Pruritus Associated with Commonly Prescribed Medications in a Tertiary Care Center
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Medications of Interest
2.3. Statistical Analysis
3. Results
3.1. Demographics
3.2. Rates of Pruritus within Three Months of Receiving Drug
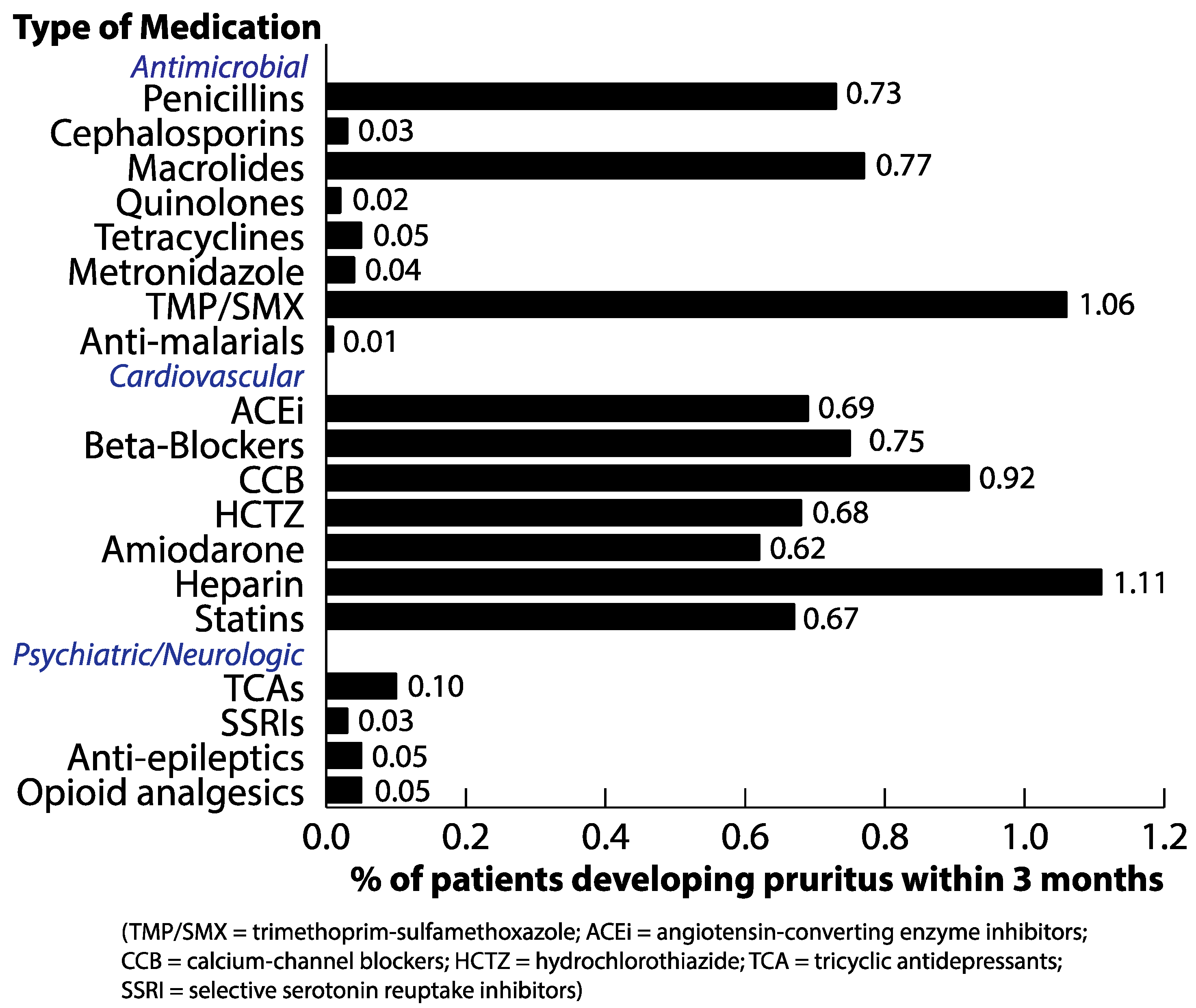
3.3. Rates of Drug Eruption among Patients with Pruritus Subsequent to Receiving Drug
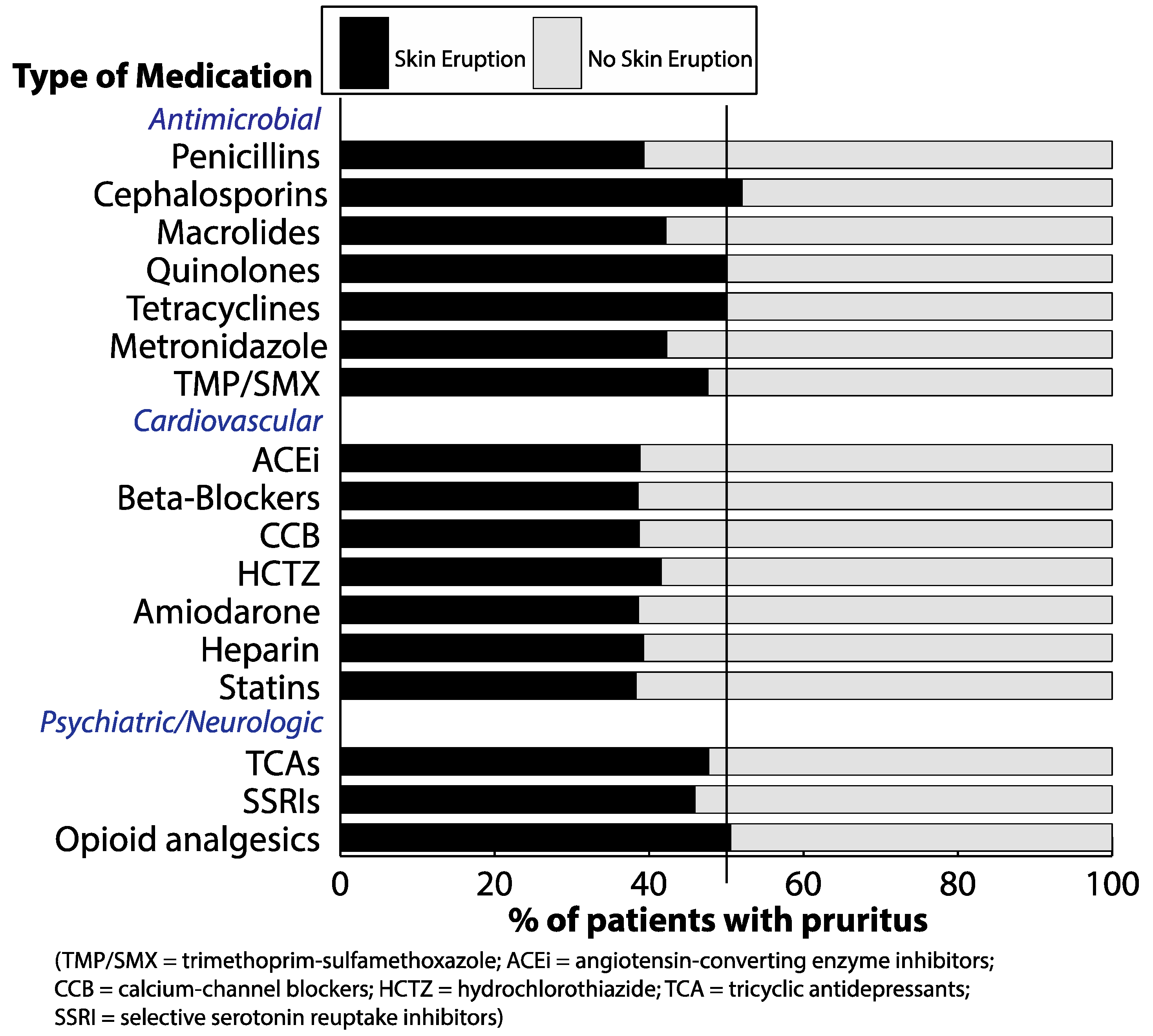
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Reich, A.; Stander, S.; Szepietowski, J.C. Drug-induced pruritus: A review. Acta Derm. Venereol. 2009, 89, 236–244. [Google Scholar] [CrossRef] [PubMed]
- Peharda, V.; Gruber, F.; Kastelan, M.; Brajac, I.; Cabrijan, L. Pruritus an important symptom of internal diseases. Acta Dermatoven. APA 2000, 9, 92–104. [Google Scholar]
- Garibyan, L.; Chiou, A.S.; Elmariah, S.B. Advanced aging skin and itch: Addressing an unmet need. Dermatol. Ther. 2013, 26, 92–103. [Google Scholar] [CrossRef] [PubMed]
- Ajayi, A.A.; Kolawole, B.A.; Udoh, S.J. Endogenous opioids, µ-opiate receptors and chloroquine-induced pruritus: A double-blind comparison of naltrexone and promethazine in patients with malaria fever who have an established history of generalized chloroquine-induced itching. Int. J. Dermatol. 2004, 43, 972–977. [Google Scholar] [CrossRef] [PubMed]
- Larson, V.A.; Tang, O.; Kang, S.; Kwatra, S.G. Association between itch and cancer in 16,925 patients with pruritus: Experience at a tertiary care center. J. Am. Acad. Dermatol. 2019, 80, 931–937. [Google Scholar] [CrossRef] [PubMed]
- Summers, E.M.; Bingham, C.S.; Dahle, K.W.; Sweeney, C.; Ying, J.; Sontheimer, R.D. Chronic eczematous eruptions in the aging: Further support for an association with exposure to calcium channel blockers. JAMA Dermatol. 2013, 149, 814–818. [Google Scholar] [CrossRef] [PubMed]
- Steckelings, U.; Artuc, M.; Wollschlager, T.; Wiehstutz, S.; Henz, B. Angiotensin-converting enzyme inhibitors as inducers of adverse cutaneous reactions. Acta Derm. Venereol. 2001, 81, 321–325. [Google Scholar] [CrossRef] [PubMed]
- Steinhoff, M.; Cevikbas, F.; Ikoma, A.; Berger, T.G. Pruritus: Management algorithms and experimental therapies. Semin. Cutan. Med. Surg. 2011, 30, 127–137. [Google Scholar] [CrossRef] [PubMed]
- Schindewolf, M.; Schwaner, S.; Wolter, M.; Kroll, H.; Recke, A.; Kaufmann, R.; Boehncke, W.H.; Lindhoff-Last, E.; Ludwig, R.J. Incidence and causes of heparin-induced skin lesions. Can. Med. Assoc. J. 2009, 181, 477–481. [Google Scholar] [CrossRef] [PubMed]
- Trautmann, A.; Seitz, C.S. Heparin allergy: Delayed-type non-ige-mediated allergic hypersensitivity to subcutaneous heparin injection. Immunol. Allergy Clin. N. Am. 2009, 29, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Waxler, B.; Dadabhoy, Z.P.; Stojiljkovic, L.; Rabito, S.F. Primer of Postoperative pruritus for anesthesiologists. Anesthesiology 2005, 103, 168–178. [Google Scholar] [CrossRef] [PubMed]
- Reich, A.; Szepietowski, J.C. Opioid-induced pruritus: an update. Clin. Exp. Dermatol. 2009, 35, 2–6. [Google Scholar] [CrossRef] [PubMed]
- Alzolibani, A.A.; Zedan, K. Macrolides in chronic inflammatory skin disorders. Mediat. Inflamm. 2012, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Luo, J.; Feng, J.; Liu, S.; Walters, E.T.; Hu, H. Molecular and cellular mechanisms that initiate pain and itch. Cell Mol. Life Sci. 2015, 72, 3201–3223. [Google Scholar] [CrossRef] [PubMed]
- Ajayi, A.A.L. Itching, chloroquine, and malaria: A review of recent molecular and neuroscience advances and their contribution to mechanistic understanding and therapeutics of chronic non-histaminergic pruritus. Int. J. Dermatol. 2019, 58, 880–891. [Google Scholar] [CrossRef] [PubMed]
- Rademaker, M. Do women have more adverse drug reactions? Am. J. Clin. Dermatol. 2001, 2, 349–351. [Google Scholar] [CrossRef] [PubMed]
| Demographic | With Pruritus within 3 Months of Drug (n = 9802) | Without Pruritus After Receiving Drug (n = 1,085,404) | p-Value * | p-Value ** |
|---|---|---|---|---|
| Gender, (%) | ||||
| Male | 30.6 | 42.4 | <0.001 | <0.001 |
| Female | 69.4 | 57.6 | <0.001 | |
| Age, (%) | ||||
| 18–29 | 8.9 | 10.9 | <0.001 | <0.001 |
| 30–39 | 11.8 | 13.8 | <0.001 | |
| 40–49 | 12.6 | 13.5 | 0.009 | |
| 50–59 | 19.1 | 17.6 | <0.001 | |
| 60–69 | 20.4 | 18.8 | <0.001 | |
| 70–79 | 16.3 | 14.8 | <0.001 | |
| 80–89 | 8.4 | 7.6 | 0.003 | |
| 90–99 | 2.4 | 2.8 | 0.017 | |
| 100+ | 0.1 | 0.2 | 0.027 | |
| Race (%) | ||||
| White/Caucasian | 48.1 | 62.8 | <0.001 | <0.001 |
| Black/African American | 38.9 | 23.1 | <0.001 | |
| Asian | 4.2 | 4.3 | 0.627 | |
| American Indian/Alaska Native | 0.4 | 0.3 | 0.072 | |
| Native Hawaiian/Pacific Islander | 0.2 | 0.1 | 0.002 | |
| Other | 7.7 | 7.4 | 0.259 | |
| Unknown | 0.5 | 1.8 | <0.001 | |
| Declined to answer | 0.2 | 0.3 | 0.071 |
| Drug Type | Number Who Received Drug (N) |
|---|---|
| Antimicrobial | |
| Penicillins | 177,487 |
| Cephalosporins | 252,342 |
| Macrolides | 124,856 |
| Quinolones | 128,248 |
| Tetracyclines | 87,497 |
| Metronidazole | 66,074 |
| TMP/SMX | 73,579 |
| Anti-malarials | 80,949 |
| Cardiovascular | |
| ACEi | 185,216 |
| Beta-blockers | 234,114 |
| CCB | 202,116 |
| HCTZ | 100,771 |
| Amiodarone | 18,357 |
| Heparin | 163,607 |
| Statins | 316,196 |
| Psychiatric/Neurologic | |
| TCAs | 43,756 |
| SSRIs | 212,244 |
| Anti-epileptics | 38,147 |
| Opioid analgesics | 592,255 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, A.H.; Kaffenberger, B.H.; Reich, A.; Szepietowski, J.C.; Ständer, S.; Kwatra, S.G. Pruritus Associated with Commonly Prescribed Medications in a Tertiary Care Center. Medicines 2019, 6, 84. https://doi.org/10.3390/medicines6030084
Huang AH, Kaffenberger BH, Reich A, Szepietowski JC, Ständer S, Kwatra SG. Pruritus Associated with Commonly Prescribed Medications in a Tertiary Care Center. Medicines. 2019; 6(3):84. https://doi.org/10.3390/medicines6030084
Chicago/Turabian StyleHuang, Amy H., Benjamin H. Kaffenberger, Adam Reich, Jacek C. Szepietowski, Sonja Ständer, and Shawn G. Kwatra. 2019. "Pruritus Associated with Commonly Prescribed Medications in a Tertiary Care Center" Medicines 6, no. 3: 84. https://doi.org/10.3390/medicines6030084
APA StyleHuang, A. H., Kaffenberger, B. H., Reich, A., Szepietowski, J. C., Ständer, S., & Kwatra, S. G. (2019). Pruritus Associated with Commonly Prescribed Medications in a Tertiary Care Center. Medicines, 6(3), 84. https://doi.org/10.3390/medicines6030084







