Diagnostic Validation of the Screening Corneal Objective Risk of Ectasia Analyzer Evaluated by Swept Source Optical Coherence Tomography for Keratoconus in an Asian Population
Abstract
:1. Introduction
2. Materials and Methods
- “Ant. Kmax”: The maximum K value of the anterior corneal surface.
- “Ant. Kmax—opposite K (AntK_oppoK)”: The difference between the maximum K value of the anterior corneal surface and the K value measured opposite the Kmax position.
- “Ant. inf.—sup. K mean (Ant_inf_supK)”: The difference between the inferior mean anterior corneal axial curvature and the superior mean anterior corneal axial curvature.
- “Ant. irregularity (Ant_irre_3 mm)”: The irregularity of the axial curvature of the anterior corneal surface at the central 3 mm ring.
- “Posterior elevation of thinnest point (post_ele_thin)”: The elevation of the posterior corneal surface at the location of the thinnest point with the best fit sphere as a reference surface.
- “Thinnest point (A_Cor_thin)”: The thinnest position of the cornea.
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Martínez-Abad, A.; Pinero, D.P. New perspectives on the detection and progression of keratoconus. J. Cataract Refract. Surg. 2017, 43, 1213–1227. [Google Scholar]
- Rabinowitz, Y.S. Videokeratographic indices to aid in screening for keratoconus. J. Refract. Surg. 1995, 11, 371–406. [Google Scholar] [CrossRef] [PubMed]
- Rabinowitz, Y.S.; McDonnell, P.J. Computer-assisted corneal topography in keratoconus. Refract. Corneal. Surg. 1989, 5, 400–408. [Google Scholar] [CrossRef] [PubMed]
- Pflugfelder, S.C.; Liu, Z.; Feuer, W.; Verm, A. Corneal thickness indices discriminate between keratoconus and contact lens-induced corneal thinning. Ophthalmology 2002, 109, 2336–2341. [Google Scholar] [CrossRef]
- Sedghipour, M.R.; Sadigh, A.L.; Motlagh, B.F. Revisiting corneal topography for the diagnosis of keratoconus: Use of Rabinowitz’s KISA% index. Clin. Ophthalmol. 2012, 6, 181–184. [Google Scholar]
- Zhang, X.; Munir, S.Z.; Sami Karim, S.A.; Munir, W.M. A review of imaging modalities for detecting early keratoconus. Eye 2021, 35, 173–187. [Google Scholar] [PubMed]
- Maeda, N.; Klyce, S.D.; Smolek, M.K.; Thompson, H.W. Automated keratoconus screening with corneal topography analysis. Investig. Ophthalmol. Vis. Sci. 1994, 35, 2749–2757. [Google Scholar]
- Belin, M.W.; Villavicencio, O.F.; Ambrósio, R.R., Jr. Tomographic parameters for the detection of keratoconus: Suggestions for screening and treatment parameters. Eye Contact Lens 2014, 40, 326–330. [Google Scholar] [CrossRef]
- Cavas-Martínez, F.; De la Cruz Sánchez, E.; Nieto Martínez, J.; Fernández Cañavate, F.; Fernández-Pacheco, D. Corneal topography in keratoconus: State of the art. Eye Vis. 2016, 3, 5. [Google Scholar]
- Saad, A.; Gatinel, D. Topographic and tomographic properties of forme fruste keratoconus corneas. Investig. Ophthalmol. Vis. Sci. 2010, 51, 5546–5555. [Google Scholar] [CrossRef]
- Georgiou, T.; Funnell, C.; Cassels-Brown, A.; O’conor, R. Influence of ethnic origin on the incidence of keratoconus and associated atopic disease in Asians and white patients. Eye 2004, 18, 379–383. [Google Scholar] [CrossRef] [PubMed]
- Pearson, A.; Soneji, B.; Sarvananthan, N.; Sandford-Smith, J. Does ethnic origin influence the incidence or severity of keratoconus? Eye 2000, 14, 625–628. [Google Scholar] [CrossRef] [PubMed]
- Haseltine, S.J.; Pae, J.; Ehrlich, J.R.; Shammas, M.; Radcliffe, N.M. Variation in corneal hysteresis and central corneal thickness among black, hispanic and white subjects. Acta Ophthalmol. 2012, 90, e626–e631. [Google Scholar] [CrossRef]
- Kok, Y.O.; Tan, G.F.L.; Loon, S.C. keratoconus in Asia. Cornea 2012, 31, 581–593. [Google Scholar] [CrossRef] [PubMed]
- Hickson-Curran, S.; Brennan, N.A.; Igarashi, Y.; Young, G. Comparative evaluation of Asian and white ocular topography. Optom. Vis. Sci. 2014, 91, 1396–1405. [Google Scholar] [CrossRef] [PubMed]
- Ucakhan, O.O.; Cetinkor, V.; Ozkan, M.; Kanpolat, A. Evaluation of Scheimpflug imaging parameters in subclinical keratoconus, keratoconus, and normal eyes. J. Cataract Refract. Surg. 2011, 37, 1116–1124. [Google Scholar] [CrossRef]
- Chan, C.; Ang, M.; Saad, A.; Chua, D.; Mejia, M.; Lim, L.; Gatinel, D. Validation of an Objective Scoring System for Forme Fruste Keratoconus Detection and Post-LASIK Ectasia Risk Assessment in Asian Eyes. Cornea 2015, 34, 996–1004. [Google Scholar] [CrossRef]
- Saad, A.; Debellemaniere, G.; Zeboulon, P.; Rizk, M.; Rouger, H.; Mazharian, A.; Grise-Dulac, A.; Panthier, C.; Gatinel, D. Discrimination between Keratoconus, Forme Fruste Keratoconus and Normal Eyes using a Novel OCT-based Tomographer. J. Cataract Refract. Surg. 2023, 49, 1092–1097. [Google Scholar] [CrossRef]
- Yun, J.S.; Min, J.S.; Kim, K.Y. Evaluation of angle-to-angle and spur-to-spur using swept source optical coherence tomography in different refractive error. PLoS ONE 2022, 17, e0277703. [Google Scholar]
- Feng, Y.; Reinstein, D.Z.; Nitter, T.; Archer, T.J.; McAlinden, C.; Bertelsen, G.; Stojanovic, A. Epithelial Thickness Mapping in Keratoconic Corneas: Repeatability and Agreement Between CSO MS-39, Heidelberg Anterion, and Optovue Avanti OCT Devices. J. Refract. Surg. 2023, 39, 474–480. [Google Scholar] [CrossRef]
- Song, M.Y.; Noh, S.R.; Kim, K.Y. Refractive prediction of four different intraocular lens calculation formulas compared between new swept source optical coherence tomography and partial coherence interferometry. PLoS ONE 2021, 16, e0251152. [Google Scholar] [CrossRef] [PubMed]
- Meduri, E.; Gillmann, K.; Bravetti, G.E.; Niegowski, L.J.; Mermoud, A.; Weinreb, R.N.; Mansouri, K. Iridocorneal angle assessment after laser iridotomy with swept-source optical coherence tomography. J. Glaucoma 2020, 29, 1030–1035. [Google Scholar] [CrossRef]
- Kanclerz, P.; Khoramnia, R.; Wang, X. Current developments in corneal topography and tomography. Diagnostics 2021, 11, 1466. [Google Scholar] [CrossRef] [PubMed]
- Godefrooij, D.A.; Gans, R.; Imhof, S.M.; Wisse, R.P. Nationwide reduction in the number of corneal transplantations for keratoconus following the implementation of cross-linking. Acta Ophthalmol. 2016, 94, 675–678. [Google Scholar] [CrossRef] [PubMed]
- Gomes, J.A.P.; Tan, D.; Rapuano, C.J.; Belin, M.W.; Ambrósio, R.J.; Guell, J.L.; Malecaze, F.; Nishida, K.; Sangwan, V.S.; Group of Panelists for the Global Delphi Panel of Keratoconus and Ectatic Diseases. Global Consensus on Keratoconus and Ectatic Diseases. Cornea 2015, 34, 359–369. [Google Scholar] [CrossRef]
- Escolano Serrano, J.; Tarazona Jaimes, C.P.; Monera Lucas, C.E.; Romero Valero, D.; Moya Martínez, A.; Martínez Toldos, J.J. Intraobserver repeatability of tomographic, pachymetric, and anatomical measurements in healthy eyes using a new swept-source optical coherence topographer. Cornea 2022, 41, 598–603. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Reinstein, D.Z.; Nitter, T.; Archer, T.J.; McAlinden, C.; Chen, X.; Bertelsen, G.; Utheim, T.P.; Stojanovic, A. Heidelberg anterion swept-source OCT corneal epithelial thickness mapping: Repeatability and agreement with optovue avanti. J. Refract. Surg. 2022, 38, 356–363. [Google Scholar] [CrossRef]
- Qin, B.; Tang, M.; Li, Y.; Zhang, X.; Chu, R.; Huang, D. Anterior segment dimensions in Asian and Caucasian eyes measured by optical coherence tomography. Ophthalmic Surg. Lasers Imaging Retin. 2012, 43, 135–142. [Google Scholar] [CrossRef]
- Saad, A.; Gatinel, D. Validation of a new scoring system for the detection of early forme of keratoconus. Age 2012, 37, 37–38. [Google Scholar] [CrossRef]
- Swets, J.A. Measuring the accuracy of diagnostic systems. Science 1988, 240, 1285–1293. [Google Scholar] [CrossRef]
- Kamiya, K.; Ishii, R.; Shimizu, K.; Igarashi, A. Evaluation of corneal elevation, pachymetry and keratometry in keratoconic eyes with respect to the stage of Amsler-Krumeich classification. Br. J. Ophthalmol. 2014, 98, 459–463. [Google Scholar] [CrossRef] [PubMed]
- Kovács, I.; Takács, Á.; Nagy, Z.Z. Evaluation of keratometric, pachymetric, and elevation parameters of keratoconic corneas with pentacam. Cornea 2009, 28, 976–980. [Google Scholar]
- Kim, K.Y.; Lee, S.; Jeon, Y.J.; Min, J.S. Anterior segment characteristics in normal and keratoconus eyes evaluated with a new type of swept-source optical coherence tomography. PLoS ONE 2022, 17, e0274071. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.; Lim, D.H.; Chung, T.-Y. Prevalence and incidence of keratoconus in South Korea: A nationwide population-based study. Am. J. Ophthalmol. 2018, 192, 56–64. [Google Scholar] [CrossRef] [PubMed]
| Variables | Normal (n = 46) | KC Suspect (n = 45) | KC (n = 60) | p Value |
|---|---|---|---|---|
| Age (years) | 29.76 ± 10.26 | 27.87 ± 10.43 | 30.28 ± 8.29 | 0.055 * |
| Sex | ||||
| Male:Female (n) | 22:24 | 24:21 | 33:27 | 0.754 † |
| Laterality | ||||
| Right | 21 (45.65%) | 26 (57.78%) | 28 (46.67%) | 0.428 † |
| Left | 25 (54.35%) | 19 (42.22%) | 32 (53.33%) | |
| Refractive errors (D) | ||||
| Spherical | −3.28 ± 2.41 | −3.10 ± 2.71 | −3.08 ± 3.04 | 0.892 * |
| Cylindrical | −0.94 ± 0.85 | −2.07 ± 1.75 | −2.67 ± 1.74 | <0.001 * |
| Average ant. Sim K (D) | 43.29 ± 1.73 | 44.48 ± 1.26 | 47.67± 5.71 | <0.001 |
| Steep (D) | 44.13 ± 1.96 | 45.74 ± 1.68 | 49.55 ± 6.61 | <0.001 |
| Flat (D) | 42.50 ± 1.66 | 43.32 ± 1.23 | 45.99 ± 5.19 | <0.001 |
| Ant. astigmatism (D) | 1.62 ± 1.05 | 2.43 ± 1.49 | 3.56 ± 2.10 | <0.001 |
| Ant. K max (D) | 44.71 ± 2.01 | 46.52 ± 1.68 | 53.95 ± 9.77 | <0.001 |
| Average Post. K (D) | −6.18 ± 0.28 | −6.37 ± 0.23 | −7.12 ± 1.20 | <0.001 |
| Steep (D) | −6.41 ± 0.34 | −6.63 ± 0.30 | −7.51 ± 1.29 | <0.001 |
| Flat (D) | −5.97 ± 0.25 | −6.14 ± 0.22 | −6.78 ± 1.16 | <0.001 |
| Post. astigmatism (D) | −0.44 ± 0.18 | −0.49 ± 0.20 | −0.73 ± 0.42 | <0.001 |
| Post. K max (D) | −6.48 ± 0.35 | −6.76 ± 0.32 | −8.86 ± 2.36 | <0.001 |
| Average total K (D) | 42.74 ± 1.76 | 44.01 ± 1.34 | 47.55 ± 6.39 | <0.001 |
| Steep (D) | 43.49 ± 1.98 | 45.18 ± 1.79 | 49.32 ± 7.19 | <0.001 |
| Flat (D) | 42.00 ± 1.68 | 42.84 ± 1.23 | 45.75 ± 4.14 | <0.001 |
| Total K (D) | 1.49 ± 1.02 | 2.34 ± 1.50 | 3.54 ± 2.46 | <0.001 |
| Central pachymetry (µm) | 539.74 ± 32.07 | 537.04 ± 25.38 | 493.15 ± 50.38 | <0.001 |
| Thinnest pachymetry (µm) | 537.11 ± 31.56 | 533.13 ± 25.23 | 477.03 ± 53.37 | <0.001 |
| Thinnest point X | 0.01 ± 0.40 | −0.07 ± 0.50 | 0.06 ± 0.61 | 0.358 |
| Thinnest point Y | −0.38 ± 0.23 | −0.46 ± 0.31 | −0.72 ± 0.42 | <0.001 |
| WTW | 12.22 ± 0.50 | 11.82 ± 0.54 | 12.08 ± 0.51 | 0.004 |
| SCORE Parameters | Normal (n = 46) | KC Suspect (n = 45) | KC (n = 60) | p Value * | p Value † | p Value ‡ | p Value § |
|---|---|---|---|---|---|---|---|
| Total value | −0.55 ± 1.38 (−3.10, 3.00) | 0.77 ± 2.10 (−1.90, 11.20) | 14.43 ± 13.41 (−0.30, 72.10) | <0.001 | <0.001 | <0.001 | <0.001 |
| Ant. K max | 44.58 ± 1.97 (41.20, 49.10) | 46.48 ± 1.68 (42.75, 50.83) | 53.96 ± 9.41 (44.34, 94.13) | <0.001 | <0.001 | <0.001 | <0.001 |
| AntK_oppoK | 0.87 ± 0.74 (0.00, 2.64) | 1.32 ± 1.01 (0.02, 4.66) | 5.90 ± 4.76 (0.25, 16.89) | <0.001 | 0.035 | <0.001 | <0.001 |
| Ant_inf_supK | 0.26 ± 0.51 (−1.07, 1.36) | 0.59 ± 0.80 (−1.38, 2.59) | 4.37 ± 3.93 (−1.55, 20.69) | <0.001 | 0.006 | <0.001 | <0.001 |
| Ant_irre_3 mm | 0.91 ± 0.38 (0.31, 1.85) | 1.27 ± 0.59 (0.29, 2.74) | 2.80 ± 1.34 (0.60, 6.07) | <0.001 | 0.007 | <0.001 | <0.001 |
| post_ele_thin | 5.61 ± 4.07 (−1.00, 18.00) | 10.33 ± 7.27 (2.00, 50.00) | 52.82 ± 38.85 (9.00, 198.00) | <0.001 | <0.001 | <0.001 | <0.001 |
| A_Cor_thin | 538.13 ± 34.35 (458, 596) | 533.00 ± 25.10 (466, 578) | 477.82 ± 53.17 (318, 568) | <0.001 | 0.319 | <0.001 | <0.001 |
| Parameters | Partial Regression Coefficient (B) | Standardized Partial Regression Coefficient (β) | p-Value | |
|---|---|---|---|---|
| SCORE Value | (R = 0.991, R2 = 0.980, Adjusted R2 = 0.981) | |||
| Ant. K_max | 0.344 | 0.229 | <0.001 | |
| AntK_oppoK | 0.880 | 0.308 | <0.001 | |
| Ant_inf_supK | 1.082 | 0.312 | <0.001 | |
| Ant_irre_3 mm | −0.939 | −0.106 | <0.001 | |
| post_ele_thin | 0.090 | 0.269 | <0.001 | |
| A_Cor_thin | −0.014 | −0.063 | 0.001 | |
| Constant | −9.267 | 0.003 | ||
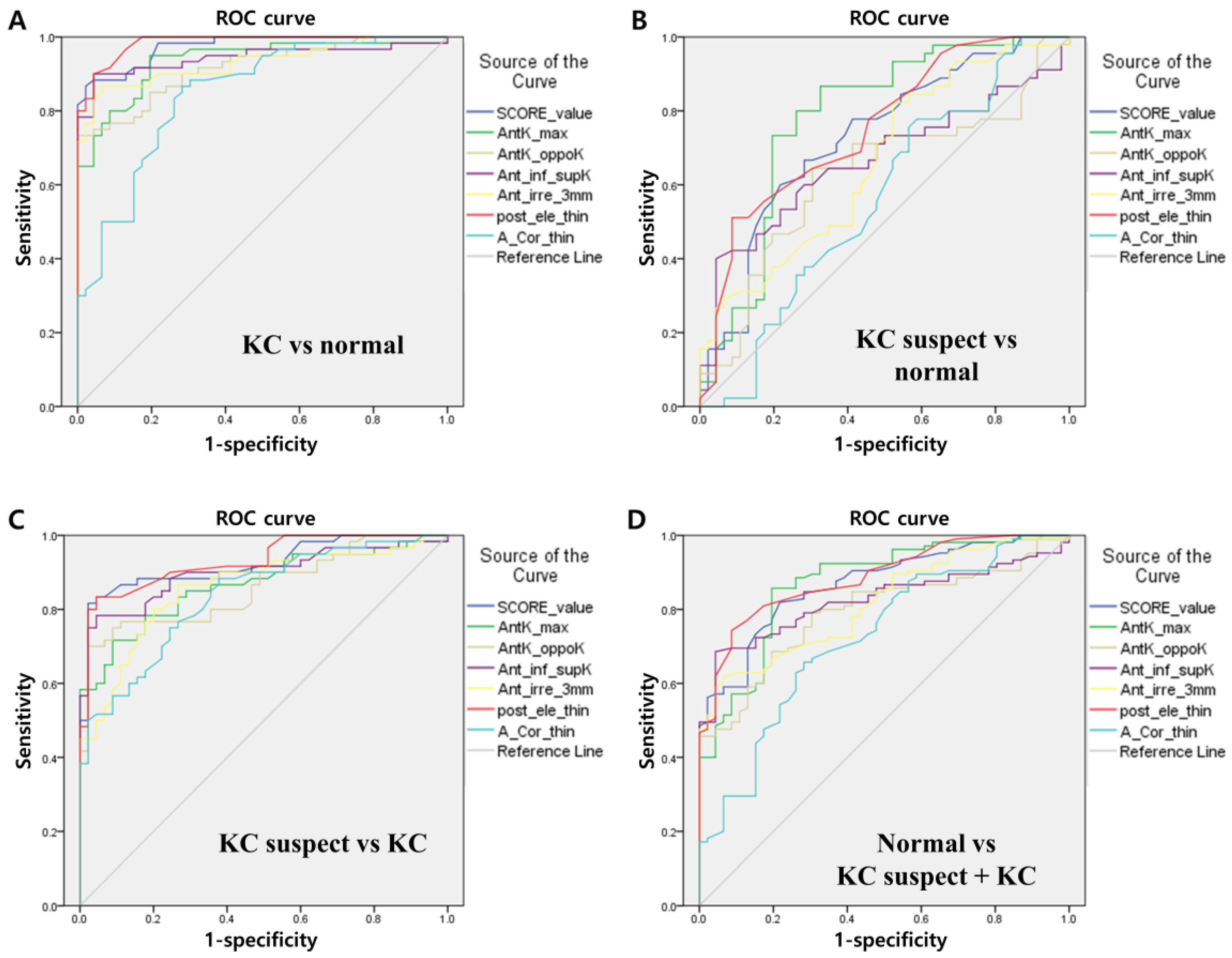
| Parameters | AUROC | SE | p Value | Cut-Off | Sensitivity | Specificity | PLR | NLR | |
|---|---|---|---|---|---|---|---|---|---|
| KC vs. normal | SCORE | 0.974 | 0.012 | 0.000 | 2.40 | 0.868 | 0.978 | 39.97 | 0.14 |
| Ant. K max | 0.934 | 0.024 | 0.000 | 45.80 | 0.950 | 0.804 | 4.86 | 0.06 | |
| AntK_oppoK | 0.917 | 0.026 | 0.000 | 2.67 | 0.733 | 1.000 | - | 0.27 | |
| Ant_inf_supK | 0.944 | 0.024 | 0.000 | 0.98 | 0.900 | 0.957 | 20.70 | 0.10 | |
| Ant_irre_3 mm | 0.932 | 0.024 | 0.000 | 1.41 | 0.867 | 0.935 | 13.29 | 0.14 | |
| post_ele_thin | 0.985 | 0.008 | 0.000 | 12.50 | 0.900 | 0.957 | 20.70 | 0.10 | |
| A_Cor_thin | 0.847 | 0.038 | 0.000 | 529.5 | 0.867 | 0.717 | 30.07 | 0.19 | |
| KC suspect vs. Normal | SCORE | 0.729 | 0.053 | 0.000 | −0.05 | 0.667 | 0.717 | 2.36 | 0.46 |
| Ant. K max | 0.781 | 0.050 | 0.000 | 44.96 | 0.867 | 0.674 | 2.66 | 0.20 | |
| AntK_oppoK | 0.629 | 0.060 | 0.035 | 1.045 | 0.644 | 0.696 | 2.12 | 0.51 | |
| Ant_inf_supK | 0.667 | 0.059 | 0.006 | 0.90 | 0.40 | 0.957 | 9.20 | 0.63 | |
| Ant_irre_3 mm | 0.663 | 0.057 | 0.007 | 0.87 | 0.822 | 0.478 | 1.58 | 0.37 | |
| post_ele_thin | 0.754 | 0.050 | 0.000 | 10.5 | 0.511 | 0.913 | 5.88 | 0.54 | |
| A_Cor_thin | 0.561 | 0.061 | 0.319 | 547.5 | 0.756 | 0.435 | 1.34 | 0.56 | |
| KC suspect vs. KC | SCORE | 0.923 | 0.026 | 0.000 | 4.45 | 0.817 | 0.978 | 36.75 | 0.19 |
| Ant. K max | 0.865 | 0.035 | 0.000 | 48.275 | 0.717 | 0.911 | 8.06 | 0.31 | |
| AntK_oppoK | 0.859 | 0.036 | 0.000 | 3.075 | 0.700 | 0.978 | 31.50 | 0.31 | |
| Ant_inf_supK | 0.899 | 0.031 | 0.000 | 1.52 | 0.783 | 0.956 | 17.63 | 0.23 | |
| Ant_irre_3 mm | 0.858 | 0.036 | 0.000 | 1.655 | 0.800 | 0.800 | 4.00 | 0.25 | |
| post_ele_thin | 0.931 | 0.024 | 0.000 | 16.5 | 0.833 | 0.956 | 18.75 | 0.17 | |
| A_Cor_thin | 0.836 | 0.038 | 0.000 | 516 | 0.750 | 0.756 | 3.07 | 0.33 | |
| KC suspect + KC vs. Normal | SCORE | 0.869 | 0.029 | 0.000 | 0.25 | 0.819 | 0.783 | 3.77 | 0.23 |
| Ant. K max | 0.869 | 0.031 | 0.000 | 45.595 | 0.857 | 0.804 | 4.38 | 0.18 | |
| AntK_oppoK | 0.793 | 0.036 | 0.000 | 1.35 | 0.686 | 0.804 | 3.50 | 0.39 | |
| Ant_inf_supK | 0.825 | 0.033 | 0.000 | 0.90 | 0.686 | 0.957 | 15.77 | 0.33 | |
| Ant_irre_3 mm | 0.817 | 0.034 | 0.000 | 1.38 | 0.619 | 0.935 | 9.49 | 0.41 | |
| post_ele_thin | 0.886 | 0.026 | 0.000 | 10.5 | 0.743 | 0.913 | 8,54 | 0.28 | |
| A_Cor_thin | 0.724 | 0.045 | 0.000 | 529.5 | 0.657 | 0.717 | 2.33 | 0.48 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, K.; Koh, K.; Lee, S.; Lee, Y. Diagnostic Validation of the Screening Corneal Objective Risk of Ectasia Analyzer Evaluated by Swept Source Optical Coherence Tomography for Keratoconus in an Asian Population. Bioengineering 2023, 10, 1335. https://doi.org/10.3390/bioengineering10111335
Kim K, Koh K, Lee S, Lee Y. Diagnostic Validation of the Screening Corneal Objective Risk of Ectasia Analyzer Evaluated by Swept Source Optical Coherence Tomography for Keratoconus in an Asian Population. Bioengineering. 2023; 10(11):1335. https://doi.org/10.3390/bioengineering10111335
Chicago/Turabian StyleKim, Kookyoung, Kyungmin Koh, Seongjun Lee, and Yongwoo Lee. 2023. "Diagnostic Validation of the Screening Corneal Objective Risk of Ectasia Analyzer Evaluated by Swept Source Optical Coherence Tomography for Keratoconus in an Asian Population" Bioengineering 10, no. 11: 1335. https://doi.org/10.3390/bioengineering10111335
APA StyleKim, K., Koh, K., Lee, S., & Lee, Y. (2023). Diagnostic Validation of the Screening Corneal Objective Risk of Ectasia Analyzer Evaluated by Swept Source Optical Coherence Tomography for Keratoconus in an Asian Population. Bioengineering, 10(11), 1335. https://doi.org/10.3390/bioengineering10111335








