Comparison of Bone Bruise Pattern Epidemiology between Anterior Cruciate Ligament Rupture and Patellar Dislocation Patients—Implications of Injury Mechanism
Abstract
:1. Introduction
2. Materials and Methods
2.1. Selection Criteria and MR Imaging
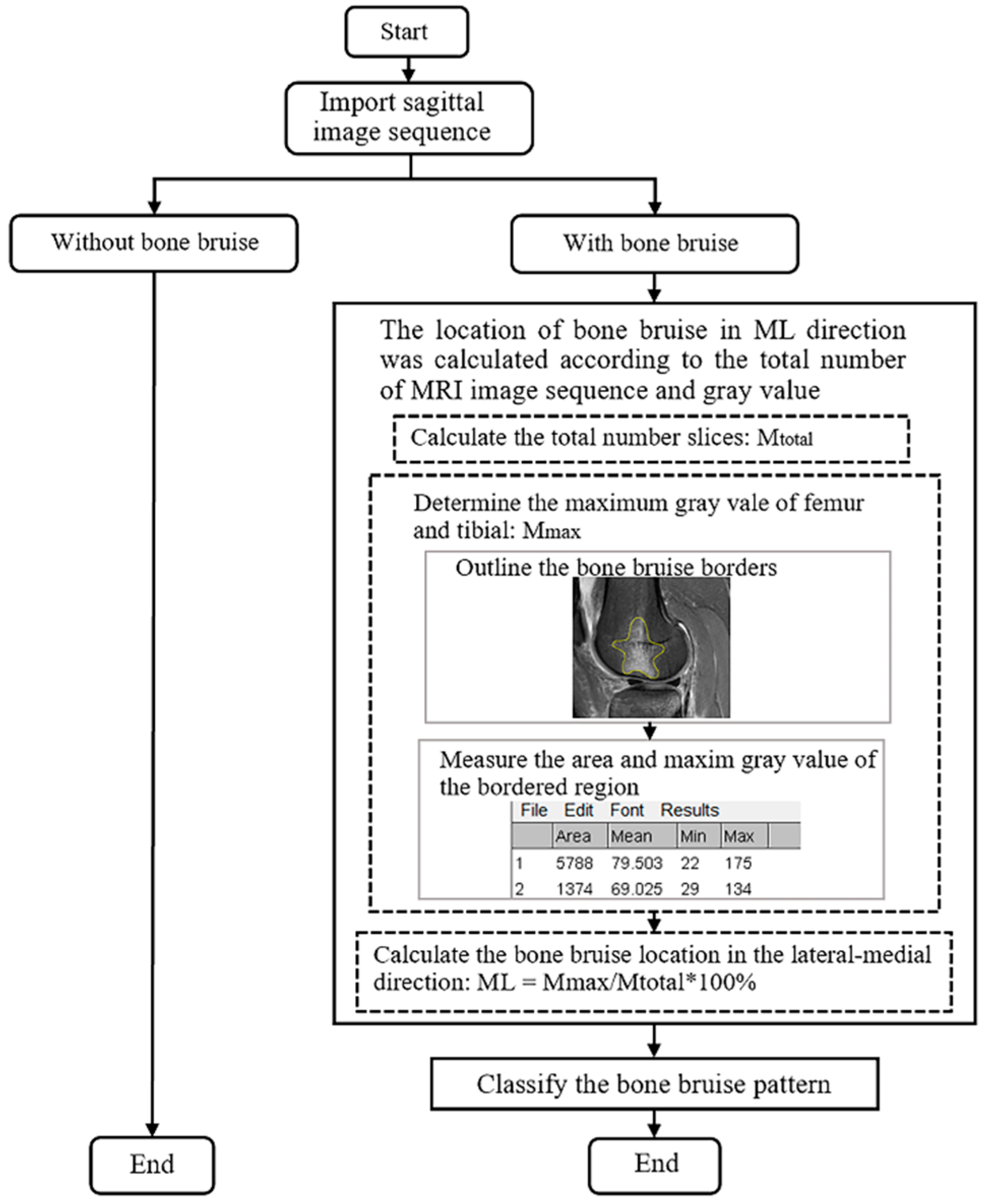
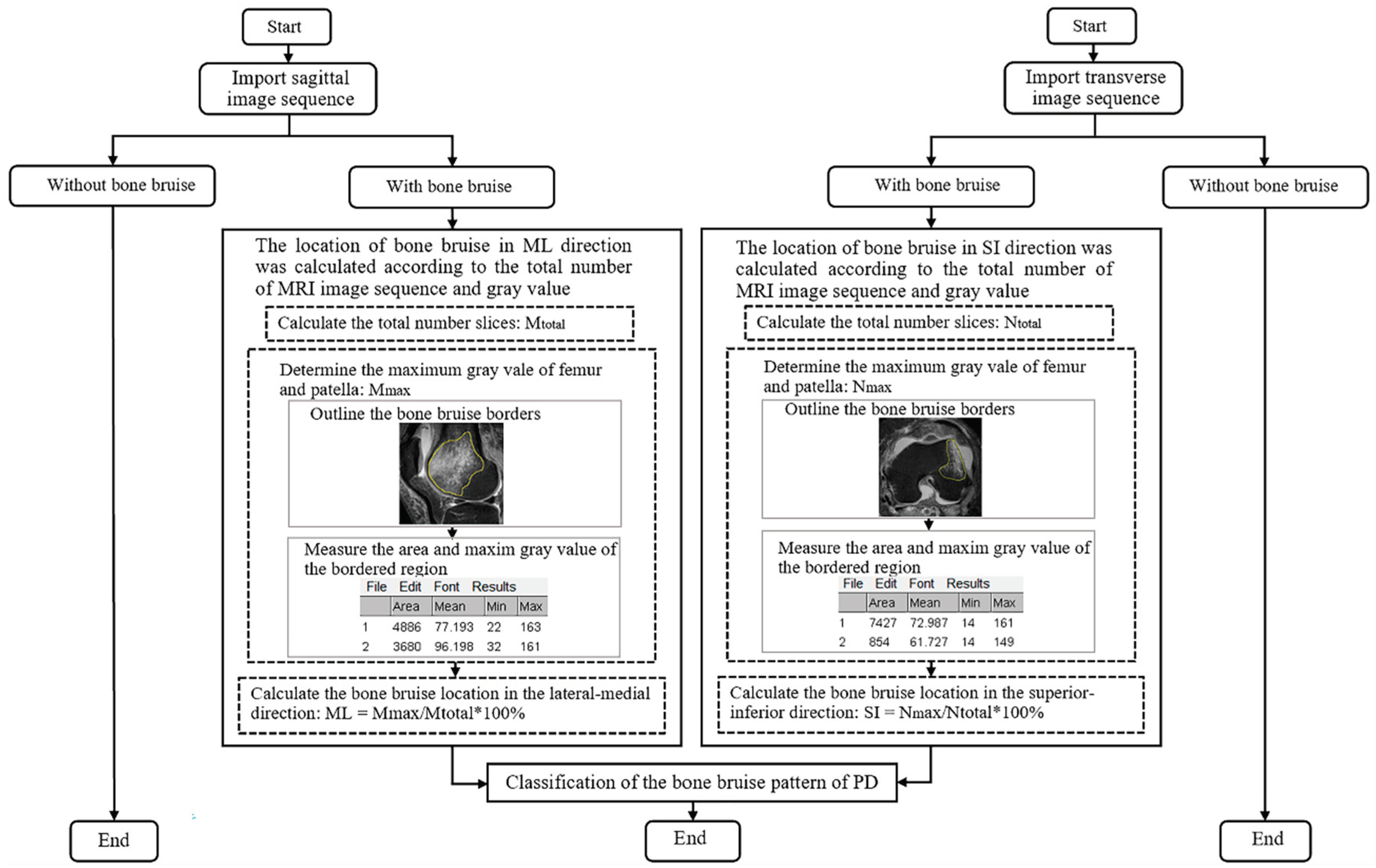
2.2. Determination of Bone Bruise Location
2.3. Statistical Analysis
3. Results
3.1. Descriptive Statistics
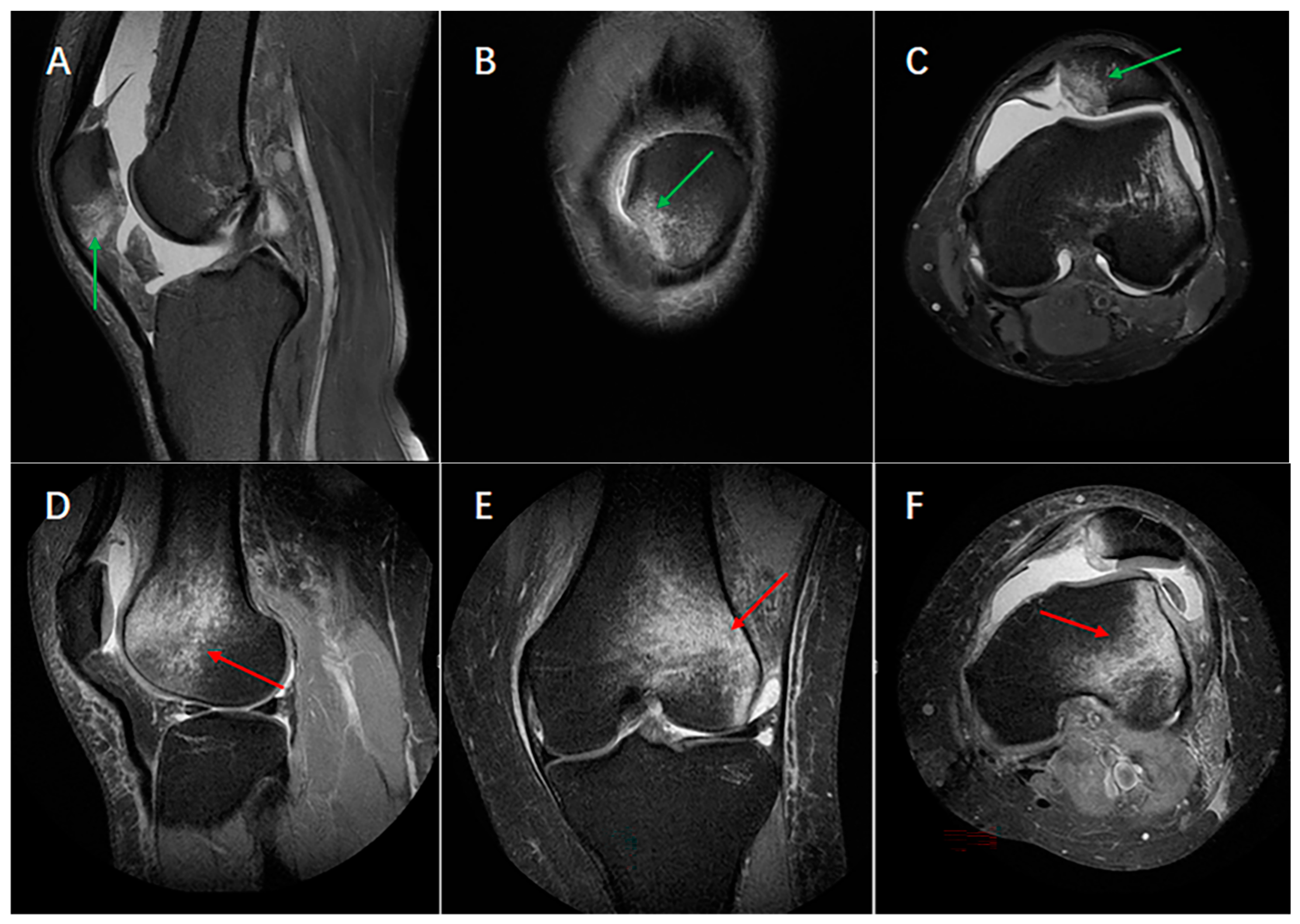
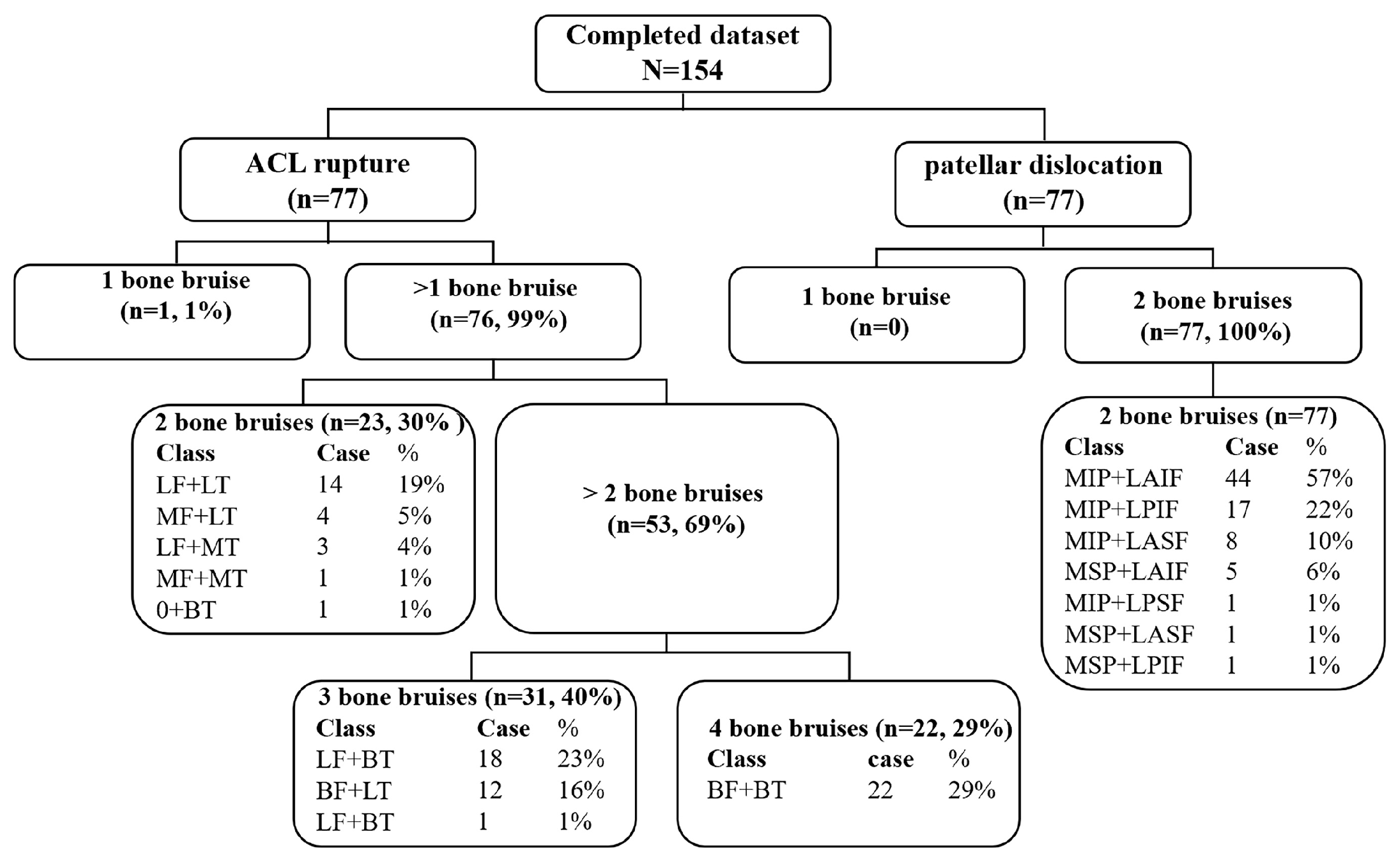
3.2. Bone Bruises Patterns of ACL Rupture and Patellar Dislocation
4. Discussion
Limitation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| MRI | Magnetic resonance imaging |
| ACL | Anterior cruciate ligament |
| BMI | Body mass index |
| SD | Mean ± standard deviation |
| LF + BT | The lateral femoral condyle and both medial and lateral tibial plateau |
| BF + LT | Both the lateral-medial femoral condyle and lateral tibial plateau |
| MF + BT | The medial femoral condyle and both lateral and medial tibial plateau |
| BF + BT | Both the lateral-medial femoral condyle and tibial plateau |
| LF + LT | The lateral femoral condyle and tibial plateau |
| MF + LT | The medial femoral condyle and lateral tibial plateau |
| LF + MT | The lateral femoral condyle and medial tibial plateau |
| MF + MT | The medial femoral condyle and tibial plateau |
| 0 + BT | Only both the medial and lateral tibial plateau |
| 0 + LT | Only the Lateral tibial plateau |
| MIP + LAIF | Medial inferior side of the patellar and the lateral anterior inferior femoral condyle |
| MIP + LPIF | Medial inferior side of the patellar and the lateral posterior inferior femoral condyle |
| MIP + LASF | Medial inferior side of the patellar and the lateral anterior superior femoral condyle |
| MSP + LAIF | Medial superior side of the patellar and the lateral anterior inferior femoral condyle |
| MIP + LPSF | Medial inferior side of the patellar and the lateral posterior superior femoral condyle |
| MSP + LASF | Medial superior side of the patellar and the lateral anterior superior femoral condyle |
| MSP + LPIF | Medial superior side of the patellar and the lateral posterior inferior femoral condyle |
References
- Qiu, L.; Sheng, B.; Li, J.; Xiao, Z.; Yuan, M.; Yang, H.; Lv, F.; Lv, F. Mechanisms of non-contact anterior cruciate ligament injury as determined by bone contusion location and severity. Quant. Imaging Med. Surg. 2021, 11, 3263–3273. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.K.; Parikh, S. Patellofemoral Instability in Children: Imaging Findings and Therapeutic Approaches. Korean J. Radiol. 2022, 23, 674–687. [Google Scholar] [CrossRef] [PubMed]
- Spang, R.C.; Jahandar, A.; Meyers, K.N.; Nguyen, J.T.; Maher, S.A.; Strickland, S.M. Dysplastic Patellofemoral Joints Lead to a Shift in Contact Forces: A 3D-Printed Cadaveric Model. Am. J. Sports Med. 2021, 49, 3344–3349. [Google Scholar] [CrossRef] [PubMed]
- Koga, H.; Nakamae, A.; Shima, Y.; Bahr, R.; Krosshaug, T. Hip and Ankle Kinematics in Noncontact Anterior Cruciate Ligament Injury Situations: Video Analysis Using Model-Based Image Matching. Am. J. Sports Med. 2018, 46, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Koga, H.; Nakamae, A.; Shima, Y.; Iwasa, J.; Myklebust, G.; Engebretsen, L.; Bahr, R.; Krosshaug, T. Mechanisms for noncontact anterior cruciate ligament injuries: Knee joint kinematics in 10 injury situations from female team handball and basketball. Am. J. Sports Med. 2010, 38, 2218–2225. [Google Scholar] [CrossRef] [PubMed]
- Farahmand, F.; Tahmasbi, M.N.; Amis, A. The contribution of the medial retinaculum and quadriceps muscles to patellar lateral stability—An in-vitro study. Knee 2004, 11, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Spritzer, C.E.; Utturkar, G.M.; Toth, A.P.; Garrett, W.E.; DeFrate, L.E. Knee Kinematics During Noncontact Anterior Cruciate Ligament Injury as Determined From Bone Bruise Location. Am. J. Sports Med. 2015, 43, 2515–2521. [Google Scholar] [CrossRef]
- Marchetti, D.C.; Moatshe, G.; Phelps, B.M.; Dahl, K.D.; Ferrari, M.B.; Chahla, J.; Turnbull, T.L.; LaPrade, R.F. The Proximal Tibiofibular Joint: A Biomechanical Analysis of the Anterior and Posterior Ligamentous Complexes. Am. J. Sports Med. 2017, 45, 1888–1892. [Google Scholar] [CrossRef]
- Kaplan, P.A.; Gehl, R.H.; Dussault, R.G.; Anderson, M.W.; Diduch, D.R. Bone contusions of the posterior lip of the medial tibial plateau (contrecoup injury) and associated internal derangements of the knee at MR imaging. Radiology 1999, 211, 747–753. [Google Scholar] [CrossRef]
- Sanders, T.G.; Medynski, M.A.; Feller, J.F.; Lawhorn, K.W. Bone contusion patterns of the knee at MR imaging: Footprint of the mechanism of injury. RadioGraphics 2000, 20, S135–S151. [Google Scholar] [CrossRef]
- Lance, E.; Deutsch, A.L.; Mink, J.H. Prior lateral patellar dislocation: MR imaging findings. Radiology 1993, 189, 905–907. [Google Scholar] [CrossRef] [PubMed]
- Mink, J.H.; Deutsch, A.L. Occult cartilage and bone injuries of the knee: Detection, classification, and assessment with MR imaging. Radiology 1989, 170, 823–829. [Google Scholar] [CrossRef] [PubMed]
- Shi, H.; Ding, L.; Ren, S.; Jiang, Y.; Zhang, H.; Hu, X.; Huang, H.; Ao, Y. Prediction of Knee Kinematics at the Time of Noncontact Anterior Cruciate Ligament Injuries Based on the Bone Bruises. Ann. Biomed. Eng. 2021, 49, 162–170. [Google Scholar] [CrossRef] [PubMed]
- Moran, J.; Lee, M.S.; Kunze, K.N.; Green, J.S.; Katz, L.D.; Wang, A.; McLaughlin, W.M.; Gillinov, S.M.; Jimenez, A.E.; Hewett, T.E.; et al. Examining the Distribution of Bone Bruise Patterns in Contact and Noncontact Acute Anterior Cruciate Ligament Injuries. Am. J. Sports Med. 2023, 51, 1155–1161. [Google Scholar] [CrossRef] [PubMed]
- Tompkins, M.A.; Rohr, S.R.; Agel, J.; Arendt, E.A. Anatomic patellar instability risk factors in primary lateral patellar dislocations do not predict injury patterns: An MRI-based study. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 677–684. [Google Scholar] [CrossRef]
- Shi, H.; Ding, L.; Ren, S.; Jiang, Y.; Zhang, H.; Hu, X.; Huang, H.; Ao, Y. Response to the Letter to the Editor on “Prediction of Knee Kinematics at Time of Noncontact Anterior Cruciate Ligament Injuries Based on Bone Bruises”. Ann. Biomed. Eng. 2021, 49, 4–6. [Google Scholar] [CrossRef]
- Sanchez-Trigo, H.; Rittweger, J.; Sañudo, B. Effects of non-supervised exercise interventions on bone mineral density in adult women: A systematic review and meta-analysis. Osteoporos. Int. 2022, 33, 1415–1427. [Google Scholar] [CrossRef]
- Lin, X.; Guo, H.; Lian, Y.; Kou, J.; Wang, G.; Chen, Y.; Wang, J.; Han, X.; Jiang, M.; Yang, Q. Osteoporosis and Related Health Status Among the Elderly Urban Residents in Elderly-Care Inns in Beijing, a Multicenter DXA Survey. Front. Endocrinol. 2022, 13, 875678. [Google Scholar] [CrossRef]
- Shi, H.; Ding, L.; Jiang, Y.; Zhang, H.; Ren, S.; Hu, X.; Liu, Z.; Huang, H.; Ao, Y. Bone Bruise Distribution Patterns After Acute Anterior Cruciate Ligament Ruptures: Implications for the Injury Mechanism. Orthop. J. Sports Med. 2020, 8, 2325967120911162. [Google Scholar] [CrossRef]
- Kim-Wang, S.Y.; Spritzer, C.E.; Owusu-Akyaw, K.; Coppock, J.A.; Goode, A.P.; Englander, Z.A.; Wittstein, J.R.; DeFrate, L.E. The Predicted Position of the Knee Near the Time of ACL Rupture Is Similar Between 2 Commonly Observed Patterns of Bone Bruising on MRI. Am. J. Sports Med. 2023, 51, 58–65. [Google Scholar] [CrossRef]
- Green, D.W.; Perea, S.H.; Kelly, A.M.; Potter, H.G. Bone Marrow Edema Injury Patterns in the Pediatric Knee: An MRI Study. HSS J. Musculoskelet. J. Hosp. Spec. Surg. 2023, 19, 107–112. [Google Scholar] [CrossRef] [PubMed]
- D’Hooghe, P.; Grassi, A.; Villa, F.D.; Alkhelaifi, K.; Papakostas, E.; Rekik, R.; Marin, T.; Tosarelli, F.; Zaffagnini, S. The injury mechanism correlation between MRI and video-analysis in professional football players with an acute ACL knee injury reveals consistent bone bruise patterns. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 121–132. [Google Scholar] [CrossRef] [PubMed]
- Berger, N.; Andreisek, G.; Karer, A.T.; Bouaicha, S.; Naraghi, A.; Manoliu, A.; Seifert, B.; Ulbrich, E.J. Association between traumatic bone marrow abnormalities of the knee, the trauma mechanism and associated soft-tissue knee injuries. Eur. Radiol. 2017, 27, 393–403. [Google Scholar] [CrossRef] [PubMed]
- Paakkala, A.; Sillanpää, P.; Huhtala, H.; Paakkala, T.; Mäenpää, H. Bone bruise in acute traumatic patellar dislocation: Volumetric magnetic resonance imaging analysis with follow-up mean of 12 months. Skelet. Radiol. 2010, 39, 675–682. [Google Scholar] [CrossRef]
- Cao, H.; An, Q.; Gou, B.; Ma, S.; Goh, E.L.; Xiong, L.; Li, Y.G.; Ao, F. A new classification of injury patterns of the medial patellofemoral ligament after acute lateral patella dislocation detected using magnetic resonance imaging studies. Injury 2019, 50, 534–540. [Google Scholar] [CrossRef]
- Quatman, C.E.; Kiapour, A.; Myer, G.D.; Ford, K.R.; Demetropoulos, C.K.; Goel, V.K.; Hewett, T.E. Cartilage pressure distributions provide a footprint to define female anterior cruciate ligament injury mechanisms. Am. J. Sports Med. 2011, 39, 1706–1713. [Google Scholar] [CrossRef]
- Hewett, T.E.; Myer, G.D.; Ford, K.R.; Heidt, R.S., Jr.; Colosimo, A.J.; McLean, S.G.; van den Bogert, A.J.; Paterno, M.V.; Succop, P. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study. Am. J. Sports Med. 2005, 33, 492–501. [Google Scholar] [CrossRef]
- Owusu-Akyaw, K.A.; Kim, S.Y.; Spritzer, C.E.; Collins, A.T.; Englander, Z.A.; Utturkar, G.M.; Garrett, W.E.; DeFrate, L.E. Determination of the Position of the Knee at the Time of an Anterior Cruciate Ligament Rupture for Male Versus Female Patients by an Analysis of Bone Bruises. Am. J. Sports Med. 2018, 46, 1559–1565. [Google Scholar] [CrossRef]
- Richmond, C.G.; Shea, K.G.; Burlile, J.F.; Heyer, A.M.; Ellis, H.B.; Wilson, P.L.; Arendt, E.A.; Tompkins, M.A. Patellar-Trochlear Morphology in Pediatric Patients from 2 to 11 Years of Age: A Descriptive Analysis Based on Computed Tomography Scanning. J. Pediatr. Orthop. 2020, 40, e96–e102. [Google Scholar] [CrossRef]
- Diederichs, G.; Köhlitz, T.; Kornaropoulos, E.; Heller, M.O.; Vollnberg, B.; Scheffler, S. Magnetic resonance imaging analysis of rotational alignment in patients with patellar dislocations. Am. J. Sports Med. 2013, 41, 51–57. [Google Scholar] [CrossRef]
- Patel, S.A.; Hageman, J.; Quatman, C.E.; Wordeman, S.C.; Hewett, T.E. Prevalence and location of bone bruises associated with anterior cruciate ligament injury and implications for mechanism of injury: A systematic review. Sports Med. 2014, 44, 281–293. [Google Scholar] [CrossRef] [PubMed]
- Deangelis, J.P.; Spindler, K.P. Traumatic Bone Bruises in the Athlete’s Knee. Sports Health 2010, 2, 398–402. [Google Scholar] [CrossRef] [PubMed]
- Agostinone, P.; Di Paolo, S.; Lucidi, G.A.; Fabbro, G.D.; Grassi, A.; Zaffagnini, S. Severe bicompartmental bone bruise is associated with rotatory instability in anterior cruciate ligament injury. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 1725–1732. [Google Scholar] [CrossRef] [PubMed]
- Sutton, K.M.; Bullock, J.M. Anterior cruciate ligament rupture: Differences between males and females. J. Am. Acad. Orthop. Surg. 2013, 21, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Boden, B.P.; Sheehan, F.T.; Torg, J.S.; Hewett, T.E. Noncontact anterior cruciate ligament injuries: Mechanisms and risk factors. J. Am. Acad. Orthop. Surg. 2010, 18, 520–527. [Google Scholar] [CrossRef] [PubMed]
- Fones, L.; Jimenez, A.E.; Cheng, C.; Chevalier, N.; Brimacombe, M.B.; Cohen, A.; Pace, J.L. Trochlear Dysplasia as Shown by Increased Sulcus Angle Is Associated With Osteochondral Damage in Patients With Patellar Instability. Arthroscopy 2021, 37, 3469–3476. [Google Scholar] [CrossRef]
- Imhoff, F.B.; Funke, V.; Muench, L.N.; Sauter, A.; Englmaier, M.; Woertler, K.; Imhoff, A.B.; Feucht, M.J. The complexity of bony malalignment in patellofemoral disorders: Femoral and tibial torsion, trochlear dysplasia, TT-TG distance, and frontal mechanical axis correlate with each other. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 897–904. [Google Scholar] [CrossRef]
- Parikh, S.N.; Lykissas, M.G.; Gkiatas, I. Predicting Risk of Recurrent Patellar Dislocation. Curr. Rev. Musculoskelet. Med. 2018, 11, 253–260. [Google Scholar] [CrossRef]
- Lyons, J.G.; Hudson, T.L.; Krishnamurthy, A.B. Epidemiology of patellar dislocations in the United States from 2001 to 2020: Results of a national emergency department database. Phys. Sport. 2022, 15, 1–10. [Google Scholar] [CrossRef]
- Pruneski, J.; O’Mara, L.; Perrone, G.S.; Kiapour, A.M. Changes in Anatomic Risk Factors for Patellar Instability During Skeletal Growth and Maturation. Am. J. Sports Med. 2022, 50, 2424–2432. [Google Scholar] [CrossRef]
- Kanakamedala, A.C.; Burnham, J.M.; Pfeiffer, T.R.; Herbst, E.; Kowalczuk, M.; Popchak, A.; Irrgang, J.; Fu, F.H.; Musahl, V. Lateral femoral notch depth is not associated with increased rotatory instability in ACL-injured knees: A quantitative pivot shift analysis. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 1399–1405. [Google Scholar] [CrossRef] [PubMed]
- Dimitriou, D.; Reimond, M.; Foesel, A.; Baumgaertner, B.; Zou, D.; Tsai, T.Y.; Helmy, N. The deep lateral femoral notch sign: A reliable diagnostic tool in identifying a concomitant anterior cruciate and anterolateral ligament injury. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 1968–1976. [Google Scholar] [CrossRef] [PubMed]
- Berthold, D.P.; Muench, L.N.; Herbst, E.; Mayr, F.; Chadayammuri, V.; Imhoff, A.B.; Feucht, M.J. High prevalence of a deep lateral femoral notch sign in patients with anterior cruciate ligament (ACL) and concomitant posterior root tears of the lateral meniscus. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 1018–1024. [Google Scholar] [CrossRef] [PubMed]


| ACL Rupture | Patellar Dislocation | p Value | |
|---|---|---|---|
| Age | 29.06 ± 6.09 | 24.83 ± 6.02 | <0.001 |
| BMI a | 23.98 ± 3.29 | 23.50 ± 3.67 | 0.404 |
| Time from injury (d) | 19.22 ± 6.40 | 14.45 ± 8.66 | <0.001 |
| Sex, man/woman, n | 63/14 | 32/45 | 0.001 |
| Injury side, left/right, n | 43/34 | 49/28 | 0.326 |
| Causing sports/daily activities, n | 77/0 | 42/35 | <0.001 |
| Bone Bruise Pattern | N (%) | |
|---|---|---|
| 3- bone bruises | ||
| LF + BT | 18 (23%) | |
| BF + LT | 12 (16%) | |
| MF + BT | 1 (1%) | |
| 4- bone bruises | ||
| BF + BT | 22 (29%) | |
| 2- bone bruises | ||
| LF + LT | 14 (19%) | |
| MF + LT | 4 (5%) | |
| LF + MT | 3 (4%) | |
| MF + MT | 1 (1%) | |
| 0 + BT | 1 (1%) | |
| 1- bone bruise | ||
| 0 + LT | 1 (1%) | |
| Total | 77 (100%) |
| Bone Bruise Pattern | N (%) |
|---|---|
| MIP + LAIF | 44 (57%) |
| MIP + LPIF | 17 (22%) |
| MIP + LASF | 8 (10%) |
| MSP + LAIF | 5 (6%) |
| MIP + LPSF | 1 (1%) |
| MSP + LASF | 1 (1%) |
| MSP + LPIF | 1 (1%) |
| Total | 77 (100%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dai, R.; Wu, Y.; Jiang, Y.; Huang, H.; Yan, W.; Shi, H.; Meng, Q.; Ren, S.; Ao, Y. Comparison of Bone Bruise Pattern Epidemiology between Anterior Cruciate Ligament Rupture and Patellar Dislocation Patients—Implications of Injury Mechanism. Bioengineering 2023, 10, 1366. https://doi.org/10.3390/bioengineering10121366
Dai R, Wu Y, Jiang Y, Huang H, Yan W, Shi H, Meng Q, Ren S, Ao Y. Comparison of Bone Bruise Pattern Epidemiology between Anterior Cruciate Ligament Rupture and Patellar Dislocation Patients—Implications of Injury Mechanism. Bioengineering. 2023; 10(12):1366. https://doi.org/10.3390/bioengineering10121366
Chicago/Turabian StyleDai, Ruilan, Yue Wu, Yanfang Jiang, Hongshi Huang, Wenqiang Yan, Huijuan Shi, Qingyang Meng, Shuang Ren, and Yingfang Ao. 2023. "Comparison of Bone Bruise Pattern Epidemiology between Anterior Cruciate Ligament Rupture and Patellar Dislocation Patients—Implications of Injury Mechanism" Bioengineering 10, no. 12: 1366. https://doi.org/10.3390/bioengineering10121366
APA StyleDai, R., Wu, Y., Jiang, Y., Huang, H., Yan, W., Shi, H., Meng, Q., Ren, S., & Ao, Y. (2023). Comparison of Bone Bruise Pattern Epidemiology between Anterior Cruciate Ligament Rupture and Patellar Dislocation Patients—Implications of Injury Mechanism. Bioengineering, 10(12), 1366. https://doi.org/10.3390/bioengineering10121366







