Inpatient Burden of Prurigo Nodularis in the United States
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Selection of Prurigo Nodularis Cohort
2.3. Statistical Analysis
3. Results
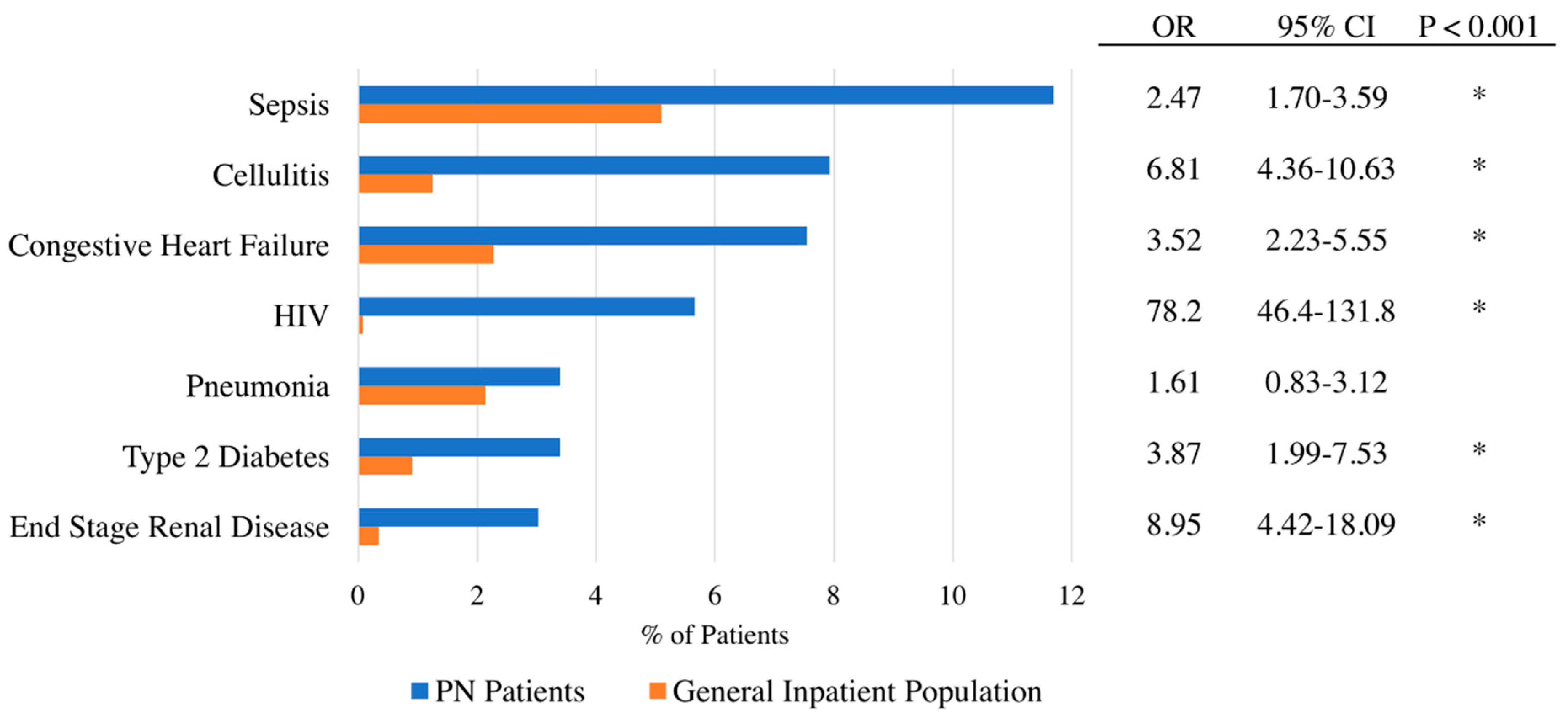
3.1. Factors Associated with Hospitalization for Prurigo Nodularis
3.2. Length of Stay and Cost of Care
3.3. Primary Reason for Admission of Prurigo Nodularis Patients
4. Discussion
Author Contributions
Funding
Institutional Review Board Status
Acknowledgments
Conflicts of Interest
References
- Pereira, M.P.; Steinke, S.; Zeidler, C.; Forner, C.; Riepe, C.; Augustin, M.; Bobko, S.; Dalgard, F.; Elberling, J.; Garcovich, S.; et al. European academy of dermatology and venereology European prurigo project: Expert consensus on the definition, classification and terminology of chronic prurigo. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 1059–1065. [Google Scholar] [CrossRef] [PubMed]
- Klein, D.; Phan, N.Q.; Grundmann, S.; Chatzigeorgakidis, E.; Iking, A.; Ständer, S. Prurigo as a symptom of atopic and non-atopic diseases: Aetiological survey in a consecutive cohort of 108 patients. J. Eur. Acad. Dermatol. Venereol. 2012, 27, 550–557. [Google Scholar]
- Konda, D.; Chandrashekar, L.; Rajappa, M.; Kattimani, S.; Thappa, D.M.; Ananthanarayanan, P.H. Serotonin and interleukin-6: Association with pruritus severity, sleep quality and depression severity in Prurigo Nodularis. Asian J. Psychiatry 2015, 17, 24–28. [Google Scholar] [CrossRef] [PubMed]
- Schneider, G.; Driesch, G.; Heuft, G.; Evers, S.; Luger, T.A.; Ständer, S. Psychosomatic cofactors and psychiatric comorbidity in patients with chronic itch. Clin. Exp. Dermatol. 2006, 31, 762–767. [Google Scholar] [CrossRef] [PubMed]
- Boozalis, E.; Tang, O.; Patel, S.; Semenov, Y.R.; Pereira, M.P.; Stander, S.; Kang, S.; Kwatra, S.G. Ethnic differences and comorbidities of 909 prurigo nodularis patients. J. Am. Acad. Dermatol. 2018, 79, 714–719. [Google Scholar] [CrossRef] [PubMed]
- Boccardi, D.; D’Auria, E.; Turati, F.; DI Vito, M.; Sortino, S.; Riva, E.; Cerri, A. Disease severity and quality of life in children with atopic dermatitis: PO-SCORAD in clinical practice. Minerva Pediatr. 2017, 69, 373–380. [Google Scholar] [PubMed]
- Coutanceau, C.; Stalder, J. Analysis of Correlations between Patient-Oriented SCORAD (PO-SCORAD) and Other Assessment Scores of Atopic Dermatitis Severity. Dermatology 2014, 229, 248–255. [Google Scholar] [CrossRef] [PubMed]
- Kneiber, D.; Valdebran, M.; Amber, K.T. Treatment-resistant prurigo nodularis: Challenges and solutions. Clin. Cosmet. Investig. Dermatol. 2019, 12, 163–172. [Google Scholar]
- Sonkoly, E.; Muller, A.; Lauerma, A.I.; Alenius, H.; Dieu-nosjean, M.; Meller, S.; Ruzicka, T.; Zlotnik, A.; Homey, B. IL-31: A new link between T cells and pruritus in atopic skin inflammation. J. Allergy Clin. Immunol. 2006, 117, 411–417. [Google Scholar] [CrossRef] [PubMed]
- D’Auria, E.; Banderali, G.; Barberi, S.; Gualandri, L.; Pietra, B. Atopic dermatitis: Recent insight on pathogenesis and novel therapeutic target. Asian Pac. J. Allergy Immunol. 2016, 34, 98–108. [Google Scholar]
- Tanaka, M.; Aiba, S.; Matsumura, N.; Aoyama, H.; Tagami, H. Prurigo nodularis consists of two distinct forms: Early-onset atopic and late-onset non-atopic. Dermatology 1995, 190, 269–276. [Google Scholar] [CrossRef]
- Larson, V.A.; Tang, O.; Stander, S.; Miller, L.S.; Kang, S.; Kwatra, S.G. Association between prurigo nodularis and malignancy in middle-aged adults. J. Am. Acad. Dermatol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Diagnoses of HIV Infection in the United States and Dependent Areas. 2017. Available online: http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html (accessed on 2 August 2019).
- Magand, F.; Nacher, M.; Cazorla, C.; Cambazard, F.; Marie, D.S.; Couppié, P. Predictive values of prurigo nodularis and herpes zoster for HIV infection and immunosuppression requiring HAART in French Guiana. Trans. R. Soc. Trop. Med. Hyg. 2011, 105, 401–404. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Tang, W.; Sang, Y.; Chen, X.; Hu, X. Prevalence of chronic kidney disease-associated pruritus among adult dialysis patients. Medicine 2018, 97, 10633. [Google Scholar]
- Winhoven, S.M.; Gawkrodger, D.J. Nodular prurigo: Metabolic diseases are a common association. Clin. Exp. Dermatol. 2007, 32, 224–225. [Google Scholar] [CrossRef] [PubMed]
| Variable | General Inpatient Population without a Diagnosis of Prurigo Nodularis | Patients with Prurigo Nodularis | Adjusted OR | p-Value | ||
|---|---|---|---|---|---|---|
| Est. Frequency | Percent (95% Confidence Interval) | Est. Frequency | Percent (95% Confidence Interval) | |||
| AGE, y | ||||||
| 0–17 | 5,479,694 | 15.3 [14.9–15.9] | 5 | 0.38 [0.05–2.64] | 0.04 | 0.002 |
| 18–39 | 7,423,759 | 20.8 [20.5–21.0] | 210 | 15.8 [11.8–20.9] | 1.00 | --- |
| 40–59 | 7,403,610 | 20.7 [20.5–21.0] | 620 | 46.8 [40.2–53.5] | 2.95 | <0.001 |
| 60–79 | 10,515,272 | 29.4 [29.0–29.7] | 390 | 29.4 [24.0–35.5] | 1.34 | 0.263 |
| >80 | 4,886,856 | 13.7 [13.5–13.9] | 100 | 7.55 [4.83–11.60] | 0.75 | 0.386 |
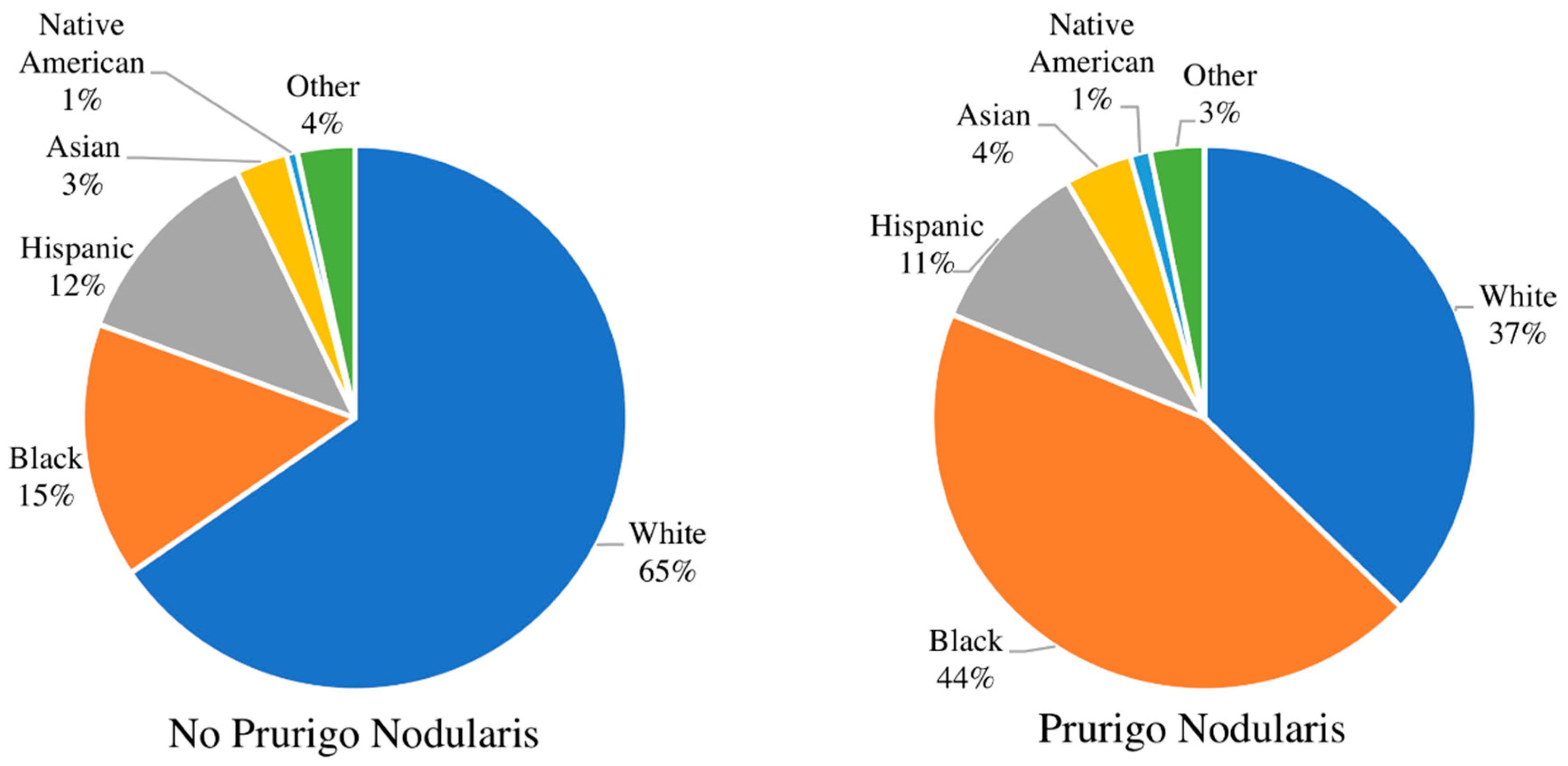
| RACE | ||||||
| White | 22,141,260 | 65.4 [64.4–66.3] | 464 | 37.2 [30.8–44.1] | 1.00 | --- |
| Black | 5,145,981 | 15.2 [14.6–15.8] | 550 | 44.0 [37.1–51.1] | 4.43 | <0.001 |
| Hispanic | 4,150,991 | 12.3 [11.6–12.9] | 130 | 10.4 [6.9–15.4] | 1.77 | 0.02 |
| Asian | 1,037,020 | 3.06 [2.83–3.32] | 50 | 4.00 [2.22–7.09] | 2.66 | 0.003 |
| Native American | 219,690 | 0.65 [0.56–0.75] | 15 | 1.20 [0.39–3.67] | 3.44 | 0.036 |
| Other | 1,156,259 | 3.42 [3.12–3.74] | 40 | 3.20 [1.63–6.20] | 1.29 | 0.586 |
| GENDER | ||||||
| Female | 15,439,345 | 43.3 [43.1–43.5] | 635 | 47.9 [41.7–54.2] | 1.00 | --- |
| Male | 20,236,076 | 56.7 [56.5–56.9] | 690 | 52.1 [45.8–58.3] | 1.00 | 0.75 |
| SEASON | ||||||
| Winter | 8,914,808 | 25.0 [25.0–25.0] | 400 | 30.2 [24.9–36.1] | 1.00 | --- |
| Spring | 9,015,068 | 25.3 [25.2–25.3] | 315 | 23.8 [19.3–29.0] | 0.81 | 0.213 |
| Summer | 8,914,118 | 25.0 [25.0–25.0] | 305 | 23.0 [18.2–28.7] | 0.73 | 0.106 |
| Fall | 8,796,723 | 24.7 [24.6–24.7] | 270 | 20.4 [15.9–25.8] | 0.72 | 0.063 |
| INCOME QUARTILE | ||||||
| First | 10,774,519 | 30.7 [29.8–31.6] | 465 | 36.9 [30.4–43.9] | 1.00 | --- |
| Second | 8,915,683 | 25.4 [24.8–26.0] | 270 | 21.4 [16.5–27.3] | 0.98 | 0.929 |
| Third | 8,387,702 | 23.9 [23.4–24.5] | 290 | 23.0 [17.9–29.1] | 1.18 | 0.398 |
| Fourth | 6,999,502 | 20.0 [19.0–20.9] | 235 | 18.7 [13.2–24.0] | 1.38 | 0.112 |
| INSURANCE | ||||||
| Medicare | 14,127,590 | 39.6 [39.1–40.1] | 645 | 49.0 [42.8–55.4] | 2.81 | <0.001 |
| Medicaid | 8,241,094 | 23.1 [22.6–23.7] | 370 | 28.1 [22.7–34.3] | 2.24 | <0.001 |
| Private | 10,734,828 | 30.1 [29.6–30.6] | 205 | 15.6 [11.6–20.7] | 1.00 | --- |
| Self-pay | 1,377,983 | 3.87 [3.71–4.03] | 65 | 4.94 [2.84–8.48] | 1.61 | 0.238 |
| No charge | 111,960 | 0.31 [0.27–0.37] | 0 | --- | ||
| Other | 1,058,214 | 2.97 [2.77–3.19] | 30 | 2.28 [1.03–4.96] | 1.28 | 0.612 |
| INSURED | ||||||
| Yes | 33,078,581 | 92.7 [92.5–92.9] | 1,220 | 92.1 [88.0–94.9] | 1.00 | --- |
| No | 1,377,983 | 3.86 [3.70–4.03] | 65 | 4.91 [2.81–8.42] | 1.00 | --- |
| Other or no charge | 1,170,174 | 3.28 [3.07–3.50] | 30 | 2.26 [1.03–4.92] | 1.00 | --- |
| REGION | ||||||
| Northeast | 6,599,084 | 18.5 [17.9–19.2] | 270 | 20.4 [15.3–26.6] | 1.00 | --- |
| Midwest | 7,933,647 | 22.2 [21.6–22.9] | 355 | 26.8 [20.2–34.6] | 1.38 | 0.14 |
| South | 14,041,126 | 39.3 [38.5–40.1] | 445 | 33.6 [26.6–41.3] | 0.91 | 0.649 |
| West | 7,122,759 | 20.0 [19.4–20.6] | 255 | 19.2 [14.0–25.9] | 1.25 | 0.328 |
| TEACHING STATUS | ||||||
| Nonteaching | 23,291,422 | 65.4 [64.7–66.1] | 1,130 | 85.3 [79.9–89.4] | 1.00 | --- |
| Teaching | 12,320,949 | 34.6 [33.9–35.3] | 195 | 14.7 [10.6–20.1] | 2.60 | <0.001 |
| HOSPITAL BED CAPACITY | ||||||
| Small | 6,674,756 | 18.7 [18.1–19.3] | 170 | 12.8 [9.1–17.7] | 1.00 | --- |
| Medium | 10,351,226 | 29.0 [28.4–29.7] | 240 | 18.1 [13.3–24.2] | 1.13 | 0.629 |
| Large | 18,632,207 | 52.2 [51.5–53.0] | 915 | 69.1 [62.1–75.2] | 2.15 | <0.001 |
| Demographic | Cost of Care | Length of Stay | ||||
|---|---|---|---|---|---|---|
| Adjusted Beta | 95% CI | p-Value | Adjusted Beta | 95% CI | p-Value | |
| AGE, y | ||||||
| 0–17 | Reference | |||||
| 18–39 | 8980.12 | [2271.54–15688.7] | 0.009 | 3.46 | [0.93–5.99] | 0.007 |
| 40–59 | 10306.25 | [3295.591–17316.91] | 0.004 | 2.72 | [0.20–5.24] | 0.034 |
| 60–79 | 17129.11 | [8512.382–25745.83] | <0.001 | 3.74 | [0.99–6.50] | 0.008 |
| >80 | 7701.64 | [−1590.12–16993.42] | 0.104 | 1.06 | [−2.43–4.57] | 0.55 |
| SEASON | ||||||
| Winter | Reference | |||||
| Spring | 2428.98 | [−3651.91–8509.88] | 0.433 | 0.34 | [−2.05–2.74] | 0.776 |
| Summer | −2276.29 | [−6883.1–2330.51] | 0.333 | −2.08 | [−4.08–−0.08] | 0.041 |
| Fall | −1365.68 | [−6400.697–3669.33] | 0.595 | −2.06 | [−4.28–0.15] | 0.069 |
| GENDER | ||||||
| Female | Reference | |||||
| Male | −2927.89 | [-7155.95–1300.16] | 0.175 | −0.23 | [−1.84–1.38] | 0.781 |
| RACE | ||||||
| White | Reference | |||||
| Black | −696.01 | [−5725.16–4333.13] | 0.786 | 0.18 | [−2.06–2.42] | 0.875 |
| Hispanic | 2806.11 | [−4865.536–10477.76] | 0.473 | −0.28 | [−2.97–2.42] | 0.841 |
| Asian | 5474.29 | [−1684.91–12633.5] | 0.134 | −0.38 | [−3.27–2.50] | 0.794 |
| Native American | 5100.59 | [−9957.69–20158.88] | 0.507 | 4.44 | [−3.10–11.99] | 0.248 |
| Other | −6695.23 | [−14271.62–881.14] | 0.083 | −2.55 | [−5.51–0.41] | 0.092 |
| INCOME QUARTILE | ||||||
| First | Reference | |||||
| Second | 1357.71 | [−4561.79–7277.22] | 0.653 | 1.47 | [−1.26–4.20] | 0.29 |
| Third | −326.29 | [−4849.39–4196.79] | 0.888 | 0.25 | [−1.59–2.09] | 0.793 |
| Fourth | 2211.26 | [−5600.19–10022.73] | 0.579 | −0.41 | [−2.73–1.90] | 0.725 |
| INSURANCE | ||||||
| Medicare | 3799.07 | [−2029.32–9627.46] | 0.201 | 2.14 | [−0.31–4.59] | 0.87 |
| Medicaid | 4274.12 | [−666.47–9214.72] | 0.09 | 2.14 | [−0.07–4.35] | 0.058 |
| Private | Reference | |||||
| Self-pay | −200.49 | [−6367.36–5966.37] | 0.949 | 0.23 | [−2.88–3.32] | 0.886 |
| No charge | ||||||
| Other | 355.35 | [−8232.30–8943.01] | 0.935 | 3.37 | [−0.96–7.70] | 0.127 |
| REGION | ||||||
| Northeast | Reference | |||||
| Midwest | 1947.42 | [−5246.55–9141.39] | 0.596 | −0.84 | [−3.76–2.08] | 0.573 |
| South | 951.9 | [−4984.18–6888.00] | 0.753 | 0.12 | [−2.44–2.68] | 0.929 |
| West | 2914.19 | [−4681.94–10510.34] | 0.452 | −0.48 | [−3.35–2.40] | 0.745 |
| TEACHING STATUS | ||||||
| Nonteaching | Reference | |||||
| Teaching | 1639.64 | [−2697.30–5976.59] | 0.459 | −0.22 | [−2.15-1.70] | 0.819 |
| HOSPITAL BED CAPACITY | ||||||
| Small | Reference | |||||
| Medium | 5096.48 | [−1453.24–11646.2] | 0.127 | 0.51 | [−2.35–3.37] | 0.727 |
| Large | 7446.41 | [1527.81–13365.01] | 0.014 | 0.6 | [−1.57–2.77] | 0.587 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Whang, K.A.; Kang, S.; Kwatra, S.G. Inpatient Burden of Prurigo Nodularis in the United States. Medicines 2019, 6, 88. https://doi.org/10.3390/medicines6030088
Whang KA, Kang S, Kwatra SG. Inpatient Burden of Prurigo Nodularis in the United States. Medicines. 2019; 6(3):88. https://doi.org/10.3390/medicines6030088
Chicago/Turabian StyleWhang, Katherine A., Sewon Kang, and Shawn G. Kwatra. 2019. "Inpatient Burden of Prurigo Nodularis in the United States" Medicines 6, no. 3: 88. https://doi.org/10.3390/medicines6030088
APA StyleWhang, K. A., Kang, S., & Kwatra, S. G. (2019). Inpatient Burden of Prurigo Nodularis in the United States. Medicines, 6(3), 88. https://doi.org/10.3390/medicines6030088





