Spatial Scattering Radiation to the Radiological Technologist during Medical Mobile Radiography
Abstract
1. Introduction
2. Materials and Methods
2.1. Experimental Setup
2.2. Measurement Points
2.3. X-ray Conditions
2.4. Radiation Measurements
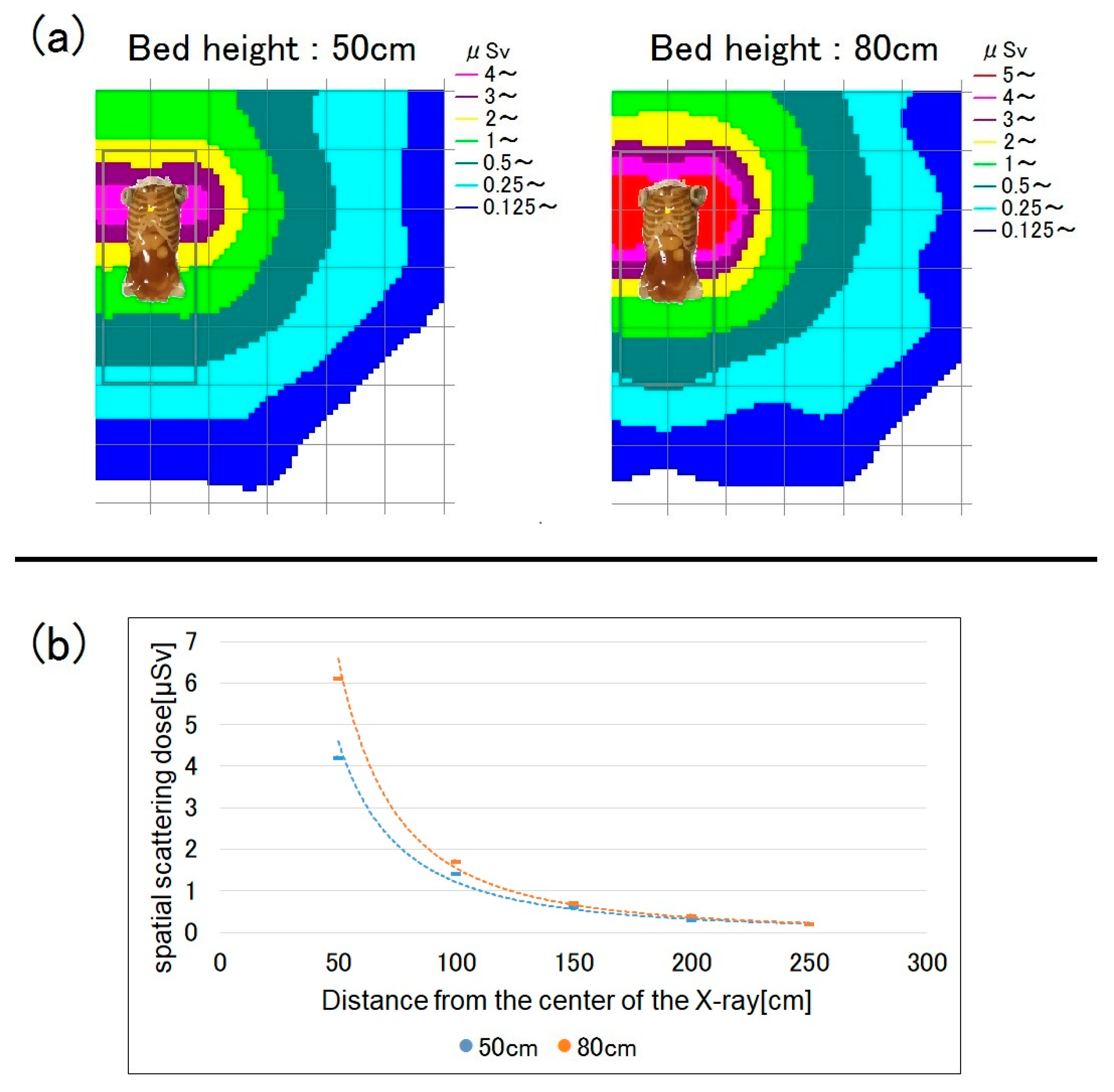
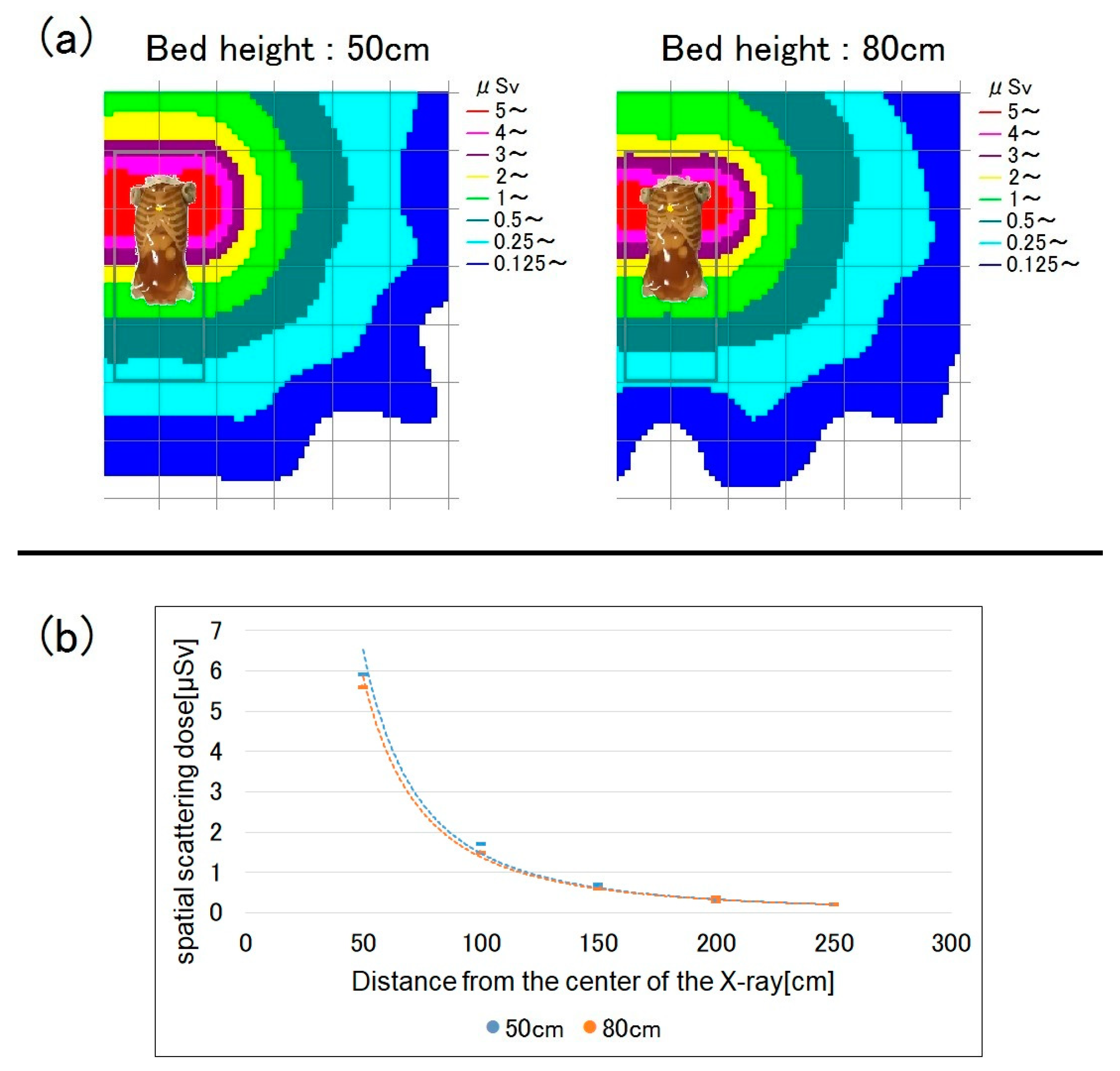
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- International Commission on Radiological Protection (ICRP). Radiological Protection in Cardiology; ICRP Publication 120; Elsevier: Amsterdam, The Netherlands, 2013; Volume 42, Available online: https://journals.sagepub.com/doi/pdf/10.1177/ANIB_42_1 (accessed on 20 December 2022).
- Matsunaga, Y.; Haba, T.; Kobayashi, M.; Suzuki, S.; Asada, Y.; Chida, K. Novel pregnant model phantoms for measurement of foetal radiation dose in x-ray examinations. J. Radiol. Prot. 2021, 41, N12–N21. [Google Scholar] [CrossRef] [PubMed]
- Nemoto, M.; Chida, K. Reducing the breast cancer risk and radiation dose of radiography for scoliosis in children: A phantom study. Diagnostics 2020, 10, 753. [Google Scholar] [CrossRef] [PubMed]
- Inaba, Y.; Nakamura, M.; Zuguchi, M.; Chida, K. Development of novel real-time radiation systems using 4-channel sensors. Sensors 2020, 20, 2741. [Google Scholar] [CrossRef]
- Matsuzaki, S.; Moritake, T.; Morota, K.; Nagamoto, K.; Nakagami, K.; Kuriyama, T.; Kunugita, N. Development and assessment of an educational application for the proper use of ceiling-suspended radiation shielding screens in angiography rooms using augmented reality technology. Eur. J. Radiol. 2021, 143, 109925. [Google Scholar] [CrossRef] [PubMed]
- Sato, T.; Eguchi, Y.; Yamazaki, C.; Hino, T.; Saida, T.; Chida, K. Development of a New Radiation Shield for the Face and Neck of IVR Physicians. Bioengineering 2022, 9, 354. [Google Scholar] [CrossRef]
- Chida, K.; Takahashi, T.; Ito, D.; Shimura, H.; Takeda, K.; Zuguchi, M. Clarifying and visualizing sources of staff-received scattered radiation in interventional procedures. Am. J. Roentgenol. 2011, 197, W900–W903. [Google Scholar] [CrossRef] [PubMed]
- Koenig, A.; Maas, J.; Viniol, S.; Etzel, R.; Fiebich, M.; Thomas, R.; Mahnken, A. Scatter radiation reduction with a radiation-absorbing pad in interventional radiology examinations. Eur. J. Radiol. 2020, 132, 109245. [Google Scholar] [CrossRef] [PubMed]
- Chida, K. What are useful methods to reduce occupational radiation exposure among radiological medical workers, especially for interventional radiology personnel? Radiol. Phys. Technol. 2022, 15, 101–115. [Google Scholar] [CrossRef]
- Chida, K.; Morishima, Y.; Inaba, Y.; Taura, M.; Ebata, A.; Takeda, K.; Shimura, H.; Zuguchi, M. Physician-received scatter radiation with angiography systems used for interventional radiology: Comparison among many X-ray systems. Radiat. Prot. Dosim. 2011, 149, 410–416. [Google Scholar] [CrossRef]
- Matsubara, K. Assessment of Radiation Dose in Medical Imaging and Interventional Radiology Procedures for Patient and Staff Safety. Diagnostics 2021, 11, 1116. [Google Scholar] [CrossRef]
- International Commission on Radiological Protection (ICRP). Avoidance of Radiation Injuries from Medical Interventional Procedures; ICRP Publication 85; Pergamon: Oxford, UK, 2000; Volume 30, Available online: https://journals.sagepub.com/doi/pdf/10.1177/ANIB_30_2 (accessed on 20 December 2022).
- Chida, K.; Ohno, T.; Kakizaki, S.; Takegawa, M.; Yuuki, H.; Nakada, M.; Takahashi, S.; Zuguchi, M. Radiation dose to the pediatric cardiac catheterization and intervention patient. Am. J. Roentgenol. 2010, 195, 1175–1179. [Google Scholar] [CrossRef] [PubMed]
- Haga, Y.; Chida, K.; Sota, M.; Kaga, Y.; Abe, M.; Inaba, Y.; Suzuki, M.; Meguro, T.; Zuguchi, M. Hybrid operating room system for the treatment of thoracic and abdominal aortic aneurysms: Evaluation of the radiation dose received by patients. Diagnostics 2020, 10, 846. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, M.; Chida, K.; Zuguchi, M. Novel Dosimeter Using a Nontoxic Phosphor for Real-Time Monitoring of Patient Radiation Dose in Interventional Radiology. AJR Am. J. Roentgenol. 2015, 205, W202–W206. [Google Scholar] [CrossRef] [PubMed]
- Kato, M.; Chida, K.; Sato, T.; Oosaka, H.; Tosa, T.; Munehisa, M.; Kadowaki, K. The necessity of follow-up for radiation skin injuries in patients after percutaneous coronary interventions: Radiation skin injuries will often be overlooked clinically. Acta Radiol. 2012, 53, 1040–1044. [Google Scholar] [CrossRef] [PubMed]
- Vañó, E.; Gonzalez, L.; Fernández, J.M.; Haskal, Z.J. Eye lens exposure to radiation in interventional suites: Caution is warranted. Radiology 2008, 248, 945–953. [Google Scholar] [CrossRef]
- Coppeta, L.; Pietroiusti, A.; Neri, A.; Spataro, A.; De Angelis, E.; Perrone, S.; Magrini, A. Risk of radiation-induced lens opacities among surgeons and interventional medical staff. Radiol. Phys. Technol. 2019, 12, 26–29. [Google Scholar] [CrossRef]
- Vañó, E.; González, L.; Beneytez, F.; Moreno, F. Lens injuries induced by occupational exposure in non-optimized interventional radiology laboratories. Br. J. Radiol. 1998, 71, 728–733. [Google Scholar] [CrossRef]
- Omar, A.; Kadesjö, N.; Palmgren, C.; Marteinsdottir, M.; Segerdahl, T.; Fransson, A. Assessment of the occupational eye lens dose for clinical staff in interventional radiology, cardiology and neuroradiology. J. Radiol. Prot. 2017, 37, 145–159. [Google Scholar] [CrossRef]
- Vigneux, G.; Pirkkanen, J.; Laframboise, T.; Prescott, H.; Tharmalingam, S.; Thome, C. Radiation-Induced Alterations in Proliferation, Migration, and Adhesion in Lens Epithelial Cells and Implications for Cataract Development. Bioengineering 2022, 9, 29. [Google Scholar] [CrossRef]
- Santos, W.S.; Maia, A.F. Evaluation of personal doses associated with the use of mobile X-rays in a Brazilian hospital. Radiat. Prot. Dosim. 2012, 150, 188–191. [Google Scholar] [CrossRef]
- Fernández, R.; Moreno-Torres, M.; Contreras, A.M.; Núñez, M.I.; Guirado, D.; Peñas, L. Patient and staff dosimetry during radiographic procedures in an intensive care unit. J. Radiol. Prot. 2015, 35, 727–732. [Google Scholar] [CrossRef] [PubMed]
- Trinh, A.M.; Schoenfeld, A.H.; Levin, T.L. Scatter radiation from chest radiographs: Is there a risk to infants in a typical NICU? Pediatr. Radiol. 2010, 40, 704–707. [Google Scholar] [CrossRef] [PubMed]
- Rubinowitz, A.N.; Siegel, M.D.; Tocino, I. Thoracic imaging in the ICU. Crit. Care Clin. 2007, 23, 539–573. [Google Scholar] [CrossRef] [PubMed]
- Eisenhuber, E.; Schaefer-Prokop, C.M.; Prosch, H.; Schima, W. Bedside chest radiography. Respir. Care 2012, 57, 427–443. [Google Scholar] [CrossRef]
- Eklund, K.; Klefsgård, R.; Ivarsson, B.; Geijer, M. Positive experience of a mobile radiography service in nursing homes. Gerontology 2012, 58, 107–111. [Google Scholar] [CrossRef]
- Brady, Z.; Scoullar, H.; Grinsted, B.; Ewert, K.; Kavnoudias, H.; Jarema, A.; Crocker, J.; Wills, R.; Houston, G.; Law, M.; et al. Technique, radiation safety and image quality for chest X-ray imaging through glass and in mobile settings during the COVID-19 pandemic. Phys. Eng. Sci. Med. 2020, 43, 765–779. [Google Scholar] [CrossRef]
- Yeung, P.; Pinson, J.A.; Lawson, M.; Leong, C.; Badawy, M.K. COVID-19 pandemic and the effect of increased utilisation of mobile X-ray examinations on radiation dose to radiographers. J. Med. Radiat. Sci. 2022, 69, 147–155. [Google Scholar] [CrossRef]
- International Commission on Radiological Protection (ICRP). ICRP Statement on Tissue Reactions/Early and Late Effects of Radiation in Normal Tissues and Organs, Threshold Doses for Tissue Reactions in a Radiation Protection Context; ICRP publication 118 Ann; Elsevier: Amsterdam, The Netherlands, 2012; Volume 41, pp. 1–322. Available online: https://www.icrp.org/publication.asp?id=ICRP%20Publication%20118 (accessed on 30 November 2022).
- Ainsbury, E.A.; Barnard, S.; Bright, S.; Dalke, C.; Jarrin, M.; Kunze, S.; Tanner, R.; Dynlacht, J.R.; Quinlan, R.A.; Graw, J.; et al. Ionizing radiation induced cataracts: Recent biological and mechanistic developments and perspectives for future research. Mutat. Res. Rev. Mutat. Res 2016, 770 Pt B, 238–261. [Google Scholar] [CrossRef]
- Haga, Y.; Chida, K.; Kaga, Y.; Sota, M.; Meguro, T.; Zuguchi, M. Occupational eye dose in interventional cardiology procedures. Sci. Rep. 2017, 7, 569. [Google Scholar] [CrossRef]
- Haga, Y.; Chida, K.; Kimura, Y.; Yamada, S.; Sota, M.; Abe, M.; Kaga, Y.; Meguro, T.; Zuguchi, M. Radiation eye dose to medical staff during respiratory endoscopy under X-ray fluoroscopy. J. Radiat. Res. 2020, 61, 691–696. [Google Scholar] [CrossRef]
- Kato, M.; Chida, K.; Ishida, T.; Sasaki, F.; Toyoshima, H.; Oosaka, H.; Terata, K.; Abe, Y.; Kinoshita, T. Occupational radiation exposure dose of the eye in department of cardiac arrhythmia physician. Radiat. Prot. Dosim. 2019, 187, 361–368. [Google Scholar] [CrossRef] [PubMed]
- Kato, M.; Chida, K.; Ishida, T.; Toyoshima, H.; Yoshida, Y.; Yoshioka, S.; Moroi, J.; Kinoshita, T. Occupational radiation exposure of the eye in neurovascular interventional physician. Radiat. Prot. Dosim. 2019, 185, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Morishima, Y.; Chida, K.; Meguro, T. Effectiveness of additional lead shielding to protect staff from scattering radiation during endoscopic retrograde cholangiopancreatography procedures. J. Radiat. Res. 2018, 59, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Cornacchia, S.; Errico, R.; La Tegola, L. The new lens dose limit: Implication for occupational radiation protection. Radiol. Med. 2019, 124, 728–735. [Google Scholar] [CrossRef]
- Ishii, H.; Haga, Y.; Sota, M.; Inaba, Y.; Chida, K. Performance of the DOSIRIS™ eye lens dosimeter. J. Radiol. Prot. 2019, 39, N19–N26. [Google Scholar] [CrossRef]
- Chiang, H.W.; Liu, Y.L.; Chen, T.R.; Chen, C.L.; Chiang, H.J.; Chao, S.Y. Scattered radiation doses absorbed by technicians at different distances from X-ray exposure: Experiments on prosthesis. Biomed. Mater. Eng. 2015, 26 (Suppl. S1), 641–650. [Google Scholar] [CrossRef]
- Fujibuchi, T. Radiation protection education using virtual reality for the isualizeion of scattered distributions during radiological examinations. J. Radiol. Prot. 2021, 41, S317–S328. [Google Scholar] [CrossRef]
- Nishi, K.; Fujibuchi, T.; Yoshinaga, T. Development of an application to visualize the spread of scattered radiation in radiography using augmented reality. J. Radiol. Prot. 2020, 40, 1299–1310. [Google Scholar] [CrossRef]
- Takata, T.; Nakabayashi, S.; Kondo, H.; Yamamoto, M.; Furui, S.; Shiraishi, K.; Kobayashi, T.; Oba, H.; Okamoto, T.; Kotoku, J. Mixed reality visualization of radiation dose for health professionals and patients in interventional radiology. J. Med. Syst. 2021, 45, 38. [Google Scholar] [CrossRef]
- Alnewaini, Z.; Langer, E.; Schaber, P.; David, M.; Kretz, D.; Steil, V.; Hesser, J. Real-time, ray casting-based scatter dose estimation for c-arm x-ray system. J. Appl. Clin. Med. Phys. 2017, 18, 144–153. [Google Scholar] [CrossRef]
- Koukorava, C.; Farah, J.; Struelens, L.; Clairand, I.; Donadille, L.; Vanhavere, F.; Dimitriou, P. Efficiency of radiation protection equipment in interventional radiology: A systematic Monte Carlo study of eye lens and whole body doses. J. Radiol. Prot. 2014, 34, 509–528. [Google Scholar] [CrossRef]
- Papadimitroulas, P. Dosimetry applications in GATE Monte Carlo toolkit. Phys. Med. 2017, 41, 136–140. [Google Scholar] [CrossRef] [PubMed]
- Platten, D.J. A Monte Carlo study of the energy spectra and transmission characteristics of scattered radiation from x-ray computed tomography. J. Radiol. Prot. 2014, 34, 445–456. [Google Scholar] [CrossRef] [PubMed]
- Vlachos, I.; Tsantilas, X.; Kalyvas, N.; Delis, H.; Kandarakis, I.; Panayiotakis, G. Measuring scatter radiation in diagnostic X rays for radiation protection purposes. Radiat. Prot. Dosim. 2015, 165, 382–385. [Google Scholar] [CrossRef] [PubMed]
- Trout, E.D.; Kelley, J.P.; Kellner, J. Scattered radiation from bedside roentgen examinations. Am. J. Roentgenol. Radium. Ther. Nucl. Med. 1972, 114, 832–836. [Google Scholar] [CrossRef] [PubMed]
- Matsunaga, Y.; Chida, K.; Kondo, Y.; Kobayashi, K.; Kobayashi, M.; Minami, K.; Suzuki, S.; Asada, Y. Diagnostic reference levels and achievable doses for common computed tomography examinations: Results from the Japanese nationwide dose survey. Br. J. Radiol. 2019, 92, 20180290. [Google Scholar] [CrossRef] [PubMed]
- Chida, K.; Inaba, Y.; Morishima, Y.; Taura, M.; Ebata, A.; Yanagawa, I.; Takeda, K.; Zuguchi, M. Comparison of dose at an interventional reference point between the displayed estimated value and measured value. Radiol. Phys. Technol. 2011, 4, 189–193. [Google Scholar] [CrossRef]
- Inaba, Y.; Nakamura, M.; Chida, K.; Zuguchi, M. Effectiveness of a novel real-time dosimeter in interventional radiology: A comparison of new and old radiation sensors. Radiol. Phys. Technol. 2018, 11, 445–450. [Google Scholar] [CrossRef]
- Ishii, H.; Chida, K.; Satsurai, K.; Haga, Y.; Kaga, Y.; Abe, M.; Inaba, Y.; Zuguchi, M. Occupational eye dose correlation with neck dose and patient-related quantities in interventional cardiology procedures. Radiol. Phys. Technol. 2021, 15, 54–62. [Google Scholar] [CrossRef]
- Inaba, Y.; Chida, K.; Kobayashi, R.; Kaga, Y.; Zuguchi, M. Fundamental study of a real-time occupational dosimetry system for interventional radiology staff. J. Radiol. Prot. 2014, 34, 65–71. [Google Scholar] [CrossRef]
- Chida, K.; Morishima, Y.; Masuyama, H.; Chiba, H.; Katahira, Y.; Inaba, Y.; Mori, I.; Maruoka, S.; Takahashi, S.; Kohzuki, M.; et al. Effect of radiation monitoring method and formula differences on estimated physician dose during percutaneous coronary intervention. Acta Radiol. 2009, 50, 170–173. [Google Scholar] [CrossRef] [PubMed]
- Morishima, Y.; Chida, K.; Katahira, Y. The effectiveness of additional lead-shielding drape and low pulse rate fluoroscopy in protecting staff from scatter radiation during cardiac resynchronization therapy (CRT). Jpn. J. Radiol. 2019, 37, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Chida, K.; Inaba, Y.; Masuyama, H.; Yanagawa, I.; Mori, I.; Saito, H.; Maruoka, S.; Zuguchi, M. Evaluating the performance of a MOSFET dosimeter at diagnostic X-ray energies for interventional radiology. Radiol. Phys. Technol. 2009, 2, 58–61. [Google Scholar] [CrossRef] [PubMed]
- Chida, K.; Saito, H.; Otani, H.; Kohzuki, M.; Takahashi, S.; Yamada, S.; Shirato, K.; Zuguchi, M. Relationship between fluoroscopic time, dose—Area product, body weight, and maximum radiation skin dose in cardiac interventional procedures. Am. J. Roentgenol. 2006, 186, 774–778. [Google Scholar] [CrossRef]
- Kato, M.; Chida, K.; Sato, T.; Oosaka, H.; Tosa, T.; Kadowaki, K. Evaluating the maximum patient radiation dose in cardiac interventional procedures. Radiat. Prot. Dosim. 2011, 143, 69–73. [Google Scholar] [CrossRef] [PubMed]
- Inaba, Y.; Chida, K.; Murabayashi, Y.; Endo, M.; Otomo, K.; Zuguchi, M. An initial investigation of a wireless patient radiation dosimeter for use in interventional radiology. Radiol. Phys. Technol. 2020, 13, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Chida, K.; Kato, M.; Inaba, Y.; Kobayashi, R.; Nakamura, M.; Abe, Y.; Zuguchi, M. Real-time patient radiation dosimeter for use in interventional radiology. Phys. Med. 2016, 32, 1475–1478. [Google Scholar] [CrossRef]
- Ishii, H.; Chida, K.; Satsurai, K.; Haga, Y.; Kaga, Y.; Abe, M.; Inaba, Y.; Zuguchi, M. A phantom study to determine the optimal placement of eye dosemeters on interventional cardiology staff. Radiat. Prot. Dosim. 2019, 185, 409–413. [Google Scholar] [CrossRef]
- Inaba, Y.; Hitachi, S.; Watanuki, M.; Chida, K. Occupational radiation dose to eye lenses in CT-guided interventions using MDCT-fluoroscopy. Diagnostics 2021, 11, 646. [Google Scholar] [CrossRef]
- Inaba, Y.; Hitachi, S.; Watanuki, M.; Chida, K. Radiation Eye Dose for Physicians in CT Fluoroscopy-Guided Biopsy. Tomography 2022, 8, 438–446. [Google Scholar] [CrossRef]
- Chida, K.; Kaga, Y.; Haga, Y.; Kataoka, N.; Kumasaka, E.; Meguro, T.; Zuguchi, M. Occupational dose in interventional radiology procedures. Am. J. Roentgenol. 2013, 200, 138–141. [Google Scholar] [CrossRef] [PubMed]
- Chida, K.; Kato, M.; Kagaya, Y.; Zuguchi, M.; Saito, H.; Ishibashi, T.; Takahashi, S.; Yamada, S.; Takai, Y. Radiation dose and radiation protection for patients and physicians during interventional procedure. J. Radiat. Res. 2010, 51, 97–105. [Google Scholar] [CrossRef]
- Endo, M.; Haga, Y.; Sota, M.; Tanaka, A.; Otomo, K.; Murabayashi, Y.; Abe, M.; Kaga, Y.; Inaba, Y.; Suzuki, M.; et al. Evaluation of novel X-ray protective eyewear in reducing the eye dose to interventional radiology physicians. J. Radiat. Res. 2021, 62, 414–419. [Google Scholar] [CrossRef] [PubMed]
- Kato, M.; Chida, K.; Munehisa, M.; Sato, T.; Inaba, Y.; Suzuki, M.; Zuguchi, M. Non-Lead Protective Aprons for the Protection of Interventional Radiology Physicians from Radiation Exposure in Clinical Settings: An Initial Study. Diagnostics 2021, 11, 1613. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, U.; Walsh, C.; Gallagher, A.; Dowling, A.; Guiney, M.; Ryan, J.M.; McEniff, N.; O’Reilly, G. Occupational radiation dose to eyes from interventional radiology procedures in light of the new eye lens dose limit from the International Commission on Radiological Protection. Br. J. Radiol. 2015, 88, 20140627. [Google Scholar] [CrossRef] [PubMed]
- Zuguchi, M.; Chida, K.; Taura, M.; Inaba, Y.; Ebata, A.; Yamada, S. Usefulness of non-lead aprons in radiation protection for physicians performing interventional procedures. Radiat. Prot. Dosim. 2008, 131, 531–534. [Google Scholar] [CrossRef]
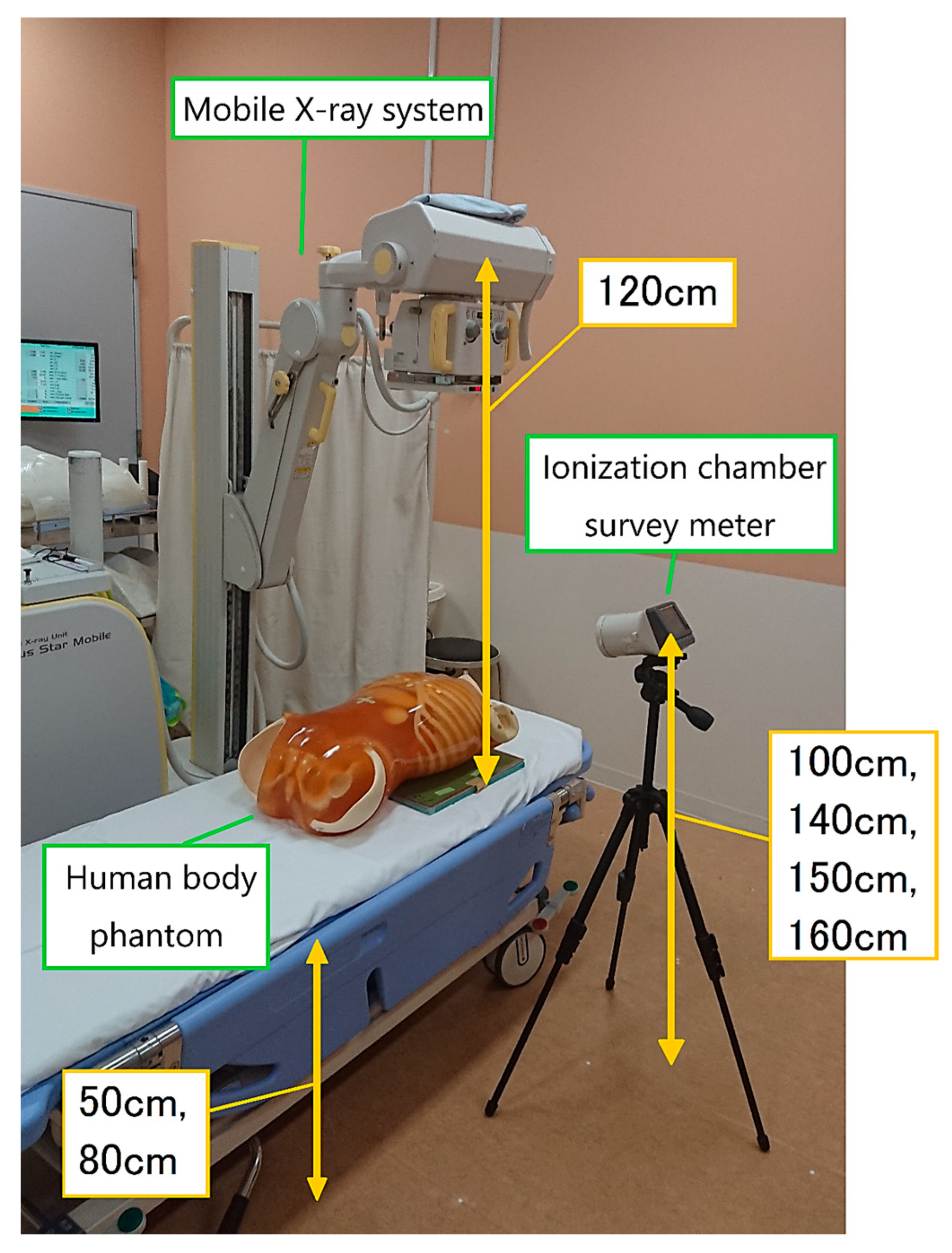
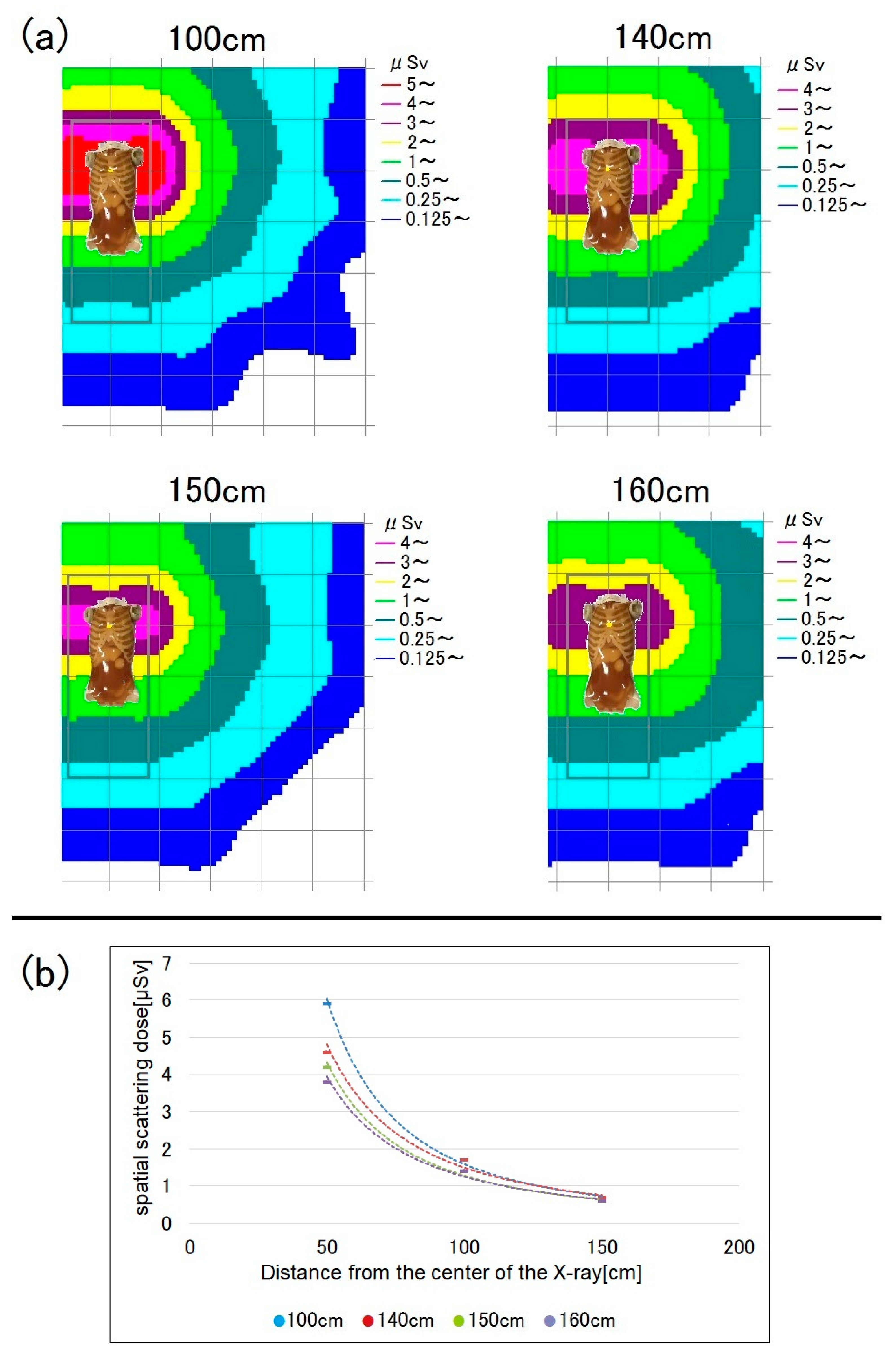
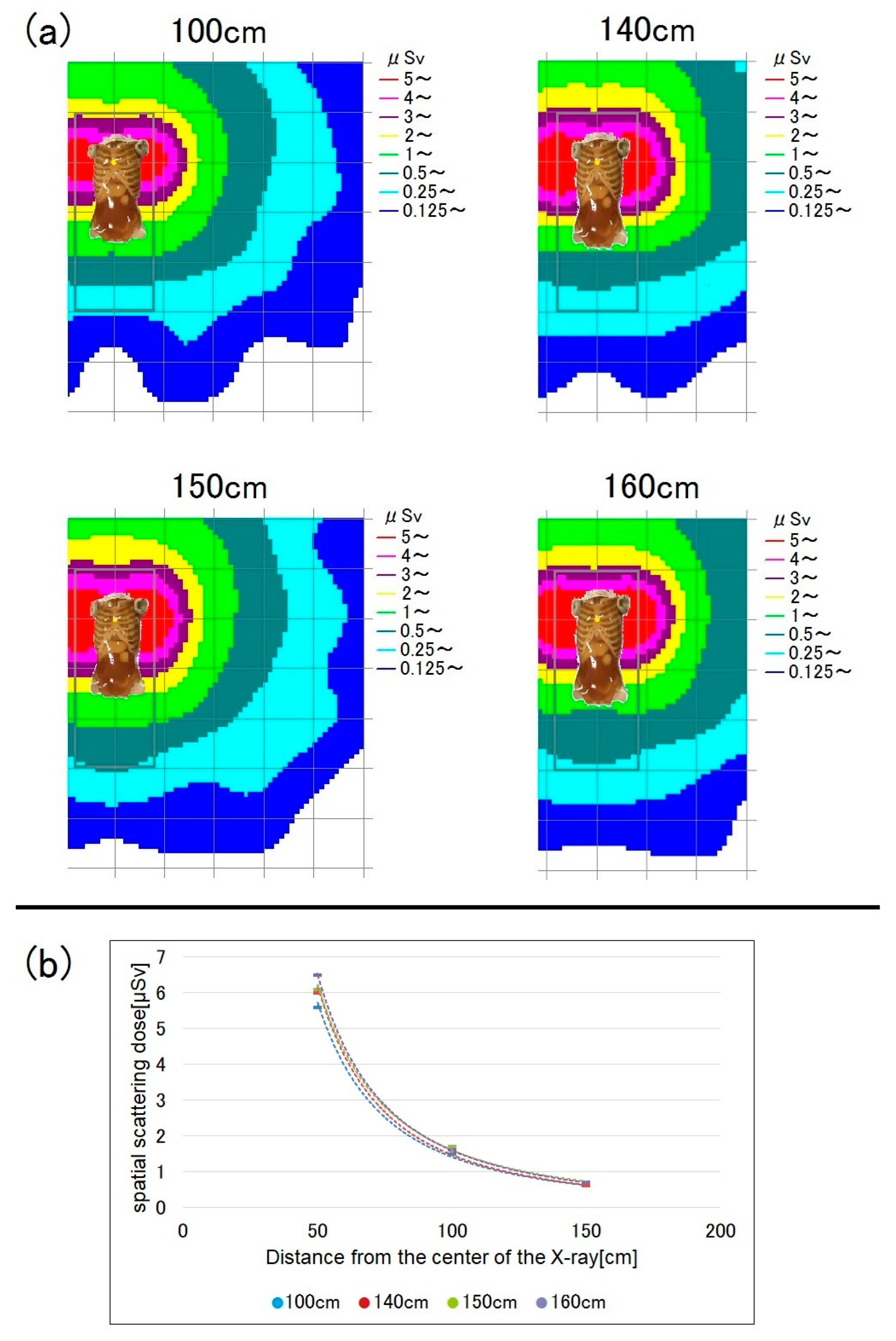
 ) were separated by a distance of 50 cm. We measured the scattered dose during mobile radiography according to the bed and measurement point heights.
) were separated by a distance of 50 cm. We measured the scattered dose during mobile radiography according to the bed and measurement point heights.
 ) were separated by a distance of 50 cm. We measured the scattered dose during mobile radiography according to the bed and measurement point heights.
) were separated by a distance of 50 cm. We measured the scattered dose during mobile radiography according to the bed and measurement point heights.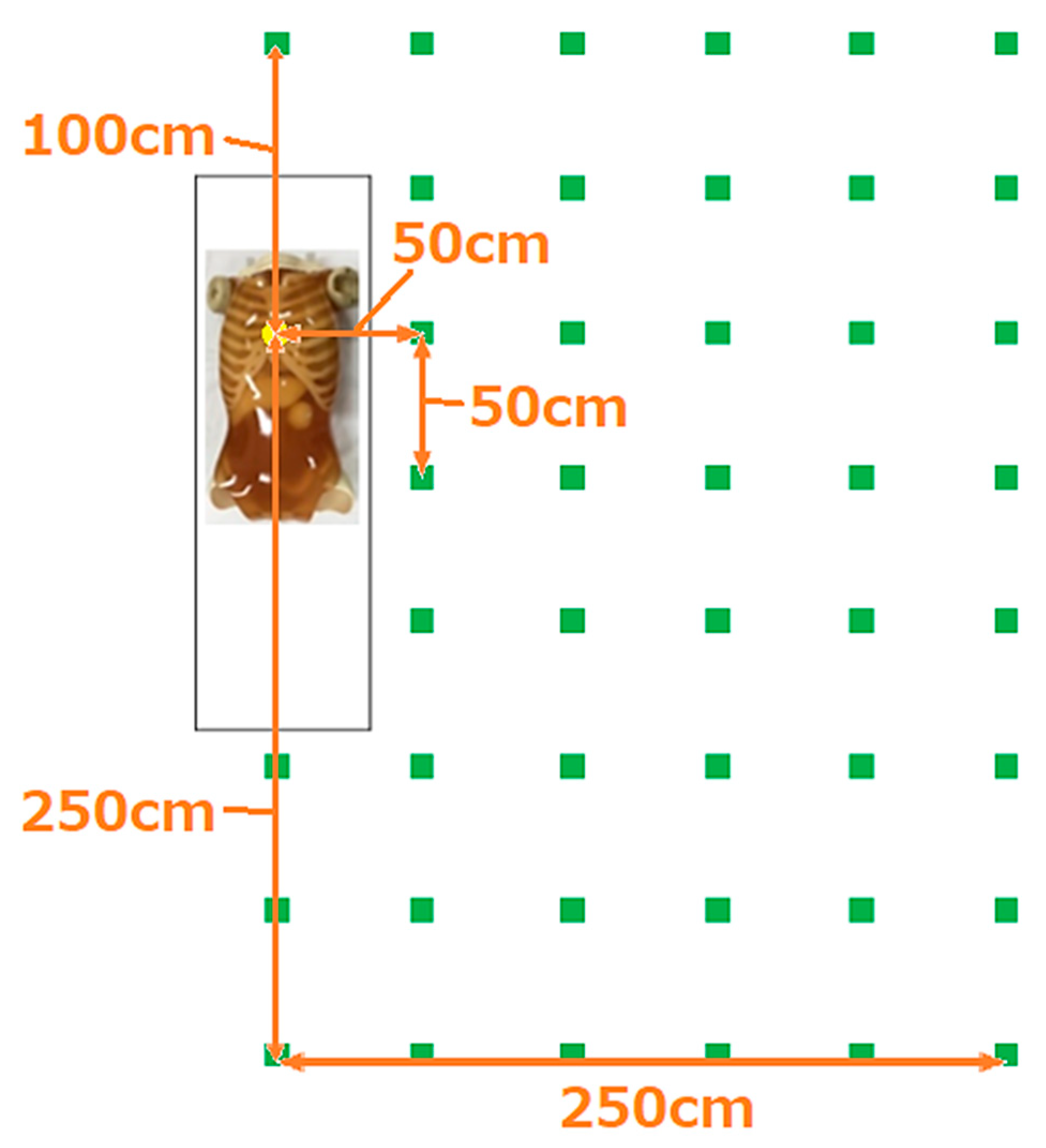

| Distance from the Center of the X-ray | |||||
|---|---|---|---|---|---|
| 50 cm | 100 cm | 150 cm | 200 cm | 250 cm | |
| Scattered radiation dose by bed height (measurement height: 150 cm) | |||||
| 50 cm | 5.9 ± 0 | 1.7 ± 0 | 0.7 ± 0 | 0.3 ± 0 | 0.2 ± 0 |
| 80 cm | 5.6 ± 0 | 1.5 ± 0 | 0.6 ± 0 | 0.33 ± 0.05 | 0.2 ± 0 |
| Scattered radiation dose by measurement height (bed height: 50 cm) | |||||
| 100 cm | 5.9 ± 0 | 1.7 ± 0 | 0.7 ± 0 | 0.3 ± 0 | 0.2 ± 0 |
| 140 cm | 4.6 ± 0 | 1.7 ± 0 | 0.7 ± 0 | - | - |
| 150 cm | 4.2 ± 0 | 1.4 ± 0 | 0.6 ± 0 | 0.3 ± 0 | 0.2 ± 0 |
| 160 cm | 3.8 ± 0 | 1.4 ± 0 | 0.6 ± 0 | - | - |
| Scattered radiation dose by measurement height (bed height: 80 cm) | |||||
| 100 cm | 5.6 ± 0 | 1.5 ± 0 | 0.6 ± 0 | 0.33 ± 0.05 | 0.2 ± 0 |
| 140 cm | 6.0 ± 0 | 1.6 ± 0 | 0.6 ± 0 | - | - |
| 150 cm | 6.1 ± 0 | 1.7 ± 0 | 0.7 ± 0 | 0.4 ± 0 | 0.2 ± 0 |
| 160 cm | 6.5 ± 0 | 1.6 ± 0 | 0.7 ± 0 | - | - |
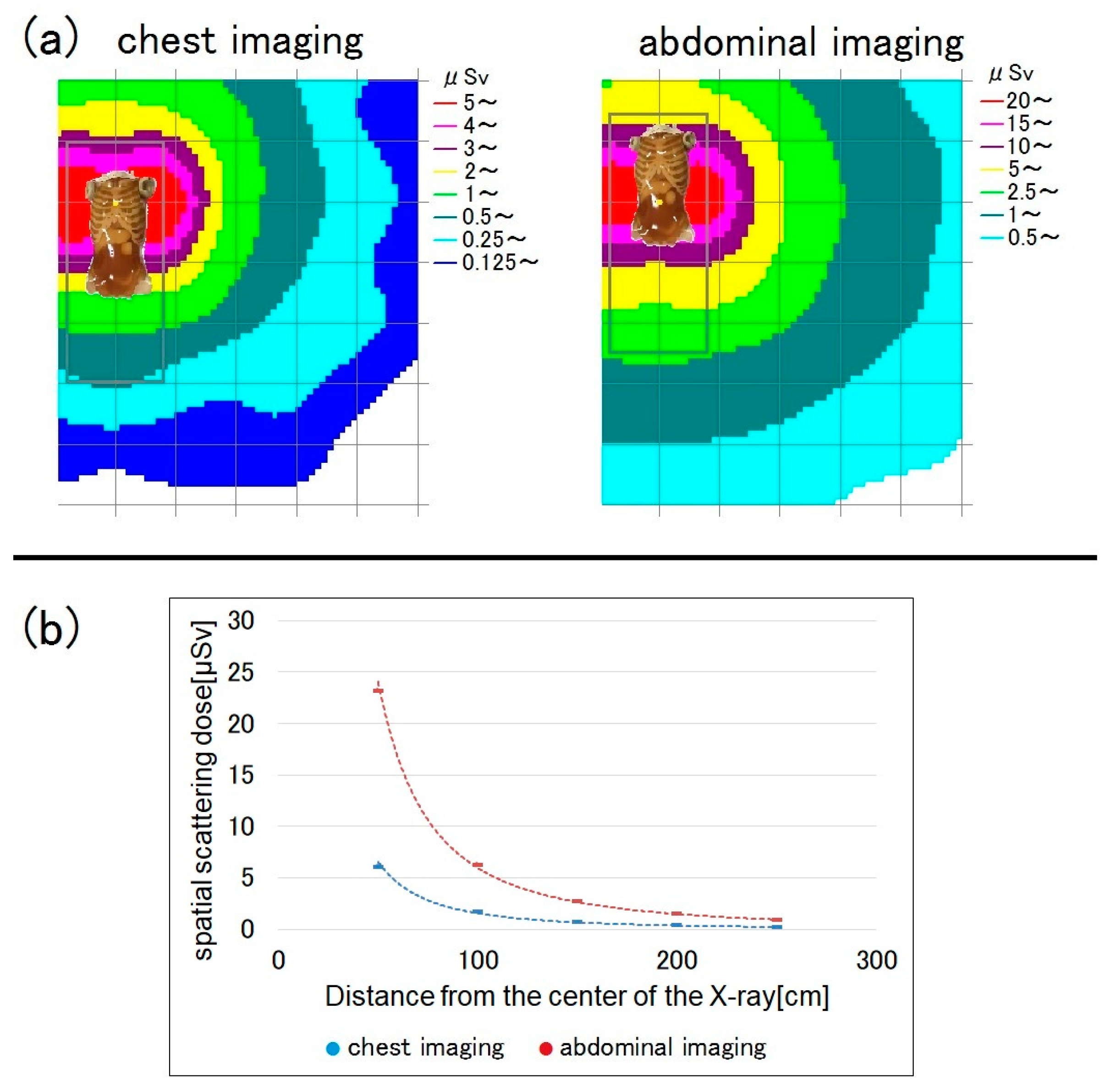
| Comparison of the spatial dose between chest and abdominal imaging (bed height = 80 cm, measurement height = 150 cm) | |||||
| Chest imaging | 6.1 ± 0 | 1.7 ± 0 | 0.7 ± 0 | 0.4 ± 0 | 0.2 ± 0 |
| Abdominal imaging | 23.2 ± 0 | 6.3 ± 0 | 2.7 ± 0 | 1.5 ± 0 | 0.9 ± 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Otomo, K.; Inaba, Y.; Abe, K.; Onodera, M.; Suzuki, T.; Sota, M.; Haga, Y.; Suzuki, M.; Zuguchi, M.; Chida, K. Spatial Scattering Radiation to the Radiological Technologist during Medical Mobile Radiography. Bioengineering 2023, 10, 259. https://doi.org/10.3390/bioengineering10020259
Otomo K, Inaba Y, Abe K, Onodera M, Suzuki T, Sota M, Haga Y, Suzuki M, Zuguchi M, Chida K. Spatial Scattering Radiation to the Radiological Technologist during Medical Mobile Radiography. Bioengineering. 2023; 10(2):259. https://doi.org/10.3390/bioengineering10020259
Chicago/Turabian StyleOtomo, Kazuki, Yohei Inaba, Keisuke Abe, Mana Onodera, Tomohiro Suzuki, Masahiro Sota, Yoshihiro Haga, Masatoshi Suzuki, Masayuki Zuguchi, and Koichi Chida. 2023. "Spatial Scattering Radiation to the Radiological Technologist during Medical Mobile Radiography" Bioengineering 10, no. 2: 259. https://doi.org/10.3390/bioengineering10020259
APA StyleOtomo, K., Inaba, Y., Abe, K., Onodera, M., Suzuki, T., Sota, M., Haga, Y., Suzuki, M., Zuguchi, M., & Chida, K. (2023). Spatial Scattering Radiation to the Radiological Technologist during Medical Mobile Radiography. Bioengineering, 10(2), 259. https://doi.org/10.3390/bioengineering10020259






