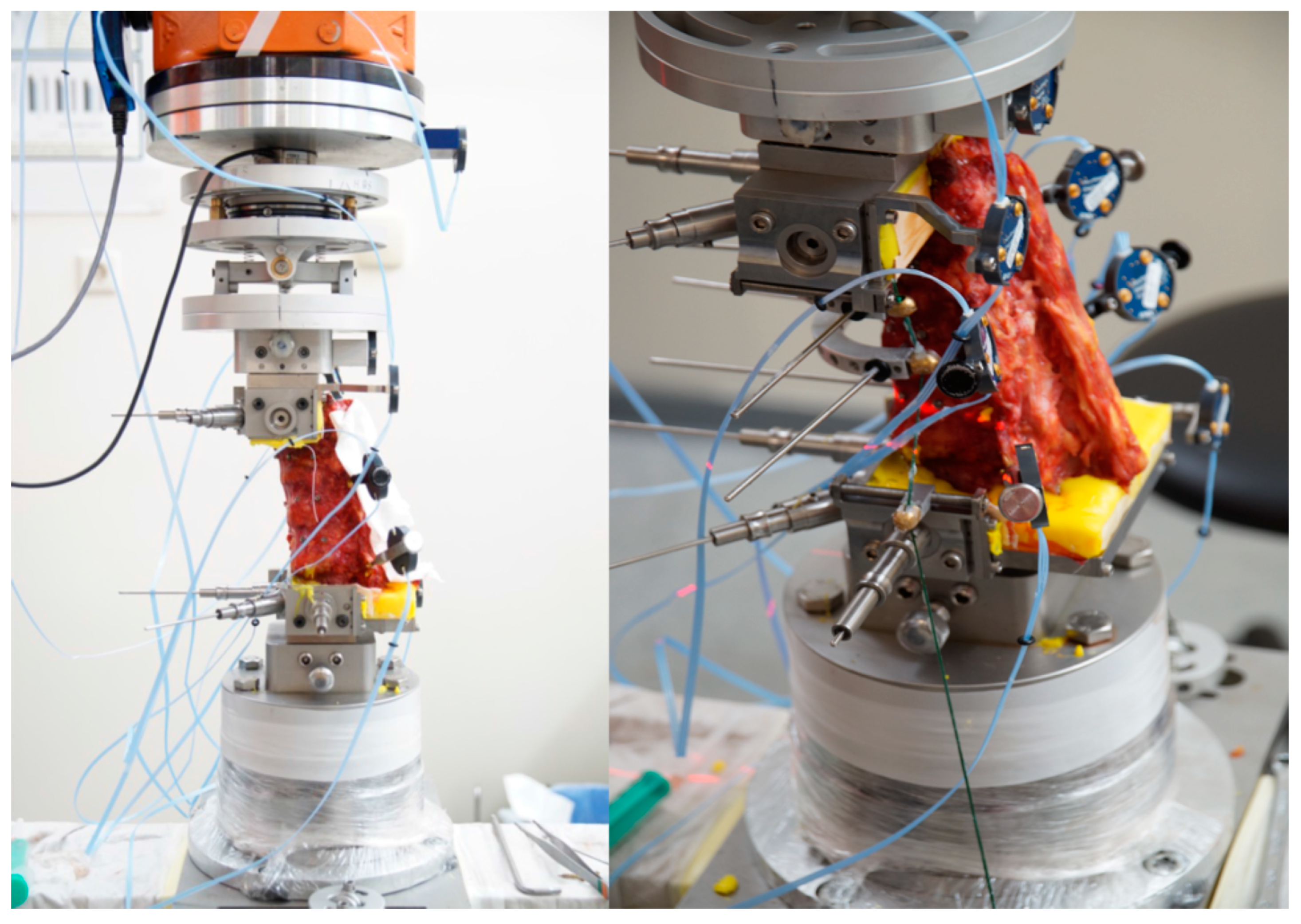
2.4. Kinematic Testing
2.5. Radiological Assessment
2.6. Groups
2.7. Statistics
3. Results
3.1. Fracture Creation and Vertebral Body Reconstruction
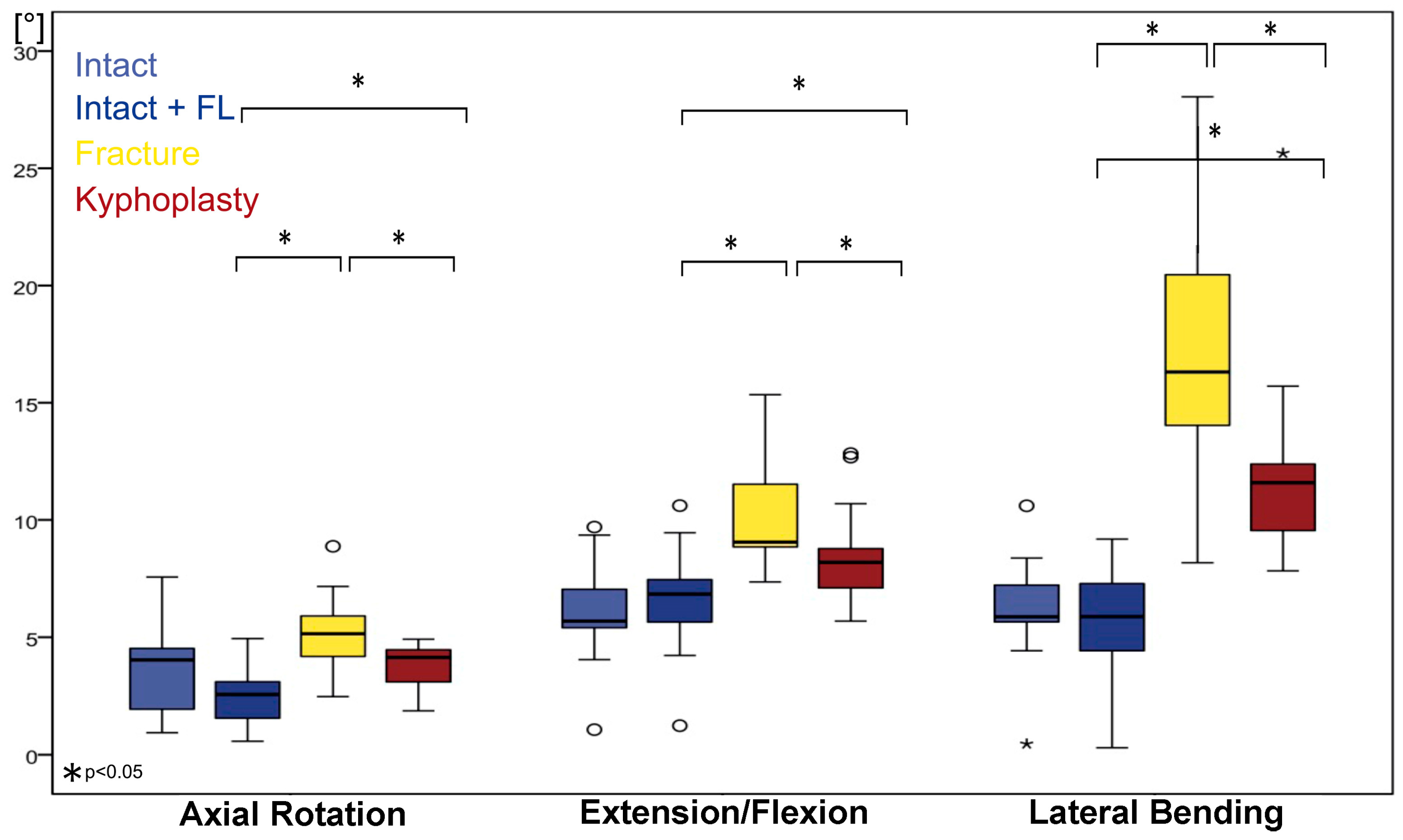
3.2. Kinematics of the Injured Segment (Th12–L1)
3.3. Extension–Flexion
3.4. Axial Rotation
3.5. Lateral Flexion
3.6. Kinematics of L1–L2
3.7. Adjacent Segments
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Garfin, S.R.; Yuan, H.A.; Reiley, M.A. New technologies in spine: Kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine 2001, 26, 1511–1515. [Google Scholar] [CrossRef]
- Zhao, G.; Liu, X.; Li, F. Balloon kyphoplasty versus percutaneous vertebroplasty for treatment of osteoporotic vertebral compression fractures (OVCFs). Osteoporos. Int. 2016, 27, 2823–2834. [Google Scholar] [CrossRef]
- Ortiz, A.O.; Zoarski, G.H.; Beckerman, M. Kyphoplasty. Tech. Vasc. Interv. Radiol. 2002, 5, 239–249. [Google Scholar] [CrossRef]
- Hoffmann, J.; Preston, G.; Whaley, J.; Khalil, J.G. Vertebral Augmentation in Spine Surgery. J. Am. Acad. Orthop. Surg. 2023, 31, 477–489. [Google Scholar] [CrossRef]
- Li, C.-H.; Chang, M.-C.; Liu, C.-L.; Chen, T.-S. Osteoporotic burst fracture with spinal canal compromise treated with percutaneous vertebroplasty. Clin. Neurol. Neurosurg. 2010, 112, 678–681. [Google Scholar] [CrossRef]
- Yao, R.; Yin, P.; Zhang, Y.; Li, D.; Zhang, X.-N.; Tao, L.; Zhou, J.; Su, Q. Is there a risk of further displacement of the fractured fragment into the spinal canal in osteoporotic vertebral burst fractures after unilateral PKP? A prospective study. Spine J. 2023, 24, 1077–1086. [Google Scholar] [CrossRef]
- Chen, Y.; Yin, P.; Hai, Y.; Su, Q.; Yang, J. Is Osteoporotic Thoracolumbar Burst Fracture a Contraindication to Percutaneous Kyphoplasty? A Systematic Review. Pain Physician 2021, 24, E685–E692. [Google Scholar]
- Oh, T.; Scheer, J.K.; Fakurnejad, S.; Dahdaleh, N.S.; Smith, Z.A. Minimally invasive spinal surgery for the treatment of traumatic thoracolumbar burst fractures. J. Clin. Neurosci. 2015, 22, 42–47. [Google Scholar] [CrossRef]
- Wilke, H.-J.; Mehnert, U.; Claes, L.E.; Bierschneider, M.M.; Jaksche, H.; Boszczyk, B.M. Biomechanical evaluation of vertebroplasty and kyphoplasty with polymethyl methacrylate or calcium phosphate cement under cyclic loading. Spine 2006, 31, 2934–2941. [Google Scholar] [CrossRef] [PubMed]
- Hartensuer, R.; Gehweiler, D.; Schulze, M.; Matuszewski, L.; Raschke, M.J.; Vordemvenne, T. Biomechanical evaluation of combined short segment fixation and augmentation of incomplete osteoporotic burst fractures. BMC Musculoskelet. Disord. 2013, 14, 360. [Google Scholar] [CrossRef] [PubMed]
- Vaccaro, A.R.; Oner, C.; Kepler, C.K.; Dvorak, M.; Schnake, K.; Bellabarba, C.; Reinhold, M.; Aarabi, B.; Kandziora, F.; Chapman, J.; et al. AOSpine thoracolumbar spine injury classification system: Fracture description, neurological status, and key modifiers. Spine 2013, 38, 2028–2037. [Google Scholar] [CrossRef] [PubMed]
- Disch, A.C.; Schmoelz, W. Cement augmentation in a thoracolumbar fracture model: Reduction and stability after balloon kyphoplasty versus vertebral body stenting. Spine 2014, 39, E1147–E1153. [Google Scholar] [CrossRef] [PubMed]
- Achatz, G.; Riesner, H.-J.; Friemert, B.; Lechner, R.; Graf, N.; Wilke, H.-J. Biomechanical in vitro comparison of radiofrequency kyphoplasty and balloon kyphoplasty. Eur. Spine J. 2017, 26, 3225–3234. [Google Scholar] [CrossRef] [PubMed]
- Holyoak, D.T.; Andreshak, T.G.; Hopkins, T.J.; Brook, A.L.; Frohbergh, M.E.; Ong, K.L. Height restoration and sustainability using bilateral vertebral augmentation systems for vertebral compression fractures: A cadaveric study. Spine J. 2022, 22, 2072–2081. [Google Scholar] [CrossRef] [PubMed]
- Wong, E.K.Y.; Whyne, C.M.; Singh, D.; Ford, M. A Biomechanical Assessment of Kyphoplasty as a Stand-Alone Treatment in a Human Cadaveric Burst Fracture Model. Spine 2015, 40, E808–E813. [Google Scholar] [CrossRef] [PubMed]
- Germaneau, A.; Vendeuvre, T.; Saget, M.; Doumalin, P.; Dupré, J.C.; Brémand, F.; Hesser, F.; Couvertier, M.; Brèque, C.; Maxy, P.; et al. A novel approach for biomechanical spine analysis: Mechanical response of vertebral bone augmentation by kyphoplasty to stabilise thoracolumbar burst fractures. J. Mech. Behav. Biomed. Mater. 2016, 59, 291–303. [Google Scholar] [CrossRef]
- Schnake, K.J.; Blattert, T.R.; Hahn, P.; Franck, A.; Hartmann, F.; Ullrich, B.; Verheyden, A.; Mörk, S.; Zimmermann, V.; Gonschorek, O.; et al. Classification of Osteoporotic Thoracolumbar Spine Fractures: Recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Glob. Spine J. 2018, 8, 46S–49S. [Google Scholar] [CrossRef] [PubMed]
- Schulze, M.; Hartensuer, R.; Gehweiler, D.; Hölscher, U.; Raschke, M.J.; Vordemvenne, T. Evaluation of a robot-assisted testing system for multisegmental spine specimens. J. Biomech. 2012, 45, 1457–1462. [Google Scholar] [CrossRef] [PubMed]
- American College of Radiology. ACR–SPR–SSR Practice Parameter for the Performance of Quantitative Computed Tomography (QCT) Bone Mineral Density. Available online: https://www.acr.org (accessed on 22 July 2024).
- Wilke, H.J.; Wenger, K.; Claes, L. Testing criteria for spinal implants: Recommendations for the standardization of in vitro stability testing of spinal implants. Eur. Spine J. 1998, 7, 148–154. [Google Scholar] [CrossRef]
- Hartensuer, R.; Gasch, A.; Gehweiler, D.; Schanz, S.; Schulze, M.; Matuszewski, L.; Langer, M.; Raschke, M.J.; Vordemvenne, T. Experimentally induced incomplete burst fractures—A novel technique for calf and human specimens. BMC Musculoskelet. Disord. 2012, 13, 45. [Google Scholar] [CrossRef]
- Patwardhan, A.G.; Havey, R.M.; Carandang, G.; Simonds, J.; Voronov, L.I.; Ghanayem, A.J.; Meade, K.P.; Gavin, T.M.; Paxinos, O. Effect of compressive follower preload on the flexion-extension response of the human lumbar spine. J. Orthop. Res. 2003, 21, 540–546. [Google Scholar] [CrossRef] [PubMed]
- Rohlmann, A.; Zander, T.; Rao, M.; Bergmann, G. Applying a follower load delivers realistic results for simulating standing. J. Biomech. 2009, 42, 1520–1526. [Google Scholar] [CrossRef] [PubMed]
- McKiernan, F.; Faciszewski, T.; Jensen, R. Reporting height restoration in vertebral compression fractures. Spine 2003, 28, 2517–2521. [Google Scholar] [CrossRef] [PubMed]
- Oner, F.C.; Verlaan, J.-J.; Verbout, A.J.; Dhert, W.J.A. Cement augmentation techniques in traumatic thoracolumbar spine fractures. Spine 2006, 31, S89–S95, discussion S104. [Google Scholar] [CrossRef] [PubMed]
- Zaryanov, A.V.; Park, D.K.; Khalil, J.G.; Baker, K.C.; Fischgrund, J.S. Cement augmentation in vertebral burst fractures. Neurosurg. Focus 2014, 37, E5. [Google Scholar] [CrossRef] [PubMed]
- Josten, C.; Schmidt, C.; Spiegl, U. Osteoporotische Wirbelkörperfrakturen der thorakolumbalen Wirbelsäule. Diagn. Behandlungsstrategien. Chir. 2012, 83, 866–874. [Google Scholar] [CrossRef] [PubMed]
- Spiegl, U.; Jarvers, J.-S.; Heyde, C.-E.; Josten, C. Osteoporotic vertebral body fractures of the thoracolumbar spine: Indications and techniques of a 360°-stabilization. Eur. J. Trauma Emerg. Surg. 2017, 43, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Evans, J.H. Biomechanics of lumbar fusion. Clin. Orthop. Relat. Res. 1985, 193, 38–46. [Google Scholar] [CrossRef]
- Uchida, K.; Kobayashi, S.; Matsuzaki, M.; Nakajima, H.; Shimada, S.; Yayama, T.; Sato, R.; Baba, H. Anterior versus posterior surgery for osteoporotic vertebral collapse with neurological deficit in the thoracolumbar spine. Eur. Spine J. 2006, 15, 1759–1767. [Google Scholar] [CrossRef]
- Marco, R.A.W.; Kushwaha, V.P. Thoracolumbar burst fractures treated with posterior decompression and pedicle screw instrumentation supplemented with balloon-assisted vertebroplasty and calcium phosphate reconstruction. J. Bone Jt. Surg. Am. 2009, 91, 20–28. [Google Scholar] [CrossRef]
- Shin, J.J.; Chin, D.K.; Yoon, Y.S. Percutaneous vertebroplasty for the treatment of osteoporotic burst fractures. Acta Neurochir. 2009, 151, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Hartmann, F.; Gercek, E.; Leiner, L.; Rommens, P.M. Kyphoplasty as an alternative treatment of traumatic thoracolumbar burst fractures Magerl type A3. Injury 2012, 43, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Ullrich, B.W.; Schenk, P.; Scheyerer, M.J.; Bäumlein, M.; Katscher, S.; Schnake, K.J.; Zimmermann, V.; Schwarz, F.; Schmeiser, G.; Scherer, M.; et al. Georg Schmorl prize of the German spine society (DWG) 2022: Current treatment for inpatients with osteoporotic thoracolumbar fractures-results of the EOFTT study. Eur. Spine J. 2023, 32, 1525–1535. [Google Scholar] [CrossRef] [PubMed]
- Blattert, T.R.; Schnake, K.J.; Gonschorek, O.; Gercek, E.; Hartmann, F.; Katscher, S.; Mörk, S.; Morrison, R.; Müller, M.; Partenheimer, A.; et al. Nonsurgical and Surgical Management of Osteoporotic Vertebral Body Fractures: Recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Glob. Spine J. 2018, 8, 50S–55S. [Google Scholar] [CrossRef] [PubMed]
- Wilke, H.J.; Wolf, S.; Claes, L.E.; Arand, M.; Wiesend, A. Stability increase of the lumbar spine with different muscle groups. A biomechanical in vitro study. Spine 1995, 20, 192–198. [Google Scholar] [CrossRef] [PubMed]
- van Dieën, J.H.; Cholewicki, J.; Radebold, A. Trunk muscle recruitment patterns in patients with low back pain enhance the stability of the lumbar spine. Spine 2003, 28, 834–841. [Google Scholar] [CrossRef] [PubMed]
- Adida, S.; Taori, S.; Wong, V.R.; Tang, A.; Sefcik, R.K.; Zhang, X.; Gerszten, P.C. Analysis of injected cement volume and clinical outcomes following balloon-assisted kyphoplasty in a series of 368 patients. Clin. Neurol. Neurosurg. 2024, 243, 108367. [Google Scholar] [CrossRef]
- Sun, N.; Zhang, Y.; Xie, D.; Chen, Y.; Liu, Y. Enhancing percutaneous kyphoplasty efficacy in elderly osteoporotic fractures through optimal cement filling ratio. Front. Endocrinol. 2024, 15, 1359550. [Google Scholar] [CrossRef]




| Specimen | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | Median | Q1 | Q3 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Native | ||||||||||||||||
| Anterior (CD) | 22.5 | 26.4 | 27.5 | 25.8 | 20.7 | 25.1 | 27 | 26.1 | 24.3 | 27.8 | 26.8 | 28.4 | 22.1 | 26.1 | 23.4 | 27.3 |
| Middle (EF) | 21.8 | 26.3 | 25.3 | 27 | 24.4 | 25.7 | 26.3 | 24.8 | 26.5 | 26.3 | 27.2 | 25.9 | 24.3 | 25.9 | 24.6 | 26.4 |
| Posterior two-thirds (GH) | 23 | 27 | 25.6 | 27.4 | 24.9 | 26.5 | 27.4 | 24.2 | 27.2 | 27.1 | 27.2 | 26.9 | 24.9 | 26.9 | 24.9 | 27.2 |
| Posterior (AB) | 28.8 | 28.8 | 28.3 | 28.3 | 23.8 | 28.6 | 29 | 27.9 | 28.1 | 28.4 | 29.1 | 30.3 | 26.9 | 28.4 | 28 | 28.9 |
| Fractured | ||||||||||||||||
| Anterior (CD) | 18.8 | 16.5 | 27 | 21.9 | 21.2 | 19.8 | 18.3 | 19.1 | 18.7 | 16.9 | 19.9 | 19.6 | 20 | 19.6 | 18.5 | 20.6 |
| Middle (EF) | 18.3 | 17.3 | 22.4 | 22 | 17.6 | 21.5 | 18.5 | 18.6 | 21 | 19.1 | 20.9 | 19.9 | 20.6 | 19.9 | 18.4 | 21.3 |
| Posterior two-thirds (GH) | 19.9 | 19 | 22.9 | 22.1 | 19.3 | 22.4 | 20 | 18.5 | 21.9 | 20.6 | 21.2 | 22 | 22.3 | 21.2 | 19.6 | 22.2 |
| Posterior (AB) | 27.1 | 26.1 | 26 | 24.9 | 24.5 | 26.6 | 23.9 | 23.2 | 27.2 | 24.8 | 27.1 | 28.3 | 26.5 | 26.1 | 24.7 | 27.1 |
| Reconstructed | ||||||||||||||||
| Anterior (CD) | 22.5 | 19.2 | 26.8 | 23.2 | 21.9 | 21 | 23.5 | 22.5 | 20.4 | 22.6 | 26 | 25.7 | 22 | 22.5 | 21.5 | 24.6 |
| Middle (EF) | 21 | 19.7 | 23.2 | 24.4 | 20.9 | 22.8 | 19.7 | 21.1 | 21.9 | 23.2 | 23.5 | 23.8 | 23.5 | 22.8 | 21.0 | 23.5 |
| Posterior two-thirds (GH) | 23.1 | 21.2 | 23.3 | 24.3 | 21.9 | 23.5 | 20.5 | 20.7 | 22.3 | 23.2 | 23.4 | 25.1 | 23.5 | 23.2 | 21.6 | 23.5 |
| Posterior (AB) | 28.6 | 26 | 27.2 | 27.6 | 24.8 | 27.2 | 24.7 | 25.3 | 27.1 | 26.8 | 27.5 | 28.9 | 27.4 | 27.2 | 25.7 | 27.6 |
| Group 1: Intact without Follower Load | Group 2: Intact with Follower Load | Group 3: Fracture with Follower Load | Group 4: Kyphoplasty with Follower Load | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Median | Q1 | Q3 | Median | Q1 | Q3 | Median | Q1 | Q3 | Median | Q1 | Q3 | |
| Axial rotation | ||||||||||||
| Th11–Th12 | 5.2 | 2.0 | 5.7 | 3.3 | 1.7 | 4.6 | 3.4 | 1.8 | 4.5 | 3.1 | 1.8 | 5.0 |
| Th12–L1 | 4.0 | 1.8 | 4.7 | 2.6 | 1.2 | 3.2 | 5.1 | 3.7 | 6.1 | 4.1 | 2.6 | 4.5 |
| L1–L2 | 3.1 | 2.5 | 3.8 | 2.1 | 1.8 | 2.6 | 2.9 | 2.1 | 3.6 | 3.1 | 2.1 | 4.1 |
| L2–L3 | 4.4 | 3.4 | 6.1 | 2.6 | 2.2 | 4.2 | 2.7 | 2.4 | 4.2 | 2.9 | 2.4 | 4.3 |
| Extension-Flexion | ||||||||||||
| Th11–Th12 | 4.8 | 3.8 | 5.6 | 4.6 | 3.5 | 5.6 | 4.7 | 4.2 | 6.6 | 5.0 | 3.0 | 6.7 |
| Th12–L1 | 5.7 | 5.2 | 8.05 | 6.8 | 5.4 | 8.4 | 9.1 | 8.8 | 12.4 | 8.2 | 6.8 | 9.7 |
| L1–L2 | 6.5 | 5.1 | 7.2 | 6.5 | 5.7 | 7.8 | 7.5 | 6.0 | 10.0 | 6.3 | 5.5 | 8.9 |
| L2–L3 | 8.2 | 6.3 | 8.9 | 8.6 | 6.3 | 9.7 | 9.0 | 6.2 | 9.9 | 9.6 | 6.3 | 9.9 |
| Lateral flexion | ||||||||||||
| Th11–Th12 | 4.2 | 3.5 | 6.4 | 3.1 | 1.7 | 4.5 | 3.6 | 1.8 | 4.6 | 3.8 | 1.4 | 4.7 |
| Th12–L1 | 5.9 | 5.2 | 7.8 | 5.9 | 4.0 | 7.4 | 16.3 | 13.9 | 20.7 | 11.6 | 9.3 | 14.0 |
| L1–L2 | 7.9 | 6.3 | 8.9 | 7.1 | 6.1 | 8.9 | 14.3 | 9.2 | 16.0 | 9.2 | 7.4 | 12.4 |
| L2– L3 | 9.9 | 6.7 | 11.7 | 9.0 | 5.9 | 11.2 | 9.8 | 5.9 | 14.9 | 9.6 | 6.6 | 13.2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Riesenbeck, O.; Czarnowski, N.; Raschke, M.J.; Oeckenpöhler, S.; Hartensuer, R. Primary Stability of Kyphoplasty in Incomplete Vertebral Body Burst Fractures in Osteoporosis: A Biomechanical Investigation. Bioengineering 2024, 11, 798. https://doi.org/10.3390/bioengineering11080798
Riesenbeck O, Czarnowski N, Raschke MJ, Oeckenpöhler S, Hartensuer R. Primary Stability of Kyphoplasty in Incomplete Vertebral Body Burst Fractures in Osteoporosis: A Biomechanical Investigation. Bioengineering. 2024; 11(8):798. https://doi.org/10.3390/bioengineering11080798
Chicago/Turabian StyleRiesenbeck, Oliver, Niklas Czarnowski, Michael Johannes Raschke, Simon Oeckenpöhler, and René Hartensuer. 2024. "Primary Stability of Kyphoplasty in Incomplete Vertebral Body Burst Fractures in Osteoporosis: A Biomechanical Investigation" Bioengineering 11, no. 8: 798. https://doi.org/10.3390/bioengineering11080798
APA StyleRiesenbeck, O., Czarnowski, N., Raschke, M. J., Oeckenpöhler, S., & Hartensuer, R. (2024). Primary Stability of Kyphoplasty in Incomplete Vertebral Body Burst Fractures in Osteoporosis: A Biomechanical Investigation. Bioengineering, 11(8), 798. https://doi.org/10.3390/bioengineering11080798







