Analysis of Static Plantar Pressures in School-Age Children with and without Functional Hallux Limitus: A Case-Control Study
Abstract
1. Introduction
2. Material and Methods
2.1. Study Design
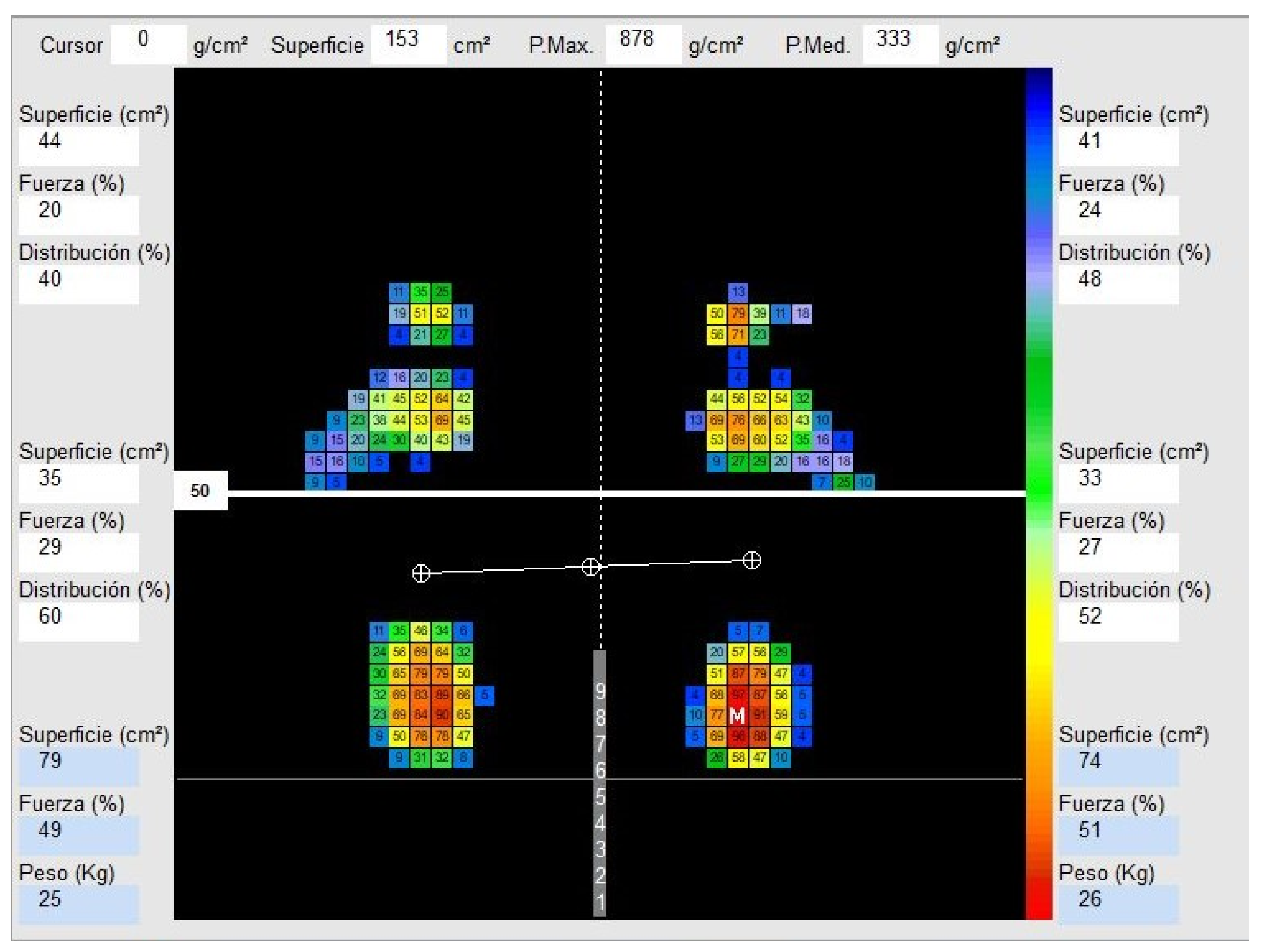
2.2. Method
2.3. Statistical Analysis
3. Results
3.1. Sociodemographic and Descriptive Data
3.2. Primary Outcome Measures
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gerbert, J. Hallux Limitus/Hallux Rigidus, 3rd, ed.; W.B. Saunders: Philadelphia, PA, USA, 2001. [Google Scholar]
- Viehöfer, A.F.; Vich, M.; Wirth, S.H.; Espinosa, N.; Camenzind, R.S. The Role of Plantar Fascia Tightness in Hallux Limitus: A Biomechanical Analysis. J. Foot Ankle Surg. 2019, 58, 465–469. [Google Scholar] [CrossRef]
- Fung, J.; Sherman, A.; Stachura, S.; Eckles, R.; Doucette, J.; Chusid, E. Nonoperative Management of Hallux Limitus Using a Novel Forefoot Orthosis. J. Foot Ankle Surg. 2020, 59, 1192–1196. [Google Scholar] [CrossRef]
- Van Gheluwe, B.; Dananberg, H.J.; Hagman, F.; Vanstaen, K. Effects of hallux limitus on plantar foot pressure and foot kinematics during walking. J. Am. Podiatr. Med. Assoc. 2006, 96, 428–436. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, P.J.; Grady, J.F.; Lenz, R.C.; Park, S.J.; Ruff, J.G. Metatarsus primus elevatus resolution after first metatarsophalangeal joint arthroplasty: Eliminating elevatus without an osteotomy-A preliminary study. J. Am. Podiatr. Med. Assoc. 2018, 108, 200–204. [Google Scholar] [CrossRef]
- Bird, A.R.; Payne, C.B. Foot function and low back pain. Foot 1999, 9, 175–180. [Google Scholar] [CrossRef]
- Dellenbaugh, S.G.; Bustillo, J. Arthritides of the foot. Med. Clin. N. Am. 2014, 98, 253–265. [Google Scholar] [CrossRef]
- Beeson, P. The surgical treatment of hallux limitus/rigidus: A critical review of the literature. Foot 2004, 14, 6–22. [Google Scholar] [CrossRef]
- Coughlin, M.J.; Jones, C.P. Hallux valgus: Demographics, etiology, and radiographic assessment. Foot Ankle Int. 2007, 28, 759–777. [Google Scholar] [CrossRef]
- Dananberg, H.J. Gait style as an etiology to chronic postural pain. Part II. Postural compensatory process. J. Am. Podiatr. Med. Assoc. 1993, 83, 615–624. [Google Scholar] [PubMed]
- Payne, C.; Chuter, V.; Miller, K. Sensitivity and specificity of the functional hallux limitus test to predict foot function. J. Am. Podiatr. Med. Assoc. 2002, 92, 269–271. [Google Scholar] [CrossRef]
- Stokes, I.A. Forces under the hallux valgus foot before and after surgery. Clin. Orthop. Relat. Res. 1979, 142, 64–72. [Google Scholar] [CrossRef]
- Nawoczenski, D.A.; Baumhauer, J.F.; Umberger, B.R. Relationship between clinical measurements and motion of the first metatarsophalangeal joint during gait. J. Bone Jt. Surg. 1999, 81, 370–376. [Google Scholar] [CrossRef]
- Nolan, K.J.; Hillstrom, H.J.; Sisto, S.A.; Elovic, E.P. First metatarsal phalangeal joint flexibility: A quantitative tool for evaluation of halux limitus. Clin. Biomech. 2008, 23, 703–704. [Google Scholar] [CrossRef]
- Okamura, K.; Egawa, K.; Ikeda, T.; Fukuda, K.; Kanai, S. Relationship between foot muscle morphology and severity of pronated foot deformity and foot kinematics during gait: A preliminary study. Gait Posture 2021, 86, 273–277. [Google Scholar] [CrossRef] [PubMed]
- Gatt, A.; Mifsud, T.; Chockalingam, N. Severity of pronation and classification of first metatarsophalangeal joint dorsiflexion increases the validity of the Hubscher Manoeuvre for the diagnosis of functional hallux limitus. Foot 2014, 24, 62–65. [Google Scholar] [CrossRef] [PubMed]
- Merker, J.; Hartmann, M.; Kreuzpointner, F.; Schwirtz, A.; Haas, J.P. Pathophysiology of juvenile idiopathic arthritis induced pes planovalgus in static and walking condition-A functional view using 3d gait analysis. Pediatr. Rheumatol. 2015, 13, 21. [Google Scholar] [CrossRef]
- Clough, J.G. Functional hallux limitus and lesser-metatarsal overload. J. Am. Podiatr. Med. Assoc. 2005, 95, 593–601. [Google Scholar] [CrossRef]
- Sánchez-Gómez, R.; Becerro-de-Bengoa-Vallejo, R.; Losa-Iglesias, M.E.; Calvo-Lobo, C.; Navarro-Flores, E.; Palomo-López, P.; Romero-Morales, C.; López-López, D. Reliability Study of Diagnostic Tests for Functional Hallux Limitus. Foot Ankle Int. 2020, 41, 457–462. [Google Scholar] [CrossRef]
- Durrant, B.; Chockalingam, N. Functional hallux limitus. J. Am. Podiatr. Med. Assoc. 2009, 99, 236–243. [Google Scholar] [CrossRef]
- Michaud, T.C.; Nawoczenski, D.A. The influence of two different types of foot orthoses on first metatarsophalangeal joint kinematics during gait in a single subject. J. Manip. Physiol. Ther. 2006, 29, 60–65. [Google Scholar] [CrossRef]
- de Bengoa Vallejo, R.B.; Iglesias, M.E.L.; Zeni, J.; Thomas, S. Reliability and repeatability of the portable EPS-platform digital pressure-plate system. J. Am. Podiatr. Med. Assoc. 2013, 103, 197–203. [Google Scholar]
- Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 2019, 13, S31–S34. [Google Scholar] [CrossRef]
- Holt, G.R. Declaration of Helsinki-the world’s document of conscience and responsibility. South. Med. J. 2014, 107, 407. [Google Scholar] [CrossRef] [PubMed]
- Halstead, J.; Redmond, A.C. Weight-bearing passive dorsiflexion of the hallux in standing is not related to hallux dorsiflexion during walking. J. Orthop. Sport. Phys. Ther. 2006, 36, 550–556. [Google Scholar] [CrossRef]
- Aquino, A.; Payne, C. Function of the windlass mechanism in excessively pronated feet. J. Am. Podiatr. Med. Assoc. 2001, 91, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Shurnas, P.S. Hallux Rigidus: Etiology, Biomechanics, and Nonoperative Treatment. Foot Ankle Clin. 2009, 14, 1–8. [Google Scholar] [CrossRef]
- Kunnasegaran, R.; Thevendran, G. Hallux Rigidus Nonoperative Treatment and Orthotics. Foot Ankle Clin. 2015, 20, 401–412. [Google Scholar] [CrossRef]
- Grady, J.F.; Axe, T.M.; Zager, E.J.; Sheldon, L.A. A retrospective analysis of 772 patients with hallux limitus. J. Am. Podiatr. Med. Assoc. 2002, 92, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Vanore, J.V.; Christensen, J.C.; Kravitz, S.R.; Schuberth, J.M.; Thomas, J.L.; Weil, L.S.; Zlotoff, H.J.; Couture, S.D. Diagnosis and treatment of first metatarsophalangeal joint disorders. Section 2: Hallux rigidus. J. Foot Ankle Surg. 2003, 42, 124–136. [Google Scholar] [CrossRef] [PubMed]
- Hanft, J.R.; Mason, E.T. A new radiographic classification for hallux limitus. J. Foot Ankle Surg. 1993, 32, 397–404. [Google Scholar]
- Munuera, P.V. Length of the sesamoids and their distance from the metatarsophalangeal joint space in feet with incipient Hallux limitus. J. Am. Podiatr. Med. Assoc. 2008, 98, 123–129. [Google Scholar] [CrossRef]
- Tzioupis, C.; Oliveto, A.; Grabherr, S.; Vallotton, J.; Riederer, B.M. Identification of the retrotalar pulley of the Flexor Hallucis Longus tendon. J. Anat. 2019, 235, 757–764. [Google Scholar] [CrossRef] [PubMed]
- Evans, R.D.L.; Averett, R.; Sanders, S. The association of hallux limitus with the accessory navicular. J. Am. Podiatr. Med. Assoc. 2002, 92, 359–365. [Google Scholar] [CrossRef] [PubMed]
- Hagedorn, T.J.; Dufour, A.B.; Riskowski, J.L.; Hillstrom, H.J.; Menz, H.B.; Casey, V.A.; Hannan, M.T. Foot Disorders, Foot Posture, and Foot Function: The Framingham Foot Study. PLoS ONE 2013, 8, e74364. [Google Scholar] [CrossRef]
- Shrader, J.A.; Siegel, K.L. Nonoperative management of functional hallux limitus in a patient with rheumatoid arthritis. Phys. Ther. 2003, 83, 831–843. [Google Scholar] [CrossRef]
- Bryant, A. Radiographic measurements and plantar pressure distribution in normal, hallux valgus and hallux limitus feet. Foot. 2000, 10, 18–22. [Google Scholar] [CrossRef]
- Gill, S.V.; Keimig, S.; Kelty-Stephen, D.; Hung, Y.C.; DeSilva, J.M. The relationship between foot arch measurements and walking parameters in children. BMC Pediatr. 2016, 16, 2. [Google Scholar] [CrossRef]

| Quantitative Descriptive Data | Total Group (n = 106) Mean ± SD (Range) | FHL (n = 53) Mean ± SD (Range) | Healthy (n = 53) Mean ± SD (Range) | p-Value |
|---|---|---|---|---|
| Age (years) | 9.47 ± 1.501 (6–12) | 9.81 ± 1.27 (8–12) | 9.13 ± 1.64 (6–12) | 0.031 † |
| Weight (kg) | 36.38 ± 11.31 (17.95–90.00) | 36.69 ± 8.50 (22.00–56.60) | 36.98 ± 13.63 (17.95–90.00) | 0.542 † |
| Height (cm) | 140.14 ± 11.44 (113.00–176.00) | 141.26 ± 9.50 (121.00–167.00) | 139.02 ± 13.10 (113.00–176.00) | 0.231 † |
| BMI (kg/m2) | 18.50 ± 3.91 (11.00–40.00) | 18.11 ± 2.81 (14.00–25.00) | 18.89 ± 4.77 (11.00–40.00) | 0.729 † |
| Sex (male/female) | 55/51 (51.9/48.1) | 23/30 (43.4/56.6) | 32/21 (60.4/39.6) | 0.120 ‡ |
| Foot Size | 35.63 ± 3.58 (15.00–44.0) | 36.18 ± 2.38 (30.0–43.0) | 35.09 ± 4.42 (15.00–44.0) | 0.099 † |
| Quantitative Descriptive Data | Total Group (n = 106) Mean ± SD (Range) | FHL (n = 53) Mean ± SD (Range) | Healthy (n = 53) Mean ± SD (Range) | p-Value |
|---|---|---|---|---|
| Left forefoot surface area (cm2) | 31.36 ± 10.83 (6–66) | 31.85 ± 9.39 (14–64) | 30.87 ± 12.17 (6–66) | 0.450 † |
| Right forefoot surface area (cm2) | 30.08 ± 12.33 (0–76) | 30.06 ± 11.54 (8–76) | 30.11 ± 13.18 (0–66) | 0.889 † |
| Left rearfoot surface area (cm2) | 32.46 ± 10.04 (17–70) | 32.66 ± 9.49 (17–55) | 32.26 ± 10.65 (19–70) | 0.565 † |
| Right rearfoot surface area (cm2) | 29.95 ± 10.51 (12–64) | 29.11 ± 8.77 (15–49) | 30.79 ± 12.03 (12–64) | 0.697 † |
| Left forefoot force (%) | 20.17 ± 7.12 (3–46) | 20.58 ± 6.50 (7–39) | 19.75 ± 7.72 (3–46) | 0.360 † |
| Right forefoot force (%) | 18.33 ± 6.80 (0–38) | 17.81 ± 6.20 (5–38) | 18.85 ± 7.37 (0–33) | 0.233 † |
| Left rearfoot force (%) | 33.50 ± 8.49 (17–63) | 33.42 ± 7.49 (17–51) | 33.58 ± 9.45 (17–63) | 0.907 † |
| Right rearfoot force (%) | 27.98 ± 7.07 (6–48) | 28.27 ± 6.46 (15.00–42) | 27.70 ± 7.69 (6–48) | 0.716 † |
| Left forefoot distribution (%) | 37.79 ± 12.41 (5–72) | 38.19 ± 11.25 (15–66) | 37.40 ± 13.57 (5–72) | 0.704 † |
| Right forefoot distribution (%) | 39.40 ± 13.77 (0–79) | 38.47 ± 11.79 (12–71) | 40.32 ± 15.56 (0–79) | 0.349 † |
| Left rearfoot distribution (%) | 62.21 ± 12.41 (28–95) | 61.81 ± 11.25 (34–85) | 62.60 ± 13.57 (28–95) | 0.704 † |
| Right rearfoot distribution (%) | 59.75 ± 14.80 (7–100) | 59.66 ± 14.21 (7–88) | 59.85 ± 15.50 (21–100) | 0.752 † |
| Left surface area (cm2) | 64.10 ± 18.87 (26–136) | 64.89 ± 15.92 (31–91) | 63.32 ± 21.55 (26–136) | 0.321 † |
| Right surface area (cm2) | 60.13 ± 20.33 (14– 130) | 59.17 ± 17.11 (32–107) | 61.09 ± 23.24 (14–130) | 0.899 † |
| Left maximum plantar pressure (kPa) | 813.63 ± 212.67 (73–1357) | 816.19 ± 184.59 (360.10–1357) | 811.06 ± 239.25 (73–1217) | 0.830 † |
| Right maximum plantar pressure (kPa) | 754.59 ± 185.56 (332.42–1424.00) | 783.28 ± 183.47 (484.40–1357.00) | 725.91 ± 184.89 (332.42–1424.00) | 0.129 † |
| Left medium plantar pressure (kPa) | 314.88 ± 64.80 (146.00–506.00) | 314.50 ± 60.15 (182.50–506.00) | 315.26 ± 69.72 (146–463.00) | 0.691 † |
| Right medium plantar pressure (kPa) | 323.21 ± 333.54 (151.00–3671.00) | 294.21 ± 57.25 (191–437) | 352.21 ± 468.67 (151.00–3671.00) | 0.793 † |
| Left force (%) | 53.81 ± 6.72 (34.00–70.00) | 54.08 ± 6.37 (42–70) | 53.55 ± 7.10 (34.00–69.00) | 0.628 † |
| Right force (%) | 46.28 ± 6.72 (30–66) | 45.92 ± 6.37 (30–58) | 46.64 ± 7.09 (31–66) | 0.498 † |
| Left weight (kg) | 19.76± 6.25 (9–44) | 19.96 ± 5.60 (9–31) | 19.57 ± 6.89 (11–44) | 0.350 † |
| Right weight (kg) | 17.11 ± 6.29 (6–46) | 16.83 ± 4.63 (9–26) | 17.40 ± 7.62 (6–46) | 0.730 † |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cuevas-Martínez, C.; Becerro-de-Bengoa-Vallejo, R.; Losa-Iglesias, M.E.; Casado-Hernández, I.; Turné-Cárceles, O.; Pérez-Palma, L.; Martiniano, J.; Gómez-Salgado, J.; López-López, D. Analysis of Static Plantar Pressures in School-Age Children with and without Functional Hallux Limitus: A Case-Control Study. Bioengineering 2023, 10, 628. https://doi.org/10.3390/bioengineering10060628
Cuevas-Martínez C, Becerro-de-Bengoa-Vallejo R, Losa-Iglesias ME, Casado-Hernández I, Turné-Cárceles O, Pérez-Palma L, Martiniano J, Gómez-Salgado J, López-López D. Analysis of Static Plantar Pressures in School-Age Children with and without Functional Hallux Limitus: A Case-Control Study. Bioengineering. 2023; 10(6):628. https://doi.org/10.3390/bioengineering10060628
Chicago/Turabian StyleCuevas-Martínez, Claudia, Ricardo Becerro-de-Bengoa-Vallejo, Marta Elena Losa-Iglesias, Israel Casado-Hernández, Oriol Turné-Cárceles, Laura Pérez-Palma, João Martiniano, Juan Gómez-Salgado, and Daniel López-López. 2023. "Analysis of Static Plantar Pressures in School-Age Children with and without Functional Hallux Limitus: A Case-Control Study" Bioengineering 10, no. 6: 628. https://doi.org/10.3390/bioengineering10060628
APA StyleCuevas-Martínez, C., Becerro-de-Bengoa-Vallejo, R., Losa-Iglesias, M. E., Casado-Hernández, I., Turné-Cárceles, O., Pérez-Palma, L., Martiniano, J., Gómez-Salgado, J., & López-López, D. (2023). Analysis of Static Plantar Pressures in School-Age Children with and without Functional Hallux Limitus: A Case-Control Study. Bioengineering, 10(6), 628. https://doi.org/10.3390/bioengineering10060628












