Artificial Tear Instillation-Induced Changes in Corneal Topography
Abstract
1. Introduction
2. Methods
2.1. Study Design and Patients
2.2. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Melles, R.B.; Holladay, J.T.; Chang, W.J. Accuracy of Intraocular Lens Calculation Formulas. Ophthalmology 2018, 125, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Melles, R.B.; Kane, J.X.; Olsen, T.; Chang, W.J. Update on Intraocular Lens Calculation Formulas. Ophthalmology 2019, 126, 1334–1335. [Google Scholar] [CrossRef] [PubMed]
- Nibandhe, A.S.; Donthineni, P.R. Understanding and Optimizing Ocular Biometry for Cataract Surgery in Dry Eye Disease: A Review. Semin. Ophthalmol. 2023, 38, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Lemp, M.A.; Foulks, G.N. The definition and classification of dry eye disease: Report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop. Ocul. Surf. 2007, 5, 75–92. [Google Scholar] [CrossRef]
- Dana, R.; Bradley, J.L.; Guerin, A.; Pivneva, I.; Stillman, I.; Evans, A.M.; Schaumberg, D.A. Estimated Prevalence and Incidence of Dry Eye Disease Based on Coding Analysis of a Large, All-age United States Health Care System. Am. J. Ophthalmol. 2019, 202, 47–54. [Google Scholar] [CrossRef]
- Liu, Z.; Pflugfelder, S.C. Corneal surface regularity and the effect of artificial tears in aqueous tear deficiency. Ophthalmology 1999, 106, 939–943. [Google Scholar] [CrossRef]
- Kim, J.; Kim, M.K.; Ha, Y.; Paik, H.J.; Kim, D.H. Improved accuracy of intraocular lens power calculation by preoperative management of dry eye disease. BMC Ophthalmol. 2021, 21, 364. [Google Scholar] [CrossRef]
- Montés-Micó, R.; Cáliz, A.; Alió, J.L. Changes in ocular aberrations after instillation of artificial tears in dry-eye patients. J. Cataract Refract. Surg. 2004, 30, 1649–1652. [Google Scholar] [CrossRef]
- Röggla, V.; Leydolt, C.; Schartmüller, D.; Schwarzenbacher, L.; Meyer, E.; Abela-Formanek, C.; Menapace, R. Influence of Artificial Tears on Keratometric Measurements in Cataract Patients. Am. J. Ophthalmol. 2021, 221, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Kathuria, A.; Shamloo, K.; Jhanji, V.; Sharma, A. Categorization of Marketed Artificial Tear Formulations Based on Their Ingredients: A Rational Approach for Their Use. J. Clin. Med. 2021, 10, 1289. [Google Scholar] [CrossRef] [PubMed]
- Bogan, S.J.; Waring, G.O., 3rd; Ibrahim, O.; Drews, C.; Curtis, L. Classification of normal corneal topography based on computer-assisted videokeratography. Arch. Ophthalmol. 1990, 108, 945–949. [Google Scholar] [CrossRef]
- Montés-Micó, R.; Cerviño, A.; Ferrer-Blasco, T.; García-Lázaro, S.; Ortí-Navarro, S. Optical quality after instillation of eyedrops in dry-eye syndrome. J. Cataract Refract. Surg. 2010, 36, 935–940. [Google Scholar] [CrossRef]
- Pavlopoulos, G.P.; Horn, J.; Feldman, S.T. The Effect of Artificial Tears on Computer-assisted Corneal Topography in Normal Eyes and After Penetrating Keratoplasty. Am. J. Ophthalmol. 1995, 119, 712–722. [Google Scholar] [CrossRef] [PubMed]
- Solomon, R.; Perry, H.D.; Donnenfeld, E.D.; Greenman, H.E. Slitlamp biomicroscopy of the tear film of patients using topical Restasis and Refresh Endura. J. Cataract Refract. Surg. 2005, 31, 661–663. [Google Scholar] [CrossRef] [PubMed]
- Garrett, Q.; Simmons, P.A.; Xu, S.; Vehige, J.; Zhao, Z.; Ehrmann, K.; Willcox, M. Carboxymethylcellulose binds to human corneal epithelial cells and is a modulator of corneal epithelial wound healing. Investig. Ophthalmol. Vis. Sci. 2007, 48, 1559–1567. [Google Scholar] [CrossRef] [PubMed]
- Hye-Min, S.; Mijung, P.; So Ra, K. The Effect of Difference in Main Components of Artifical Tears on Tear Film Stability of Soft Contact Lenses Wearers. J. Korean Ophthalmic Opt. Soc. 2016, 21, 351–360. [Google Scholar] [CrossRef]
- Zimmer, A.K.; Maincent, P.; Thouvenot, P.; Kreuter, J. Hydrocortisone delivery to healthy and inflamed eyes using a micellar polysorbate 80 solution or albumin nanoparticles. Int. J. Pharm. 1994, 110, 211–222. [Google Scholar] [CrossRef]
- Park, D.-Y.; Lim, D.H.; Hwang, S.; Hyun, J.; Chung, T.-Y. Comparison of astigmatism prediction error taken with the Pentacam measurements, Baylor nomogram, and Barrett formula for toric intraocular lens implantation. BMC Ophthalmol. 2017, 17, 156. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.-H.; Pu, C.; Lin, K.-K.; Lee, J.-S.; Hou, C.-H. Prediction of residual astigmatism in cataract surgery at different diameter zones using optical biometry measurement. Sci. Rep. 2022, 12, 4305. [Google Scholar] [CrossRef]
- Ho, Y.-J.; Sun, C.-C.; Lee, J.-S.; Lin, K.-K.; Hou, C.-H. Comparison of using Galilei Dual Scheimpflug Analyzer G4 and Barrett formula in predicting low cylinder preoperatively for cataract surgeries. Eur. J. Ophthalmol. 2020, 30, 1320–1327. [Google Scholar] [CrossRef]
- Abulafia, A.; Barrett, G.D.; Kleinmann, G.; Ofir, S.; Levy, A.; Marcovich, A.L.; Michaeli, A.; Koch, D.D.; Wang, L.; Assia, E.I. Prediction of refractive outcomes with toric intraocular lens implantation. J. Cataract Refract. Surg. 2015, 41, 936–944. [Google Scholar] [CrossRef]
- Reitblat, O.; Levy, A.; Kleinmann, G.; Assia, E.I. Accuracy of intraocular lens power calculation using three optical biometry measurement devices: The OA-2000, Lenstar-LS900 and IOLMaster-500. Eye 2018, 32, 1244–1252. [Google Scholar] [CrossRef]
- Novak, K.D.; Kohnen, T.; Chang-Godinich, A.; Soper, B.A.; Kennedy, P.; Wang, Q.; Padrick, T.; Koch, D.D. Changes in computerized videokeratography induced by artificial tears. J. Cataract Refract. Surg. 1997, 23, 1023–1028. [Google Scholar] [CrossRef]
- Yu, J.; Wu, M.; Crosser, V.; Tauber, J. Changes in corneal topography after instillation of artificial lubricants. ARVO abstract 4345. Investig. Ophthalmol. Vis. Sci. 1994, 35, 2194. [Google Scholar]
- Hasegawa, Y.; Okamoto, F.; Nakano, S.; Hiraoka, T.; Oshika, T. Effect of preoperative corneal astigmatism orientation on results with a toric intraocular lens. J. Cataract Refract. Surg. 2013, 39, 1846–1851. [Google Scholar] [CrossRef] [PubMed]
- Mimouni, M.; Nemet, A.; Pokroy, R.; Sela, T.; Munzer, G.; Kaiserman, I. The effect of astigmatism axis on visual acuity. Eur. J. Ophthalmol. 2017, 27, 308–311. [Google Scholar] [CrossRef] [PubMed]
- Huang, F.C.; Tseng, S.H.; Shih, M.H.; Chen, F.K. Effect of artificial tears on corneal surface regularity, contrast sensitivity, and glare disability in dry eyes. Ophthalmology 2002, 109, 1934–1940. [Google Scholar] [CrossRef] [PubMed]
- Starr, C.E.; Gupta, P.K.; Farid, M.; Beckman, K.A.; Chan, C.C.; Yeu, E.; Gomes, J.A.; Ayers, B.D.; Berdahl, J.P.; Holland, E.J. An algorithm for the preoperative diagnosis and treatment of ocular surface disorders. J. Cataract Refract. Surg. 2019, 45, 669–684. [Google Scholar] [CrossRef]
- Epitropoulos, A.T.; Matossian, C.; Berdy, G.J.; Malhotra, R.P.; Potvin, R. Effect of tear osmolarity on repeatability of keratometry for cataract surgery planning. J. Cataract Refract. Surg. 2015, 41, 1672–1677. [Google Scholar] [CrossRef] [PubMed]
- Hovanesian, J.; Epitropoulos, A.; Donnenfeld, E.D.; Holladay, J.T. The Effect of Lifitegrast on Refractive Accuracy and Symptoms in Dry Eye Patients Undergoing Cataract Surgery. Clin. Ophthalmol. 2020, 14, 2709–2716. [Google Scholar] [CrossRef]
| Product | Refresh Plus® Lubricant Eye Drops | Revita® Eye Drops |
|---|---|---|
| Active ingredient | 0.5% sodium carboxymethyl cellulose | 1.0% polysorbate 80 |
| Other ingredients | Sodium chloride, sodium lactate solution, potassium chloride, calcium chloride hydrate, magnesium chloride hydrate, hydrochloric acid, sodium hydroxide, purified water | Sodium chloride, D-mannitol, retinyl palmitate, citric acid, sodium citrate hydrate, disodium edetate hydrate, sodium hydroxide, water for injection |
| Preservative | None | None |
| Manufacturer | Allergan | Eden pharma |
| Volume (mL) | 0.8 | 0.4 |
| Use | The instillation of 1 drop of artificial tear | The instillation of 1 drop of artificial tear |
| All (n = 135) | PSB (n = 101) | CMC (n = 34) | p Value | |
|---|---|---|---|---|
| Age (years) | 57.2 ± 16.6 | 58.5 ± 16.0 | 53.4 ± 17.9 | 0.125 |
| Sex (M/F) | 65/75 | 48/53 | 17/17 | 0.803 † |
| Laterality (R/L) | 84/51 | 67/34 | 17/17 | 0.089 † |
| Steep Sim K (D) | 44.59 ± 2.48 | 44.52 ± 2.56 | 44.79 ± 2.24 | 0.576 |
| Flat Sim K (D) | 43.21 ± 2.00 | 43.21 ± 1.99 | 43.21 ± 2.02 | 0.987 |
| Mean Sim K (D) | 43.90 ± 2.02 | 43.86 ± 2.04 | 44.00 ± 1.97 | 0.725 |
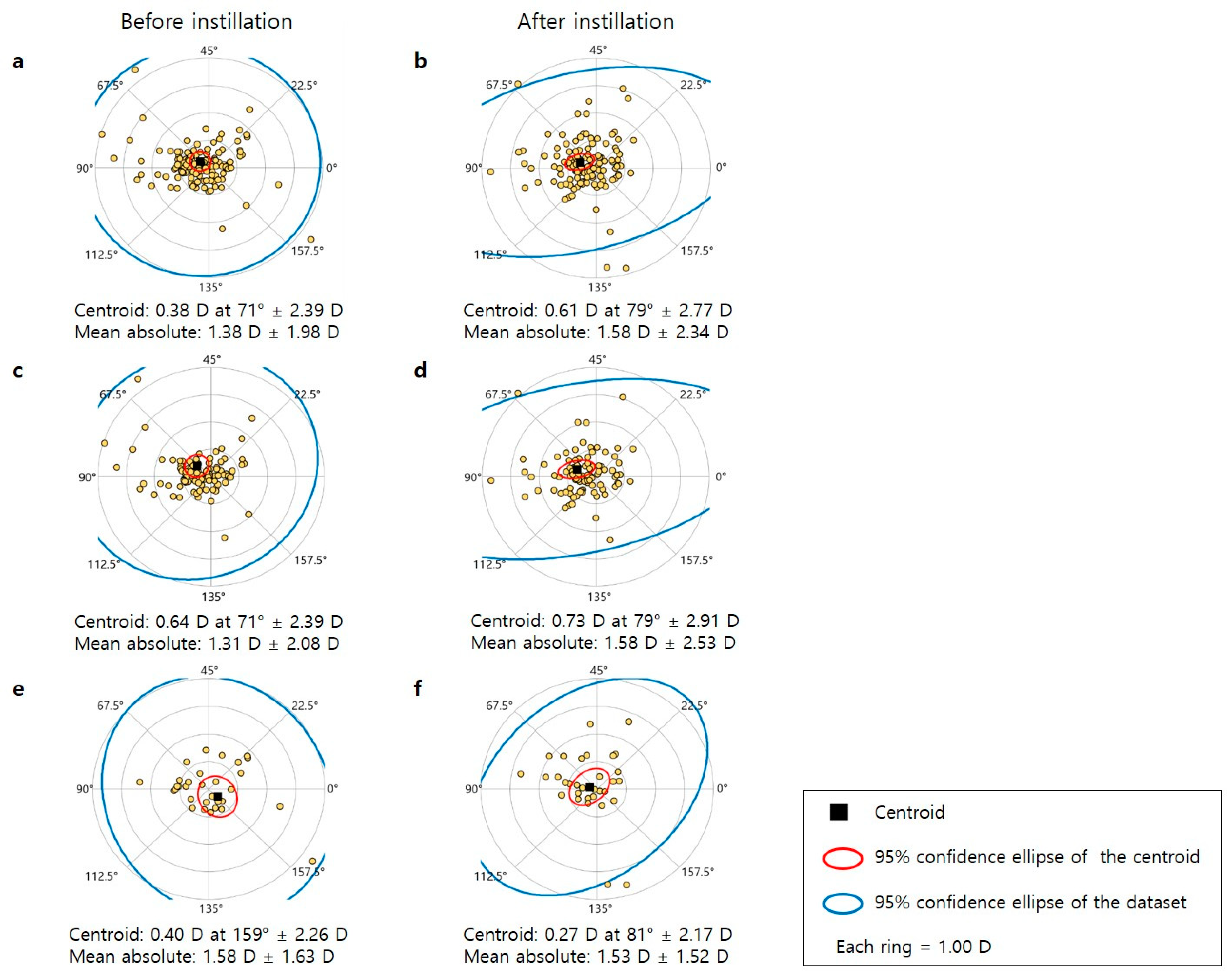
| Sim Kastig (D) | 1.38 ± 2.00 | 1.31 ± 2.10 | 1.58 ± 1.65 | 0.496 |
| Axis of Sim Kastig (°) | 80.95 | 77.87 | 90.09 | 0.216 |
| KPI (%) | 19.27 ± 21.1 | 19.7 ± 20.7 | 18.0 ± 22.4 | 0.679 |
| Kappa distance (mm) | 0.37 ± 0.34 | 0.38 ± 0.37 | 0.34 ± 0.21 | 0.560 |
| TBUT (sec) | 5.14 ± 1.07 | 5.02 ± 1.16 | 5.50 ± 0.62 | 0.199 |
| Cornea OSS (points) | 0.48 ± 0.84 | 0.52 ± 0.87 | 0.36 ± 0.74 | 0.359 |
| Before Eye Drops | After Eye Drops | p Value | |
|---|---|---|---|
| All (PSB + CMC, n = 135) | |||
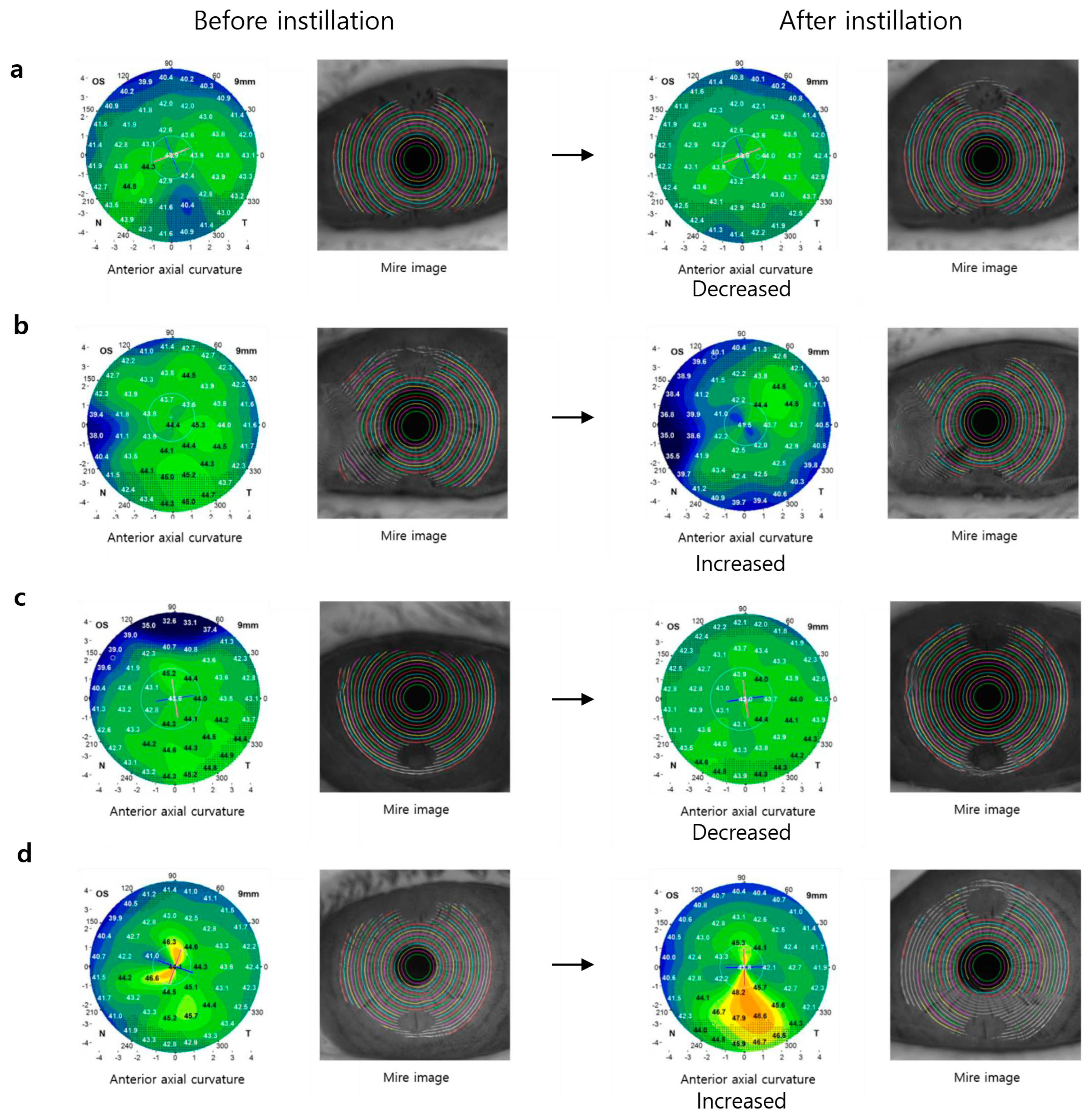
| Mean Sim K (D) | 43.90 ± 2.02 | 44.07 ± 2.26 | 0.006 * |
| Astigmatism of Sim K (D) | 1.38 ± 1.99 | 1.49 ± 2.03 | 0.095 |
| Steep axis of astigmatism (°) | 80.9 ± 43.6 | 83.1 ± 40.0 | 0.558 |
| Changes in the axis of astigmatism ≥ 10° (n, %) | NA | 70 (51.9%) | |
| Changes in the axis of astigmatism ≥ 30° (n, %) | NA | 27 (20.0%) | |
| Central K of anterior axial curvature (D) | 43.90 ± 2.03 | 43.80 ± 4.39 | 0.548 |
| Mid K of anterior axial curvature (D) | 43.32 ± 1.84 | 43.42 ± 1.88 | 0.027 * |
| Peripheral K of anterior axial curvature (D) | 41.74 ± 1.66 | 41.78 ± 1.62 | 0.597 |
| Mean total corneal power (D) | 42.39 ± 4.20 | 42.77 ± 2.25 | 0.200 |
| Astigmatism of total corneal power (D) | 1.64 ± 2.56 | 1.79 ± 2.63 | 0.426 |
| Kappa distance | 0.37 ± 0.34 | 0.36 ± 0.30 | 0.659 |
| KPI (%) | 19.27 ± 21.06 | 17.53 ± 19.10 | 0.157 |
| PSB (n = 101) | |||
| Mean Sim K (D) | 43.86 ± 2.04 | 44.04 ± 2.36 | 0.012 * |
| Astigmatism of Sim K (D) | 1.31 ± 2.10 | 1.48 ± 2.17 | 0.049 * |
| Changes in the axis of astigmatism ≥ 10° (n, %) | NA | 51 (50.5%) | |
| Changes in the axis of astigmatism ≥ 30° (n, %) | NA | 22 (21.8%) | |
| Mean total corneal power (D) | 42.26 ± 4.73 | 42.73 ± 2.34 | 0.238 |
| Astigmatism of Total corneal power (D) | 1.50 ± 2.36 | 1.83 ± 2.89 | 0.120 |
| Kappa distance | 0.38 ± 0.37 | 0.38 ± 0.32 | 0.992 |
| KPI (%) | 19.70 ± 20.67 | 16.70 ± 16.12 | 0.028 * |
| CMC (n = 34) | |||
| Mean Sim K (D) | 44.00 ± 1.97 | 44.17 ± 1.93 | 0.230 |
| Astigmatism of Sim K (D) | 1.58 ± 1.65 | 1.53 ± 1.54 | 0.608 |
| Changes in the axis of astigmatism ≥ 10° (n, %) | NA | 19 (55.9%) | |
| Changes in the axis of astigmatism ≥ 30° (n, %) | NA | 5 (14.7%) | |
| Mean total corneal power (D) | 42.78 ± 1.86 | 42.91 ± 1.98 | 0.278 |
| Astigmatism of Total corneal power (D) | 2.06 ± 3.08 | 1.68 ± 1.68 | 0.365 |
| Kappa distance | 0.34 ± 0.21 | 0.30 ± 0.20 | 0.282 |
| KPI (%) | 17.97 ± 22.44 | 19.99 ± 26.18 | 0.460 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, Y.; Kim, T.H.; Paik, H.J.; Kim, D.H. Artificial Tear Instillation-Induced Changes in Corneal Topography. Bioengineering 2024, 11, 121. https://doi.org/10.3390/bioengineering11020121
Lee Y, Kim TH, Paik HJ, Kim DH. Artificial Tear Instillation-Induced Changes in Corneal Topography. Bioengineering. 2024; 11(2):121. https://doi.org/10.3390/bioengineering11020121
Chicago/Turabian StyleLee, Yunjin, Tae Hun Kim, Hae Jung Paik, and Dong Hyun Kim. 2024. "Artificial Tear Instillation-Induced Changes in Corneal Topography" Bioengineering 11, no. 2: 121. https://doi.org/10.3390/bioengineering11020121
APA StyleLee, Y., Kim, T. H., Paik, H. J., & Kim, D. H. (2024). Artificial Tear Instillation-Induced Changes in Corneal Topography. Bioengineering, 11(2), 121. https://doi.org/10.3390/bioengineering11020121






