Artificial Intelligence Support for Informal Patient Caregivers: A Systematic Review
Abstract
1. Introduction
1.1. Background
1.2. Problem Statement and Research Questions
- How does AI impact the support of informal caregivers for patients?
- How well do various AI strategies perform in caregiver-related tasks for informal caregivers?
- What obstacles prohibit the integration of AI solutions in caregiving?
- What weaknesses exist in the present research, and which areas are recommended for future exploration?
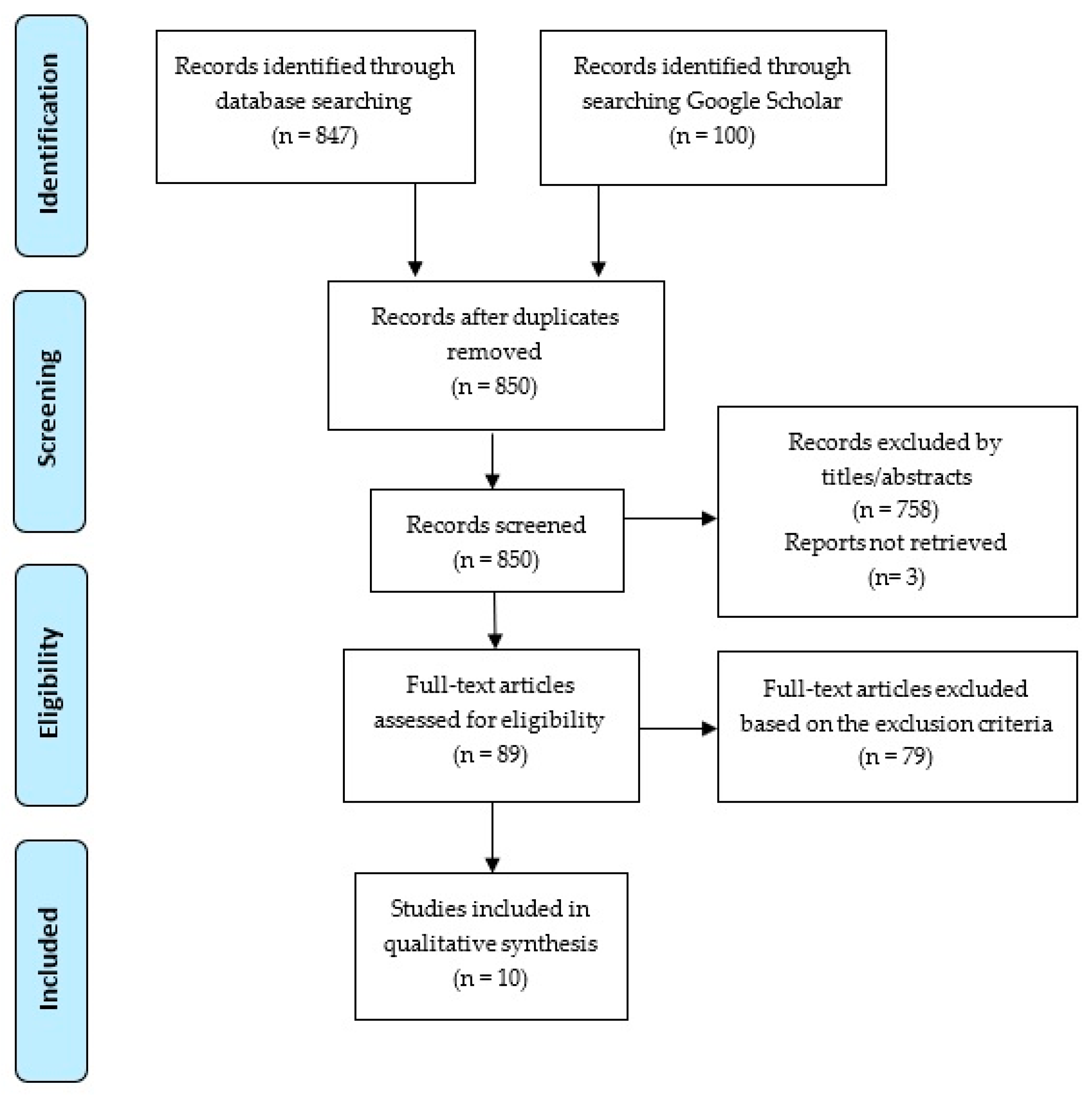
2. Methods
2.1. Databases Searched and Search Strategy
2.2. Study Eligibility and Selection Process
2.3. Data Quality and Risk of Bias Assessment
2.4. Data Synthesis and Analysis
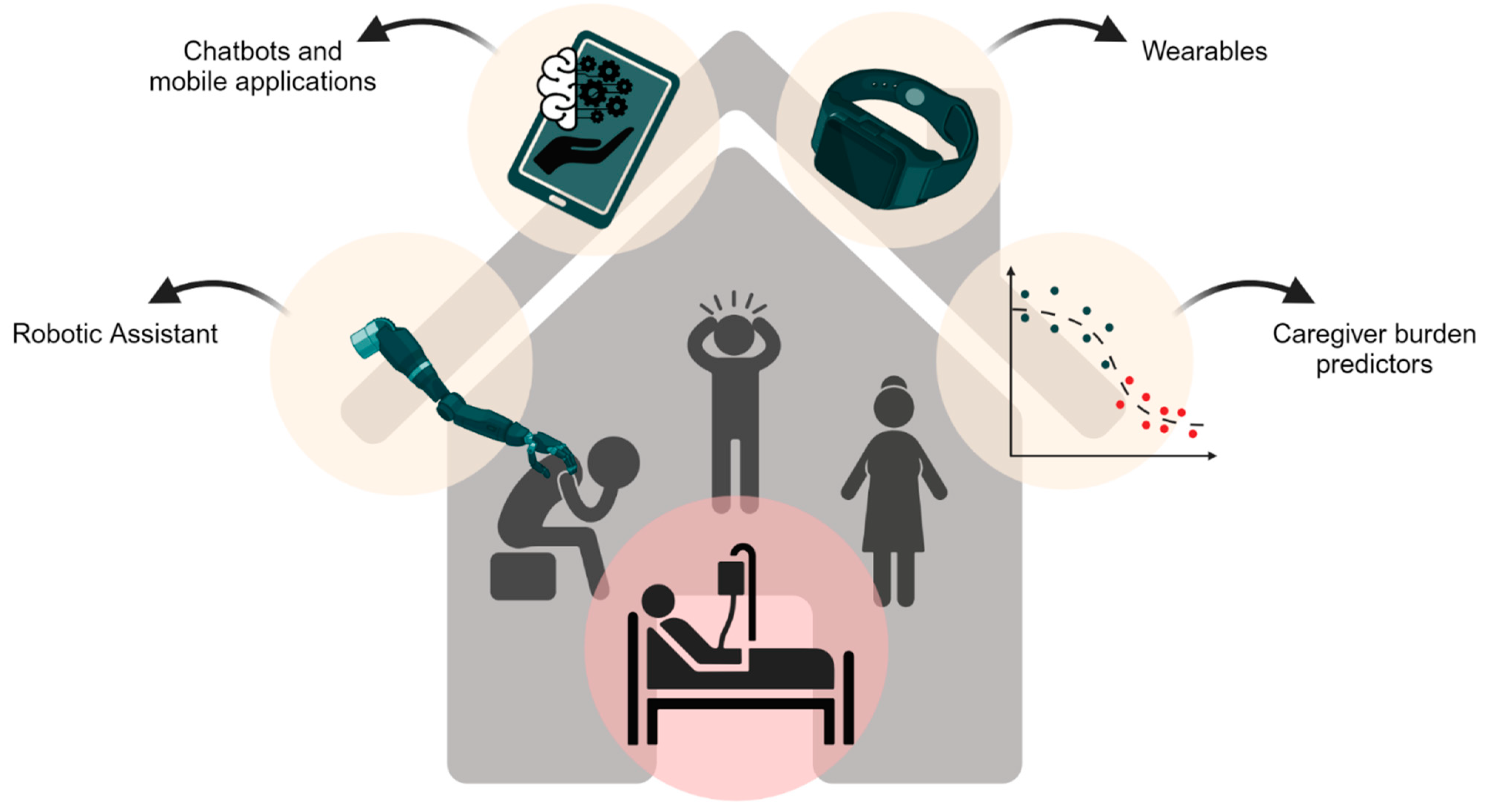
3. Results
Characteristics of Included Studies
4. Discussion
4.1. Implications and Key Findings
4.1.1. Mental Health Support for Family and Informal Caregivers
4.1.2. How Does AI Enhance Decision Making for Caregivers?
4.1.3. AI, Caregivers’ Burden, and Quality of Life
4.2. Limitations
4.3. Recommendations for Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Mason, D. Family Caregiving: Realities and Policy. In Proceedings of the JAMA Forum Archive; American Medical Association: Chicago, IL, USA, 2016. [Google Scholar]
- Reinhard, S.C.; Levine, C.; Samis, S. Home Alone: Family Caregivers Providing Complex Chronic Care; AARP Public Policy Institute: Washington, DC, USA, 2012; Volume 50. [Google Scholar]
- Hensely-Schinkinger, S.; de Carvalho, A.F.P.; Glanznig, M.; Tellioğlu, H. The definition and use of personas in the design of technologies for informal caregivers. In Proceedings of the Human-Computer Interaction: Design and Evaluation: 17th International Conference, HCI International, Los Angeles, CA, USA, 2–7 August 2015; Lecture Notes in Computer Science (Including Subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics). pp. 202–213. [Google Scholar]
- Amabili, G.; Maranesi, E.; Margaritini, A.; Benadduci, M.; Barbarossa, F.; Casaccia, S.; Nap, H.H.; Bevilacqua, R. Usability and Feasibility Assessment of a Social Assistive Robot for the Older People: Results from the GUARDIAN Project. Bioengineering 2024, 11, 20. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.-M.; Chen, Y.-J.; Chen, S.-C.; Zheng, S.-F. Creating an AI-Enhanced Morse Code Translation System Based on Images for People with Severe Disabilities. Bioengineering 2023, 10, 1281. [Google Scholar] [CrossRef] [PubMed]
- Gruenerbel, L.; Heinrich, F.; Böhlhoff-Martin, J.; Röper, L.; Machens, H.-G.; Gruenerbel, A.; Schillinger, M.; Kist, A.; Wenninger, F.; Richter, M.; et al. Wearable Prophylaxis Tool for AI-Driven Identification of Early Warning Patterns of Pressure Ulcers. Bioengineering 2023, 10, 1125. [Google Scholar] [CrossRef] [PubMed]
- Ahn, K.; Cho, M.; Kim, S.W.; Lee, K.E.; Song, Y.; Yoo, S.; Jeon, S.Y.; Kim, J.L.; Yoon, D.H.; Kong, H.-J. Deep Learning of Speech Data for Early Detection of Alzheimer’s Disease in the Elderly. Bioengineering 2023, 10, 1093. [Google Scholar] [CrossRef] [PubMed]
- Luo, X.; Tan, H.; Wen, W. Recent Advances in Wearable Healthcare Devices: From Material to Application. Bioengineering 2024, 11, 358. [Google Scholar] [CrossRef] [PubMed]
- Berg, K.M.; Fortinsky, R.H.; Robison, J. Family caregivers needed—No training provided. JAMA Intern. Med. 2019, 179, 835–836. [Google Scholar] [CrossRef] [PubMed]
- Cloyes, K.G.; Hart, S.E.; Jones, A.K.; Ellington, L. Where are the family caregivers? Finding family caregiver-related content in foundational nursing documents. J. Prof. Nurs. 2020, 36, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Adelman, R.D.; Tmanova, L.L.; Delgado, D.; Dion, S.; Lachs, M.S. Caregiver burden: A clinical review. JAMA 2014, 311, 1052–1060. [Google Scholar] [CrossRef] [PubMed]
- Al-Megren, S.; Majrashi, K.; Allwihan, R.M. “The Dementia Diva Strikes Again!”: A Thematic Analysis of How Informal Carers of Persons with Dementia Use TikTok. In Proceedings of the Extended Abstracts of MobileHCI 2021—ACM International Conference on Mobile Human-Computer Interaction: Mobile Apart, Mobile Together, Online, 27 September 2021. [Google Scholar]
- Miranda, D.; Favela, J.; Ibarra, C. Detecting state anxiety when caring for people with dementia. In Proceedings of the Ambient Intelligence for Health: First International Conference, AmIHEALTH 2015, Puerto Varas, Chile, 1–4 December 2015; Lecture Notes in Computer Science (Including Subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics). pp. 98–109. [Google Scholar]
- Pettini, A. Real-Time Assessment of the Burden on the Community of Informal Caregivers. A Pilot Study. Int. J. Community Well-Being 2020, 3, 491–505. [Google Scholar] [CrossRef]
- Chi, N.-C.; Demiris, G. Family caregivers’ pain management in end-of-life care: A systematic review. Am. J. Hosp. Palliat. Med. 2017, 34, 470–485. [Google Scholar] [CrossRef]
- Lauer-Schmaltz, M.W.; Kerim, I.; Hansen, J.P.; Gulyás, G.M.; Andersen, H.B. Human Digital Twin-based interactive dashboards for informal caregivers of stroke patients. In Proceedings of the 16th International Conference on PErvasive Technologies Related to Assistive Environments, Corfu, Greece, 5–7 July 2023; ACM International Conference Proceeding Series. pp. 215–221. [Google Scholar]
- Choi, K.W.; Shaffer, K.M.; Zale, E.L.; Funes, C.J.; Koenen, K.C.; Tehan, T.; Rosand, J.; Vranceanu, A.M. Early risk and resiliency factors predict chronic posttraumatic stress disorder in caregivers of patients admitted to a neuroscience ICU. Crit. Care Med. 2018, 46, 713–719. [Google Scholar] [CrossRef] [PubMed]
- Blasioli, E.; Hassini, E. E-Health Technological Ecosystems: Advanced Solutions to Support Informal Caregivers and Vulnerable Populations during the COVID-19 Outbreak. Telemed. e-Health 2022, 28, 138–149. [Google Scholar] [CrossRef] [PubMed]
- Czaja, S.J.; Perdomo, D.; Lee, C.C. The role of technology in supporting family caregivers. In Proceedings of the Human Aspects of IT for the Aged Population. Design for Aging: Second International Conference, ITAP 2016, Held as Part of HCI International 2016, Toronto, ON, Canada, 17–22 July 2016; Lecture Notes in Computer Science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics). pp. 178–185. [Google Scholar]
- Egan, K.J.; Clark, P.; Deen, Z.; Dutu, C.P.; Wilson, G.; McCann, L.; Lennon, M.; Maguire, R. Understanding Current Needs and Future Expectations of Informal Caregivers for Technology to Support Health and Well-being: National Survey Study. JMIR Aging 2022, 5, e15413. [Google Scholar] [CrossRef] [PubMed]
- Demiris, G.; Washington, K.; Ulrich, C.M.; Popescu, M.; Oliver, D.P. Innovative Tools to Support Family Caregivers of Persons with Cancer: The Role of Information Technology. Semin. Oncol. Nurs. 2019, 35, 384–388. [Google Scholar] [CrossRef] [PubMed]
- Denecke, K.; May, R.; Borycki, E.M.; Kushniruk, A.W. Digital health as an enabler for hospital@ home: A rising trend or just a vision? Front. Public Health 2023, 11, 1137798. [Google Scholar] [CrossRef] [PubMed]
- Désormeaux-Moreau, M.; Michel, C.M.; Vallières, M.; Racine, M.; Poulin-Paquet, M.; Lacasse, D.; Gionet, P.; Genereux, M.; Lachiheb, W.; Provencher, V. Mobile apps to support family caregivers of people with Alzheimer disease and related dementias in managing disruptive behaviors: Qualitative study with users embedded in a scoping review. JMIR Aging 2021, 4, e21808. [Google Scholar] [CrossRef] [PubMed]
- Doorenbos, A.Z.; Jang, M.K.; Li, H.; Lally, R.M. eHealth Education: Methods to enhance oncology nurse, patient, and caregiver teaching. Clin. J. Oncol. Nurs. 2020, 24, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Egan, K.J.; Hodgson, W.; Dunlop, M.D.; Imperatore, G.; Kirk, A.; Maguire, R. A Novel Mobile App (“CareFit”) to Support Informal Caregivers to Undertake Regular Physical Activity from Home during and beyond COVID-19 Restrictions: Co-design and Prototype Development Study. JMIR Form. Res. 2021, 5, e27358. [Google Scholar] [CrossRef] [PubMed]
- Hensely-Schinkinger, S. Support services for informal caregivers: Survey with providers in Austria. In Proceedings of the Computers Helping People with Special Needs: 15th International Conference, ICCHP 2016, Linz, Austria, 13–15 July 2016; Lecture Notes in Computer Science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics). pp. 310–313. [Google Scholar]
- Morandín-Ahuerma, F. What is Artificial Intelligence? Int. J. Res. Publ. Rev. 2022, 3, 1947–1951. [Google Scholar] [CrossRef]
- Ala-Kitula, A.; Talvitie-Lamberg, K.; Tyrväinen, P.; Silvennoinen, M. Developing Solutions for Healthcare—Deploying Artificial Intelligence to an Evolving Target. In Proceedings of the 2017 International Conference on Computational Science and Computational Intelligence (CSCI), Las Vegas, NV, USA, 14–16 December 2017; pp. 1637–1642. [Google Scholar]
- Ho, A. Live Like Nobody is Watching: Relational Autonomy in the Age of Artificial Intelligence Health Monitoring; Oxford University Press: Oxford, UK, 2023. [Google Scholar]
- Roski, J.; Hamilton, B.; Chapman, W.; Heffner, J.; Trivedi, R.; Del Fiol, G.; Kukafka, R.; Bleicher, P.; Estiri, H.; Klann, J. How Artificial Intelligence is Changing Health and Health Care; National Academy of Medicine: Washington, DC, USA, 2019; Volume 58. [Google Scholar]
- Baisch, S.; Kolling, T.; Rühl, S.; Klein, B.; Pantel, J.; Oswald, F.; Knopf, M. Emotional robots in a nursing context: Empirical analysis of the present use and the effects of Paro and Pleo. Z. Gerontol. Geriatr. 2018, 51, 16–24. [Google Scholar] [CrossRef]
- Broadbent, E.; Tamagawa, R.; Patience, A.; Knock, B.; Kerse, N.; Day, K.; MacDonald, B.A. Attitudes towards health-care robots in a retirement village. Australas J. Ageing 2012, 31, 115–120. [Google Scholar] [CrossRef] [PubMed]
- Johnston, C. Ethical Design and Use of Robotic Care of the Elderly. J. Bioethical Inq. 2022, 19, 11–14. [Google Scholar] [CrossRef] [PubMed]
- Kodate, N.; Donnelly, S.; Suwa, S.; Tsujimura, M.; Kitinoja, H.; Hallila, J.; Toivonen, M.; Ide, H.; Yu, W. Home-care robots—Attitudes and perceptions among older people, carers and care professionals in Ireland: A questionnaire study. Health Soc. Care Community 2022, 30, 1086–1096. [Google Scholar] [CrossRef] [PubMed]
- Neef, C.; Schneider, S.; Richert, A. An architecture for social robot-assisted subjective and objective health monitoring. In Proceedings of the 2022 IEEE International Conference on Advanced Robotics and Its Social Impacts (ARSO), Long Beach, CA, USA, 28–30 May 2022; pp. 1–6. [Google Scholar]
- Kouroubali, A.; Kondylakis, H.; Logothetidis, F.; Katehakis, D.G. Developing an AI-Enabled Integrated Care Platform for Frailty. Healthcare 2022, 10, 443. [Google Scholar] [CrossRef] [PubMed]
- Kearns, W.; Laine, M.; Oh, E.; Thompson, H.; Demiris, G. 278 Understanding Perspectives on Artificial Intelligence Technologies for Sleep Self-Management. Sleep 2021, 44, A111. [Google Scholar] [CrossRef]
- Gappa, H.; Mohamad, Y.; Heiba, N.; Zenz, D.; Mesenhöller, T.; Zurkuhlen, A.; Pöpper, J.; Schmidt-Barzynski, W. A step forward in supporting home care more effectively: Individually tailored in-home care consultancy utilizing machine learning. In Proceedings of the 10th International Conference on Software Development and Technologies for Enhancing Accessibility and Fighting Info-Exclusion, Lisbon, Portugal, 31 August–2 September 2022; pp. 31–36. [Google Scholar]
- Chen, H.; Zhao, Y.; Zhao, T.; Chen, J.; Li, S.; Zhao, S. Emotion Recognition of the Elderly Living Alone Based on Deep Learning. In Proceedings of the 2021 IEEE International Conference on Consumer Electronics-Taiwan (ICCE-TW), Penghu, Taiwan, 15–17 September 2021; pp. 1–2. [Google Scholar]
- Gencturk, M.; Laleci Erturkmen, G.B.; Gappa, H.; Schmidt-Barzynski, W.; Steinhoff, A.; Abizanda, P.; Robbins, T.; Pournik, O.; Ahmad, B.; Randeva, H.; et al. The design of a mobile platform providing personalized assistance to older multimorbid patients with mild dementia or mild cognitive impairment (MCI). In Proceedings of the 10th International Conference on Software Development and Technologies for Enhancing Accessibility and Fighting Info-Exclusion, Lisbon Portugal, 31 August–2 September 2022; Association for Computing Machinery: New York, NY, USA, 2022; pp. 37–43. [Google Scholar]
- Girju, R.; Girju, M. Design considerations for an NLP-driven empathy and emotion interface for clinician training via telemedicine. In Proceedings of the Second Workshop on Bridging Human—Computer Interaction and Natural Language Processing, Online, 15 July 2022; pp. 21–27. [Google Scholar]
- Chiang, C.Y.; Chen, Y.L.; Yu, C.W.; Yuan, S.M.; Hong, Z.W. An Efficient Component-Based Framework for Intelligent Home-Care System Design with Video and Physiological Monitoring Machineries. In Proceedings of the 2011 Fifth International Conference on Genetic and Evolutionary Computing, Kitakyushu, Japan, 29 August–1 September 2011; pp. 33–36. [Google Scholar]
- Chung, J.; Demiris, G.; Thompson, H.J. Ethical Considerations Regarding the Use of Smart Home Technologies for Older Adults: An Integrative Review. Annu. Rev. Nurs. Res. 2016, 34, 155–181. [Google Scholar] [CrossRef] [PubMed]
- Gelhaus, L. High-tech homes mean a brighter future for seniors. Provider 2002, 28, 40–42. [Google Scholar] [PubMed]
- Sánchez, P.A.M.; Fernández, P.C.; González, P.S.; Charvill, J.; Lofti, A.; Langensiepen, C.S.; Pacheco, J.L.G.; Saunders, A.; Berckmans, K.; Gaspersic, J.; et al. iCarer Project: Intelligent Care Guidance and Learning Services Platform for Informal Carers of the Elderly. In Proceedings of the XXXII Congreso Anual de la Sociedad Española de Ingeniería Biomédica (CASEIB 2014), Barcelona, Spain, 26–28 November 2014. [Google Scholar]
- Wongpun, S.; Guha, S. Elderly care recommendation system for informal caregivers using case-based reasoning. In Proceedings of the 2017 IEEE 2nd Advanced Information Technology, Electronic and Automation Control Conference (IAEAC), Chongqing, China, 25–26 March 2017; pp. 548–552. [Google Scholar]
- Costa, V.; Messina, M.; Bottone, M.; Sperandeo, R.; Esposito, A.; Maldonato, N.M.; Cioffi, V.; Ronza, G.d.; Iennaco, D.; Dolce, P.; et al. A deep learning algorithm to prevent burnout risk in Family Caregivers of patients undergoing dialysis treatment. In Proceedings of the 2018 9th IEEE International Conference on Cognitive Infocommunications (CogInfoCom), Budapest, Hungary, 22–24 August 2018; pp. 299–304. [Google Scholar]
- Antoniadi, A.M.; Galvin, M.; Heverin, M.; Hardiman, O.; Mooney, C. Prediction of caregiver burden in amyotrophic lateral sclerosis: A machine learning approach using random forests applied to a cohort study. BMJ Open. 2020, 10, e033109. [Google Scholar] [CrossRef] [PubMed]
- Antoniadi, A.M.; Galvin, M.; Heverin, M.; Hardiman, O.; Mooney, C. Prediction of caregiver quality of life in amyotrophic lateral sclerosis using explainable machine learning. Sci. Rep. 2021, 11, 12237. [Google Scholar] [CrossRef]
- Wolff, D.; Kupka, T.; Marschollek, M. Extending a knowledge-based system with learning capacity. In Proceedings of the Studies in Health Technology and Informatics; IOS Press: Amsterdam, The Netherlands, 2019; pp. 150–155. [Google Scholar]
- Kim, J.W.; Choi, Y.L.; Jeong, S.H.; Han, J. A Care Robot with Ethical Sensing System for Older Adults at Home. Sensors 2022, 2, 7515. [Google Scholar] [CrossRef]
- Wunderlich, P.; Wiegrabe, F.; Dorksen, H. Digital Case Manager-A Data-Driven Tool to Support Family Caregivers with Initial Guidance. Int. J. Environ. Res. Public Health 2023, 20, 1215. [Google Scholar] [CrossRef] [PubMed]
- Aziz, A.A.; Treur, J.; Van Der Wal, C.N. An ambient agent model for support of informal caregivers during stress. In Proceedings of the 25th International Conference on Industrial Engineering and Other Applications of Applied Intelligent Systems, IEA/AIE 2012, Dalian, China, 9–12 June 2012; Lecture Notes in Computer Science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics). pp. 501–513. [Google Scholar]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef] [PubMed]
- Suksawatchon, U.; Suksawatchon, J.; Lawang, W. Health risk analysis expert system for family caregiver of person with disabilities using data mining techniques. ECTI Trans. Comput. Inf. Technol. 2018, 12, 62–72. [Google Scholar] [CrossRef]
- Joerin, A.; Rauws, M.; Ackerman, M.L. Psychological artificial intelligence service, Tess: Delivering on-demand support to patients and their caregivers: Technical report. Cureus 2019, 11, e3972. [Google Scholar] [CrossRef] [PubMed]
- Demiris, G.; Oliver, D.P.; Washington, K.T.; Chadwick, C.; Voigt, J.D.; Brotherton, S.; Naylor, M.D. Examining spoken words and acoustic features of therapy sessions to understand family caregivers’ anxiety and quality of life. Int. J. Med. Inform. 2022, 160, 104716. [Google Scholar] [CrossRef] [PubMed]
- Fulmer, R.; Joerin, A.; Gentile, B.; Lakerink, L.; Rauws, M. Using Psychological Artificial Intelligence (Tess) to Relieve Symptoms of Depression and Anxiety: Randomized Controlled Trial. JMIR Ment. Health 2018, 5, e64. [Google Scholar] [CrossRef]
- Aziz, A.A.; Treur, J.; van der Wal, C.N. Modelling Caregiving Interactions during Stress. In Proceedings of the Brain Informatics, Berlin, Heidelberg, 28–30 August 2010; pp. 263–273. [Google Scholar]
- Lilleheie, I.; Debesay, J.; Bye, A.; Bergland, A. The tension between carrying a burden and feeling like a burden: A qualitative study of informal caregivers’ and care recipients’ experiences after patient discharge from hospital. Int. J. Qual Stud. Health Well-Being 2021, 16, 1855751. [Google Scholar] [CrossRef]
- Nakken, N.; Janssen, D.J.A.; van den Bogaart, E.H.A.; Wouters, E.F.M.; Franssen, F.M.E.; Vercoulen, J.; Spruit, M.A. Informal caregivers of patients with COPD: Home Sweet Home? Eur. Respir. Rev. 2015, 24, 498–504. [Google Scholar] [CrossRef] [PubMed]
- Stroka, M.A. The Mental and Physical Burden of Caregiving. Demand Supply Health Econ. Ejournal 2014. Available online: https://ssrn.com/abstract=2470552 (accessed on 9 January 2024). [CrossRef]
- Aoki, S. BioRender. Available online: https://www.biorender.com/ (accessed on 9 January 2024).
- Moons, K.G.M.; Wolff, R.F.; Riley, R.D.; Whiting, P.F.; Westwood, M.; Collins, G.S.; Reitsma, J.B.; Kleijnen, J.; Mallett, S. PROBAST: A Tool to Assess Risk of Bias and Applicability of Prediction Model Studies: Explanation and Elaboration. Ann. Intern. Med. 2019, 170, W1–W33. [Google Scholar] [CrossRef]
| Research Unit | Search Terms/Keywords |
|---|---|
| Technologies | AI, ML, NLP, artificial intelligence, machine learning, deep learning, neural networks, and natural language processing |
| Care context | home caregivers, home care, care at home, family caregivers, home caretaker, home carers, home patient caregivers, home-based patient care, home caregivers for patients, home care for patients, non-professional caregiver, informal caregiver, unpaid caregiver, unpaid informal carer, and relative caregiver |
| Exclusion criteria | healthy child, general child care, nurse, doctor, physician, and medical professional |
| Author | Location | Study Aim | Study Design | Participants | Type of AI | Validation Method | Metric Scores |
|---|---|---|---|---|---|---|---|
| Aziz et al., 2012 [53] | Netherlands | Designing an ambient agent to assist caregivers of patients with depression. | Model development and validation | Three fictional types of caregivers (CG1, CG2, and CG3) in simulation experiments | Model-based reasoning | Simulation experiments Verification of identified properties | N/A |
| Suksawatchon et al., 2018 [55] | Thailand | Introducing a new expert system to assess caregivers’ health risk levels in mental, physical, and social domains and provide customized interventions for each. | Model development and validation | Data of 150 caregivers to train and evaluate the RAC model | RAC: HRAS (classifier technique and rule-based classifier) SCUT algorithm (hybrid sampling technique) ML: Decision tree Naive Bayes (Kernel) NN LibSVM | k-fold CV Experts with annotated and unseen data | Accuracy with SCUT: NN: mental (ACC at 94.71%), social (ACC at 95.36%); LibSVM: physical (ACC at 93.42%) Precision with SCUT: NN: mental (94.81%), physical (94.81%), and social (95.95%) Recall with SCUT: NN: mental (94.74%); LibSVM: physical (93.42%); NN: social (95.40%) F-measure with SCUT: NN: mental (94.67%); LibSVM: physical (93.30%); NN: social (95.41%) |
| Costa et al., 2018 [47] | Italy | Assessing burnout risk in dialysis patient caregivers and develop a stress measurement tool. | Model development and validation | Seven hundred and thirteen family caregivers of dialysis patients | ML: DNN | Hold-Out validation | Sample training (%) and sample test (%): Correct forecast (no stress): 62.80, 72.00 Correct forecast (stress): 78.80, 83.70 Global accuracy: 71.60, 78.70 Area under ROC: 0.802, 0.802 |
| Joerin et al., 2018 [56] | Canada | Examining how a mental health chatbot provides customized, immediate emotional support to family caregivers at a non-profit organization. | Technical report | Relatives of patients aged 20–59, with most between 50 and 59 | Tess chatbot | N/A | N/A |
| Wolff et al., 2019 [50] | Germany | Using a personalized system to offer targeted educational content to caregivers based on their needs. | Model development and validation | Three thousand and two hundred artificially created profiles for training the ANN and six hundred and forty randomly generated profiles for the validation set | ML: ANN | Hold-Out Validation End-Validation Set Utilized Termination Criterion | Total training epochs: 374,700 Incorrectly ordered training profiles: 8 out of 3200 Final MSE (training set): 8.585 × 10−8 Final MSE (validation set): 7.731 × 10−8 |
| Antoniadi et al., 2020 [48] | Ireland | Predicting caregiver burden in ALS patients and identify related features using machine learning. | Model development and validation | Ninety ALS patients and their primary caregivers | ML: random forest | 10-fold CV | Metric/model: Model M2, Model M3, and Model M9 Ten-fold CV—sensitivity: 0.82, 0.80, and 0.71 Ten-fold CV—specificity: 0.77, 0.83, and 0.63 Independent test data—sensitivity: 0.92, 0.80, and 0.84 Independent test data—specificity: 0.78, 0.78, and 0.72 AUC: 0.85, 0.83, and 0.79 |
| Antoniadi et al., 2021 [49] | Ireland | Identifying caregiver QoL predictors and creating models for a CDSS. | Model development and validation | Ninety patient and caregiver pairs | ML: LASSO XGBoost | Hold-Out Validation | Model: F1, recall, precision, and AUC Predictors of QoL: Baseline: 0.76, 0.72, 0.81, and 0.72; Full: 0.84, 0.83, 0.86, and 0.80; M7: 0.83, 0.83, 0.83, and 0.77 CDSS models: Baseline-CDSS: 0.52, 0.45, 0.62, and 0.50; Full-CDSS: 0.71, 0.72, 0.70, and 0.61; M10-CDSS: 0.75, 0.79, 0.72, and 0.65; M6-CDSS: 0.70, 0.72, 0.68, and 0.58 |
| Kim et al., 2022 [51] | Korea | Developing “Dori,” a robot for supporting frail elderly at home, balancing their dignity and caregiver values within the HCAI framework. | Technical report | Caregivers, nurses, and clinicians | ML | N/A | Caregivers, medical staff, T-value, and p-value Cognitive activity: 6.05 (±1.77), 5.64 (±2.23), 0.96, and 0.344 Emotional activity: 6.36 (±1.78), 5.6 (±3.04), 1.63, and 0.109 Physical activity: 5.82 (±2.69), 5.32 (±2.62), 1.02, and 0.311 Medication instruction: 6.05 (±2.59), 6.04 (±1.64), 0.01, and 0.990 Caregiver management: 5.86 (±2.94), 5.4 (±2.32), 0.96, and 0.342 |
| Demiris et al., 2022 [57] | United States | Evaluating ML classifiers’ relation to anxiety and QoL based on spoken words and features from caregiver–therapist talks. | Model development and validation | Dataset of 124 audio-recorded conversations between hospice patient caregivers and a therapist | ML: LR (text and audio) DL: (ASR System (DeepSpeech2)) | Hold-Out Validation | Classifier: precision, recall, accuracy, and specificity CQLI-R (total): 73%, 79%, 76%, and 73% Physical: 80%, 86%, 83%, and 80% Financial: 69%, 90%, 81%, and 75% Social: 82%, 69%, 73%, and 78% Emotional: 77%, 63%, 68%, and 75% GAD: 92%, 88%, and 89% |
| Wunderlich et al., 2023 [52] | Germany | Using ML to guide family caregivers in healthcare decisions and caregiving tasks. | Model development and validation | Twenty-eight use cases, crafted by care experts | ML: random forest | Two-fold and ten-fold CV | Metrics: Dataset 100, Dataset 500, Dataset 1000 Accuracy: 80.00%, 99.33%, and 99.33% F1-score: 0.9306, 0.9993, and 0.9993 Two-fold CV: 56%, 97.78%, and 99.7% Ten-fold CV: 73%, 99.2%, and 99.8% Hamming loss: 0.01764, 0.00039, and 0.00039 Coverage error: 6.06, 4.85, and 4.94 Label ranking average precision: 0.9209, 0.9993, and 0.9993 Label ranking loss: 0.0648, 0.0011, and 0.0011 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Borna, S.; Maniaci, M.J.; Haider, C.R.; Gomez-Cabello, C.A.; Pressman, S.M.; Haider, S.A.; Demaerschalk, B.M.; Cowart, J.B.; Forte, A.J. Artificial Intelligence Support for Informal Patient Caregivers: A Systematic Review. Bioengineering 2024, 11, 483. https://doi.org/10.3390/bioengineering11050483
Borna S, Maniaci MJ, Haider CR, Gomez-Cabello CA, Pressman SM, Haider SA, Demaerschalk BM, Cowart JB, Forte AJ. Artificial Intelligence Support for Informal Patient Caregivers: A Systematic Review. Bioengineering. 2024; 11(5):483. https://doi.org/10.3390/bioengineering11050483
Chicago/Turabian StyleBorna, Sahar, Michael J. Maniaci, Clifton R. Haider, Cesar A. Gomez-Cabello, Sophia M. Pressman, Syed Ali Haider, Bart M. Demaerschalk, Jennifer B. Cowart, and Antonio Jorge Forte. 2024. "Artificial Intelligence Support for Informal Patient Caregivers: A Systematic Review" Bioengineering 11, no. 5: 483. https://doi.org/10.3390/bioengineering11050483
APA StyleBorna, S., Maniaci, M. J., Haider, C. R., Gomez-Cabello, C. A., Pressman, S. M., Haider, S. A., Demaerschalk, B. M., Cowart, J. B., & Forte, A. J. (2024). Artificial Intelligence Support for Informal Patient Caregivers: A Systematic Review. Bioengineering, 11(5), 483. https://doi.org/10.3390/bioengineering11050483











