Estimating Worldwide Impact of Low Physical Activity on Risk of Developing Ischemic Heart Disease-Related Disability: An Updated Search in the 2019 Global Health Data Exchange (GHDx)
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Source
2.3. Statistical Analysis
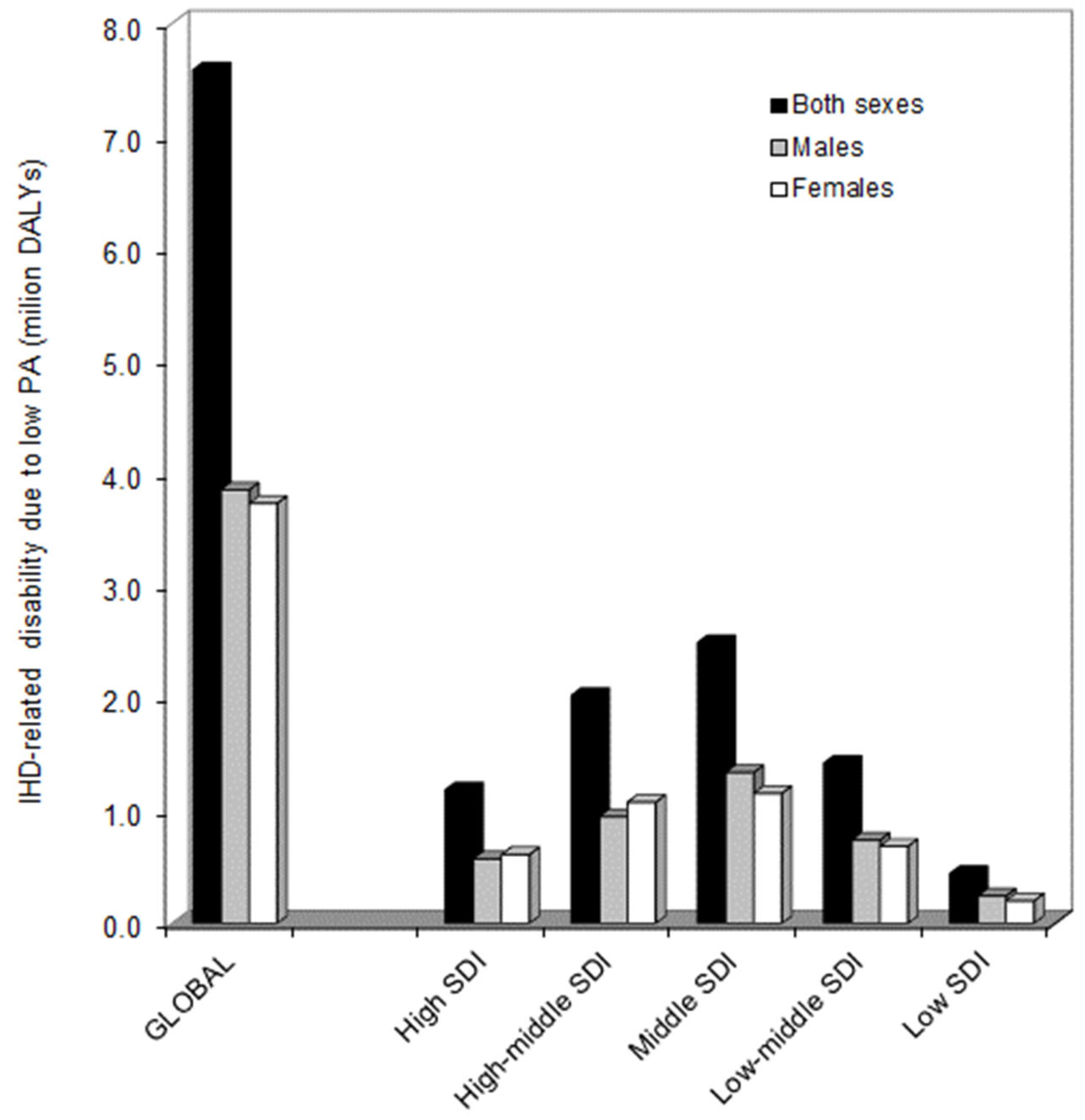
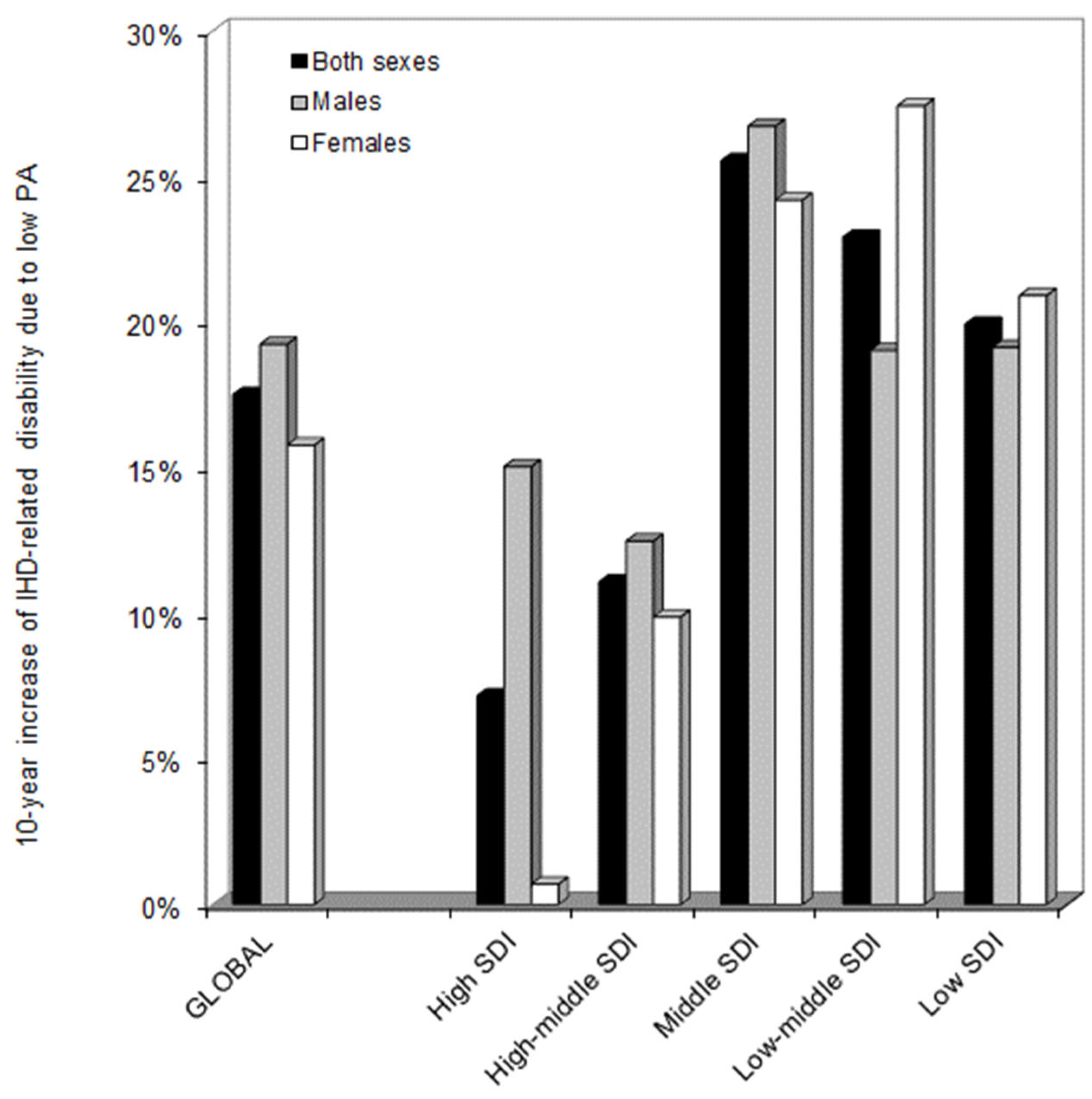
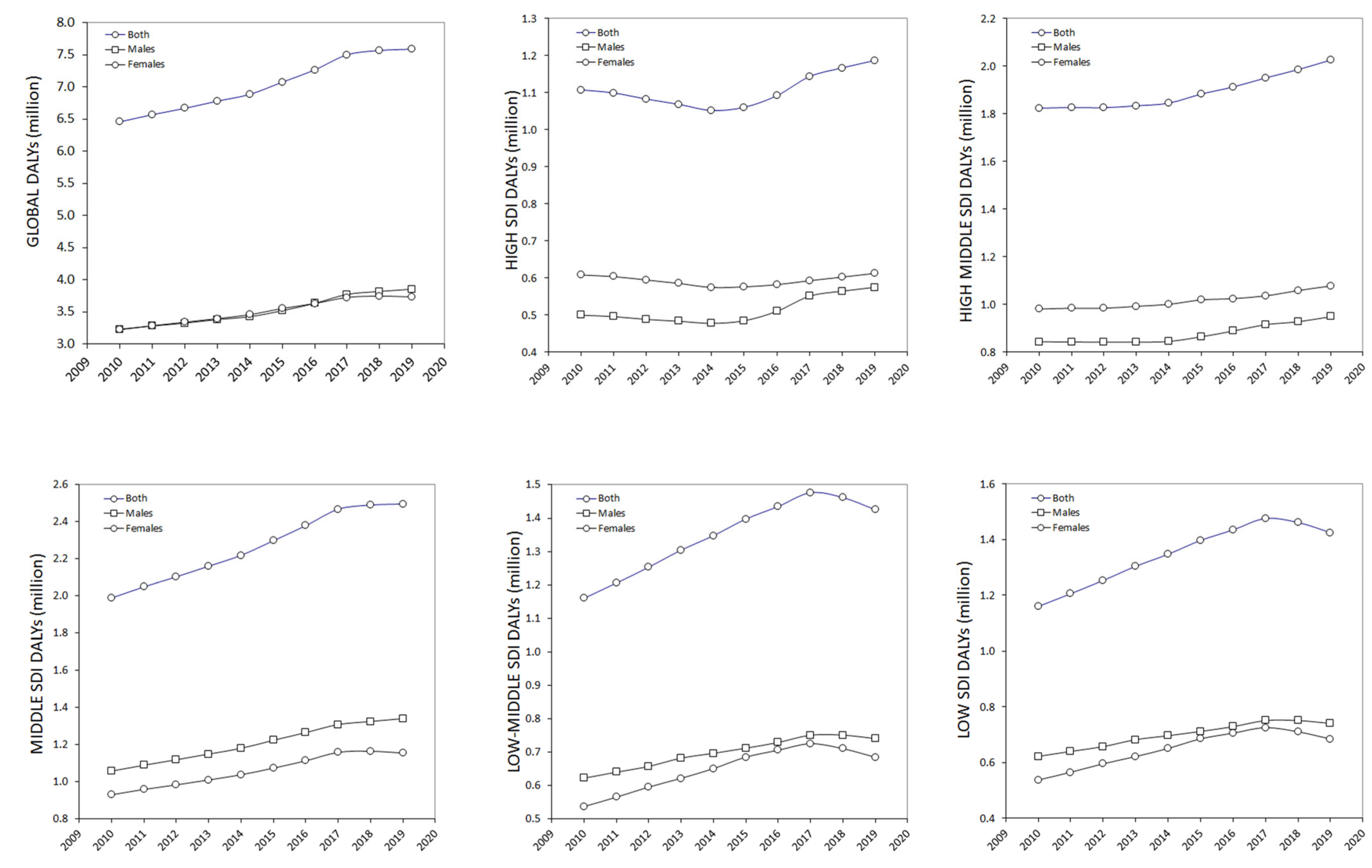
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Alonso, A.; Beaton, A.Z.; Bittencourt, M.S.; Boehme, A.K.; Buxton, A.E.; Carson, A.P.; Commodore-Mensah, Y.; et al. Heart Disease and Stroke Statistics-2022 Update: A Report From the American Heart Association. Circulation 2022, 145, e153–e639, Erratum in Circulation 2022, 146, e141. [Google Scholar] [CrossRef]
- Fletcher, G.F.; Blair, S.N.; Blumenthal, J.; Caspersen, C.; Chaitman, B.; Epstein, S.; Falls, H.; Froelicher, E.S.; Froelicher, V.F.; Pina, I.L. Statement on exercise. Benefits and recommendations for physical activity programs for all Americans. A statement for health professionals by the Committee on Exercise and Cardiac Rehabilitation of the Council on Clinical Cardiology, American Heart association. Circulation 1992, 86, 340–344. [Google Scholar] [CrossRef]
- Kahlmeier, S.; Wijnhoven, T.M.; Alpiger, P.; Schweizer, C.; Breda, J.; Martin, B.W. National physical activity recommendations: Systematic overview and analysis of the situation in European countries. BMC Public Health 2015, 15, 133. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The Physical Activity Guidelines for Americans. JAMA 2018, 320, 2020–2028. [Google Scholar] [CrossRef]
- Tcymbal, A.; Gelius, P.; Abu-Omar, K.; Foster, C.; Whiting, S.; Mendes, R.; Titze, S.; Dorner, T.E.; Halbwachs, C.; Duclos, M.; et al. Development of national physical activity recommendations in 18 EU member states: A comparison of methodologies and the use of evidence. BMJ Open 2021, 11, e041710. [Google Scholar] [CrossRef]
- Mok, A.; Khaw, K.T.; Luben, R.; Wareham, N.; Brage, S. Physical activity trajectories and mortality: Population based cohort study. BMJ 2019, 365, l2323. [Google Scholar] [CrossRef]
- Lee, I.M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T.; Lancet Physical Activity Series Working Group. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef]
- Carlson, S.A.; Adams, E.K.; Yang, Z.; Fulton, J.E. Percentage of Deaths Associated With Inadequate Physical Activity in the United States. Prev. Chronic Dis. 2018, 15, E38. [Google Scholar] [CrossRef]
- Cheng, W.; Zhang, Z.; Cheng, W.; Yang, C.; Diao, L.; Liu, W. Associations of leisure-time physical activity with cardiovascular mortality: A systematic review and meta-analysis of 44 prospective cohort studies. Eur. J. Prev. Cardiol. 2018, 25, 1864–1872. [Google Scholar] [CrossRef]
- Hansen, K.W.; Peytz, N.; Blokstra, A.; Bojesen, S.E.; Celis-Morales, C.; Chrysohoou, C.; Clays, E.; De Bacquer, D.; Galatius, S.; Gray, S.R.; et al. Association of fatal myocardial infarction with past level of physical activity: A pooled analysis of cohort studies. Eur. J. Prev. Cardiol. 2021, 28, 1590–1598. [Google Scholar] [CrossRef]
- Posadzki, P.; Pieper, D.; Bajpai, R.; Makaruk, H.; Könsgen, N.; Neuhaus, A.L.; Semwal, M. Exercise/physical activity and health outcomes: An overview of Cochrane systematic reviews. BMC Public Health 2020, 20, 1724. [Google Scholar] [CrossRef]
- Lippi, G.; Sanchis-Gomar, F. An Estimation of the Worldwide Epidemiologic Burden of Physical Inactivity-Related Ischemic Heart Disease. Cardiovasc. Drugs Ther. 2020, 34, 133–137. [Google Scholar] [CrossRef]
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Global Health Data Exchange. Global Burden of Disease Study 2019 (GBD 2019) Data Resources. Available online: https://ghdx.healthdata.org/gbd-2019 (accessed on 23 September 2022).
- Lippi, G.; Schena, F.; Guidi, G.C. Health benefits of physical activity. CMAJ 2006, 175, 776. [Google Scholar] [CrossRef]
- Lavie, C.J.; Ozemek, C.; Carbone, S.; Katzmarzyk, P.T.; Blair, S.N. Sedentary Behavior, Exercise, and Cardiovascular Health. Circ. Res. 2019, 124, 799–815. [Google Scholar] [CrossRef]
- Lippi, G.; Mattiuzzi, C.; Sanchis-Gomar, F. Physical exercise and migraine: For or against? Ann. Transl. Med. 2018, 6, 181. [Google Scholar] [CrossRef]
- Sanchis-Gomar, F.; Lavie, C.J.; Mehra, M.R.; Henry, B.M.; Lippi, G. Obesity and Outcomes in COVID-19: When an Epidemic and Pandemic Collide. Mayo Clin. Proc. 2020, 95, 1445–1453. [Google Scholar] [CrossRef]
- Ding, D.; Lawson, K.D.; Kolbe-Alexander, T.L.; Finkelstein, E.A.; Katzmarzyk, P.T.; van Mechelen, W.; Pratt, M.; Lancet Physical Activity Series 2 Executive Committee. The economic burden of physical inactivity: A global analysis of major non-communicable diseases. Lancet 2016, 388, 1311–1324. [Google Scholar] [CrossRef]
- Nikitara, K.; Odani, S.; Demenagas, N.; Rachiotis, G.; Symvoulakis, E.; Vardavas, C. Prevalence and correlates of physical inactivity in adults across 28 European countries. Eur. J. Public Health 2021, 31, 840–845. [Google Scholar] [CrossRef]
- Ozemek, C.; Lavie, C.J.; Rognmo, Ø. Global physical activity levels—Need for intervention. Prog. Cardiovasc. Dis. 2019, 62, 102–107. [Google Scholar] [CrossRef] [PubMed]
- Oja, P.; Titze, S. Physical activity recommendations for public health: Development and policy context. EPMA J. 2011, 2, 253–259. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef]
- Fletcher, G.F.; Landolfo, C.; Niebauer, J.; Ozemek, C.; Arena, R.; Lavie, C.J. Promoting Physical Activity and Exercise: JACC Health Promotion Series. J. Am. Coll. Cardiol. 2018, 72, 1622–1639. [Google Scholar] [CrossRef]
| Search Field | Search Term |
|---|---|
| Risk | “Low physical activity” |
| Measure | “DALYs” |
| Metric | “Number” |
| Cause | “Ischemic heart disease” |
| Location | “Global”; “High SDI”; “High–middle SDI”; “Middle SDI”; “Low–middle SDI”; “Low SDI” |
| Age | “+25 years” |
| Sex | “Both”; “Female”; Male” |
| Year | “2010”; “2011”; “2012”; “2013”; “2014”; “2015”; “2016”; “2017”; “2018”; “2019” |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lippi, G.; Sanchis-Gomar, F.; Mattiuzzi, C.; Lavie, C.J. Estimating Worldwide Impact of Low Physical Activity on Risk of Developing Ischemic Heart Disease-Related Disability: An Updated Search in the 2019 Global Health Data Exchange (GHDx). Medicines 2022, 9, 55. https://doi.org/10.3390/medicines9110055
Lippi G, Sanchis-Gomar F, Mattiuzzi C, Lavie CJ. Estimating Worldwide Impact of Low Physical Activity on Risk of Developing Ischemic Heart Disease-Related Disability: An Updated Search in the 2019 Global Health Data Exchange (GHDx). Medicines. 2022; 9(11):55. https://doi.org/10.3390/medicines9110055
Chicago/Turabian StyleLippi, Giuseppe, Fabian Sanchis-Gomar, Camilla Mattiuzzi, and Carl J. Lavie. 2022. "Estimating Worldwide Impact of Low Physical Activity on Risk of Developing Ischemic Heart Disease-Related Disability: An Updated Search in the 2019 Global Health Data Exchange (GHDx)" Medicines 9, no. 11: 55. https://doi.org/10.3390/medicines9110055
APA StyleLippi, G., Sanchis-Gomar, F., Mattiuzzi, C., & Lavie, C. J. (2022). Estimating Worldwide Impact of Low Physical Activity on Risk of Developing Ischemic Heart Disease-Related Disability: An Updated Search in the 2019 Global Health Data Exchange (GHDx). Medicines, 9(11), 55. https://doi.org/10.3390/medicines9110055








