Monitoring Resistance Training in Real Time with Wearable Technology: Current Applications and Future Directions
Abstract
:1. Introduction
2. General Principles of Resistance Training
2.1. Progressive Overload
2.2. Specificity
2.3. Variation
2.4. Individualization
2.5. Proper Form and Technique
2.6. Rest and Recovery
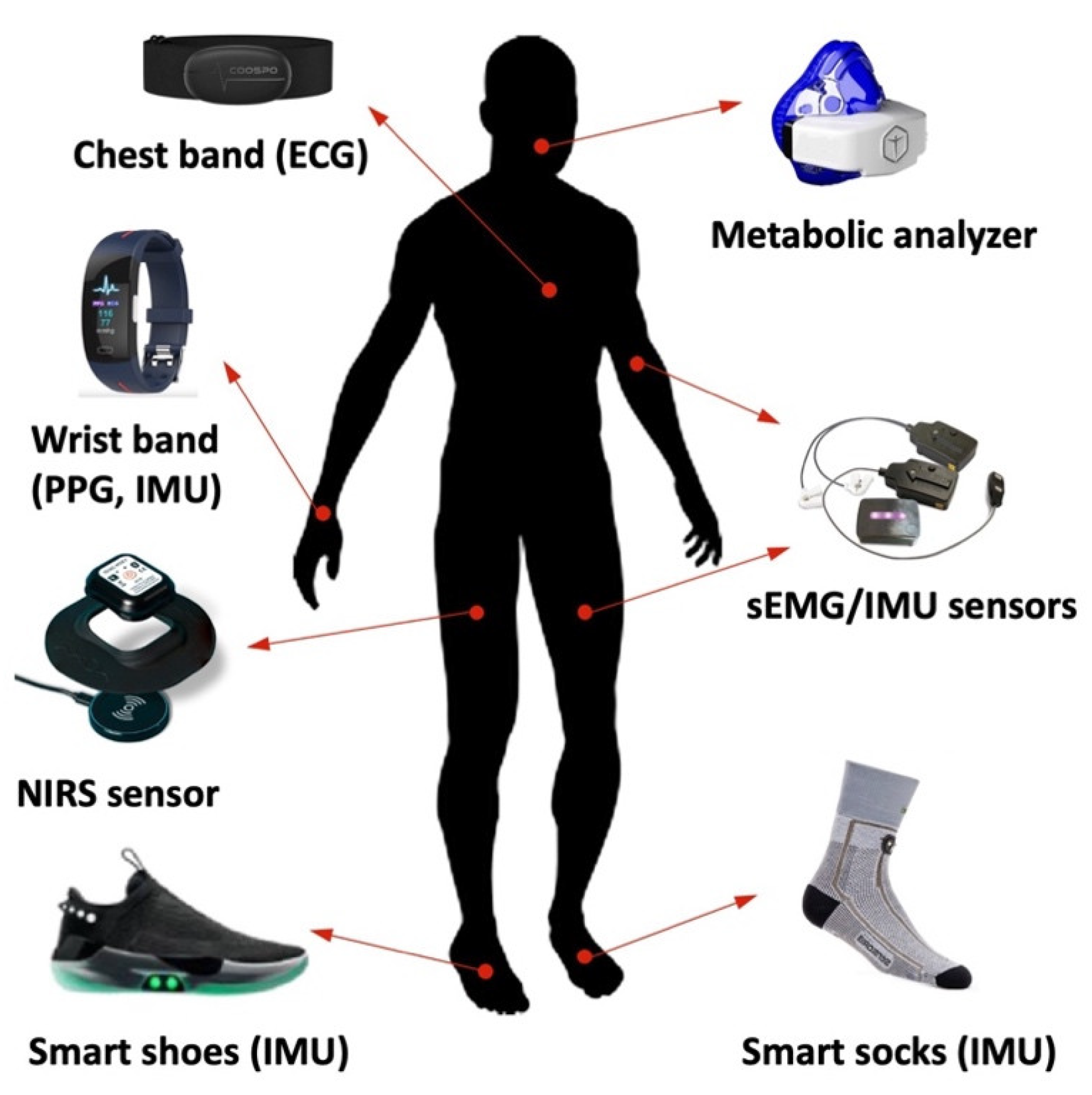
3. Wearable Devices for Measuring Physiological Parameters during Training
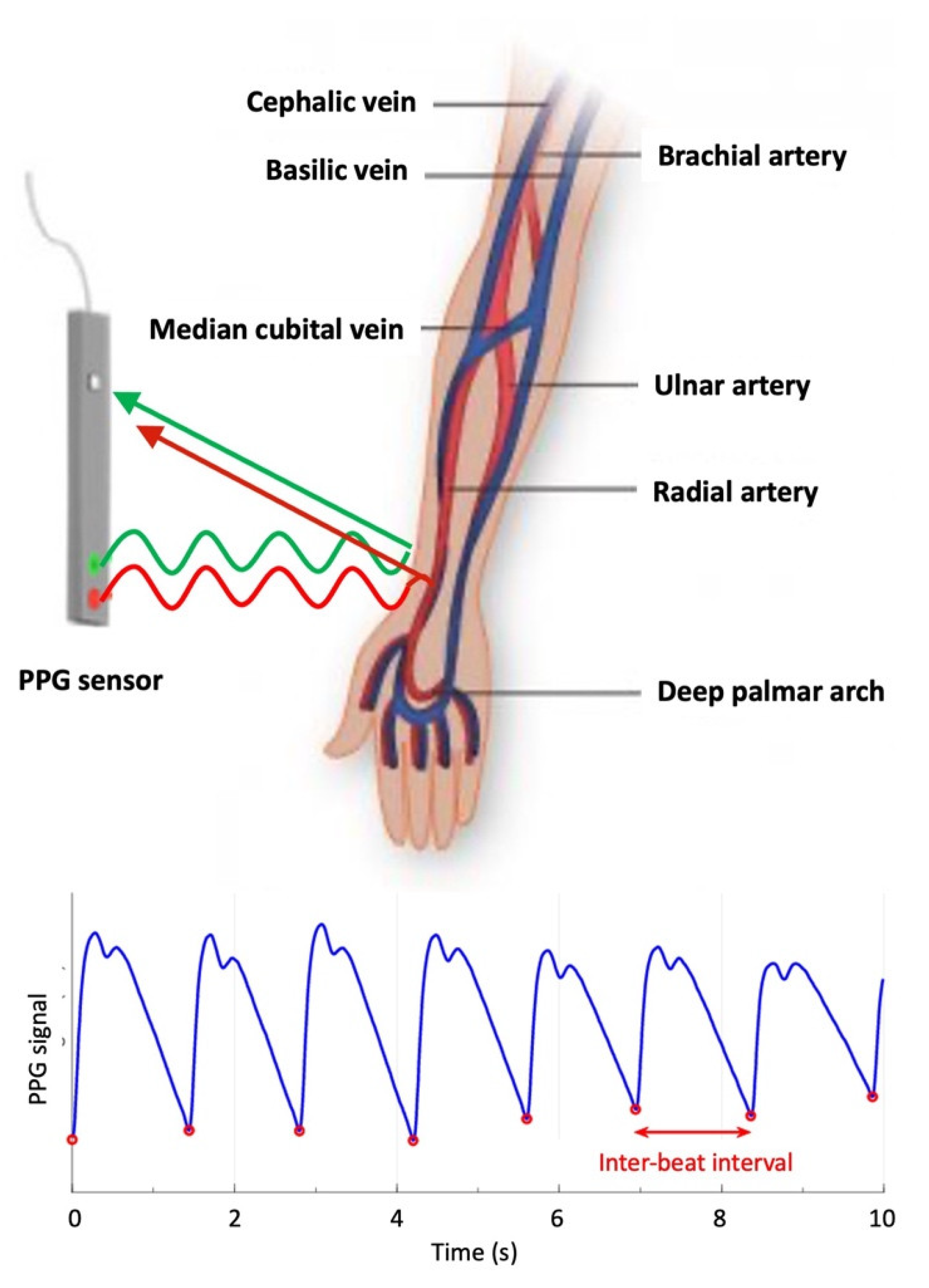
3.1. Photoplethysmography for Heart Rate Monitoring
3.2. Electrocardiography to Track Cardiac Output and Heart Rate Variability
3.3. Electromyography to Monitor Muscle Fatigue Conditions during Exercise
3.4. Near-Infrared Spectroscopy to Measure Changes in Oxygen Saturation in Muscles
3.5. Portable Metabolic Analyzers for Assessing Energy Expenditure and Metabolic Rate
4. Wearable Devices for Measuring Biomechanical Parameters during Training
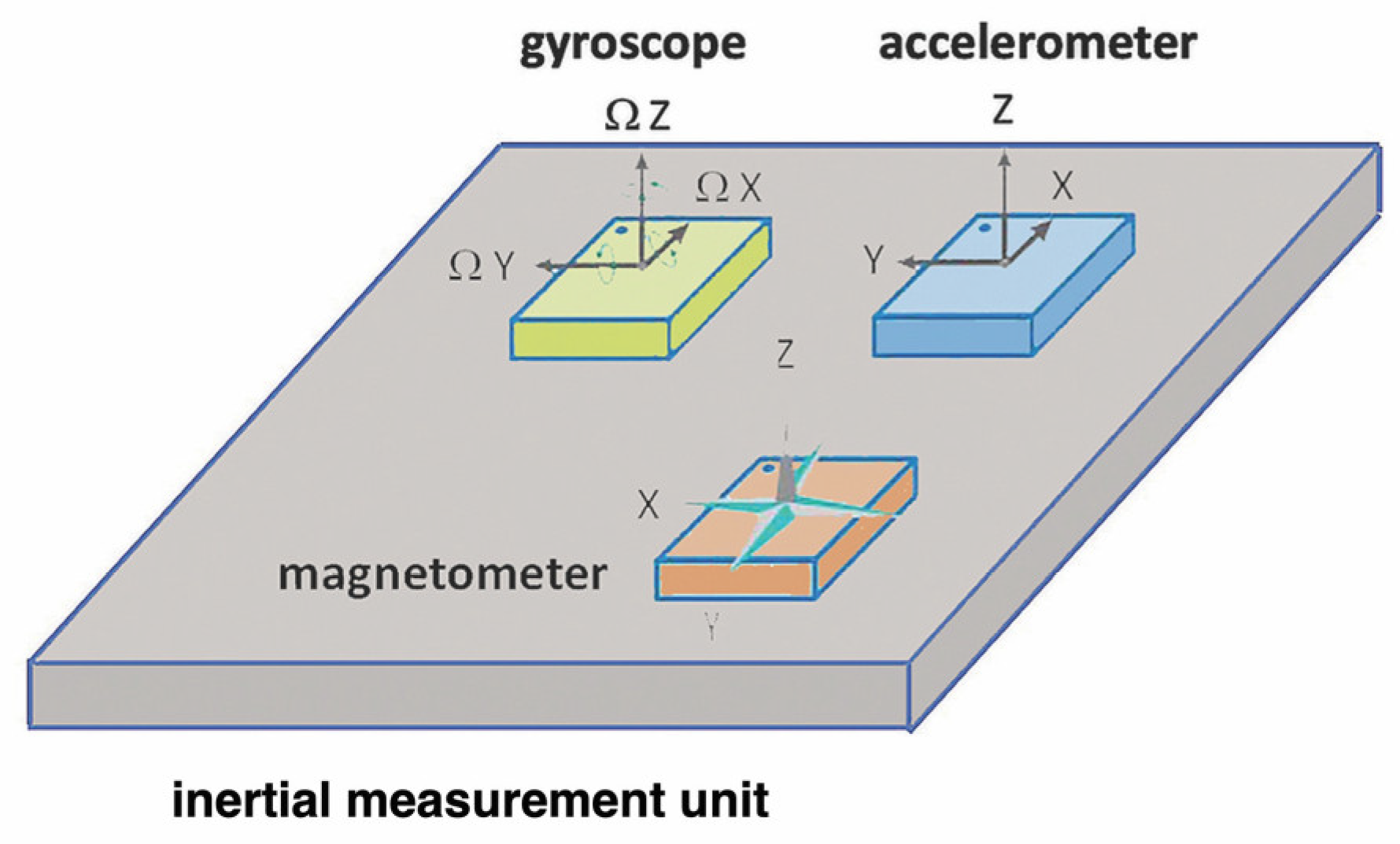
4.1. Inertial Measurement Units (IMUs) for Tracking Movement Patterns and Velocity
4.2. Force Sensors for Measuring the Amount of Force Generated
4.3. Pressure Sensors for Assessing Foot Pressure and Balance
5. Applications of Wearables in Resistance Training Research
5.1. Assessment of Training Load and Fatigue
5.2. Optimization of Exercise Technique and Performance
5.3. Monitoring of Recovery and Injury Prevention
6. Limitations of Wearable Technology in Resistance Training Research
6.1. Accuracy and Reliability of Measurements
6.2. Validation and Standardization of Wearable Technology
6.3. Ethical Considerations and Privacy Concerns
7. Conclusions and Future Perspectives
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Carvalho, L.; Junior, R.M.; Barreira, J.; Schoenfeld, B.J.; Orazem, J.; Barroso, R. Muscle Hypertrophy and Strength Gains after Resistance Training with Different Volume-Matched Loads: A Systematic Review and Meta-Analysis. Appl. Physiol. Nutr. Metab. 2022, 47, 357–368. [Google Scholar] [CrossRef]
- Westcott, W.L. Resistance Training Is Medicine: Effects of Strength Training on Health. Curr. Sports Med. Rep. 2012, 11, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Sayer, A.A. Sarcopenia. Lancet 2019, 393, 2636–2646. [Google Scholar] [CrossRef] [PubMed]
- Yasuda, T. Selected Methods of Resistance Training for Prevention and Treatment of Sarcopenia. Cells 2022, 11, 1389. [Google Scholar] [CrossRef]
- Schoenfeld, B.J.; Grgic, J.; Ogborn, D.; Krieger, J.W. Strength and Hypertrophy Adaptations Between Low- vs. High-Load Resistance Training: A Systematic Review and Meta-Analysis. J. Strength Cond. Res. 2017, 31, 3508–3523. [Google Scholar] [CrossRef]
- Sperlich, B.; Aminian, K.; Düking, P.; Holmberg, H.-C. Editorial: Wearable Sensor Technology for Monitoring Training Load and Health in the Athletic Population. Front. Physiol. 2019, 10, 1520. [Google Scholar] [CrossRef]
- Dunn, J.; Runge, R.; Snyder, M. Wearables and the Medical Revolution. Per. Med. 2018, 15, 429–448. [Google Scholar] [CrossRef] [PubMed]
- Mcleod, J.C.; Stokes, T.; Phillips, S.M. Resistance Exercise Training as a Primary Countermeasure to Age-Related Chronic Disease. Front. Physiol. 2019, 10, 645. [Google Scholar] [CrossRef]
- Martins, A.D.; Fernandes, O.; Pereira, A.; Oliveira, R.; Alderete Goñi, F.D.; Leite, N.J.C.; Brito, J.P. The Effects of High-Speed Resistance Training on Health Outcomes in Independent Older Adults: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 5390. [Google Scholar] [CrossRef]
- Khodadad Kashi, S.; Mirzazadeh, Z.S.; Saatchian, V. A Systematic Review and Meta-Analysis of Resistance Training on Quality of Life, Depression, Muscle Strength, and Functional Exercise Capacity in Older Adults Aged 60 Years or More. Biol. Res. Nurs. 2023, 25, 88–106. [Google Scholar] [CrossRef]
- Currier, B.S.; Mcleod, J.C.; Banfield, L.; Beyene, J.; Welton, N.J.; D’Souza, A.C.; Keogh, J.A.J.; Lin, L.; Coletta, G.; Yang, A.; et al. Resistance Training Prescription for Muscle Strength and Hypertrophy in Healthy Adults: A Systematic Review and Bayesian Network Meta-Analysis. Br. J. Sports Med. 2023. Online. [Google Scholar] [CrossRef] [PubMed]
- Schoenfeld, B.J.; Ratamess, N.A.; Peterson, M.D.; Contreras, B.; Tiryaki-Sonmez, G. Influence of Resistance Training Frequency on Muscular Adaptations in Well-Trained Men. J. Strength Cond. Res. 2015, 29, 1821–1829. [Google Scholar] [CrossRef] [PubMed]
- Morrissey, M.C.; Harman, E.A.; Johnson, M.J. Resistance Training Modes: Specificity and Effectiveness. Med. Sci. Sports Exerc. 1995, 27, 648–660. [Google Scholar] [CrossRef] [PubMed]
- Kraemer, W.J.; Ratamess, N.A. Fundamentals of Resistance Training: Progression and Exercise Prescription. Med. Sci. Sports Exerc. 2004, 36, 674–688. [Google Scholar] [CrossRef]
- Skorski, S.; Mujika, I.; Bosquet, L.; Meeusen, R.; Coutts, A.J.; Meyer, T. The Temporal Relationship Between Exercise, Recovery Processes, and Changes in Performance. Int. J. Sports Physiol. Perform. 2019, 14, 1015–1021. [Google Scholar] [CrossRef]
- Kellmann, M.; Bertollo, M.; Bosquet, L.; Brink, M.; Coutts, A.J.; Duffield, R.; Erlacher, D.; Halson, S.L.; Hecksteden, A.; Heidari, J.; et al. Recovery and Performance in Sport: Consensus Statement. Int. J. Sports Physiol. Perform. 2018, 13, 240–245. [Google Scholar] [CrossRef]
- Torous, J.; Stern, A.D.; Bourgeois, F.T. Regulatory Considerations to Keep Pace with Innovation in Digital Health Products. NPJ Digit. Med. 2022, 5, 121. [Google Scholar] [CrossRef]
- Awad, S.; Aljuburi, L.; Lumsden, R.S.; Mpandzou, M.; Marinus, R. Connected Health in US, EU, and China: Opportunities to Accelerate Regulation of Connected Health Technologies to Optimize Their Role in Medicines Development. Front. Med. 2023, 10, 1248912. [Google Scholar] [CrossRef]
- Baskan, A.; Goncu-Berk, G. User Experience of Wearable Technologies: A Comparative Analysis of Textile-Based and Accessory-Based Wearable Products. Appl. Sci. 2022, 12, 11154. [Google Scholar] [CrossRef]
- Gupta, K.; Sinhal, R.; Badhiye, S.S. Remote Photoplethysmography-Based Human Vital Sign Prediction Using Cyclical Algorithm. J. Biophotonics 2023, e202300286. [Google Scholar] [CrossRef]
- Correia, B.; Dias, N.; Costa, P.; Pêgo, J.M. Validation of a Wireless Bluetooth Photoplethysmography Sensor Used on the Earlobe for Monitoring Heart Rate Variability Features during a Stress-Inducing Mental Task in Healthy Individuals. Sensors 2020, 20, 3905. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Weaver, R.G.; Armstrong, B.; Burkart, S.; Zhang, S.; Beets, M.W. Validity of Wrist-Worn Photoplethysmography Devices to Measure Heart Rate: A Systematic Review and Meta-Analysis. J. Sports Sci. 2020, 38, 2021–2034. [Google Scholar] [CrossRef] [PubMed]
- Charlton, P.H.; Kyriacou, P.; Mant, J.; Alastruey, J. Acquiring Wearable Photoplethysmography Data in Daily Life: The PPG Diary Pilot Study. Eng. Proc. 2020, 2, 80. [Google Scholar] [CrossRef]
- Kinnunen, H.; Häkkinen, K.; Schumann, M.; Karavirta, L.; Westerterp, K.R.; Kyröläinen, H. Training-Induced Changes in Daily Energy Expenditure: Methodological Evaluation Using Wrist-Worn Accelerometer, Heart Rate Monitor, and Doubly Labeled Water Technique. PLoS ONE 2019, 14, 0219563. [Google Scholar] [CrossRef]
- Wulterkens, B.M.; Fonseca, P.; Hermans, L.W.A.; Ross, M.; Cerny, A.; Anderer, P.; Long, X.; van Dijk, J.P.; Vandenbussche, N.; Pillen, S.; et al. It Is All in the Wrist: Wearable Sleep Staging in a Clinical Population versus Reference Polysomnography. Nat. Sci. Sleep 2021, 13, 885–897. [Google Scholar] [CrossRef]
- Liu, P.-K.; Ting, N.; Chiu, H.-C.; Lin, Y.-C.; Liu, Y.-T.; Ku, B.-W.; Lee, P.-L. Validation of Photoplethysmography and Acceleration-Based Sleep Staging in a Community Sample: Comparison with Polysomnography and Actiwatch. J. Clin. Sleep Med. 2023. [Google Scholar] [CrossRef]
- Chennaoui, M.; Arnal, P.J.; Sauvet, F.; Léger, D. Sleep and Exercise: A Reciprocal Issue? Sleep Med. Rev. 2015, 20, 59–72. [Google Scholar] [CrossRef]
- Stein, P.K.; Pu, Y. Heart Rate Variability, Sleep and Sleep Disorders. Sleep Med. Rev. 2012, 16, 47–66. [Google Scholar] [CrossRef]
- Wang, J.-J.; Liu, S.-H.; Tsai, C.-H.; Manousakas, I.; Zhu, X.; Lee, T.-L. Signal Quality Analysis of Single-Arm Electrocardiography. Sensors 2023, 23, 5818. [Google Scholar] [CrossRef]
- Lee, M.H.; Jang, G.Y.; Kim, Y.E.; Yoo, P.J.; Wi, H.; Oh, T.I.; Woo, E.J. Portable Multi-Parameter Electrical Impedance Tomography for Sleep Apnea and Hypoventilation Monitoring: Feasibility Study. Physiol. Meas. 2018, 39, 124004. [Google Scholar] [CrossRef]
- Dobrzynski, H.; Anderson, R.H.; Atkinson, A.; Borbas, Z.; D’Souza, A.; Fraser, J.F.; Inada, S.; Logantha, S.J.R.J.; Monfredi, O.; Morris, G.M.; et al. Structure, Function and Clinical Relevance of the Cardiac Conduction System, Including the Atrioventricular Ring and Outflow Tract Tissues. Pharmacol. Ther. 2013, 139, 260–288. [Google Scholar] [CrossRef]
- Bayram, M.; Yancy, C.W. Transthoracic Impedance Cardiography: A Noninvasive Method of Hemodynamic Assessment. Heart Fail. Clin. 2009, 5, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Merghani, A.; Mont, L. Exercise and the Heart: The Good, the Bad, and the Ugly. Eur. Heart J. 2015, 36, 1445–1453. [Google Scholar] [CrossRef]
- Pingitore, A.; Peruzzi, M.; Clarich, S.C.; Palamà, Z.; Sciarra, L.; Cavarretta, E. An Overview of the Electrocardiographic Monitoring Devices in Sports Cardiology: Between Present and Future. Clin. Cardiol. 2023, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Xhyheri, B.; Manfrini, O.; Mazzolini, M.; Pizzi, C.; Bugiardini, R. Heart Rate Variability Today. Prog. Cardiovasc. Dis. 2012, 55, 321–331. [Google Scholar] [CrossRef]
- Rogers, B.; Gronwald, T. Fractal Correlation Properties of Heart Rate Variability as a Biomarker for Intensity Distribution and Training Prescription in Endurance Exercise: An Update. Front. Physiol. 2022, 13, 879071. [Google Scholar] [CrossRef] [PubMed]
- De Luca, C.J.; Adam, A.; Wotiz, R.; Gilmore, L.D.; Nawab, S.H. Decomposition of Surface EMG Signals. J. Neurophysiol. 2006, 96, 1646–1657. [Google Scholar] [CrossRef]
- Bartuzi, P.; Roman-Liu, D. Assessment of Muscle Load and Fatigue with the Usage of Frequency and Time-Frequency Analysis of the EMG Signal. Acta Bioeng. Biomech. 2014, 16, 31–39. [Google Scholar]
- Budinger, T.F. Biomonitoring with Wireless Communications. Annu. Rev. Biomed. Eng. 2003, 5, 383–412. [Google Scholar] [CrossRef]
- Örücü, S.; Selek, M. Design and Validation of Multichannel Wireless Wearable SEMG System for Real-Time Training Performance Monitoring. J. Healthc. Eng. 2019, 2019, 4580645. [Google Scholar] [CrossRef]
- Liang, Z.; Wang, X.; Guo, J.; Ye, Y.; Zhang, H.; Xie, L.; Tao, K.; Zeng, W.; Yin, E.; Ji, B. A Wireless, High-Quality, Soft and Portable Wrist-Worn System for SEMG Signal Detection. Micromachines 2023, 14, 1085. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Correa, M.; Cruz-Ortiz, D. Low-Cost Wearable Band Sensors of Surface Electromyography for Detecting Hand Movements. Sensors 2022, 22, 5931. [Google Scholar] [CrossRef] [PubMed]
- Klusiewicz, A.; Rębiś, K.; Ozimek, M.; Czaplicki, A. The Use of Muscle Near-Infrared Spectroscopy (NIRS) to Assess the Aerobic Training Loads of World-Class Rowers. Biol. Sport 2021, 38, 713–719. [Google Scholar] [CrossRef]
- Paulauskas, R.; Nekriošius, R.; Dadelienė, R.; Sousa, A.; Figueira, B. Muscle Oxygenation Measured with Near-Infrared Spectroscopy Following Different Intermittent Training Protocols in a World-Class Kayaker—A Case Study. Sensors 2022, 22, 8238. [Google Scholar] [CrossRef] [PubMed]
- Sanni, A.A.; McCully, K.K. Interpretation of Near-Infrared Spectroscopy (NIRS) Signals in Skeletal Muscle. J. Funct. Morphol. Kinesiol. 2019, 4, 28. [Google Scholar] [CrossRef]
- Benni, P.B.; MacLeod, D.; Ikeda, K.; Lin, H.-M. A Validation Method for Near-Infrared Spectroscopy Based Tissue Oximeters for Cerebral and Somatic Tissue Oxygen Saturation Measurements. J. Clin. Monit. Comput. 2018, 32, 269–284. [Google Scholar] [CrossRef]
- Miranda-Fuentes, C.; Chirosa-Ríos, L.J.; Guisado-Requena, I.M.; Delgado-Floody, P.; Jerez-Mayorga, D. Changes in Muscle Oxygen Saturation Measured Using Wireless Near-Infrared Spectroscopy in Resistance Training: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 4293. [Google Scholar] [CrossRef]
- Hodges, L.D.; Brodie, D.A.; Bromley, P.D. Validity and Reliability of Selected Commercially Available Metabolic Analyzer Systems. Scand. J. Med. Sci. Sports 2005, 15, 271–279. [Google Scholar] [CrossRef]
- Sordi, A.F.; Mariano, I.R.; Silva, B.F.; Magnani Branco, B.H. Resting Metabolic Rate in Bodybuilding: Differences between Indirect Calorimetry and Predictive Equations. Clin. Nutr. ESPEN 2022, 51, 239–245. [Google Scholar] [CrossRef]
- Robles-González, L.; Gutiérrez-Hellín, J.; Aguilar-Navarro, M.; Ruiz-Moreno, C.; Muñoz, A.; Del-Coso, J.; R Ruiz, J.; Amaro-Gahete, F.J. Inter-Day Reliability of Resting Metabolic Rate and Maximal Fat Oxidation during Exercise in Healthy Men Using the Ergostik Gas Analyzer. Nutrients 2021, 13, 4308. [Google Scholar] [CrossRef]
- Tsekouras, Y.E.; Tambalis, K.D.; Sarras, S.E.; Antoniou, A.K.; Kokkinos, P.; Sidossis, L.S. Validity and Reliability of the New Portable Metabolic Analyzer PNOE. Front. Sports Act. Living 2019, 1, 24. [Google Scholar] [CrossRef] [PubMed]
- Yao, P.; Guo, W.; Sheng, X.; Zhang, D.; Zhu, X. A Portable Multi-Channel Wireless NIRS Device for Muscle Activity Real-Time Monitoring. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2014, 2014, 3719–3722. [Google Scholar] [CrossRef] [PubMed]
- Seo, H.-C.; Shin, D.; Leem, C.H.; Joo, S. Development of a Portable Respiratory Gas Analyzer for Measuring Indirect Resting Energy Expenditure (REE). J. Healthc. Eng. 2021, 2021, 8870749. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.; Akhundov, R.; James, C.; Edwards, S.; Snodgrass, S.J. Variations in Concurrent Validity of Two Independent Inertial Measurement Units Compared to Gold Standard for Upper Body Posture during Computerised Device Use. Sensors 2023, 23, 6761. [Google Scholar] [CrossRef]
- Zhang, H.; Song, Y.; Li, C.; Dou, Y.; Wang, D.; Wu, Y.; Chen, X.; Liu, D. Validation of a Wearable System for Lower Extremity Assessment. Orthop. Surg. 2023, 9999, 9999. [Google Scholar] [CrossRef]
- Samatas, G.G.; Pachidis, T.P. Inertial Measurement Units (IMUs) in Mobile Robots over the Last Five Years: A Review. Designs 2022, 6, 17. [Google Scholar] [CrossRef]
- Sabatini, A.M. Estimating Three-Dimensional Orientation of Human Body Parts by Inertial/Magnetic Sensing. Sensors 2011, 11, 1489–1525. [Google Scholar] [CrossRef]
- Yi, C.; Ma, J.; Guo, H.; Han, J.; Gao, H.; Jiang, F.; Yang, C. Estimating Three-Dimensional Body Orientation Based on an Improved Complementary Filter for Human Motion Tracking. Sensors 2018, 18, 3765. [Google Scholar] [CrossRef]
- Hoang, T.; Shiao, Y. New Method for Reduced-Number IMU Estimation in Observing Human Joint Motion. Sensors 2023, 23, 5712. [Google Scholar] [CrossRef]
- Hernández, A.L.; Barrera Cortés, M.C.; Barón, A.Á.; TéllezTinjacá, L.A.; Guío, Á.H.A. Competitive Advantage of Wearable Technology in Sports Training. Wearable Technol. 2022, 3, 47. [Google Scholar] [CrossRef]
- Sander, J.; Kumme, R. Comparison of Force Measuring Devices with Static and Continuous Loading. Meas. Sens. 2021, 18, 100241. [Google Scholar] [CrossRef]
- Jiang, Y.; Wang, D.; Ying, J.; Chu, P.; Qian, Y.; Chen, W. Design and Preliminary Validation of Individual Customized Insole for Adults with Flexible Flatfeet Based on the Plantar Pressure Redistribution. Sensors 2021, 21, 1780. [Google Scholar] [CrossRef] [PubMed]
- Lambrich, J.; Hagen, M.; Schwiertz, G.; Muehlbauer, T. Concurrent Validity and Test-Retest Reliability of Pressure-Detecting Insoles for Static and Dynamic Movements in Healthy Young Adults. Sensors 2023, 23, 4913. [Google Scholar] [CrossRef] [PubMed]
- Burch, K.; Doshi, S.; Chaudhari, A.; Thostenson, E.; Higginson, J. Estimating Ground Reaction Force with Novel Carbon Nanotube-Based Textile Insole Pressure Sensors. Wearable Technol. 2023, 4, E8. [Google Scholar] [CrossRef] [PubMed]
- Rivera, C.E. Core and Lumbopelvic Stabilization in Runners. Phys. Med. Rehabil. Clin. N. Am. 2016, 27, 319–337. [Google Scholar] [CrossRef]
- Morin, P.; Muller, A.; Pontonnier, C.; Dumont, G. Evaluation of the Foot Center of Pressure Estimation from Pressure Insoles during Sidestep Cuts, Runs and Walks. Sensors 2022, 22, 5628. [Google Scholar] [CrossRef]
- Ludwig, M.; Hoffmann, K.; Endler, S.; Asteroth, A.; Wiemeyer, J. Measurement, Prediction, and Control of Individual Heart Rate Responses to Exercise-Basics and Options for Wearable Devices. Front. Physiol. 2018, 9, 778. [Google Scholar] [CrossRef]
- Elshafei, M.; Shihab, E. Towards Detecting Biceps Muscle Fatigue in Gym Activity Using Wearables. Sensors 2021, 21, 759. [Google Scholar] [CrossRef]
- Sorbie, G.G.; Williams, M.J.; Boyle, D.W.; Gray, A.; Brouner, J.; Gibson, N.; Baker, J.S.; Easton, C.; Ugbolue, U.C. Intra-Session and Inter-Day Reliability of the Myon 320 Electromyography System During Sub-Maximal Contractions. Front. Physiol. 2018, 9, 309. [Google Scholar] [CrossRef]
- Belbasis, A.; Fuss, F.K. Muscle Performance Investigated with a Novel Smart Compression Garment Based on Pressure Sensor Force Myography and Its Validation Against EMG. Front. Physiol. 2018, 9, 408. [Google Scholar] [CrossRef]
- Clemente, F.M.; Akyildiz, Z.; Pino-Ortega, J.; Rico-González, M. Validity and Reliability of the Inertial Measurement Unit for Barbell Velocity Assessments: A Systematic Review. Sensors 2021, 21, 2511. [Google Scholar] [CrossRef]
- Chambers, R.; Gabbett, T.J.; Cole, M.H.; Beard, A. The Use of Wearable Microsensors to Quantify Sport-Specific Movements. Sports Med. 2015, 45, 1065–1081. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Liu, X.; Xuan, B.; Zhang, J.; Liu, Z.; Zhang, Y. Selection of EMG Sensors Based on Motion Coordinated Analysis. Sensors 2021, 21, 1147. [Google Scholar] [CrossRef] [PubMed]
- Krzysztofik, M.; Wilk, M.; Wojdała, G.; Gołaś, A. Maximizing Muscle Hypertrophy: A Systematic Review of Advanced Resistance Training Techniques and Methods. Int. J. Environ. Res. Public Health 2019, 16, 4897. [Google Scholar] [CrossRef]
- Adesida, Y.; Papi, E.; McGregor, A.H. Exploring the Role of Wearable Technology in Sport Kinematics and Kinetics: A Systematic Review. Sensors 2019, 19, 1597. [Google Scholar] [CrossRef]
- Cao, R.; Azimi, I.; Sarhaddi, F.; Niela-Vilen, H.; Axelin, A.; Liljeberg, P.; Rahmani, A.M. Accuracy Assessment of Oura Ring Nocturnal Heart Rate and Heart Rate Variability in Comparison with Electrocardiography in Time and Frequency Domains: Comprehensive Analysis. J. Med. Internet Res. 2022, 24, e27487. [Google Scholar] [CrossRef]
- Altini, M.; Kinnunen, H. The Promise of Sleep: A Multi-Sensor Approach for Accurate Sleep Stage Detection Using the Oura Ring. Sensors 2021, 21, 4302. [Google Scholar] [CrossRef]
- Roberts, D.M.; Schade, M.M.; Mathew, G.M.; Gartenberg, D.; Buxton, O.M. Detecting Sleep Using Heart Rate and Motion Data from Multisensor Consumer-Grade Wearables, Relative to Wrist Actigraphy and Polysomnography. Sleep 2020, 43, zsaa045. [Google Scholar] [CrossRef] [PubMed]
- Ko, P.-R.T.; Kientz, J.A.; Choe, E.K.; Kay, M.; Landis, C.A.; Watson, N.F. Consumer Sleep Technologies: A Review of the Landscape. J. Clin. Sleep Med. 2015, 11, 1455–1461. [Google Scholar] [CrossRef]
- Henselmans, M.; Bjørnsen, T.; Hedderman, R.; Vårvik, F.T. The Effect of Carbohydrate Intake on Strength and Resistance Training Performance: A Systematic Review. Nutrients 2022, 14, 856. [Google Scholar] [CrossRef]
- Di Giminiani, R.; Cardinale, M.; Ferrari, M.; Quaresima, V. Validation of Fabric-Based Thigh-Wearable EMG Sensors and Oximetry for Monitoring Quadriceps Activity during Strength and Endurance Exercises. Sensors 2020, 20, 4664. [Google Scholar] [CrossRef]
- Li, R.T.; Kling, S.R.; Salata, M.J.; Cupp, S.A.; Sheehan, J.; Voos, J.E. Wearable Performance Devices in Sports Medicine. Sports Health 2016, 8, 74–78. [Google Scholar] [CrossRef]
- Tu, J.; Gao, W. Ethical Considerations of Wearable Technologies in Human Research. Adv. Healthc. Mater. 2021, 10, 2100127. [Google Scholar] [CrossRef] [PubMed]
- Krigolson, O.E.; Hammerstrom, M.R.; Abimbola, W.; Trska, R.; Wright, B.W.; Hecker, K.G.; Binsted, G. Using Muse: Rapid Mobile Assessment of Brain Performance. Front. Neurosci. 2021, 15, 634147. [Google Scholar] [CrossRef] [PubMed]
- Mascia, A.; Collu, R.; Spanu, A.; Fraschini, M.; Barbaro, M.; Cosseddu, P. Wearable System Based on Ultra-Thin Parylene C Tattoo Electrodes for EEG Recording. Sensors 2023, 23, 766. [Google Scholar] [CrossRef]
- Hortobágyi, T.; Granacher, U.; Fernandez-Del-Olmo, M.; Howatson, G.; Manca, A.; Deriu, F.; Taube, W.; Gruber, M.; Márquez, G.; Lundbye-Jensen, J.; et al. Functional Relevance of Resistance Training-Induced Neuroplasticity in Health and Disease. Neurosci. Biobehav. Rev. 2021, 122, 79–91. [Google Scholar] [CrossRef]
- Gorzi, A.; Rezapour, N.; Jabbari, S.; Youzbashi, L.; Salehi, J.; Gahreman, D.; Krause Neto, W. Deceptive Intensities: An Exploratory Strategy for Overcoming Early Central Fatigue in Resistance Training. Physiol. Behav. 2022, 255, 113921. [Google Scholar] [CrossRef] [PubMed]
- Bryson, D. Smart Clothing and Wearable Technology in Medical and Healthcare Applications. Smart Clothes Wearable Technol. 2023, 573–581. [Google Scholar] [CrossRef]
- Nahavandi, D.; Alizadehsani, R.; Khosravi, A.; Acharya, U.R. Application of Artificial Intelligence in Wearable Devices: Opportunities and Challenges. Comput. Methods Programs Biomed. 2022, 213, 106541. [Google Scholar] [CrossRef]
- Yu, K.-H.; Beam, A.L.; Kohane, I.S. Artificial Intelligence in Healthcare. Nat. Biomed. Eng. 2018, 2, 719–731. [Google Scholar] [CrossRef]
- Lydakis, A.; Meng, Y.; Munroe, C.; Wu, Y.-N.; Begum, M. A Learning-Based Agent for Home Neurorehabilitation. IEEE Int. Conf. Rehabil. Robot. 2017, 2017, 1233–1238. [Google Scholar] [CrossRef] [PubMed]
- Le Noury, P.; Polman, R.; Maloney, M.; Gorman, A. A Narrative Review of the Current State of Extended Reality Technology and How It Can Be Utilised in Sport. Sports Med. 2022, 52, 1473–1489. [Google Scholar] [CrossRef] [PubMed]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Beukelaar, T.T.; Mantini, D. Monitoring Resistance Training in Real Time with Wearable Technology: Current Applications and Future Directions. Bioengineering 2023, 10, 1085. https://doi.org/10.3390/bioengineering10091085
de Beukelaar TT, Mantini D. Monitoring Resistance Training in Real Time with Wearable Technology: Current Applications and Future Directions. Bioengineering. 2023; 10(9):1085. https://doi.org/10.3390/bioengineering10091085
Chicago/Turabian Stylede Beukelaar, Toon T., and Dante Mantini. 2023. "Monitoring Resistance Training in Real Time with Wearable Technology: Current Applications and Future Directions" Bioengineering 10, no. 9: 1085. https://doi.org/10.3390/bioengineering10091085
APA Stylede Beukelaar, T. T., & Mantini, D. (2023). Monitoring Resistance Training in Real Time with Wearable Technology: Current Applications and Future Directions. Bioengineering, 10(9), 1085. https://doi.org/10.3390/bioengineering10091085







