Cancer Drug Delivery Systems Using Bacterial Toxin Translocation Mechanisms
Abstract
1. Introduction
2. Anthrax Toxin PA-Based Cancer Drug Delivery
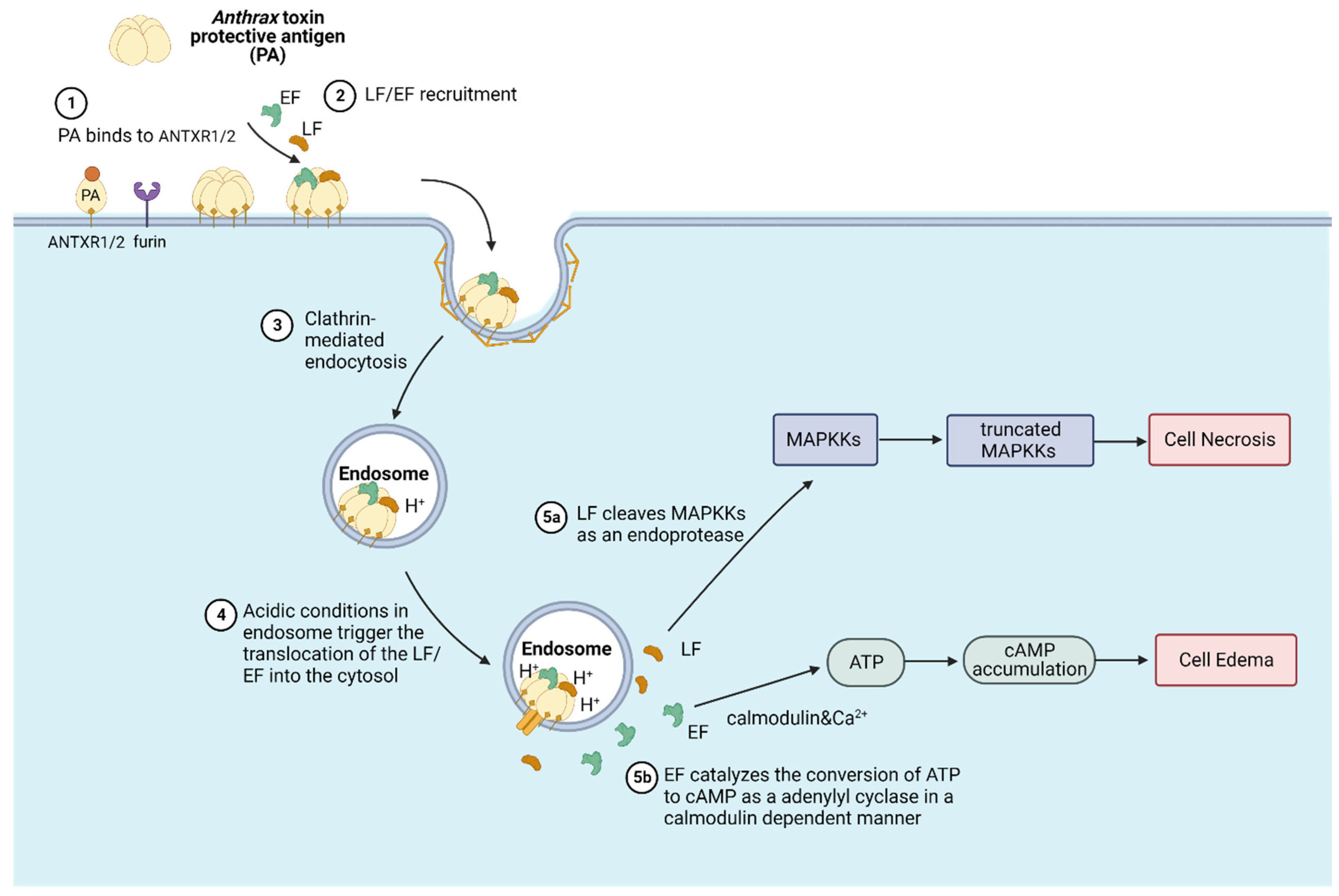
2.1. Anthrax Toxin
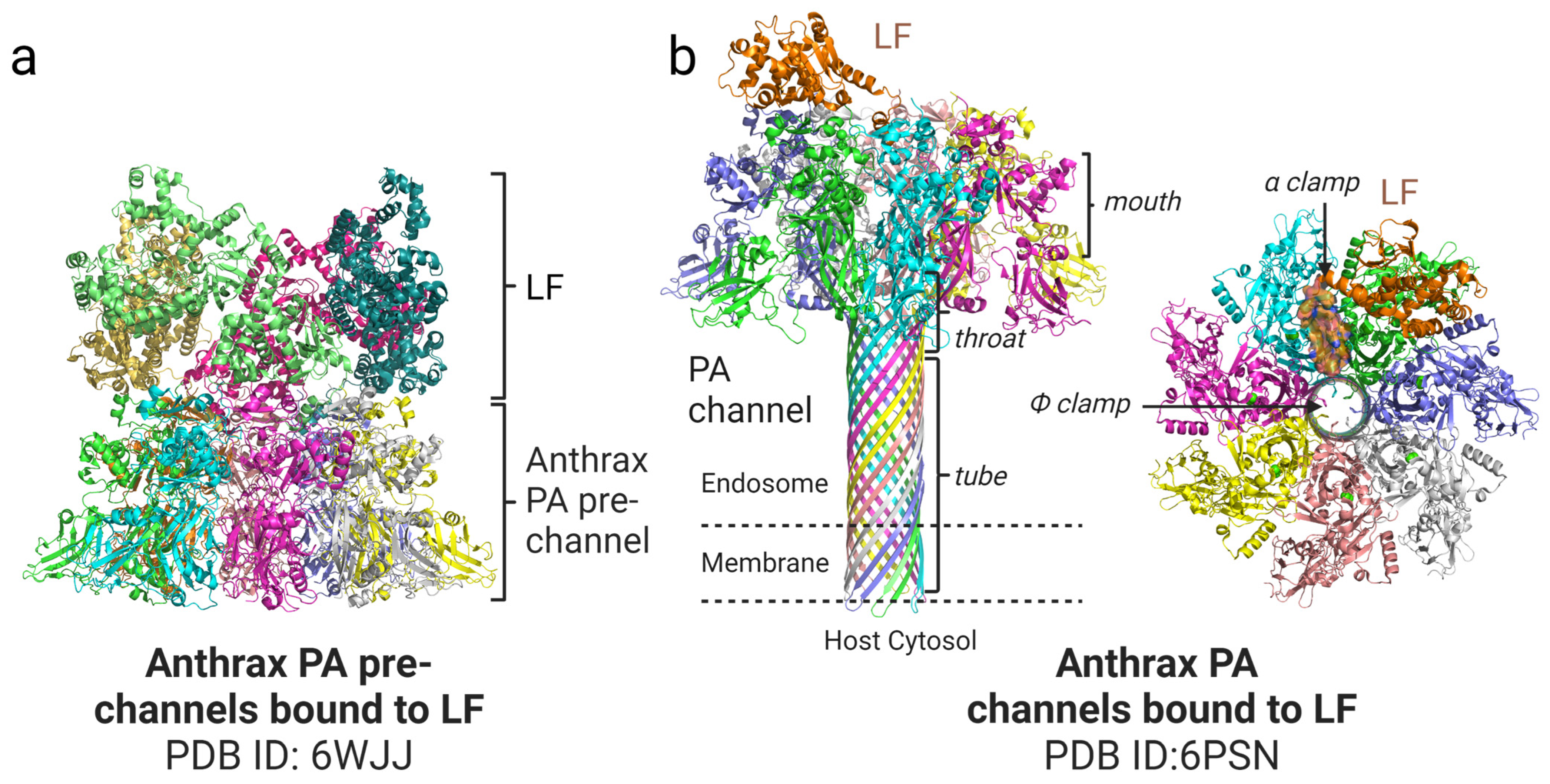
2.2. Anthrax Translocation Mechanisms
2.3. Anthrax Toxin PA-Based Drug Delivery for Cancer Therapy
| Toxin/Toxin Fragment | Targeting Moiety | Target Cancer Cells or Diseases | Obtained Outcome | References |
|---|---|---|---|---|
| C-terminus of PA | c-Myc | c-Myc-specific hybridoma cell line | Mouse macrophages and c-Myc-specific hybridoma cell killing | [43] |
| Mutant PA (PA N682A D683A) | EGF | EGFR positive Human A431 epidermoid carcinoma cells | Enzymatic effector proteins transported into A431 carcinoma cells | [36] |
| Mutant PA (mPA) | HER2 Affibody | HER2 positive breast cancer cell lines | Specific killing of HER2 positive breast cancer cell lines; no off-target killing of HER2-negative cells | [38] |
| Zymogen activation PA | ANTXR1/2 | Ovarian tumor cell lines | Selective killing of ovarian tumor cells; inhibition of ovarian tumor growth in preclinical xenograft models | [42] |
3. Diphtheria Toxin Translocation Domain-Based Cancer Drug Delivery
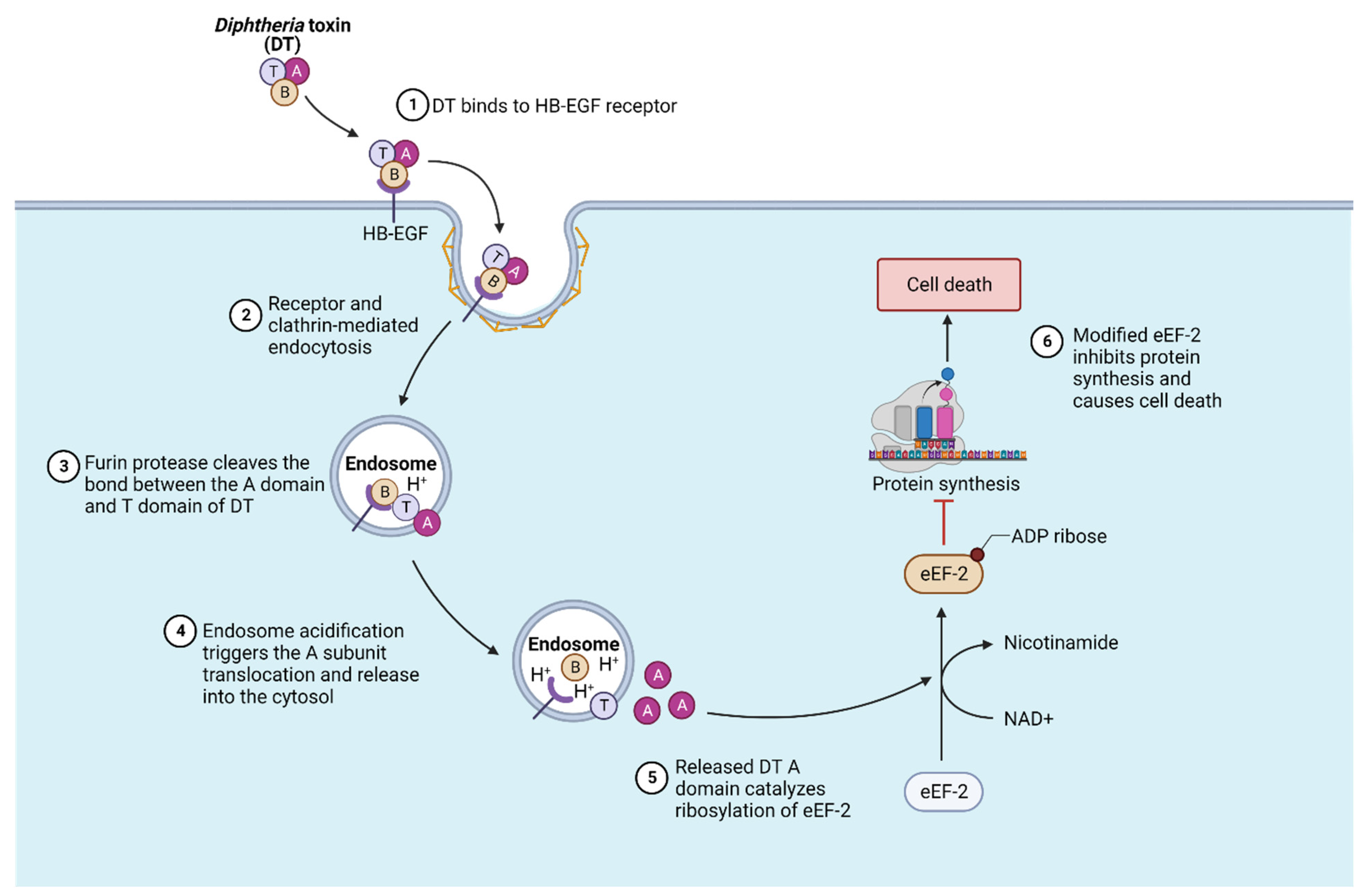
3.1. Diphtheria Toxin and Its Mechanism of Translocation
3.2. Diphtheria Toxin T Domain-Based Drug Delivery
4. Pseudomonas Exotoxin A Translocation Domain-Based Cancer Drug Delivery
4.1. Pseudomonas Exotoxin A and Its Translocation Mechanism
4.2. Pseudomonas Exotoxin-Based Cancer Drug Delivery
5. Discussion
6. Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ITs | immunotoxins |
| PA | protective antigen |
| LF | lethal factor |
| EF | edema factor |
| ANTXR1 | anthrax toxin receptor 1 |
| ANTXR2 | anthrax toxin receptor 2 |
| PA83 | 83-kDa PA monomer |
| PA63 | 63-kDa PA monomer |
| MAPKKs | mitogen-activated protein kinase kinases |
| cAMP | cyclic adenosine monophosphate |
| ADP | adenosine diphosphate |
| EGF | epidermal growth factor |
| EGFR | epidermal growth factor receptor |
| HER2 | human epidermal growth factor receptor 2 |
| HB-EGF | heparin-binding EGF-like growth factor |
| IL-2 | interleukin-2 |
| IL-2R | interleukin-2 receptor |
| IC50s | half maximal inhibitory concentrations |
| CD4+ | CD4-positive |
| BPDCN | blastic plasmacytoid dendritic cell neoplasm |
| CR | complete response |
| PR | partial response |
| CTCL | cutaneous T-cell lymphoma |
| NHL | non-Hodgkin lymphoma |
| Treg | regulatory T cell |
| CCR4 | CC chemokine receptor 4 |
| AML | acute myeloid leukemia |
| PE | Pseudomonas exotoxin A |
| Foxp3 | forkhead box p3 |
| LRP1 | low-density lipoprotein receptor-related protein 1 |
| ER | endoplasmic reticulum |
| Fab | Fragment antigen-binding |
| EpCAM | Epithelial cell adhesion molecule |
| HCL | hairy cell leukemia |
| eCISs | extracellular contractile injection systems |
| EMA | European Medicines Agency |
| FDA | Food and Drug Administration |
| FRET | fluorescence resonance energy transfer |
| cryo-EM | cryo-Electron Microscopy |
| NAD | Nicotinamide adenine dinucleotide |
| EF-2 | elongation factor-2 |
| eEF-2 | eukaryotic elongation factor-2 |
| dsFv | disulfide stabilized variable fragment |
| CD22 | cluster of differentiation22 |
| CAR-T | chimeric antigen receptor T cells |
References
- Chiloeches, M.L.; Bergonzini, A.; Frisan, T. Bacterial toxins are a never-ending source of surprises: From natural born killers to negotiators. Toxins 2021, 13, 426. [Google Scholar] [CrossRef]
- Clark, G.C.; Casewell, N.R.; Elliott, C.T.; Harvey, A.L.; Jamieson, A.G.; Strong, P.N.; Turner, A.D. Friends or Foes? Emerging Impacts of Biological Toxins. Trends Biochem. Sci. 2019, 44, 365–379. [Google Scholar] [CrossRef] [PubMed]
- Xiong, X.; Tian, S.; Yang, P.; Lebreton, F.; Bao, H.; Sheng, K.; Yin, L.; Chen, P.; Zhang, J.; Qi, W.; et al. Emerging enterococcus pore-forming toxins with MHC/HLA-I as receptors. Cell 2022, 185, 1157–1171.e22. [Google Scholar] [CrossRef] [PubMed]
- Dong, M.; Masuyer, G.; Stenmark, P. Botulinum and Tetanus Neurotoxins. Annu. Rev. Biochem. 2019, 20, 811–837. [Google Scholar] [CrossRef] [PubMed]
- Yin, L.; Masuyer, G.; Zhang, S.; Zhang, J.; Miyashita, S.I.; Burgin, D.; Lovelock, L.; Coker, S.F.; Fu, T.M.; Stenmark, P.; et al. Characterization of a membrane binding loop leads to engineering botulinum neurotoxin B with improved therapeutic efficacy. PLoS Biol. 2020, 18, e3000618. [Google Scholar] [CrossRef] [PubMed]
- Dong, M.; Yeh, F.; Tepp, W.H.; Dean, C.; Johnson, E.A.; Janz, R.; Chapman, E.R. SV2 Is the Protein Receptor for Botulinum Neurotoxin A. Science 2006, 312, 592–596. [Google Scholar] [CrossRef]
- Orrell, K.E.; Mansfield, M.J.; Doxey, A.C.; Melnyk, R.A. The C. difficile toxin B membrane translocation machinery is an evolutionarily conserved protein delivery apparatus. Nat. Commun. 2020, 11, 432. [Google Scholar] [CrossRef]
- Mansfield, M.J.; Doxey, A.C. Genomic insights into the evolution and ecology of botulinum neurotoxins. Pathog. Dis. 2018, 76, fty040. [Google Scholar] [CrossRef]
- Jiang, J.; Pentelute, B.L.; Collier, R.J.; Zhou, Z.H. Atomic structure of anthrax protective antigen pore elucidates toxin translocation. Nature 2015, 521, 545–549. [Google Scholar] [CrossRef]
- Khounlo, R.; Kim, J.; Yin, L.; Shin, Y.K. Botulinum Toxins A and E Inflict Dynamic Destabilization on t-SNARE to Impair SNARE Assembly and Membrane Fusion. Structure 2017, 25, 1679–1686.e5. [Google Scholar] [CrossRef]
- Choe, S.; Bennett, M.J.; Fujii, G.; Curmi, P.M.G.; Kantardjieff, K.A.; Collier, R.J.; Eisenberg, D. The crystal structure of diphtheria toxin. Nature 1992, 357, 216–222. [Google Scholar] [CrossRef] [PubMed]
- Lacy, D.B.; Tepp, W.; Cohen, A.C.; DasGupta, B.R.; Stevens, R.C. Crystal structure of botulinum neurotoxin type A and implications for toxicity. Nat. Struct. Biol. 1998, 5, 898–902. [Google Scholar] [CrossRef] [PubMed]
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Parkin, D.M.; Piñeros, M.; Znaor, A.; Bray, F. Cancer statistics for the year 2020: An overview. Int. J. Cancer 2021, 149, 778–789. [Google Scholar] [CrossRef]
- Denkberg, G.; Lev, A.; Eisenbach, L.; Benhar, I.; Reiter, Y. Selective Targeting of Melanoma and APCs Using a Recombinant Antibody with TCR-Like Specificity Directed Toward a Melanoma Differentiation Antigen. J. Immunol. 2003, 171, 2197–2207. [Google Scholar] [CrossRef] [PubMed]
- Zahaf, N.I.; Schmidt, G. Bacterial toxins for cancer therapy. Toxins 2017, 9, 236. [Google Scholar] [CrossRef] [PubMed]
- Pastan, I.; Hassan, R.; FitzGerald, D.J.; Kreitman, R.J. Immunotoxin treatment of cancer. Annu. Rev. Med. 2007, 58, 221–237. [Google Scholar] [CrossRef]
- Syed, Y.Y. Tagraxofusp: First Global Approval. Drugs 2019, 79, 579–583. [Google Scholar] [CrossRef]
- Dhillon, S. Moxetumomab Pasudotox: First Global Approval. Drugs 2019, 78, 1763–1767. [Google Scholar] [CrossRef]
- Shafiee, F.; Aucoin, M.G.; Jahanian-Najafabadi, A. Targeted Diphtheria Toxin-Based Therapy: A Review Article. Front. Microbiol. 2019, 10, 2340. [Google Scholar] [CrossRef]
- Zhang, S.; Finkelstein, A.; Collier, R.J. Evidence That Translocation of Anthrax Toxin’s Lethal Factor is Initiated by Entry of Its N Terminus into the Protective Antigen Channel. Proc. Natl. Acad. Sci. USA 2004, 101, 16756–16761. [Google Scholar] [CrossRef]
- Van Der Goot, G.; Young, J.A.T. Receptors of anthrax toxin and cell entry. Mol Asp. Med. 2009, 30, 406–412. [Google Scholar] [CrossRef]
- Sun, J.; Jacquez, P. Roles of anthrax toxin receptor 2 in anthrax toxin membrane insertion and pore formation. Toxins 2016, 8, 34. [Google Scholar] [CrossRef] [PubMed]
- Scobie, H.M.; Marlett, J.M.; Rainey, G.J.A.; Lacy, D.B.; Collier, R.J.; Young, J.A.T. Anthrax toxin receptor 2 determinants that dictate the pH threshold of toxin pore formation. PLoS ONE 2007, 2, e329. [Google Scholar] [CrossRef] [PubMed]
- Kintzer, A.F.; Thoren, K.L.; Sterling, H.J.; Dong, K.C.; Feld, G.K.; Tang, I.I.; Zhang, T.T.; Williams, E.R.; Berger, J.M.; Krantz, B.A. The Protective Antigen Component of Anthrax Toxin Forms Functional Octameric Complexes. J. Mol. Biol. 2009, 392, 614–629. [Google Scholar] [CrossRef] [PubMed]
- Kintzer, A.F.; Sterling, H.J.; Tang, I.I.; Williams, E.R.; Krantz, B.A. Anthrax toxin receptor drives protective antigen oligomerization and stabilizes the heptameric and octameric oligomer by a similar mechanism. PLoS ONE 2010, 5, e13888. [Google Scholar] [CrossRef]
- Lowe, D.E.; Glomski, I.J. Cellular and physiological effects of anthrax exotoxin and its relevance to disease. Front. Cell. Infect. Microbiol. 2012, 2, 76. [Google Scholar] [CrossRef]
- Zhou, K.; Liu, S.; Hardenbrook, N.J.; Cui, Y.; Krantz, B.A.; Zhou, Z.H.; Zhou, K.; Liu, S.; Hardenbrook, N.J.; Cui, Y.; et al. Atomic Structures of Anthrax Prechannel Bound with Full-Length Lethal and Edema Factors ll ll Article Atomic Structures of Anthrax Prechannel Bound with Full-Length Lethal and Edema Factors. Struct. 2020, 28, 879–887.e3. [Google Scholar] [CrossRef]
- Hardenbrook, N.J.; Liu, S.; Zhou, K.; Ghosal, K.; Hong Zhou, Z.; Krantz, B.A. Atomic structures of anthrax toxin protective antigen channels bound to partially unfolded lethal and edema factors. Nat. Commun. 2020, 11, 840. [Google Scholar] [CrossRef]
- Collier, R.J. Membrane translocation by anthrax toxin. Mol. Asp. Med. 2009, 30, 413–422. [Google Scholar] [CrossRef]
- Gonti, S.; Westler, W.M.; Miyagi, M.; Bann, J.G. Site-Specific Labeling and 19F NMR Provide Direct Evidence for Dynamic Behavior of the Anthrax Toxin Pore ϕ-Clamp Structure. Biochemistry 2021, 60, 643–647. [Google Scholar] [CrossRef]
- Krantz, B.A.; Trivedi, A.D.; Cunningham, K.; Christensen, K.A.; Collier, R.J. Acid-induced unfolding of the amino-terminal domains of the lethal and edema factors of anthrax toxin. J. Mol. Biol. 2004, 344, 739–756. [Google Scholar] [CrossRef] [PubMed]
- Bachran, C.; Leppla, S.H. Tumor targeting and drug delivery by anthrax toxin. Toxins 2016, 8, 197. [Google Scholar] [CrossRef]
- Fu, X.; Shi, X.; Yin, L.; Liu, J.; Joo, K.; Lee, J.; Chang, Z. Small heat shock protein IbpB acts as a robust chaperone in living cells by hierarchically activating its multi-type substrate-binding residues. J. Biol. Chem. 2013, 288, 11897–11906. [Google Scholar] [CrossRef]
- Arora, N.; Klimpels, R.; Singhso, Y.; Lepplall, S.H. Fusions of Anthrax Toxin Lethal Factor to the ADP-ribosylation Domain of Pseudomonas Exotoxin A Are Potent Cytotoxins Which Are Translocated to the Cytosol of Mammalian Cells. J. Biol. Chem. 1992, 267, 15542–15548. [Google Scholar] [CrossRef]
- Arora, N.; Leppla, S.H. Residues 1-254 of anthrax toxin lethal factor are sufficient to cause cellular uptake of fused polypeptides. J. Biol. Chem. 1993, 268, 3334–3341. [Google Scholar] [CrossRef] [PubMed]
- Mechaly, A.; Mccluskey, A.J.; Collier, R.J. Changing the Receptor Specificity of Anthrax Toxin. mBio 2012, 3, e00088-12. [Google Scholar] [CrossRef]
- Jack, S.; Madhivanan, K.; Ramadesikan, S.; Subramanian, S.; Edwards, D.F., II; Elzey, B.D.; Dhawan, D.; McCluskey, A.; Kischuk, E.M.; Loftis, A.R.; et al. A novel, safe, fast and efficient treatment for Her2-positive and negative bladder cancer utilizing an EGF-anthrax toxin chimera. Int. J. Cancer 2019, 146, 449–460. [Google Scholar] [CrossRef] [PubMed]
- Mccluskey, A.J.; Olive, A.J.; Starnbach, M.N.; Collier, R.J. Targeting HER2-positive cancer cells with receptor-redirected anthrax protective antigen. Mol. Oncol. 2012, 7, 440–451. [Google Scholar] [CrossRef]
- Liu, S.; Bugge, T.H.; Leppla, S.H. Targeting of Tumor Cells by Cell Surface Urokinase Plasminogen Activator-dependent Anthrax Toxin. J. Biol. Chem. 2001, 276, 17976–17984. [Google Scholar] [CrossRef]
- Tan, Y.; Tajik, A.; Chen, J.; Jia, Q.; Chowdhury, F.; Wang, L.; Chen, J.; Zhang, S.; Hong, Y.; Yi, H.; et al. Matrix softness regulates plasticity of tumour-repopulating cells via H3K9 demethylation and Sox2 expression. Nat. Commun. 2014, 5, 4619. [Google Scholar] [CrossRef]
- Vasculature, T.; Liu, S.; Wang, H.; Currie, B.M.; Molinolo, A.; Leung, H.J.; Moayeri, M.; Basile, J.R.; Alfano, R.W.; Gutkind, J.S.; et al. Matrix Metalloproteinase-activated Anthrax Lethal Toxin Demonstrates High Potency in Targeting. J. Biol. Chem. 2008, 283, 529–540. [Google Scholar]
- Duru, N.; Pawar, N.R.; Martin, E.W.; Buzza, M.S.; Conway, G.D.; Lapidus, R.G.; Liu, S.; Reader, J.; Rao, G.G.; Roque, D.M.; et al. Selective targeting of metastatic ovarian cancer using an engineered anthrax prodrug activated by membrane-anchored serine proteases. Proc. Natl. Acad. Sci. USA 2022, 119, e2201423119. [Google Scholar] [CrossRef] [PubMed]
- Varughese, M.; Chi, A.; Teixeira, A.V.; Nicholls, P.J.; Keith, J.M.; Leppla, S.H. Internalization of a Bacillus anthracis Protective Antigen-c-Myc Fusion Protein Mediated by Cell Surface Anti-c-Myc Antibodies. Mol. Med. 1998, 4, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Holmes, R.K. Biology and molecular epidemiology of diphtheria toxin and the tox gene. J. Infect. Dis. 2000, 181 (Suppl. S1), 156–167. [Google Scholar] [CrossRef]
- Barksdale, L.; Garmise, L. Kengo Horibata Virulence, toxinogeny, and lysogeny in Corynebacterium diphtheriae. Ann. N. Y. Acad. Sci. 1960, 88, 1093–1108. [Google Scholar] [CrossRef]
- Prygiel, M.; Polak, M.; Mosiej, E.; Wdowiak, K.; Formińska, K.; Zasada, A.A. New Corynebacterium Species with the Potential to Produce Diphtheria Toxin. Pathogens 2022, 11, 1264. [Google Scholar] [CrossRef]
- Naglich, J.G.; Metherall, J.E.; Russell, D.W.; Eidels, L. Expression cloning of a diphtheria toxin receptor: Identity with a heparin-binding EGF-like growth factor precursor. Cell 1992, 69, 1051–1061. [Google Scholar] [CrossRef]
- Draper, R.K.; Simon, M.I. The entry of diphtheria toxin into the mammalian cell cytoplasm: Evidence for lysosomal involvement. J. Cell Biol. 1980, 87, 849–854. [Google Scholar] [CrossRef] [PubMed]
- Madshus, I.H.; Olsnes, S.; Stenmark, H. Membrane translocation of diphtheria toxin carrying passenger protein domains. Infect. Immun. 1992, 60, 3296–3302. [Google Scholar] [CrossRef]
- Arnold, A.E.; Smith, L.J.; Beilhartz, G.; Bahlmann, L.C.; Jameson, E.; Melnyk, R.; Shoichet, M.S. Attenuated diphtheria toxin mediates siRNA delivery. Sci. Adv. 2020, 6, eaaz4848. [Google Scholar] [CrossRef]
- Sugiman-Marangos, S.N.; Gill, S.K.; Mansfield, M.J.; Orrell, K.E.; Doxey, A.C.; Melnyk, R.A. Structures of distant diphtheria toxin homologs reveal functional determinants of an evolutionarily conserved toxin scaffold. Commun. Biol. 2022, 5, 375. [Google Scholar] [CrossRef]
- Kaul, P.; Silverman, J.; Shen, W.H.; Blanke, S.R.; Huynh, P.D.; Finkelstein, A.; Collier, R.J. Roles of Glu 349 and Asp 352 in membrane insertion and translocation by diphtheria toxin. Protein Sci. 1996, 5, 687–692. [Google Scholar] [CrossRef] [PubMed]
- Senzel, L.; Gordon, M.; Blaustein, R.O.; Oh, K.J.; Collier, R.J.; Finkelstein, A. Topography of diphtheria toxin’s T domain in the open channel state. J. Gen. Physiol. 2000, 115, 421–434. [Google Scholar] [CrossRef] [PubMed]
- LeMaistre, C.F.; Craig, F.E.; Meneghetti, C.; McMullin, B.; Boldt, D.H.; Reuben, J.; Rosenblum, M.; Parker, K.; Woodworth, T. Phase I Trial of a 90-Minute Infusion of the Fusion Toxin DAB486IL-2 in Hematological Cancers. Cancer Res. 1993, 53, 3930–3934. [Google Scholar] [PubMed]
- Tepler, I.; Schwartz, G.; Parker, K.; Charette, J.; Kadin, M.E.; Woodworth, T.G.; Schnipper, L.E. Phase I Trial of an Interleukin-2 Fusion Toxin (DAB4861L-2) in Hematologic Malignancies: Complete Response in a Patient with Hodgkin’s Disease Refractory to Chemotherapy. Cancer 1993, 73, 1276–1285. [Google Scholar] [CrossRef]
- Eklund, J.W.; Kuzel, T.M. Denileukin diftitox: A concise clinical review. Expert Rev. Anticancer Ther. 2005, 5, 33–38. [Google Scholar] [CrossRef]
- Peraino, J.S.; Zhang, H.; Rajasekera, P.V.; Wei, M.; Madsen, J.C.; Sachs, D.H.; Huang, C.A.; Wang, Z. Diphtheria toxin-based bivalent human IL-2 fusion toxin with improved efficacy for targeting human CD25+ cells. J. Immunol. Methods 2014, 405, 57–66. [Google Scholar] [CrossRef]
- Baluna, R.; Rizo, J.; Gordon, B.E.; Ghetie, V.; Vitetta, E.S. Evidence for a structural motif in toxins and interleukin-2 that may be responsible for binding to endothelial cells and initiating vascular leak syndrome. Proc. Natl. Acad. Sci. USA 1999, 96, 3957–3962. [Google Scholar] [CrossRef]
- Smallshaw, J.E.; Ghetie, V.; Rizo, J.; Fulmer, J.R.; Trahan, L.L.; Ghetie, M.A.; Vitetta, E.S. Genetic engineering of an immunotoxin to eliminate pulmonary vascular leak in mice. Nat. Biotechnol. 2003, 21, 387–391. [Google Scholar] [CrossRef]
- Cheung, L.S.; Fu, J.; Kumar, P.; Kumar, A.; Urbanowski, M.E.; Ihms, E.A.; Parveen, S.; Bullen, C.K.; Patrick, G.J.; Harrison, R.; et al. Second-generation IL-2 receptor-targeted diphtheria fusion toxin exhibits antitumor activity and synergy with anti–PD-1 in melanoma. Proc. Natl. Acad. Sci. USA 2019, 116, 3100–3105. [Google Scholar] [CrossRef]
- LeMaistre, C.F.; Meneghetti, C.; Rosenblum, M.; Reuben, J.; Parker, K.; Shaw, J.; Deisseroth, A.; Woodworth, T.; Parkinson, D.R. Phase I trial of an interleukin-2 (IL-2) fusion toxin (DAB486IL-2) in hematologic malignancies expressing the IL-2 receptor. Blood 1992, 79, 2547–2554. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Kessler, E.; Su, L.J.; Thorburn, A.; Frankel, A.E.; Li, Y.; La Rosa, F.G.; Shen, J.; Li, C.Y.; Varella-Garcia, M.; et al. Diphtheria toxin-epidermal growth factor fusion protein DAB 389EGF for the treatment of bladder cancer. Clin. Cancer Res. 2013, 19, 148–157. [Google Scholar] [CrossRef] [PubMed]
- Sweeney, E.B.; Foss, F.M.; Murphy, J.R.; Vanderspek, J.C. Interleukin 7 (IL-7) receptor-specific cell killing by DAB389 IL-7: A novel agent for the elimination of IL-7 receptor positive cells. Bioconjug. Chem. 1998, 9, 201–207. [Google Scholar] [CrossRef]
- Rustamzadeh, E.; Hall, W.A.; Todhunter, D.A.; Low, W.C.; Liu, H.; Panoskaltsis-Mortari, A.; Vallera, D.A. Intracranial therapy of glioblastoma with the fusion protein DTIL13 in immunodeficient mice. Int. J. Cancer 2006, 118, 2594–2601. [Google Scholar] [CrossRef]
- Oh, S.; Ohlfest, J.R.; Todhunter, D.A.; Vallera, V.D.; Hall, W.A.; Chen, H.; Vallera, D.A. Intracranial elimination of human glioblastoma brain tumors in nude rats using the bispecific ligand-directed toxin, DTEGF13 and convection enhanced delivery. J. Neurooncol. 2009, 95, 331–342. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Pratts, S.G.; Zhang, H.; Spencer, P.J.; Yu, R.; Tonsho, M.; Shah, J.A.; Tanabe, T.; Powell, H.R.; Huang, C.A.; et al. Treg depletion in non-human primates using a novel diphtheria toxin-based anti-human CCR4 immunotoxin. Mol. Oncol. 2016, 10, 553–565. [Google Scholar] [CrossRef]
- McKee, M.L.; FitzGerald, D.J. Reduction of furin-nicked Pseudomonas exotoxin A: An unfolding story. Biochemistry 1999, 38, 16507–16513. [Google Scholar] [CrossRef]
- Zerial, M.; McBride, H. Rab proteins as membrane organizers. Nat. Rev. Mol. Cell Biol. 2001, 2, 107–117. [Google Scholar] [CrossRef]
- Kreitman, R.J.; Pastan, I. Importance of the glutamate residue of KDEL in increasing the cytotoxicity of Pseudomonas exotoxin derivatives and for increased binding to the KDEL receptor. Biochem. J. 1995, 307, 29–37. [Google Scholar] [CrossRef]
- Michalska, M.; Wolf, P. Pseudomonas Exotoxin A: Optimized by evolution for effective killing. Front. Microbiol. 2015, 6, 963. [Google Scholar] [CrossRef]
- Allured, V.S.; Collier, R.J.; Carroll, S.F.; McKay, D.B. Structure of exotoxin A of Pseudomonas aeruginosa at 3.0-Angstrom resolution. Proc. Natl. Acad. Sci. USA 1986, 83, 1320–1324. [Google Scholar] [CrossRef] [PubMed]
- Wedekind, J.E.; Trame, C.B.; Dorywalska, M.; Koehl, P.; Raschke, T.M.; McKee, M.; FitzGerald, D.; Collier, R.J.; McKay, D.B. Refined crystallographic structure of Pseudomonas aeruginosa exotoxin A and its implications for the molecular mechanism of toxicity. J. Mol. Biol. 2001, 314, 823–837. [Google Scholar] [CrossRef]
- Ogata, M.; Chaudhary, V.K.; Pastan, I.; FitzGerald, D.J. Processing of Pseudomonas exotoxin by a cellular protease results in the generation of a 37,000-Da toxin fragment that is translocated to the cytosol. J. Biol. Chem. 1990, 265, 20678–20685. [Google Scholar] [CrossRef] [PubMed]
- Iglewski, B.H.; Liu, P.V.; Kabat, D. Mechanism of action of Pseudomonas aeruginosa exotoxin A: Adenosine diphosphate ribosylation of mammalian elongation factor 2 in vitro and in vivo. Infect. Immun. 1977, 15, 138–144. [Google Scholar] [CrossRef]
- Havaei, S.M.; Aucoin, M.G.; Jahanian-najafabadi, A. Pseudomonas Exotoxin-Based Immunotoxins: Over Three Decades of Efforts on Targeting Cancer Cells With the Toxin. Front. Oncol. 2021, 11, 781800. [Google Scholar] [CrossRef] [PubMed]
- Kreitman, R.J.; Wilson, W.H.; Bergeron, K.; Raggio, M.; Stetler-Stevenson, M.; FitzGerald, D.J.; Pastan, I. Efficacy of the Anti-CD22 Recombinant Immunotoxin BL22 in Chemotherapy-Resistant Hairy-Cell Leukemia. N. Engl. J. Med. 2001, 345, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Alderson, R.F.; Kreitman, R.J.; Chen, T.; Yeung, P.; Herbst, R.; Fox, J.; Pastan, I. CAT-8015: A second-generation Pseudomonas exotoxin a-based immunotherapy targeting CD22-expressing hematologic malignancies. Clin. Cancer Res. 2009, 15, 832–839. [Google Scholar] [CrossRef] [PubMed]
- Bokori-Brown, M.; Metz, J.; Petrov, P.G.; Mussai, F.; De Santo, C.; Smart, N.J.; Saunders, S.; Knight, B.; Pastan, I.; Titball, R.W.; et al. Interactions between Pseudomonas immunotoxins and the plasma membrane: Implications for CAT-8015 immunotoxin therapy. Front. Oncol. 2018, 8, 553. [Google Scholar] [CrossRef]
- Kunwar, S.; Chang, S.; Westphal, M.; Vogelbaum, M.; Sampson, J.; Barnett, G.; Shaffrey, M.; Ram, Z.; Piepmeier, J.; Prados, M.; et al. Phase III randomized trial of CED of IL13-PE38QQR vs. Gliadel wafers for recurrent glioblastoma. Neuro-Oncology 2010, 12, 871–881. [Google Scholar] [CrossRef]
- Kowalski, M.; Guindon, J.; Brazas, L.; Moore, C.; Entwistle, J.; Cizeau, J.; Jewett, M.A.S.; Macdonald, G.C. A Phase II Study of Oportuzumab Monatox: An Immunotoxin Therapy for Patients with Noninvasive Urothelial Carcinoma In Situ Previously Treated with Bacillus Calmette-Guérin. JURO 2012, 188, 1712–1718. [Google Scholar] [CrossRef]
- Alewine, C.; Ahmad, M.; Peer, C.J.; Hu, Z.I.; Lee, M.; Kindrick, J.D.; Thomas, A.; Steinberg, S.M.; Trepel, J.B.; Figg, D.; et al. Phase I/II Study of the Mesothelin-targeted Immunotoxin LMB-100 with Nab-Paclitaxel for Patients with Advanced Pancreatic Adenocarcinoma. Clin. Cancer Res. 2021, 26, 828–836. [Google Scholar] [CrossRef]
- Weber, F.; Asher, A.; Bucholz, R.; Berger, M.; Prados, M.; Chang, S. Safety, tolerability, and tumor response of IL4-Pseudomonas exotoxin (NBI-3001) in patients with recurrent malignant glioma. J. Neurooncol. 2003, 64, 125–137. [Google Scholar] [CrossRef]
- Chandramohan, V.; Bao, X.; Keir, S.T.; Pegram, C.N.; Szafranski, S.E.; Piao, H.; Kuan, C.-T.; Wikstrand, C.J.; Pastan, I.H.; McLendon, R.E.; et al. Construction of an immunotoxin, D2C7-(scdsFv)-PE38KDEL, targeting EGFRwt and EGFRvIII for brain tumor therapy. Clin. Cancer Res. 2013, 19, 4717–4727. [Google Scholar] [CrossRef]
- Posey, J.A.; Khazaeli, M.B.; Bookman, M.A.; Nowrouzi, A.; Grizzle, W.E.; Thornton, J.; Carey, D.E.; Lorenz, J.M.; Sing, A.P.; Siegall, C.B.; et al. A Phase I Trial of the Single-Chain Immunotoxin SGN-10 ( BR96 sFv-PE40 ) in Patients with Advanced Solid Tumors 1. Clin. Cancer Res. 2002, 8, 3092–3099. [Google Scholar] [PubMed]
- Kreitz, J.; Friedrich, M.J.; Guru, A.; Lash, B.; Saito, M.; Macrae, R.K.; Zhang, F. Programmable protein delivery with a bacterial contractile injection system. Nature 2023, 616, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Tian, S.; Liu, Y.; Appleton, E.; Wang, H.; Church, G.M.; Dong, M. Targeted intracellular delivery of Cas13 and Cas9 nucleases using bacterial toxin-based platforms. Cell Rep. 2022, 38, 110476. [Google Scholar] [CrossRef] [PubMed]
- Segel, M.; Lash, B.; Song, J.; Ladha, A.; Liu, C.C.; Jin, X.; Mekhedov, S.L.; Macrae, R.K.; Koonin, E.V.; Zhang, F. Mammalian retrovirus-like protein PEG10 packages its own mRNA and can be pseudotyped for mRNA delivery. Science 2021, 373, 882–889. [Google Scholar] [CrossRef]
- Izzedine, H.; Mathian, A.; Amoura, Z.; Ng, J.H.; Jhaveri, K.D. Anticancer Drug-Induced Capillary Leak Syndrome. Kidney Int. Rep. 2022, 7, 945–953. [Google Scholar] [CrossRef] [PubMed]
- Mazor, R.; Vassall, A.N.; Eberle, J.A.; Beers, R.; Weldon, J.E.; Venzon, D.J.; Tsang, K.Y.; Benhar, I.; Pastan, I. Identification and elimination of an immunodominant T-cell epitope in recombinant immunotoxins based on Pseudomonas exotoxin A. Proc. Natl. Acad. Sci. USA 2012, 109, E3597–E3603. [Google Scholar] [CrossRef] [PubMed]
- Mazor, R.; Onda, M.; Park, D.; Addissie, S.; Xiang, L.; Zhang, J.; Hassan, R.; Pastan, I. Dual B- and T-cell de-immunization of recombinant immunotoxin targeting mesothelin with high cytotoxic activity. Oncotarget 2016, 7, 29916–29926. [Google Scholar] [CrossRef]
- Mazor, R.; Crown, D.; Addissie, S.; Jang, Y.; Kaplan, G.; Pastan, I. Elimination of murine and human T-cell epitopes in recombinant immunotoxin eliminates neutralizing and anti-drug antibodies in vivo. Cell. Mol. Immunol. 2017, 14, 432–442. [Google Scholar] [CrossRef]
- Mazor, R.; King, E.M.; Pastan, I. Strategies to Reduce the Immunogenicity of Recombinant Immunotoxins. Am. J. Pathol. 2018, 188, 1736–1743. [Google Scholar] [CrossRef]
- Alami, M.; Taupiac, M.P.; Reggio, H.; Bienvenüe, A.; Beaumelle, B. Involvement of ATP-dependent Pseudomonas exotoxin translocation from a late recycling compartment in lymphocyte intoxication procedure. Mol. Biol. Cell 1998, 9, 387–402. [Google Scholar] [CrossRef]
- Yin, L.; Kim, J.; Shin, Y.K. Complexin splits the membrane-proximal region of a single SNAREpin. Biochem. J. 2016, 473, 2219–2224. [Google Scholar] [CrossRef] [PubMed]
- Su, C.C.; Yin, L.; Kumar, N.; Dai, L.; Radhakrishnan, A.; Bolla, J.R.; Lei, H.T.; Chou, T.H.; Delmar, J.A.; Rajashankar, K.R.; et al. Structures and transport dynamics of a Campylobacter jejuni multidrug efflux pump. Nat. Commun. 2017, 8, 171. [Google Scholar] [CrossRef] [PubMed]
- Blum, T.R.; Liu, H.; Packer, M.S.; Xiong, X.; Lee, P.G.; Zhang, S.; Richter, M.; Minasov, G.; Satchell, K.J.F.; Dong, M.; et al. Phage-assisted evolution of botulinum neurotoxin proteases with reprogrammed specificity. Science 2021, 371, 803–810. [Google Scholar] [CrossRef] [PubMed]
- Shaik, M.S.; Ikediobi, O.; Turnage, V.D.; McSween, J.; Kanikkannan, N.; Singh, M. Long-circulating monensin nanoparticles for the potentiation of immunotoxin and anticancer drugs. J. Pharm. Pharmacol. 2010, 53, 617–627. [Google Scholar] [CrossRef]
- Yin, B.; Wong, W.; Ng, Y.; Yang, M.; Leung, F.K. Smart Design of Nanostructures for Boosting Tumor Immunogenicity in Cancer Immunotherapy. Pharmaceutics 2023, 15, 1427. [Google Scholar] [CrossRef]
- Mokhtari, R.B.; Homayouni, T.S.; Baluch, N.; Morgatskaya, E.; Kumar, S.; Das, B.; Yeger, H. Combination therapy in combating cancer. Oncotarget 2017, 8, 38022–38043. [Google Scholar] [CrossRef]
- Grosser, R.; Cherkassky, L.; Chintala, N.; Adusumilli, P.S. Combination Immunotherapy with CAR T Cells and Checkpoint Blockade for the Treatment of Solid Tumors. Cancer Cell 2019, 36, 471–482. [Google Scholar] [CrossRef]
| Toxin/Toxin Fragment | Targeting Moiety | Target Cancer Cells or Diseases | Obtained Outcome | References |
|---|---|---|---|---|
| DAB486 | IL-2 | CTCL, Hematological cancers, NHL | Significant tumor reductions in heavily treated patient group; half of the patients developed an antibody response to the toxin | [54,61] |
| DT389 | IL-2 | CTCL, Hematological cancers, NHL | Patients showed significant improvement in tumor response and quality of life | [56] |
| DT388 | IL-3 | BPDCN, AML | The drug exhibited potent cytotoxicity towards BPDCN and AML cell lines; the IT treatment showed robust clinical activity in patients with BPDCN | [17] |
| DAB389 | EGF | Bladder cancer, lung cancer | Human bladder cancer lines showed specific and robust response with DAB389EGF treatment | [62] |
| DAB389 | IL-7 | Hematopoietic malignancies | DAB389IL-7 fusion protein is selectively cytotoxic for cells bearing the IL-7 receptor | [63] |
| DT389 | IL-13 | Glioblastoma | DT389IL-13 fusion protein resulted in significant tumor volume reduction and the significantly prolonged survival of mice with brain tumors | [64] |
| DT390 | IL-13 and EGF bispecific ligand | Glioblastoma, prostate, and pancreatic cancer | DTEGF13 protein selectively killed human glioblastomas and showed a higher activity than its monospecific IT counterparts | [65] |
| DT390 | CCR4 scFv | Glioblastoma, prostate, and pancreatic cancer | CCR4 IT depleted monkey CCR4(+) cells in vitro; around 80% CCR4(+)Foxp3(+) Tregs were depleted in the tested monkeys | [66] |
| Toxin/Toxin Fragment | Targeting Moiety | Target Cancer Cells or Diseases | Obtained Outcome | References |
|---|---|---|---|---|
| PE38 | IL-4 | Solid tumors, recurrent malignant glioma | Tumor necrosis following treatment in many patients | [82] |
| PE38 | IL-13 | Glioblastoma | The IT was well-tolerated but had no survival advantage compared with Gliadel wafers in a Phase III evaluation | [79] |
| PE38 | Anti-CD22 antibody | Hairy cell leukemia | IT treatment resulted in rapid depletion of CD19(+)B cells and rapid reduction in tumor volume | [18] |
| PE24 | Humanized anti-mesothelin Fab | Pancreatic adenocarcinoma | The drug showed antitumor activity in around half of the treated patients | [81] |
| PE38 | Anti-EGFR antibody | Glioblastoma | ADA against the drug and capillary leak syndrome was seen as a dose-limiting factor | [83] |
| PE40 | Lewis(Y) carbohydrate antigen targeting BR96 sFv | Lewis(Y)-positive metastatic carcinoma | The drug achieved prolonged survival in intracranial tumor models | [84] |
| PE252-608 fragment | Humanized anti-EpCAM single chain antibody | Non-muscle invasive bladder cancer | Complete response achieved in half of the patients with mild to moderate adverse effects that were treatable | [80] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yin, L.; Thaker, H. Cancer Drug Delivery Systems Using Bacterial Toxin Translocation Mechanisms. Bioengineering 2023, 10, 813. https://doi.org/10.3390/bioengineering10070813
Yin L, Thaker H. Cancer Drug Delivery Systems Using Bacterial Toxin Translocation Mechanisms. Bioengineering. 2023; 10(7):813. https://doi.org/10.3390/bioengineering10070813
Chicago/Turabian StyleYin, Linxiang, and Hatim Thaker. 2023. "Cancer Drug Delivery Systems Using Bacterial Toxin Translocation Mechanisms" Bioengineering 10, no. 7: 813. https://doi.org/10.3390/bioengineering10070813
APA StyleYin, L., & Thaker, H. (2023). Cancer Drug Delivery Systems Using Bacterial Toxin Translocation Mechanisms. Bioengineering, 10(7), 813. https://doi.org/10.3390/bioengineering10070813






