Influence of Lateral Sitting Wedges on the Rasterstereographically Measured Scoliosis Angle in Patients Aged 10–18 Years with Adolescent Idiopathic Scoliosis
Abstract
1. Introduction
2. Materials and Methods
- Patients with an age of 10–18 years (including 18);
- A Cobb angle of 10–50° with lumbar/thoraco-lumbar involvement;
- No pain (numeric rating scale (NRS) ≤ 4);
- No acute illness, no chronic diseases with influence on balance;
- No previous surgery;
- BMI < 30 kg/m2;
- No change in the surface of the back due to large scars/tattoos.
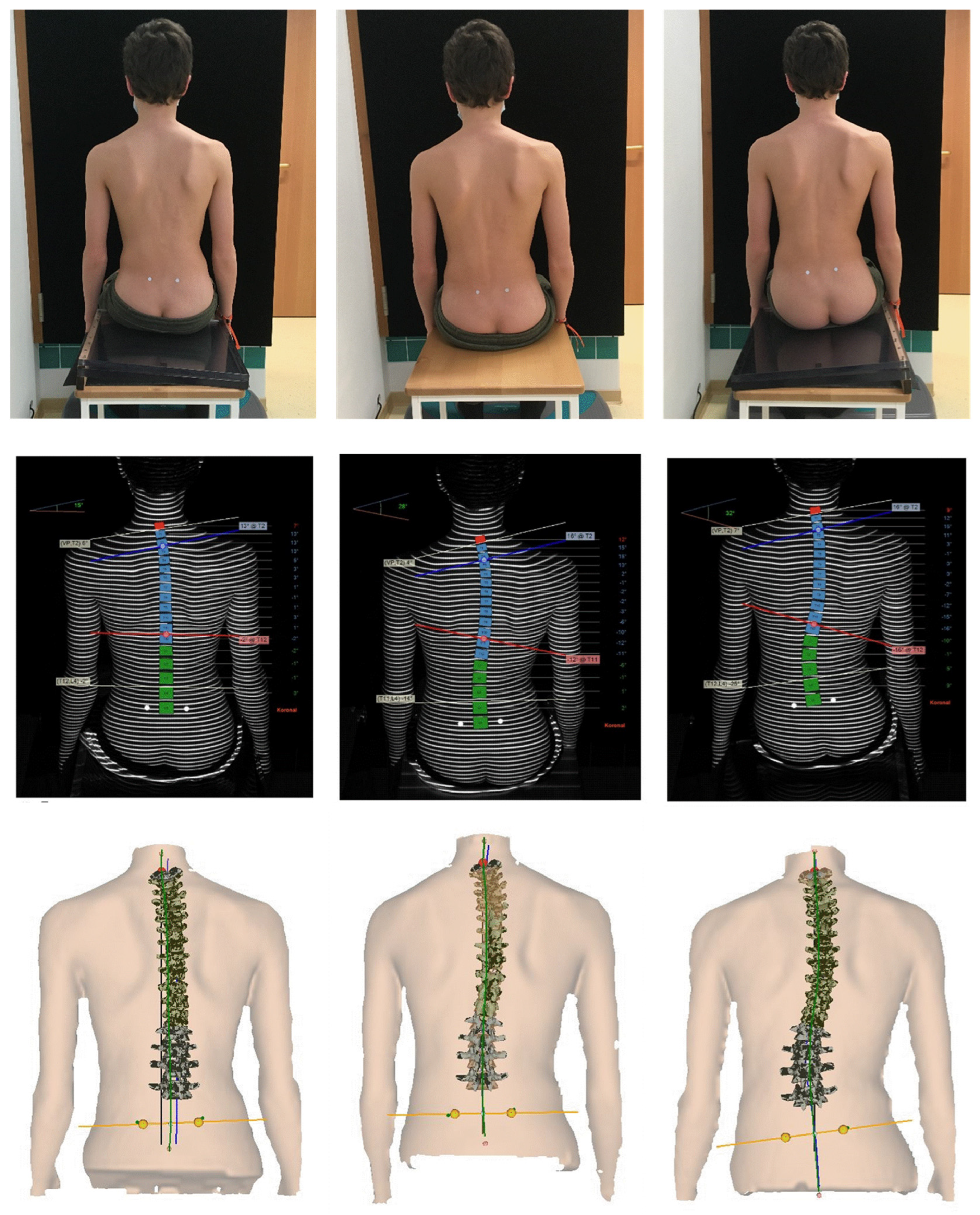
2.1. Method
2.2. Target Parameters
2.3. Statistics
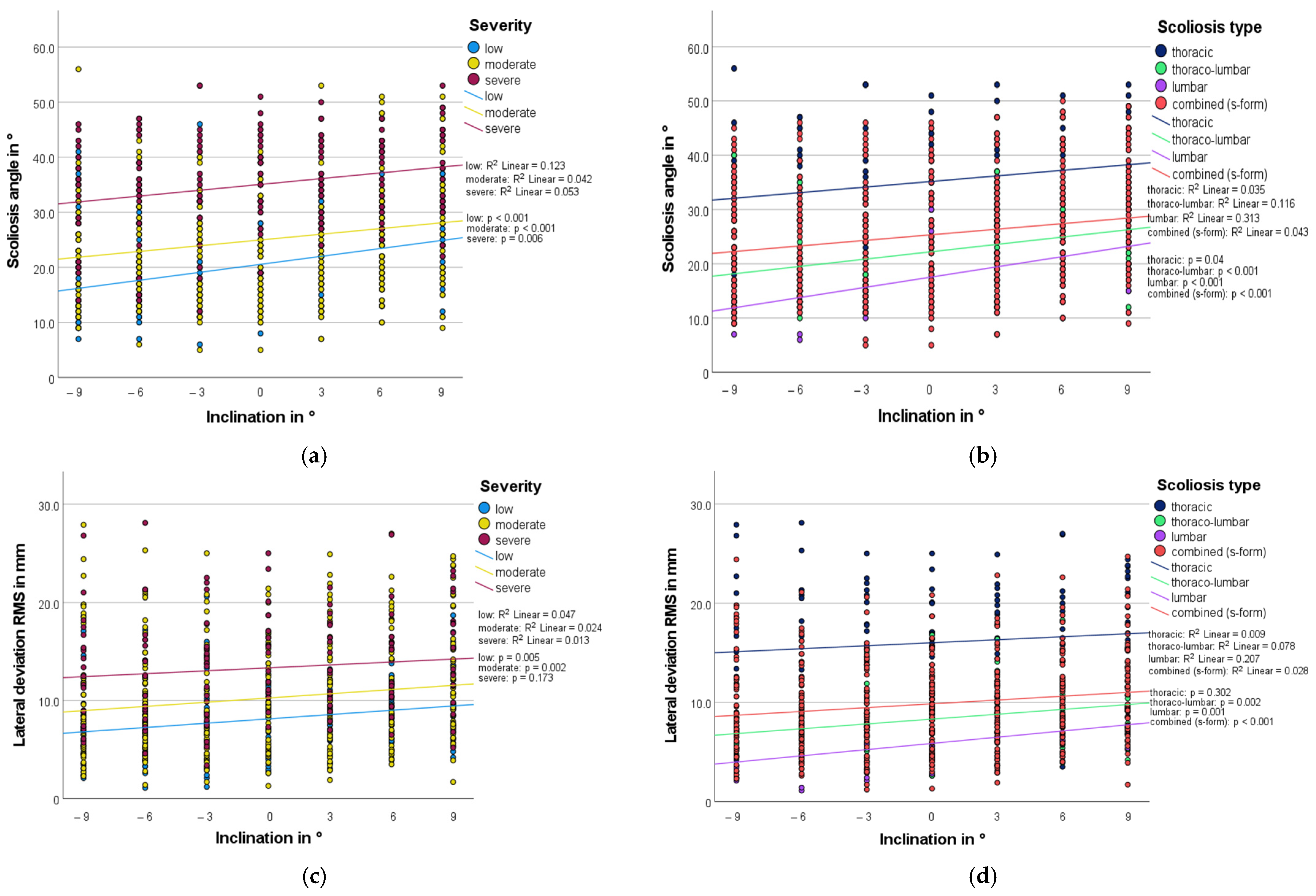
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Trobisch, P.; Suess, O.; Schwab, F. Idiopathic scoliosis. Dtsch Arztebl. Int. 2010, 107, 875–883, quiz 884. [Google Scholar] [CrossRef]
- Negrini, S.; Donzelli, S.; Aulisa, A.G.; Czaprowski, D.; Schreiber, S.; de Mauroy, J.C.; Diers, H.; Grivas, T.B.; Knott, P.; Kotwicki, T.; et al. 2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord. 2018, 13, 3. [Google Scholar] [CrossRef]
- Wang, H.; Tetteroo, D.; Arts, J.J.C.; Markopoulos, P.; Ito, K. Quality of life of adolescent idiopathic scoliosis patients under brace treatment: A brief communication of literature review. Qual. Life Res. 2021, 30, 703–711. [Google Scholar] [CrossRef]
- Stein, G.H.; Eysel, P.H.; Scheyerer, M.J.H. Expertise Orthopädie und Unfallchirurgie—Wirbelsäule; Georg Thieme Verlag KG: Stuttgart, Germany, 2019. [Google Scholar]
- Negrini, S.; Minozzi, S.; Bettany-Saltikov, J.; Chockalingam, N.; Grivas, T.B.; Kotwicki, T.; Maruyama, T.; Romano, M.; Zaina, F. Braces for idiopathic scoliosis in adolescents. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef]
- Burger, M.; Coetzee, W.; du Plessis, L.Z.; Geldenhuys, L.; Joubert, F.; Myburgh, E.; van Rooyen, C.; Vermeulen, N. The effectiveness of Schroth exercises in adolescents with idiopathic scoliosis: A systematic review and meta-analysis. S. Afr. J. Physiother. 2019, 75, 904. [Google Scholar] [CrossRef] [PubMed]
- Schreiber, S.; Parent, E.C.; Hill, D.L.; Hedden, D.M.; Moreau, M.J.; Southon, S.C. Patients with adolescent idiopathic scoliosis perceive positive improvements regardless of change in the Cobb angle—Results from a randomized controlled trial comparing a 6-month Schroth intervention added to standard care and standard care alone. SOSORT 2018 Award winner. BMC Musculoskelet. Disord. 2019, 20, 319. [Google Scholar]
- Nash, C.L., Jr.; Gregg, E.C.; Brown, R.H.; Pillai, K. Risks of exposure to X-rays in patients undergoing long-term treatment for scoliosis. J. Bone Joint Surg. Am. 1979, 61, 371–374. [Google Scholar] [CrossRef] [PubMed]
- Ronckers, C.M.; Land, C.E.; Miller, J.S.; Stovall, M.; Lonstein, J.E.; Doody, M.M. Cancer mortality among women frequently exposed to radiographic examinations for spinal disorders. Radiat. Res. 2010, 174, 83–90. [Google Scholar] [CrossRef]
- Simony, A.; Hansen, E.J.; Christensen, S.B.; Carreon, L.Y.; Andersen, M.O. Incidence of cancer in adolescent idiopathic scoliosis patients treated 25 years previously. Eur. Spine J. 2016, 25, 3366–3370. [Google Scholar] [CrossRef]
- Drerup, B. Rasterstereographic measurement of scoliotic deformity. Scoliosis 2014, 9, 22. [Google Scholar] [CrossRef]
- Drerup, B.; Ellger, B.; Bentrup, F.M.Z.; Hierholzer, E. Functional examinations with rasterstereography. A new method for the biomechanical analysis of skeletal geometry. Orthopade 2001, 30, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Dubousset, J. 3D analysis of scoliotic deformity development and 3D chain of balance in a scoliosis patient. Hir. Pozvonočnika Spine Surg. 2016, 13, 108–113. [Google Scholar] [CrossRef]
- Zabjek, K.F.; Leroux, M.A.; Coillard, C.; Martinez, X.; Griffet, J.; Simard, G.; Rivard, C.H. Acute postural adaptations induced by a shoe lift in idiopathic scoliosis patients. Eur. Spine J. 2001, 10, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Raczkowski, J.W.; Daniszewska, B.; Zolynski, K. Functional scoliosis caused by leg length discrepancy. Arch. Med. Sci. 2010, 6, 393–398. [Google Scholar] [CrossRef] [PubMed]
- Huber, G.; Köppel, M. Analyse der Sitzzeiten von Kindern und Jugendlichen zwischen 4 und 20 Jahren. Dtsch Z. Sportmed. 2017, 68, 101–106. [Google Scholar] [CrossRef]
- Drerup, B.; Hierholzer, E. Back shape measurement using video rasterstereography and three-dimensional reconstruction of spinal shape. Clin. Biomech. 1994, 9, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Schulte, T.L.; Hierholzer, E.; Boerke, A.; Lerner, T.; Liljenqvist, U.; Bullmann, V.; Hackenberg, L. Raster stereography versus radiography in the long-term follow-up of idiopathic scoliosis. J. Spinal Disord. Technol. 2008, 21, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Frerich, J.M.; Hertzler, K.; Knott, P.; Mardjetko, S. Comparison of radiographic and surface topography measurements in adolescents with idiopathic scoliosis. Open Orthop. J. 2012, 6, 261–265. [Google Scholar] [CrossRef]
- Tabard-Fougere, A.; Bonnefoy-Mazure, A.; Hanquinet, S.; Lascombes, P.; Armand, S.; Dayer, R. Validity and reliability of spine rasterstereography in patients with adolescent idiopathic scoliosis. Spine 2017, 42, 98–105. [Google Scholar] [CrossRef]
- Mohokum, M.; Schulein, S.; Skwara, A. The validity of rasterstereography: A systematic review. Orthop. Rev. 2015, 7, 68–73. [Google Scholar]
- Knott, P.; Sturm, P.; Lonner, B.; Cahill, P.; Betsch, M.; McCarthy, R.; Kelly, M.; Lenke, L.; Betz, R. Multicenter comparison of 3D spinal measurements using surface topography with those from conventional radiography. Spine Deform. 2016, 4, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Knott, P.; Mardjetko, S.; Rollet, M.; Baute, S.; Riemenschneider, M.; Muncie, L. Evaluation of the reproducibility of the formetric 4D measurements for scoliosis. Scoliosis 2010, 5, O10. [Google Scholar] [CrossRef]
- Drerup, B.; Hierholzer, E. Automatic localization of anatomical landmarks on the back surface and construction of a body-fixed coordinate system. J. Biomech. 1987, 20, 961–970. [Google Scholar] [CrossRef] [PubMed]
- Liljenqvist, U.; Halm, H.; Hierholzer, E.; Drerup, B.; Weiland, M. 3-dimensional surface measurement of spinal deformities with video rasterstereography. Z. Orthop. Ihre Grenzgeb. 1998, 136, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Bendix, T.; Biering-Sørensen, F. Posture of the trunk when sitting on forward inclining seats. Scand. J. Rehabil. Med. 1983, 15, 197–203. [Google Scholar]
- Kim, J.W.; Kang, M.H.; Noh, K.H.; Kim, J.S.; Oh, J.S. A sloped seat wedge can change the kinematics of the lumbar spine of seated workers with limited hip flexion. J. Phys. Ther. Sci. 2014, 26, 1173–1175. [Google Scholar] [CrossRef][Green Version]
- Rothschild, D.; Ng, S.Y.; Ng, Y.L.E. Indications of sole lift and foot orthoses in the management of mild idiopathic scoliosis-A review. J. Phys. Ther. Sci. 2020, 32, 251–256. [Google Scholar] [CrossRef]
- Betsch, M.; Wild, M.; Grosse, B.; Rapp, W.; Horstmann, T. The effect of simulating leg length inequality on spinal posture and pelvic position: A dynamic rasterstereographic analysis. Eur. Spine J. 2012, 21, 691–697. [Google Scholar] [CrossRef]
- Grivas, T.B.; Angouris, K.; Chandrinos, M.; Kechagias, V. Truncal changes in children with mild limb length inequality: A surface topography study. Scoliosis Spinal Disord. 2018, 13, 27. [Google Scholar] [CrossRef]
- Kwon, Y.J.; Song, M.; Baek, I.H.; Lee, T. The effect of simulating a leg-length discrepancy on pelvic position and spinal posture. J. Phys. Ther. Sci. 2015, 27, 689–691. [Google Scholar] [CrossRef]
- Young, R.S.; Andrew, P.D.; Cummings, G.S. Effect of simulating leg length inequality on pelvic torsion and trunk mobility. Gait Posture 2000, 11, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Betsch, M.; Rapp, W.; Przibylla, A.; Jungbluth, P.; Hakimi, M.; Schneppendahl, J.; Thelen, S.; Wild, M. Determination of the amount of leg length inequality that alters spinal posture in healthy subjects using rasterstereography. Eur. Spine J. 2013, 22, 1354–1361. [Google Scholar] [CrossRef] [PubMed]
- Lehnert-Schroth, C.; Auner-Gröbl, P. Dreidimensionale Skoliosebehandlung: Atmungs-Orthopädie System Schroth: Ein physiotherapeutisches Konzept zur Verbesserung von Wirbelsäulenverkrümmungen, 9th ed.; Elsevier GmbH: München, Germany, 2021. [Google Scholar]
- Schumann, K.; Püschel, I.; Maier-Hennes, A.; Weiss, H.R. Postural changes in patients with scoliosis in different postural positions revealed by surface topography. Stud. Health Technol. Inform. 2008, 140, 140–143. [Google Scholar]
- Canales, J.; Cordás, T.; Cavalcante, A.; Moreno, R. Posture and body image in individuals with major depressive disorder: A controlled study. Rev. Bras. Psiquiatr. 2010, 32, 375–380. [Google Scholar] [CrossRef] [PubMed]
- Popescu, D. Bildgebende strahlungsfreie Vermessung der Rotation der Wirbelkörper idiopathischer Skoliosen: Analyse und Vergleich von optischen Wirbelsäulenvermessungen per Videorasterstereografie (Formetric 3D) versus offener Magnetresonanztomografie (MRT) im Stehen. Ph.D. Thesis, Charité—Universitätsmedizin Berlin, Berlin, Germany, 2020. [Google Scholar]
- Park, J.H.; Jeon, H.S.; Park, H.W. Effects of the Schroth exercise on idiopathic scoliosis: A meta-analysis. Eur. J. Phys. Rehab. Med. 2018, 54, 440–449. [Google Scholar] [CrossRef]
- van den Bogaart, M.; van Royen, B.J.; Haanstra, T.M.; de Kleuver, M.; Faraj, S.S.A. Predictive factors for brace treatment outcome in adolescent idiopathic scoliosis: A best-evidence synthesis. Eur. Spine J. 2019, 28, 511–525. [Google Scholar] [CrossRef]
- de Mauroy, J.C.; Lecante, C.; Barral, F.; Pourret, S. Prospective study and new concepts based on scoliosis detorsion of the first 225 early in-brace radiological results with the new Lyon brace: ARTbrace. Scoliosis 2014, 9, 19. [Google Scholar] [CrossRef][Green Version]
- Knott, P.; Techy, F.; Cotter, T.; Jansen, L.; Kove, P.; Loving, J.; Poletis, K.; Mardjetlko, S. Retrospective analysis of immediate in-brace correction of scoliosis attainable in patients with AIS: A SOSORT initiative. Scoliosis 2013, 8, O49. [Google Scholar] [CrossRef]
- Hamzaoglu, A.; Talu, U.; Tezer, M.; Mirzanli, C.; Domanic, U.; Goksan, S.B. Assessment of curve flexibility in adolescent idiopathic scoliosis. Spine 2005, 30, 1637–1642. [Google Scholar] [CrossRef]
- Gram, M.C.; Hasan, Z. The spinal curve in standing and sitting postures in children with idiopathic scoliosis. Spine 1999, 24, 169–177. [Google Scholar] [CrossRef]
- Negrini, S.; Aulisa, A.G.; Aulisa, L.; Circo, A.B.; de Mauroy, J.C.; Durmala, J.; Grivas, T.B.; Knott, P.; Kotwicki, T.; Maruyama, T.; et al. 2011 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis 2012, 7, 3. [Google Scholar] [CrossRef] [PubMed]
- Maruyama, T.; Takeshita, K. Surgical treatment of scoliosis: A review of techniques currently applied. Scoliosis 2008, 3, 6. [Google Scholar] [CrossRef] [PubMed]
- Stücker, R. Die wachsende Wirbelsäule. Der Orthopäde 2016, 45, 534–539. [Google Scholar] [CrossRef] [PubMed]
- Ponseti, I.V.; Friedman, B. Prognosis in idiopathic scoliosis. J. Bone Joint Surg. Am. 1950, 32a, 381–395. [Google Scholar] [CrossRef] [PubMed]
- Suh, S.-W.; Modi, H.N.; Yang, J.-H.; Hong, J.-Y. Idiopathic scoliosis in Korean schoolchildren: A prospective screening study of over 1 million children. Eur. Spine J. 2011, 20, 1087–1094. [Google Scholar] [CrossRef] [PubMed]
- DIERS International GmbH. Gebrauchsanweisung DIERS formetric III; DIERS International GmbH: Wiesbaden, Germany, 2015. [Google Scholar]
- Sangeux, M.; Marin, F.; Charleux, F.; Dürselen, L.; Ho Ba Tho, M.C. Quantification of the 3D relative movement of external marker sets vs. bones based on magnetic resonance imaging. Clin. Biomech. 2006, 21, 984–991. [Google Scholar] [CrossRef]
- Stagni, R.; Fantozzi, S.; Cappello, A.; Leardini, A. Quantification of soft tissue artefact in motion analysis by combining 3D fluoroscopy and stereophotogrammetry: A study on two subjects. Clin. Biomech. 2005, 20, 320–329. [Google Scholar] [CrossRef]




| Mean ± SD Total | Min/Max | Sex | Mean ± SD by Sex | |
|---|---|---|---|---|
| size (cm) | 167.1 ± 8.3 | 147/190 | male | 179.6 ± 8.8 |
| female | 165.5 ± 6.8 | |||
| weight (kg) | 55.9 ± 9.6 | 38/84 | male | 63.1 ± 11.8 |
| female | 55.0 ± 8.9 | |||
| BMI (kg/m2) | 20.0 ± 2.8 | 16.2/29.36 | male | 19.5 ± 3.4 |
| female | 20.0 ± 2.7 | |||
| age (years) | 15.1 ± 1.6 | 11.7/18.8 | male | 16.0 ± 1.4 |
| female | 15.0 ± 1.6 |
| Severity | Number (Percentage Share) | Scoliosis Type | Number (Percentage Share) |
|---|---|---|---|
| low | 24 (24.2%) | thoracic | 17 (17.2%) |
| moderate | 55 (55.6%) | thoraco-lumbar | 17 (17.2%) |
| severe | 20 (20.2%) | lumbar | 7 (7.1%) |
| combined (s-form) | 58 (58.6%) |
| Scoliosis Angle (°) | Lateral Deviation RMS (mm) | |||||
|---|---|---|---|---|---|---|
| Level Seat | Optimal Correction | Change (Percentage Share) | Level Seat | Optimal Correction | Change (Percentage Share) | |
| Severity | ||||||
| low | 19.3 ± 7.1 | 12.8 ± 5.2 | 6.5 (33.7%) | 7.4 ± 3.4 | 4.7 ± 2.9 | 2.7 (36.5%) |
| moderate | 24.4 ± 10.0 | 18.4 ± 8.3 | 6.0 (24.6%) | 10.0 ± 5.2 | 7.0 ± 4.6 | 3.0 (30.0%) |
| severe | 37.1 ± 8.5 | 27.5 ± 9.1 | 9.6 (25.9%) | 14.1 ± 4.8 | 9.5 ± 4.3 | 4.6 (32.6%) |
| Scoliosis type | ||||||
| thoracic | 35.2 ± 11.7 | 27.2 ± 8.8 | 8.0 (22.7%) | 15.7 ± 6.0 | 11.7 ± 5.8 | 4.0 (25.5%) |
| thoraco-lumbar | 21.9 ± 7.2 | 15.2 ± 6.0 | 6.7 (30.6%) | 8.0 ± 3.8 | 5.5 ± 2.6 | 2.5 (31.3%) |
| lumbar | 18.6 ± 7.2 | 10.3 ± 3.4 | 8.3 (44.6%) | 6.4 ± 4.1 | 3.1 ± 2.0 | 3.3 (51.6%) |
| combined (s-form) | 24.9 ± 10.3 | 18.6 ± 8.9 | 6.3 (25.6%) | 9.7 ± 4.3 | 6.4 ± 3.6 | 3.3 (34.0%) |
| Mean NRS Value | |||||
|---|---|---|---|---|---|
| Level Seat | Optimal Correction of Scoliosis Angle | Change (Percentage Share) | Optimal Correction Lateral Deviation RMS | Change (Percentage Share) | |
| Severity | |||||
| low | 1.9 ± 1.6 | 4.2 ± 2.7 | 2.3 (121.1%) | 4.3 ± 2.6 | 2.4 (126.3%) |
| moderate | 2.3 ± 1.7 | 3.4 ± 2.3 | 1.1 (47.8%) | 3.7 ± 2.4 | 1.4 (60.9%) |
| severe | 2.6 ± 1.5 | 3.4 ± 2.6 | 0.8 (30.8%) | 3.2 ± 2.2 | 0.6 (23.1%) |
| Scoliosis type | |||||
| thoracic | 1.9 ± 1.2 | 4.4 ± 2.3 | 2.5 (131.6%) | 4.0 ± 2.3 | 2.1 (110.5%) |
| thoraco-lumbar | 1.8 ± 1.2 | 3.7 ± 2.2 | 1.9 (105.6%) | 3.8 ± 2.1 | 2.0 (111.1%) |
| lumbar | 1.9 ± 1.8 | 2.7 ± 2.1 | 0.8 (42.1%) | 2.7 ± 2.1 | 0.8 (42.1%) |
| combined (s-form) | 2.5 ± 1.8 | 3.4 ± 2.6 | 0.9 (36.0%) | 3.8 ± 2.6 | 1.3 (52.0%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Feustel, A.; Konradi, J.; Wolf, C.; Huthwelker, J.; Westphal, R.; Chow, D.; Hülstrunk, C.; Drees, P.; Betz, U. Influence of Lateral Sitting Wedges on the Rasterstereographically Measured Scoliosis Angle in Patients Aged 10–18 Years with Adolescent Idiopathic Scoliosis. Bioengineering 2023, 10, 1086. https://doi.org/10.3390/bioengineering10091086
Feustel A, Konradi J, Wolf C, Huthwelker J, Westphal R, Chow D, Hülstrunk C, Drees P, Betz U. Influence of Lateral Sitting Wedges on the Rasterstereographically Measured Scoliosis Angle in Patients Aged 10–18 Years with Adolescent Idiopathic Scoliosis. Bioengineering. 2023; 10(9):1086. https://doi.org/10.3390/bioengineering10091086
Chicago/Turabian StyleFeustel, Andreas, Jürgen Konradi, Claudia Wolf, Janine Huthwelker, Ruben Westphal, Daniel Chow, Christian Hülstrunk, Philipp Drees, and Ulrich Betz. 2023. "Influence of Lateral Sitting Wedges on the Rasterstereographically Measured Scoliosis Angle in Patients Aged 10–18 Years with Adolescent Idiopathic Scoliosis" Bioengineering 10, no. 9: 1086. https://doi.org/10.3390/bioengineering10091086
APA StyleFeustel, A., Konradi, J., Wolf, C., Huthwelker, J., Westphal, R., Chow, D., Hülstrunk, C., Drees, P., & Betz, U. (2023). Influence of Lateral Sitting Wedges on the Rasterstereographically Measured Scoliosis Angle in Patients Aged 10–18 Years with Adolescent Idiopathic Scoliosis. Bioengineering, 10(9), 1086. https://doi.org/10.3390/bioengineering10091086








