Admission Serum Potassium Levels in Hospitalized Patients and One-Year Mortality
Abstract
1. Introduction
2. Methods
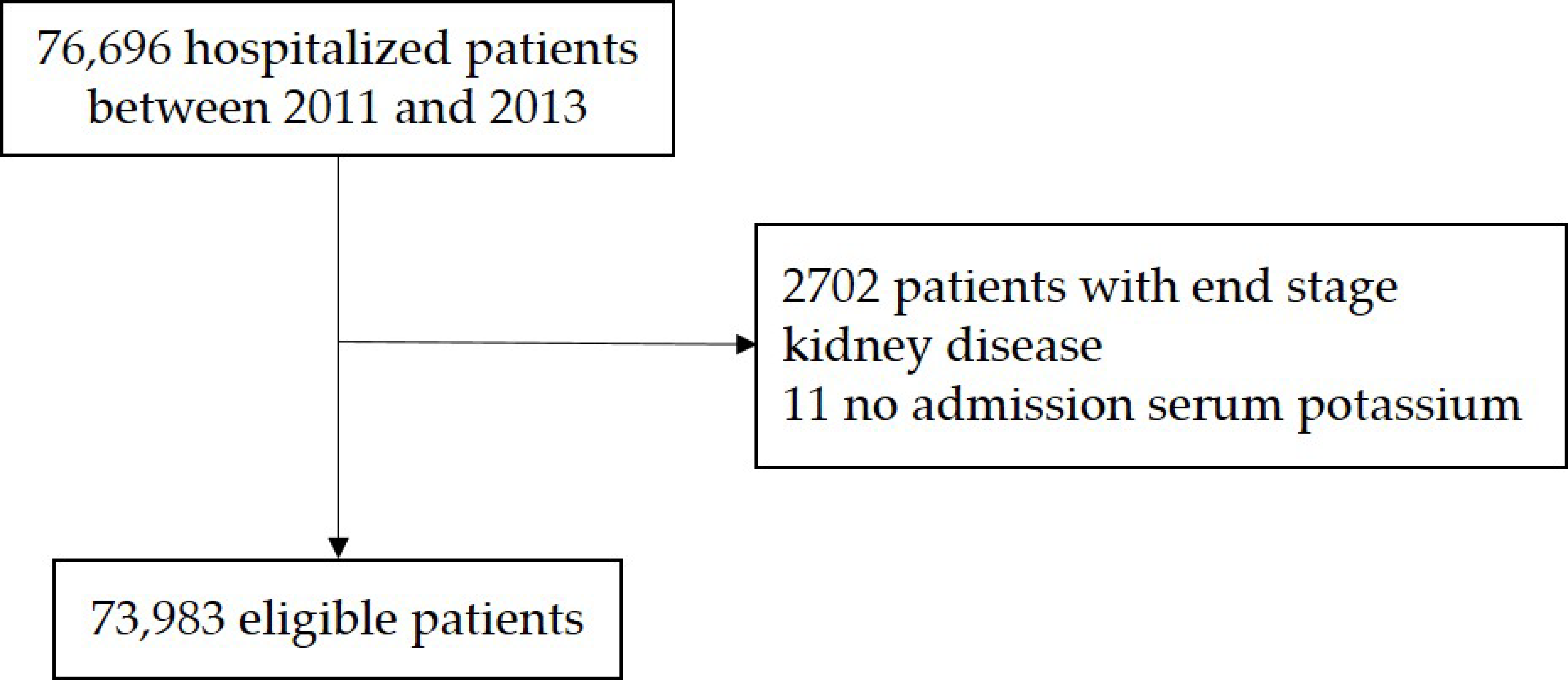
2.1. Patient Population
2.2. Statistical Analysis
3. Results
3.1. Baseline Characteristics
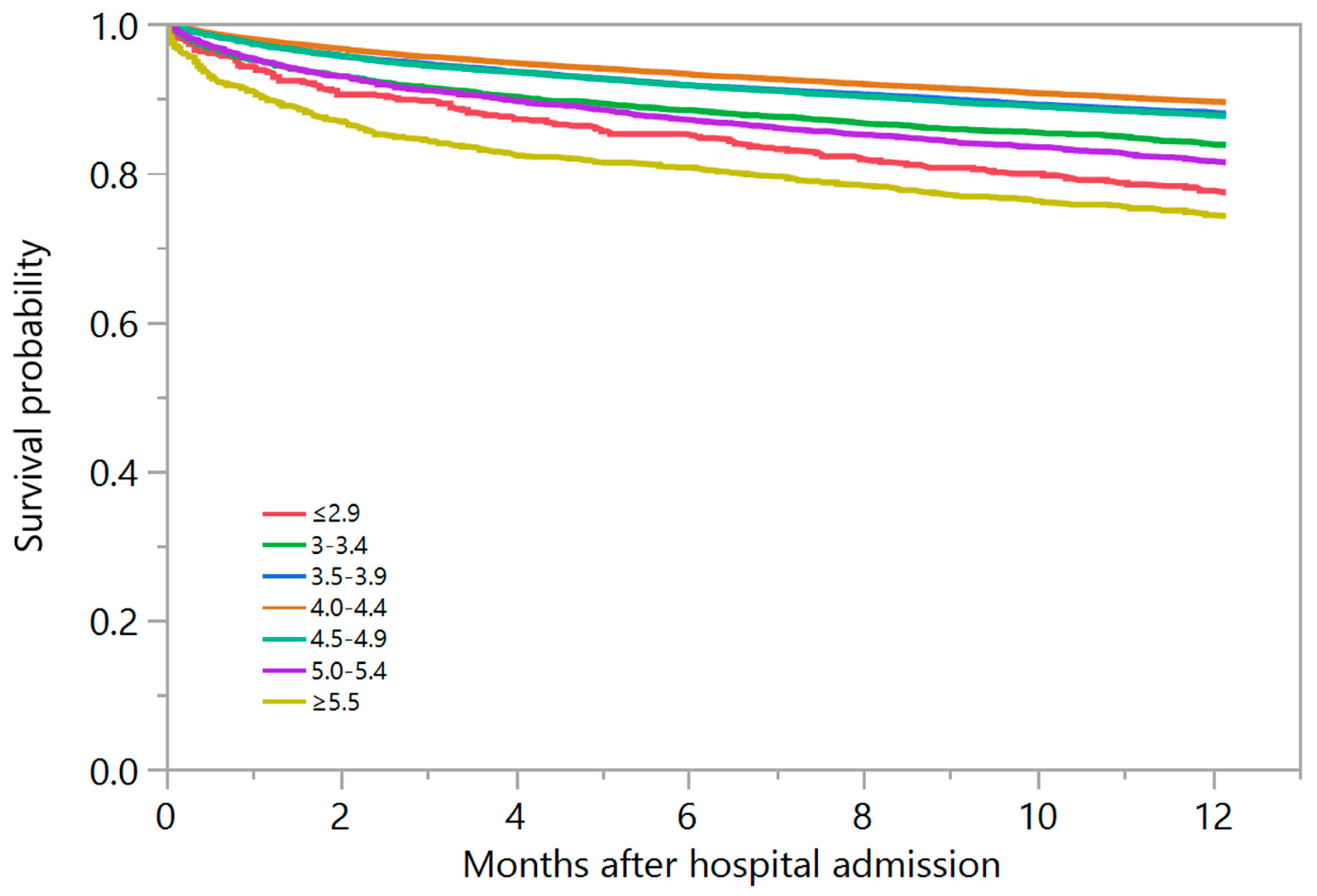
3.2. Admission Serum Potassium and One-Year Mortality
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Palaka, E.; Grandy, S.; Darlington, O.; McEwan, P.; van Doornewaard, A. Associations between serum potassium and adverse clinical outcomes: A systematic literature review. Int. J. Clin. Pract. 2019. [Google Scholar] [CrossRef]
- Collins, A.J.; Pitt, B.; Reaven, N.; Funk, S.; McGaughey, K.; Wilson, D.; Bushinsky, D.A. Association of Serum Potassium with All-Cause Mortality in Patients with and without Heart Failure, Chronic Kidney Disease, and/or Diabetes. Am. J. Nephrol. 2017, 46, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Bowling, C.B.; Pitt, B.; Ahmed, M.I.; Aban, I.B.; Sanders, P.W.; Mujib, M.; Campbell, R.C.; Love, T.E.; Aronow, W.S.; Allman, R.M.; et al. Hypokalemia and outcomes in patients with chronic heart failure and chronic kidney disease: Findings from propensity-matched studies. Circ. Heart Fail. 2010, 3, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Acker, C.G.; Johnson, J.P.; Palevsky, P.M.; Greenberg, A. Hyperkalemia in hospitalized patients: Causes, adequacy of treatment, and results of an attempt to improve physician compliance with published therapy guidelines. Arch. Intern. Med. 1998, 158, 917–924. [Google Scholar] [CrossRef] [PubMed]
- Paice, B.J.; Paterson, K.R.; Onyanga-Omara, F.; Donnelly, T.; Gray, J.M.; Lawson, D.H. Record linkage study of hypokalaemia in hospitalized patients. Postgrad. Med. J. 1986, 62, 187–191. [Google Scholar] [CrossRef] [PubMed]
- Cheungpasitporn, W.; Thongprayoon, C.; Kittanamongkolchai, W.; Sakhuja, A.; Mao, M.A.; Erickson, S.B. Impact of admission serum potassium on mortality in patients with chronic kidney disease and cardiovascular disease. QJM 2017, 110, 713–719. [Google Scholar] [CrossRef] [PubMed]
- Hoppe, L.K.; Muhlack, D.C.; Koenig, W.; Carr, P.R.; Brenner, H.; Schottker, B. Association of Abnormal Serum Potassium Levels with Arrhythmias and Cardiovascular Mortality: A Systematic Review and Meta-Analysis of Observational Studies. Cardiovasc. Drugs Ther. 2018, 32, 197–212. [Google Scholar] [CrossRef] [PubMed]
- Colombo, M.G.; Kirchberger, I.; Amann, U.; Dinser, L.; Meisinger, C. Association of serum potassium concentration with mortality and ventricular arrhythmias in patients with acute myocardial infarction: A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2018, 25, 576–595. [Google Scholar] [CrossRef]
- Siscovick, D.S.; Raghunathan, T.E.; Psaty, B.M.; Koepsell, T.D.; Wicklund, K.G.; Lin, X.; Cobb, L.; Rautaharju, P.M.; Copass, M.K.; Wagner, E.H. Diuretic therapy for hypertension and the risk of primary cardiac arrest. N. Engl. J. Med. 1994, 330, 1852–1857. [Google Scholar] [CrossRef]
- Cohen, H.W.; Madhavan, S.; Alderman, M.H. High and low serum potassium associated with cardiovascular events in diuretic-treated patients. J. Hypertens. 2001, 19, 1315–1323. [Google Scholar] [CrossRef]
- Basnet, S.; Dhital, R.; Tharu, B.; Ghimire, S.; Poudel, D.R.; Donato, A. Influence of abnormal potassium levels on mortality among hospitalized heart failure patients in the US: Data from National Inpatient Sample. J. Commun. Hosp. Intern. Med. Perspect. 2019, 9, 103–107. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Chen, P.; Chen, J.; Wang, L.; Wei, Y.; Xu, D. Association of Low Serum Potassium Levels and Risk for All-Cause Mortality in Patients With Chronic Kidney Disease: A Systematic Review and Meta-Analysis. Ther. Apher. Dial. 2019, 23, 22–31. [Google Scholar] [CrossRef] [PubMed]
- Kovesdy, C.P. Epidemiology of hyperkalemia: An update. Kidney Int. Suppl. 2016, 6, 3–6. [Google Scholar] [CrossRef] [PubMed]
- Fleet, J.L.; Shariff, S.Z.; Gandhi, S.; Weir, M.A.; Jain, A.K.; Garg, A.X. Validity of the International Classification of Diseases 10th revision code for hyperkalaemia in elderly patients at presentation to an emergency department and at hospital admission. BMJ Open 2012, 2. [Google Scholar] [CrossRef] [PubMed]
- Kovesdy, C.P. Updates in hyperkalemia: Outcomes and therapeutic strategies. Rev. Endoc. Metab. Disord. 2017, 18, 41–47. [Google Scholar] [CrossRef]
- Brueske, B.; Sidhu, M.S.; Schulman-Marcus, J.; Kashani, K.B.; Barsness, G.W.; Jentzer, J.C. Hyperkalemia Is Associated With Increased Mortality Among Unselected Cardiac Intensive Care Unit Patients. J. Am. Heart Assoc. 2019, 8, e011814. [Google Scholar] [CrossRef]
- Xi, H.; Yu, R.H.; Wang, N.; Chen, X.Z.; Zhang, W.C.; Hong, T. Serum potassium levels and mortality of patients with acute myocardial infarction: A systematic review and meta-analysis of cohort studies. Eur. J. Prev. Cardiol. 2019, 26, 145–156. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., III; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef]
- Charlson, M.; Szatrowski, T.P.; Peterson, J.; Gold, J. Validation of a combined comorbidity index. J. Clin. Epidemiol. 1994, 47, 1245–1251. [Google Scholar] [CrossRef]
- Weiss, J.N.; Qu, Z.; Shivkumar, K. Electrophysiology of Hypokalemia and Hyperkalemia. Circ. Arrhythm. Electrophysiol. 2017, 10. [Google Scholar] [CrossRef]
- Skogestad, J.; Aronsen, J.M. Hypokalemia-Induced Arrhythmias and Heart Failure: New Insights and Implications for Therapy. Front. Physiol. 2018, 9, 1500. [Google Scholar] [CrossRef] [PubMed]
- Janse, M.J.; van Capelle, F.J.; Morsink, H.; Kleber, A.G.; Wilms-Schopman, F.; Cardinal, R.; d’Alnoncourt, C.N.; Durrer, D. Flow of “injury” current and patterns of excitation during early ventricular arrhythmias in acute regional myocardial ischemia in isolated porcine and canine hearts. Evidence for two different arrhythmogenic mechanisms. Circ. Res. 1980, 47, 151–165. [Google Scholar] [CrossRef] [PubMed]
| Variables | All | Serum Potassium Level at Hospital Admission (mEq/L) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| ≤2.9 | 3.0–3.4 | 3.5–3.9 | 4.0–4.4 | 4.5–4.9 | 5.0–5.4 | ≥5.5 | p | ||
| N | 73,983 | 700 | 3943 | 17,315 | 29,815 | 16,381 | 4463 | 1366 | |
| Age (year) | 61 ± 18 | 59 ± 18 | 60 ± 19 | 58 ± 19 | 61 ± 18 | 63 ± 17 | 66 ± 16 | 67 ± 16 | <0.001 |
| Male | 38,973 (53) | 273 (39) | 1556 (39) | 7999 (46) | 16,131 (54) | 9522 (58) | 2670 (60) | 822 (60) | <0.001 |
| Caucasian | 68,809 (93) | 642 (92) | 3562 (9) | 15,819 (91) | 27,791 (93) | 15,497 (95) | 4220 (95) | 1278 (94) | <0.001 |
| eGFR (mL/min/1.73 m2) | 80 ± 26 | 82 ± 34 | 84 ± 28 | 86 ± 26 | 82 ± 25 | 76 ± 25 | 67 ± 27 | 54 ± 27 | <0.001 |
| Principal diagnosis | <0.001 | ||||||||
| 15,716 (21) | 128 (18) | 844 (21) | 3747 (22) | 6291 (21) | 3380 (21) | 1019 (23) | 307 (22) | |
| 1879 (3) | 75 (11) | 137 (3) | 384 (2) | 558 (2) | 459 (3) | 158 (4) | 108 (8) | |
| 6920 (9) | 80 (11) | 537 (14) | 1824 (11) | 2594 (9) | 1335 (8) | 429 (10) | 121 (9) | |
| 11,558 (16) | 59 (8) | 347 (9) | 2000 (12) | 4756 (16) | 3209 (20) | 953 (21) | 234 (17) | |
| 2171 (3) | 51 (7) | 269 (7) | 600 (3) | 705 (2) | 374 (2) | 111 (2) | 61 (4) | |
| 2968 (4) | 25 (4) | 213 (5) | 638 (4) | 1098 (4) | 673 (4) | 222 (5) | 99 (7) | |
| 11,434 (15) | 140 (20) | 699 (18) | 3070 (18) | 4573 (15) | 2248 (14) | 528 (11) | 176 (13) | |
| 21,337 (29) | 142 (20) | 897 (23) | 5052 (29) | 9240 (31) | 4703 (29) | 1043 (23) | 260 (19) | |
| Charlson score | 1.7 ± 2.3 | 1.8 ± 2.5 | 1.7 ± 2.3 | 1.5 ± 2.2 | 1.6 ± 2.2 | 1.9 ± 2.4 | 2.3 ± 2.6 | 2.8 ± 2.7 | <0.001 |
| Comorbidities | |||||||||
| 5260 (7) | 38 (5) | 227 (6) | 1009 (6) | 2042 (7) | 1347 (8) | 423 (9) | 174 (13) | <0.001 |
| 4679 (6) | 60 (9) | 275 (7) | 965 (6) | 1665 (6) | 1112 (7) | 421 (9) | 181 (13) | <0.001 |
| 2065 (3) | 20 (3) | 106 (3) | 371 (2) | 736 (2) | 552 (3) | 199 (4) | 81 (6) | <0.001 |
| 5228 (7) | 52 (7) | 315 (8) | 1118 (6) | 1944 (7) | 1247 (8) | 398 (9) | 154 (11) | <0.001 |
| 13,752 (19) | 114 (16) | 669 (17) | 2743 (16) | 5096 (17) | 3414 (21) | 1206 (27) | 510 (37) | <0.001 |
| 6131 (8) | 56 (8) | 326 (8) | 1197 (7) | 2227 (7) | 1518 (9) | 586 (13) | 221 (16) | <0.001 |
| 1713 (3) | 24 (3) | 114 (3) | 408 (2) | 581 (2) | 369 (2) | 150 (3) | 67 (5) | <0.001 |
| Medications | |||||||||
| 20,068 (27) | 162 (23) | 974 (25) | 4067 (23) | 7930 (27) | 4745 (29) | 1627 (36) | 563 (41) | <0.001 |
| 22,020 (30) | 341 (49) | 1659 (42) | 5452 (31) | 7974 (27) | 4508 (28) | 1490 (33) | 596 (44) | <0.001 |
| 8317 (11) | 401 (57) | 1025 (26) | 2246 (13) | 2731 (9) | 1336 (8) | 431 (10) | 147 (11) | <0.001 |
| Acute kidney injury | 7602 (10) | 113 (16) | 404 (10) | 1295 (7) | 2303 (8) | 1955 (12) | 953 (21) | 579 (42) | <0.001 |
| Mechanical ventilation | 6949 (9) | 131 (19) | 646 (16) | 2008 (12) | 2498 (8) | 1165 (7) | 338 (8) | 163 (12) | <0.001 |
| Electrolyte at admission | |||||||||
| 138 ± 4 | 137 ± 7 | 138 ± 5 | 138 ± 4 | 138 ± 4 | 138 ± 4 | 137 ± 4 | 136 ± 5 | <0.001 |
| 103 ± 5 | 101 ± 11 | 103 ± 6 | 103 ± 5 | 103 ± 4 | 103 ± 4 | 103 ± 5 | 102 ± 6 | <0.001 |
| 25 ± 3 | 25 ± 7 | 25 ± 4 | 25 ± 3 | 25 ± 3 | 25 ± 3 | 25 ± 4 | 24 ± 5 | <0.001 |
| Serum Potassium Level at Admission (mEq/L) | 1-Year Mortality (%) | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|---|
| HR (95% CI) | p | Adjusted HR (95% CI) | p | ||
| ≤2.9 | 22.6% | 2.34 (1.96–2.79) | <0.001 | 1.67 (1.39–2.01) | <0.001 |
| 3.0–3.4 | 16.4% | 1.66 (1.51–1.82) | <0.001 | 1.36 (1.23–1.49) | <0.001 |
| 3.5–3.9 | 12.1% | 1.16 (1.09–1.24) | <0.001 | 1.19 (1.11–1.26) | <0.001 |
| 4.0–4.4 | 10.6% | 1 (reference) | − | 1 (reference) | − |
| 4.5–4.9 | 12.4% | 1.20 (1.12–1.27) | <0.001 | 1.02 (0.96–1.09) | 0.46 |
| 5.0–5.4 | 18.6% | 1.87 (1.72–2.04) | <0.001 | 1.30 (1.19–1.41) | <0.001 |
| ≥5.5 | 25.8% | 2.84 (2.52–3.20) | <0.001 | 1.62 (1.43–1.83) | <0.001 |
| Serum Potassium Level at Admission (mEq/L) | 1-Year Mortality (%) | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|---|
| HR (95% CI) | p | Adjusted HR (95% CI) | p | ||
| ≤2.9 | 27.7% | 2.94 (2.02–4.27) | <0.001 | 2.30 (1.57–3.38) | <0.001 |
| 3.0–3.4 | 17.5% | 1.77 (1.45–2.17) | <0.001 | 1.64 (1.34–2.02) | <0.001 |
| 3.5–3.9 | 13.1% | 1.21 (1.06–1.38) | 0.005 | 1.29 (1.13–1.47) | <0.001 |
| 4.0–4.4 | 11.0% | 1 (reference) | − | 1 (reference) | − |
| 4.5–4.9 | 13.5% | 1.25 (1.09–1.43) | 0.001 | 1.02 (0.89–1.16) | 0.81 |
| 5.0–5.4 | 18.3% | 1.75 (1.46–2.10) | <0.001 | 1.14 (0.94–1.37) | 0.17 |
| ≥5.5 | 26.5% | 2.76 (2.15–3.54) | <0.001 | 1.47 (1.14–1.89) | 0.003 |
| Serum Potassium Level at Admission (mEq/L) | 1-Year Mortality (%) | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|---|
| HR (95% CI) | p | Adjusted HR (95% CI) | p | ||
| ≤2.9 | 32.5% | 1.82 (1.38–2.39) | <0.001 | 1.94 (1.47–2.56) | <0.001 |
| 3.0–3.4 | 23.6% | 1.28 (1.09–1.51) | 0.002 | 1.23 (1.05–1.45) | 0.01 |
| 3.5–3.9 | 22.5% | 1.18 (1.06–1.31) | 0.002 | 1.22 (1.10–1.36) | <0.001 |
| 4.0–4.4 | 19.6% | 1 (reference) | − | 1 (reference) | − |
| 4.5–4.9 | 18.9% | 0.97 (0.88–1.06) | 0.48 | 0.93 (0.84–1.02) | 0.12 |
| 5.0–5.4 | 25.0% | 1.33 (1.18–1.50) | <0.001 | 1.14 (1.01–1.28) | 0.03 |
| ≥5.5 | 29.6% | 1.70 (1.48–1.97) | <0.001 | 1.32 (1.14–1.53) | <0.001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thongprayoon, C.; Cheungpasitporn, W.; Hansrivijit, P.; Mao, M.A.; Medaura, J.; Bathini, T.; Chewcharat, A.; Erickson, S.B. Admission Serum Potassium Levels in Hospitalized Patients and One-Year Mortality. Medicines 2020, 7, 2. https://doi.org/10.3390/medicines7010002
Thongprayoon C, Cheungpasitporn W, Hansrivijit P, Mao MA, Medaura J, Bathini T, Chewcharat A, Erickson SB. Admission Serum Potassium Levels in Hospitalized Patients and One-Year Mortality. Medicines. 2020; 7(1):2. https://doi.org/10.3390/medicines7010002
Chicago/Turabian StyleThongprayoon, Charat, Wisit Cheungpasitporn, Panupong Hansrivijit, Michael A. Mao, Juan Medaura, Tarun Bathini, Api Chewcharat, and Stephen B. Erickson. 2020. "Admission Serum Potassium Levels in Hospitalized Patients and One-Year Mortality" Medicines 7, no. 1: 2. https://doi.org/10.3390/medicines7010002
APA StyleThongprayoon, C., Cheungpasitporn, W., Hansrivijit, P., Mao, M. A., Medaura, J., Bathini, T., Chewcharat, A., & Erickson, S. B. (2020). Admission Serum Potassium Levels in Hospitalized Patients and One-Year Mortality. Medicines, 7(1), 2. https://doi.org/10.3390/medicines7010002






